Abstract
Patients with chronic spontaneous urticaria (CSU) have a higher risk of developing hypertension. This study aimed to determine whether acupuncture could decrease the risk of hypertension in patients with CSU. We enrolled patients newly diagnosed with CSU between 1 January 2008, and 31 December 2018, from the Taiwanese National Health Insurance Research Database. The claims data were assessed from the index date to 31 December 2019. A Cox regression model was used to compare the hazard ratios (HRs) of the two cohorts. The cumulative incidence of hypertension was estimated using the Kaplan–Meier method. After propensity score matching with a 1:1 ratio, 43,547 patients with CSU who received acupuncture were matched with 43,547 patients with CSU who did not receive acupuncture in this study. After considering potential confounding factors, patients who received acupuncture had a significantly lower risk of hypertension than those in the control group (adjusted hazard ratio = 0.56, 95% confidence interval = 0.54–0.58). Patients who received medications combined with acupuncture tended to have the lowest risk of hypertension. This study revealed that acupuncture decreases the risk of hypertension in patients with CSU in Taiwan. The detailed mechanisms can be further clarified through prospective studies.
1. Introduction
Hypertension is a disease that is highly prevalent worldwide and increases the risk of several fatal conditions, such as ischemic stroke, intracerebral hemorrhage, acute myocardial infarction, heart failure, and aortic dissection [1,2,3]. Hypertension is the most prevalent modifiable risk factor for premature cardiovascular disease, even when compared to cigarette smoking, dyslipidemia, and diabetes [4]. The exact etiology and mechanism of primary hypertension remain unclear, but the risk factors, such as age, obesity, family history, race, and a high-sodium diet, are well-known [5]. The more risk factors we become aware of, the better we can prevent or control hypertension.
A previous study found that chronic idiopathic urticaria (CIU) was associated with a higher risk of hypertension [6]. This study reminded us that patients with CIU may be considered for the evaluation of masked hypertension. CIU is an intractable skin disease characterized by persistent intense itching, wheals, and/or angioedema lasting for six weeks or longer, as opposed to acute urticaria, which does not have any specific identifiable triggers. The terms “chronic urticaria,” “chronic idiopathic urticaria,” and “chronic spontaneous urticaria” have been used interchangeably, but “chronic spontaneous urticaria,” or CSU, has been most widely used by specialists [7], as it emphasizes an endogenous cause and non-inducible nature. Another study reported that hypertension is associated with an extended duration of CSU [8]. However, CSU and hypertension, which belong to different medical specialties, have rarely been discussed together in modern medicine.
Acupuncture has been widely used in Asian [9,10,11] and Western countries [12,13,14,15]. In Taiwan, the National Health Insurance (NHI) program provides coverage for more than 23 million residents. Traditional Chinese medicine (TCM) services, including acupuncture, have been reimbursed since 1996 [16]. The Taiwanese National Health Insurance Research Database (NHIRD) includes demographic, diagnostic, interventional, and long-term follow-up data on more than 99% of the population in Taiwan [17]. A study found that 23% of people in Taiwan used acupuncture from 1996 to 2002 [9]. Another study revealed that acupuncture was increasingly popular in Taiwan from 2002 to 2011 [18]. Acupuncture is often used in combination with Western medications. To determine whether acupuncture could decrease the risk of hypertension in patients with CSU, we used the NHIRD to conduct a population-based cohort study.
The study was conducted between 2008 and 2019 and included patients with CSU who received acupuncture or not. The primary endpoint was the occurrence of hypertension. The two cohorts were matched through 1:1 propensity score matching by age, sex, index year, comorbidities, medications, monthly income, urbanization level, and occupation. The study included 43,547 patients with CSU receiving acupuncture matched with 43,547 patients with CSU who did not receive acupuncture. The results showed that the acupuncture group had a significantly lower risk of hypertension than those in the control group (adjusted HR = 0.58, 95% confidence interval (CI) = 0.55–0.60). In the interaction analysis, patients receiving medications combined with acupuncture tended to have the lowest risk of hypertension.
2. Materials and Methods
2.1. Data Source
We used data from the NHIRD from January 1, 2008, to December 31, 2019, as our data source, provided by the Health and Welfare Data Science Center (HWDC) of the Ministry of Health and Welfare of Taiwan. Healthcare information, including outpatient visits, hospital admissions, and prescription medications, was used in this study, and the International Classification of Disease, Ninth & Tenth Revision, Clinical Modification (ICD-9-CM & ICD-10-CM) recorded disease diagnoses. NHIRD provides a large sample size and reduces selection bias while including long-term follow-up data. HWDC policies ensure the safety and privacy of this data source. The institutional review board of China Medical University (CMUH110- REC1-038[CR-2]) has approved this study.
2.2. Study Population
The study population comprised patients with CSU (ICD 9 708.1, ICD 10 L50.1). Patients who received acupuncture between 2008 and 2018 were defined as the acupuncture cohort and those who did not receive acupuncture were defined as the non-acupuncture cohort. The index date was the first date of acupuncture in the acupuncture cohort, whereas a random date between 2008 and 2018 was the index date in the non-acupuncture cohort. We excluded patients who had missing sex or age data (1.3%) and those who had any hypertension diagnosis before the index date. In addition, the two cohorts were matched through 1:1 propensity score matching by age, sex, index year, comorbidities, medications, monthly income, urbanization level, and occupation. A flow chart for study design is shown in the Supplementary Materials (Figure S1).
2.3. Primary Endpoint and Confounding Variables
The occurrence of hypertension (ICD 9 401-405, ICD 10 I10-I15) between 2008 and 2019 was considered the primary endpoint. Hypertension patients were identified at least twice from principal/secondary diagnoses in outpatient visits or one visit with hospitalizations from 2008 to 2019 during the follow-up period. All patients were followed from the index date to the occurrence of hypertension, death, withdrawal from the NHI program, or 31 December 2019. Patients with diabetes mellitus or hyperlipidemia comorbidities or those receiving cetirizine, desloratadine, fexofenadine, levocetirizine, or loratadine medications before the endpoint were included as confounding variables. In addition, patient characteristics including monthly income, urbanization level, and occupation were considered.
2.4. Statistical Analysis
Continuous variables of patient characteristics were presented as means and standard errors, and categorical variables were presented as numbers and percentages. The differences between the two cohorts were evaluated using Student’s t-test and χ2 test. Univariate and multivariate Cox regression models were used to estimate the crude hazard ratio (HR) and adjusted HR of hypertension associated with risk factors. The multivariate analysis included age, sex, comorbidities, medications, monthly income, urbanization level, and occupation. The competing-risk regression models accounted for the competing risk of death and computed the subhazard ratio (SHR) of hypertension. Kaplan–Meier survival curves were plotted to compare the cumulative incidence rate of hypertension, and the log-rank test was used to examine the differences between the acupuncture and non-acupuncture cohorts. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) or R Studio (version 3.5.2).
3. Results
3.1. Demographic Characteristics of Study Population
Table 1 shows the 43,547 patients with CSU receiving acupuncture matched with 43,547 patients with CSU who did not receive acupuncture in this study. The average ages of the acupuncture and non-acupuncture cohorts were 40.1 ± 13.0 years and 40.2 ± 13.2 years, respectively. Approximately 68% of patients with CSU were female. The majority of patients had white-collar occupations and lived in areas of urbanization level 1. The number of patients with diabetes mellitus or hyperlipidemia did not differ between the two cohorts (p > 0.05). The proportions of patients with CSU, with and without acupuncture, who were on medication were as follows: cetirizine (86.1% vs. 79.2%), desloratadine (42.2% vs. 36.0%), fexofenadine (93.7% vs. 89.1%), levocetirizine (71.5% vs. 63.0%), and loratadine (72.0% vs. 65.3%).

Table 1.
Demographic characteristics of the non-acupuncture and acupuncture groups in patients. with chronic spontaneous urticaria.
3.2. Risk of Hypertension According to Whether the CSU Patients Underwent Acupuncture and Other Covariates
The risk of hypertension according to the presence of covariates is presented in Table 2. The results showed that patients treated with acupuncture had a significantly lower risk of hypertension than those in the control group (adjusted HR = 0.58, 95% confidence interval (CI) = 0.55–0.60). The Kaplan–Meier curves in Figure 1 shows a visual picture of the cumulative incidence of hypertension. Patients with comorbidities had a significantly higher risk of hypertension (adjusted HR = 1.15 and 1.51 for type 2 diabetes and hyperlipidemia, respectively, both p < 0.001). In contrast, patients receiving medication had a significantly lower risk of hypertension (adjusted HRs < 1, p < 0.001). Compared to white-collar occupation patients, blue-collar occupation patients had a significantly higher risk of hypertension (adjusted HR = 1.22, 95% CI = 1.17–1.28, p < 0.001), while other patients had a significantly lower risk of hypertension (adjusted HR = 0.79, 95% CI = 0.62–0.99). Patients who lived in urbanization level 2 (adjusted HR = 1.23, 95% CI = 1.03–1.46, p = 0.02) and level 3 (adjusted HR = 1.31, 95% CI = 1.09–1.58, p = 0.004) areas had a greater risk of hypertension than those who lived in urbanization level 4 areas. Moreover, patients with a monthly income lower than NTD 20,000 had a higher risk than those with a monthly income greater than NTD 40,000 (adjusted HR = 1.42, 95% CI = 1.13–1.79, p = 0.001).

Table 2.
Cox model with hazard ratio and 95% confidence interval of hypertension with receiving acupuncture and other covariates among the patients with chronic spontaneous urticaria.
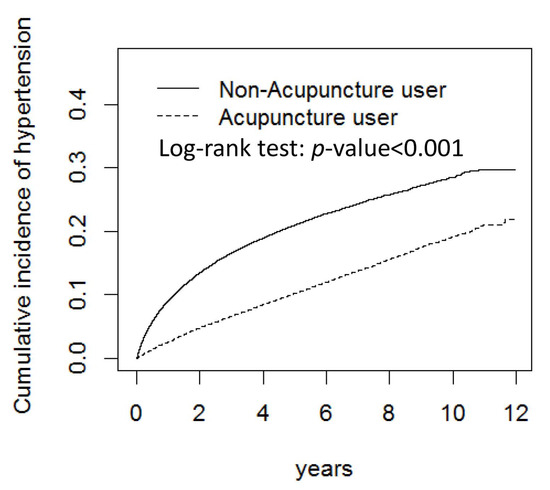
Figure 1.
The cumulative incidence of hypertension during the follow-up period between the acupuncture and no-acupuncture groups.
3.3. Risk of Hypertension among Patients with CSU Who Received and Did Not Receive Acupuncture
Table 3 shows that regardless of sex, age, comorbidities, and medications, acupuncture users tended to have a lower risk of hypertension than non-acupuncture users (all adjusted HRs < 1, p <0.001). The results showed that patients treated with acupuncture had a significantly lower risk of hypertension than those without acupuncture treatment (adjusted HR = 0.52, 95% confidence interval (CI) = 0.50–0.55 for female and adjusted HR = 0.56, 95% confidence interval (CI) = 0.53–0.60 for male). Table 4 shows the SHRs of hypertension in the acupuncture and non-acupuncture cohorts. Patients receiving acupuncture had a lower risk of hypertension than those in the control group (adjusted SHR = 0.56, 95% CI = 0.54–0.58) after adjusting for potential confounding factors.

Table 3.
Incidence rates, hazard ratios, and confidence intervals of hypertension for patients with CSU who received and did not receive acupuncture, stratified by sex, age, comorbidities, and medications.

Table 4.
Accepted acupuncture cohort to no-acupuncture cohort subhazard ratio of hypertension estimated using competing-risk regression models.
3.4. The Interaction EFFECT of Medication and Acupuncture on Hypertension
In the interaction analysis, Table 5 shows that patients who received medications, acupuncture, or combined therapy, tended to have a lower risk of hypertension compared to the nontherapy group. The group taking medications combined with acupuncture showed the lowest risk of hypertension (adjusted HR = 0.10, 95% CI = 0.09–0.12, p-value < 0.001).

Table 5.
Incidence and hazard ratios of hypertension among different therapy groups.
4. Discussion
To our knowledge, this is the first study to demonstrate that the risk of hypertension in patients with CSU can be decreased by acupuncture, using data from the NHIRD with Cox regression models. The main findings of our study are as follows: (1) the benefits of acupuncture for reducing the incidence of hypertension in patients with CSU were independent of sex, age, baseline comorbidities, and drug use, and (2) the group taking medication combined with acupuncture had the lowest risk of hypertension.
The association between hypertension and CSU may be attributed to alterations in the endothelium and blood coagulation/fibrinolysis pathways [6]. Recent studies have reported that systemic hypertension is commonly associated with a procoagulant state [19]. Other studies have suggested that the coagulation cascade pathway may contribute to the pathogenesis of CSU. A recent study by Yuhki et al. suggested that medications targeting activated coagulation factors and/or complement components may represent new and effective treatments for patients with severe and refractory CSU [20]. A double-blind placebo-controlled study by Parslew et al. showed a response of CSU to warfarin [21].
Moreover, the association between hypertension and CSU may be related to inflammation [6]. Recent studies have found an association between inflammation markers and hypertension, and a study by Wang et al. found that biomarkers such as C-reactive protein (CRP) and plasminogen activator inhibitor-1 were significantly related to incident hypertension [22]. Studies have suggested that inflammation markers such as pentraxin-3 and CRP may be useful for the assessment of CSU disease activity [23,24].
In addition, hypertension and CSU may be linked to autoimmunity [6]. Mathis et al. suggested that the presence of self-antigens and the subsequent activation of the adaptive immune system against them may promote the development of hypertension [25]. Several studies have reported that oral cyclosporine and omalizumab are effective in treating patients with CSU, and the results provide further evidence supporting the hypothesis of an autoimmune pathogenesis of CSU [26,27,28].
The mechanism of the protective effect of acupuncture against hypertension in patients with CSU may involve the following three pathways: first, a study by Elisabet et al. found that low-frequency electroacupuncture counteracted a possible prothrombotic state in women with polycystic ovary syndrome [29], suggesting that the improvement of coagulation/fibrinolysis is a possible mechanism; second, the World Health Organization recommends acupuncture for the treatment of 16 types of inflammatory diseases [30], and several clinical studies have investigated whether acupuncture could treat inflammatory diseases and decrease CRP levels [31,32], suggesting an anti-inflammatory mechanism; and third, a study by Wang et al. suggested that acupuncture therapy has had promising results in a variety of autoimmune diseases, including multiple sclerosis, irritable bowel disease, rheumatoid arthritis, myasthenia gravis, systemic lupus erythematosus, and ankylosing spondylitis [33]. Another study by Sun Kwang Kim suggested that acupuncture enhances natural killer cell activity and can have dual immunomodulatory effects on either Th1- or Th2-skewed conditions to maintain homeostasis [34], altogether indicating an immunoregulatory mechanism.
Mental health disorders are associated with both CSU and hypertension. Several studies have suggested that anxiety and depression are associated with a higher risk of hypertension [35,36,37,38]. A study by Hamam suggested that physicians treating patients with hypertension should be aware of the role that anxiety and depression play in treatment efficacy and compliance [39]. Several studies have revealed that patients with CSU frequently have anxiety and depression, which are probably exacerbated by the symptoms of itching and sleep disturbance [40,41,42,43]. Studies have suggested that acupuncture treatment can alleviate anxiety and depression [44,45,46,47], which may benefit patients with CSU by decreasing the risk of hypertension.
One strength of our study is the use of population-based data that were highly representative of the general population. As more than 99% of patients in Taiwan are enrolled in the NHIRD, the external validity of the findings could be enhanced. However, the present results should be interpreted in light of the limitations arising from the nature of the retrospective analysis and characteristics of the NHIRD database. The evidence derived from retrospective cohort studies is generally of lower statistical quality than that derived from randomized trials because of potential bias related to the adjustments for confounding variables. Information on patient factors was not recorded in the NHIRD, and many important potential confounders were not controlled for in this analysis, which may result in residual confounding factors, such as family history, body mass index, diet, physical activity, smoking, alcohol consumption, and hypnotic medications. In addition, people using acupuncture may require more management by medications, and they may have an especially unique approach to treatment or may be more conscious of their health issues and management; therefore, self-selection bias may occur. Primary and secondary hypertension were not separated into groups in our study, which could also have led to some bias. In addition, the NHIRD database did not reveal the acupoints for CSU treatment; therefore, the mechanism of action of acupoints remains unclear.
Although the definite relationship between CSU and hypertension remains unclear, we discuss several possible pathways by which acupuncture decreases the risk of hypertension in patients with CSU. Further prospective studies using single or several acupoints, according to TCM theories or modern medical mechanisms, with or without Western medications, to investigate their relationships, may uncover clinically applicable strategies. These may be more effective in helping patients with CSU become aware of hypertension and receive a better diagnosis and treatment in advance, which will help improve disease prevention.
5. Conclusions
Our study found that acupuncture decreases the risk of hypertension in patients with CSU in Taiwan. Among the different therapy groups, medication combined with acupuncture was associated with the lowest risk of hypertension. This suggests that patients with CSU may choose acupuncture as an adjuvant therapy combined with regular medications for CSU symptoms to prevent the incidence of hypertension. The detailed mechanisms require further clarification in future prospective studies.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare11101510/s1, Figure S1: flow chart.
Author Contributions
Conceptualization, H.-W.C. and M.-F.S.; methodology, C.-Y.H. and P.-J.S.; validation, C.-L.L. and W.-L.L.; formal analysis, W.-L.L.; investigation, W.-D.L. and H.-W.C.; resources, C.-L.L.; data curation, W.-L.L.; writing—original draft preparation, H.-W.C.; writing—review and editing, H.-W.C. and M.-F.S.; visualization, S.-L.P.; supervision, W.-D.L.; project administration, M.-F.S.; funding acquisition, H.-W.C. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported in part by National Science and Technology Council (NSTC 112-2321-B-039-006), Ministry of Science and Technology (MOST 111-2321-B-039-005) and the China Medical University Hospital (DMR-111-105; DMR-112-087). We are grateful to the Health Data Science Center, China Medical University Hospital for providing administrative, technical, and funding support. The funders had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation. No additional external funding was received for the study.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of China Medical University Hospital (CMUH110- REC1-038[CR-2]).
Informed Consent Statement
Since the patient identifications in the NHIRD have been scrambled, encrypted and de-identified by the Taiwan government for academic research use, the informed consent was waived by the Research Ethics Committee of the China Medical University Hospital.
Data Availability Statement
The dataset used in this study was obtained from the Taiwan Ministry of Health and Welfare (MOHW). The Ministry of Health and Welfare must approve of the application to access these data. Any researcher interested in accessing this dataset can submit an application form to the Ministry of Health and Welfare to request access. Please contact the staff of the MOHW (Email: stcarolwu@mohw.gov.tw) for further assistance. Taiwan Ministry of Health and Welfare Address: No.488, Sec. 6, Zhongxiao E. Rd., Nangang Dist., Taipei City 115, Taiwan (R.O.C.). Phone: +886-2-8590-6848.
Acknowledgments
This study was based in part on data from the NHIRD, which were provided by the National Health Insurance Administration and the Ministry of Health and Welfare and managed by the National Health Research Institutes. The interpretations and conclusions contained herein do not represent those of the National Health Insurance Administration, Ministry of Health and Welfare, or the National Health Research Institutes.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kokubo, Y.; Kamide, K.; Okamura, T.; Watanabe, M.; Higashiyama, A.; Kawanishi, K.; Okayama, A.; Kawano, Y. Impact of high-normal blood pressure on the risk of cardiovascular disease in a Japanese urban cohort: The Suita study. Hypertension 2008, 52, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Evangelista, A.; Isselbacher, E.M.; Bossone, E.; Gleason, T.G.; Eusanio, M.D.; Sechtem, U.; Ehrlich, M.P.; Trimarchi, S.; Braverman, A.C.; Myrmel, T.; et al. Insights From the International Registry of Acute Aortic Dissection: A 20-Year Experience of Collaborative Clinical Research. Circulation 2018, 137, 1846–1860. [Google Scholar] [CrossRef] [PubMed]
- Di Palo, K.E.; Barone, N.J. Hypertension and Heart Failure: Prevention, Targets, and Treatment. Heart Fail. Clin. 2020, 16, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.W. Established risk factors and coronary artery disease: The Framingham Study. Am. J. Hypertens. 1994, 7, 7S–12S. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, e13–e115. [Google Scholar] [CrossRef]
- Chang, H.W.; Cheng, H.M.; Yen, H.R.; Hsu, C.Y.; Lee, Y.C.; Chiang, J.H.; Sun, M.F. Association between chronic idiopathic urticaria and hypertension: A population-based retrospective cohort study. Ann. Allergy Asthma Immunol. 2016, 116, 554–558. [Google Scholar] [CrossRef]
- Zuberbier, T.; Aberer, W.; Asero, R.; Abdul Latiff, A.H.; Baker, D.; Ballmer-Weber, B.; Bernstein, J.A.; Bindslev-Jensen, C.; Brzoza, Z.; Buense Bedrikow, R.; et al. The EAACI/GA(2)LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. Allergy 2018, 73, 1393–1414. [Google Scholar] [CrossRef]
- Nebiolo, F.; Bergia, R.; Bommarito, L.; Bugiani, M.; Heffler, E.; Carosso, A.; Castiglioni, G.; Guida, G.; Badiu, I.; Pizzimenti, S.; et al. Effect of arterial hypertension on chronic urticaria duration. Ann. Allergy Asthma Immunol. 2009, 103, 407–410. [Google Scholar] [CrossRef]
- Chen, F.P.; Kung, Y.Y.; Chen, T.J.; Hwang, S.J. Demographics and patterns of acupuncture use in the Chinese population: The Taiwan experience. J. Altern. Complement. Med. 2006, 12, 379–387. [Google Scholar] [CrossRef]
- Ishizaki, N.; Yano, T.; Kawakita, K. Public status and prevalence of acupuncture in Japan. Evid. Based Complement. Altern. Med. 2010, 7, 493–500. [Google Scholar] [CrossRef]
- Hwang, J.H.; Han, D.W.; Yoo, E.K.; Kim, W.Y. The utilisation of Complementary and Alternative Medicine (CAM) among ethnic minorities in South Korea. BMC Complement. Altern. Med. 2014, 14, 103. [Google Scholar] [CrossRef] [PubMed]
- Upchurch, D.M.; Rainisch, B.W. A sociobehavioral wellness model of acupuncture use in the United States, 2007. J. Altern. Complement. Med. 2014, 20, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Vincent, A.; Kruk, K.M.; Cha, S.S.; Bauer, B.A.; Martin, D.P. Utilisation of acupuncture at an academic medical centre. Acupunct. Med. 2010, 28, 189–190. [Google Scholar] [CrossRef]
- Cramer, H.; Chung, V.C.; Lauche, R.; Zhang, Y.; Zhang, A.; Langhorst, J.; Dobos, G. Characteristics of acupuncture users among internal medicine patients in Germany. Complement. Ther. Med. 2015, 23, 423–429. [Google Scholar] [CrossRef]
- Xue, C.C.; Zhang, A.L.; Lin, V.; Myers, R.; Polus, B.; Story, D.F. Acupuncture, chiropractic and osteopathy use in Australia: A national population survey. BMC Public Health 2008, 8, 105. [Google Scholar] [CrossRef]
- Huang, M.C.; Yen, H.R.; Lin, C.L.; Lee, Y.C.; Sun, M.F.; Wu, M.Y. Acupuncture decreased the risk of stroke among patients with fibromyalgia in Taiwan: A nationwide matched cohort study. PLoS ONE 2020, 15, e0239703. [Google Scholar] [CrossRef]
- Hsing, A.W.; Ioannidis, J.P. Nationwide Population Science: Lessons From the Taiwan National Health Insurance Research Database. JAMA Intern. Med. 2015, 175, 1527–1529. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.Y.; Lee, Y.C.; Lin, C.L.; Huang, M.C.; Sun, M.F.; Yen, H.R. Trends in use of acupuncture among adults in Taiwan from 2002 to 2011: A nationwide population-based study. PLoS ONE 2018, 13, e0195490. [Google Scholar] [CrossRef] [PubMed]
- Makris, T.K.; Stavroulakis, G.A.; Krespi, P.G.; Hatzizacharias, A.N.; Triposkiadis, F.K.; Tsoukala, C.G.; Votteas, V.V.; Kyriakidis, M.K. Fibrinolytic/hemostatic variables in arterial hypertension: Response to treatment with irbesartan or atenolol. Am. J. Hypertens. 2000, 13, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Yanase, Y.; Takahagi, S.; Ozawa, K.; Hide, M. The Role of Coagulation and Complement Factors for Mast Cell Activation in the Pathogenesis of Chronic Spontaneous Urticaria. Cells 2021, 10, 1759. [Google Scholar] [CrossRef]
- Parslew, R.; Pryce, D.; Ashworth, J.; Friedmann, P.S. Warfarin treatment of chronic idiopathic urticaria and angio-oedema. Clin. Exp. Allergy 2000, 30, 1161–1165. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.J.; Gona, P.; Larson, M.G.; Levy, D.; Benjamin, E.J.; Tofler, G.H.; Jacques, P.F.; Meigs, J.B.; Rifai, N.; Selhub, J.; et al. Multiple biomarkers and the risk of incident hypertension. Hypertension 2007, 49, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Takahagi, S.; Mihara, S.; Iwamoto, K.; Morioke, S.; Okabe, T.; Kameyoshi, Y.; Hide, M. Coagulation/fibrinolysis and inflammation markers are associated with disease activity in patients with chronic urticaria. Allergy 2010, 65, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Kasperska-Zajac, A.; Grzanka, A.; Misiolek, M.; Mazur, B.; Machura, E. Pentraxin-3 as a local inflammatory marker in chronic spontaneous urticaria. Cytokine 2015, 76, 566–568. [Google Scholar] [CrossRef] [PubMed]
- Mathis, K.W.; Broome, H.J.; Ryan, M.J. Autoimmunity: An underlying factor in the pathogenesis of hypertension. Curr. Hypertens. Rep. 2014, 16, 424. [Google Scholar] [CrossRef]
- Agache, I.; Rocha, C.; Pereira, A.; Song, Y.; Alonso-Coello, P.; Sola, I.; Beltran, J.; Posso, M.; Akdis, C.A.; Akdis, M.; et al. Efficacy and safety of treatment with omalizumab for chronic spontaneous urticaria: A systematic review for the EAACI Biologicals Guidelines. Allergy 2021, 76, 59–70. [Google Scholar] [CrossRef]
- Tharp, M.D.; Bernstein, J.A.; Kavati, A.; Ortiz, B.; MacDonald, K.; Denhaerynck, K.; Abraham, I.; Lee, C.S. Benefits and Harms of Omalizumab Treatment in Adolescent and Adult Patients With Chronic Idiopathic (Spontaneous) Urticaria: A Meta-analysis of “Real-world” Evidence. JAMA Dermatol. 2019, 155, 29–38. [Google Scholar] [CrossRef]
- Toubi, E.; Blant, A.; Kessel, A.; Golan, T.D. Low-dose cyclosporin A in the treatment of severe chronic idiopathic urticaria. Allergy 1997, 52, 312–316. [Google Scholar] [CrossRef]
- Stener-Victorin, E.; Baghaei, F.; Holm, G.; Janson, P.O.; Olivecrona, G.; Lonn, M.; Manneras-Holm, L. Effects of acupuncture and exercise on insulin sensitivity, adipose tissue characteristics, and markers of coagulation and fibrinolysis in women with polycystic ovary syndrome: Secondary analyses of a randomized controlled trial. Fertil. Steril. 2012, 97, 501–508. [Google Scholar] [CrossRef]
- Li, N.; Guo, Y.; Gong, Y.; Zhang, Y.; Fan, W.; Yao, K.; Chen, Z.; Dou, B.; Lin, X.; Chen, B.; et al. The Anti-Inflammatory Actions and Mechanisms of Acupuncture from Acupoint to Target Organs via Neuro-Immune Regulation. J. Inflamm. Res. 2021, 14, 7191–7224. [Google Scholar] [CrossRef]
- Inci, H.; Inci, F. Acupuncture Effects on Blood Parameters in Patients with Fibromyalgia. Med. Acupunct. 2021, 33, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Shi, G.X.; Tu, J.F.; Wang, T.Q.; Yang, J.W.; Wang, L.Q.; Lin, L.L.; Wang, Y.; Li, Y.T.; Liu, C.Z. Effect of Electro-Acupuncture (EA) and Manual Acupuncture (MA) on Markers of Inflammation in Knee Osteoarthritis. J. Pain. Res. 2020, 13, 2171–2179. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhu, F.; Huang, W.; Chen, Z.; Zhao, P.; Lei, Y.; Liu, Y.; Liu, X.; Sun, B.; Li, H. Therapeutic Effect and Mechanism of Acupuncture in Autoimmune Diseases. Am. J. Chin. Med. 2022, 50, 639–652. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.K.; Bae, H. Acupuncture and immune modulation. Auton. Neurosci. 2010, 157, 38–41. [Google Scholar] [CrossRef]
- Ginty, A.T.; Carroll, D.; Roseboom, T.J.; Phillips, A.C.; de Rooij, S.R. Depression and anxiety are associated with a diagnosis of hypertension 5 years later in a cohort of late middle-aged men and women. J. Hum. Hypertens. 2013, 27, 187–190. [Google Scholar] [CrossRef]
- Sensoy, B.; Gunes, A.; Ari, S. Anxiety and depression levels in Covid-19 disease and their relation to hypertension. Clin. Exp. Hypertens. 2021, 43, 237–241. [Google Scholar] [CrossRef]
- Scalco, A.Z.; Scalco, M.Z.; Azul, J.B.; Lotufo Neto, F. Hypertension and depression. Clinics 2005, 60, 241–250. [Google Scholar] [CrossRef]
- Bergantin, L.B. Depression Rises the Risk of Hypertension Incidence: Discussing the Link through the Ca2+/cAMP Signalling. Curr. Hypertens. Rev. 2020, 16, 73–78. [Google Scholar] [CrossRef]
- Hamam, M.S.; Kunjummen, E.; Hussain, M.S.; Nasereldin, M.; Bennett, S.; Miller, J. Anxiety, Depression, and Pain: Considerations in the Treatment of Patients with Uncontrolled Hypertension. Curr. Hypertens. Rep. 2020, 22, 106. [Google Scholar] [CrossRef]
- Choi, G.S.; Nam, Y.H.; Park, C.S.; Kim, M.Y.; Jo, E.J.; Park, H.K.; Kim, H.K. Anxiety, depression, and stress in Korean patients with chronic urticaria. Korean J. Intern. Med. 2020, 35, 1507–1516. [Google Scholar] [CrossRef]
- Huang, Y.; Xiao, Y.; Jing, D.; Li, J.; Zhang, J.; Chen, X.; Shen, M. Association of Chronic Spontaneous Urticaria with Anxiety and Depression in Adolescents: A Mediation Analysis. Front. Psychiatry 2021, 12, 655802. [Google Scholar] [CrossRef]
- Tat, T.S. Higher Levels of Depression and Anxiety in Patients with Chronic Urticaria. Med. Sci. Monit. 2019, 25, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Tzur Bitan, D.; Berzin, D.; Cohen, A. The association of chronic spontaneous urticaria (CSU) with anxiety and depression: A nationwide cohort study. Arch. Dermatol. Res. 2021, 313, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Amorim, D.; Amado, J.; Brito, I.; Fiuza, S.M.; Amorim, N.; Costeira, C.; Machado, J. Acupuncture and electroacupuncture for anxiety disorders: A systematic review of the clinical research. Complement. Ther. Clin. Pract. 2018, 31, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.A.; de Lacey, S.; Chapman, M.; Ratcliffe, J.; Norman, R.J.; Johnson, N.P.; Fahey, P. The effects of acupuncture on the secondary outcomes of anxiety and quality of life for women undergoing IVF: A randomized controlled trial. Acta Obstet. Gynecol. Scand. 2019, 98, 460–469. [Google Scholar] [CrossRef]
- Armour, M.; Smith, C.A.; Wang, L.Q.; Naidoo, D.; Yang, G.Y.; MacPherson, H.; Lee, M.S.; Hay, P. Acupuncture for Depression: A Systematic Review and Meta-Analysis. J. Clin. Med. 2019, 8, 1140. [Google Scholar] [CrossRef]
- Liu, C.; Zhao, Y.; Qin, S.; Wang, X.; Jiang, Y.; Wu, W. Randomized controlled trial of acupuncture for anxiety and depression in patients with chronic insomnia. Ann. Transl. Med. 2021, 9, 1426. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).