Translation and Validation of the Arabic Version of the Athlete Sleep Screening Questionnaire
Abstract
1. Introduction
2. Background
3. Materials and Methods
3.1. Study Design
3.2. Translation Procedure
3.3. Participants
3.4. Procedure
3.5. Outcome Measures
3.6. Statistical Analysis
4. Results
4.1. Cross-Cultural Adaptation
4.2. Study Participants
4.3. Floor and Ceiling Effects
4.4. Internal Consistency
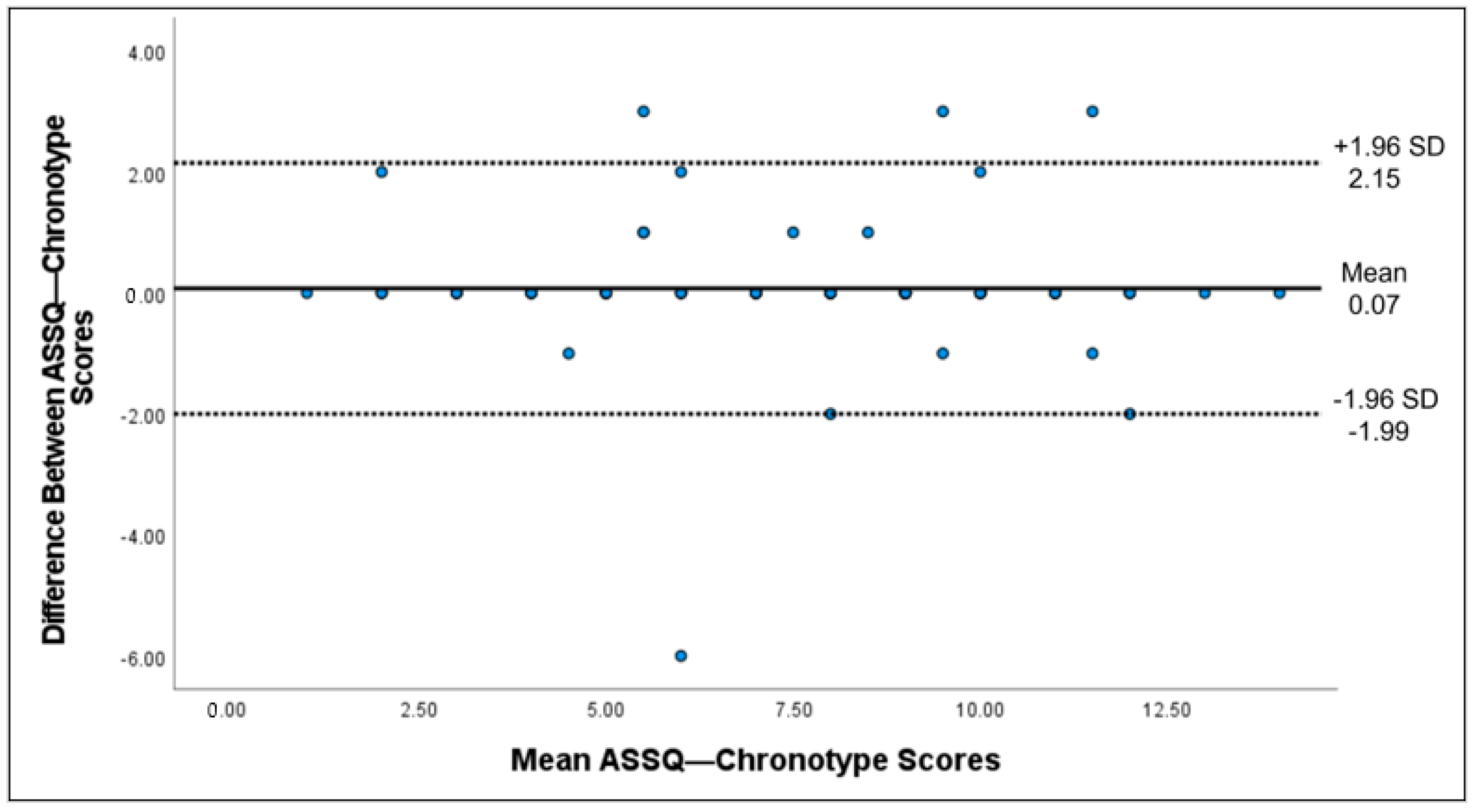
4.5. Test-Retest Reliability
4.6. Convergent Validity
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Roberts, S.S.H.; Teo, W.P.; Warmington, S.A. Effects of training and competition on the sleep of elite athletes: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 513–522. [Google Scholar] [CrossRef] [PubMed]
- Fallon, K.E. Blood tests in tired elite athletes: Expectations of athletes, coaches and sport science/sports medicine staff. Br. J. Sports Med. 2007, 41, 41–44. [Google Scholar] [CrossRef]
- Nédélec, M.; McCall, A.; Carling, C.; Legall, F.; Berthoin, S.; Dupont, G. Recovery in soccer: Part ii: Recovery strategies. Sports Med. 2013, 43, 9–22. [Google Scholar] [CrossRef] [PubMed]
- Nédélec, M.; Halson, S.; Abaidia, A.E.; Ahmaidi, S.; Dupont, G. Stress, sleep and recovery in elite soccer: A critical review of the literature. Sports Med. 2015, 45, 1387–1400. [Google Scholar] [CrossRef] [PubMed]
- Chennaoui, M.; Arnal, P.J.; Drogou, C.; Sauvet, F.; Gomez-Merino, D. Sleep extension increases IGF-I concentrations before and during sleep deprivation in healthy young men. Appl. Physiol. Nutr. Metab. 2016, 41, 963–970. [Google Scholar] [CrossRef] [PubMed]
- Frank, M.G.; Benington, J.H. The role of sleep in memory consolidation and brain plasticity: Dream or reality? Neuroscientist 2006, 12, 477–488. [Google Scholar] [CrossRef]
- Besedovsky, L.; Lange, T.; Born, J. Sleep and immune function. Pflügers Arch. Eur. J. Physiol. 2012, 463, 121–137. [Google Scholar] [CrossRef]
- Halson, S.L. Sleep in elite athletes and nutritional interventions to enhance sleep. Sports Med. 2014, 44 (Suppl. 1), S13–S23. [Google Scholar] [CrossRef]
- Samuels, C. Sleep, recovery, and performance: The new frontier in high-performance athletics. Neurol. Clin. 2008, 26, 169–180. [Google Scholar] [CrossRef]
- Allada, R.; Siegel, J.M. Unearthing the phylogenetic roots of sleep. Curr Biol. 2008, 18, R670–R679. [Google Scholar] [CrossRef]
- Crocker, A.; Sehgal, A. Genetic analysis of sleep. Genes Dev. 2010, 24, 1220–1235. [Google Scholar] [CrossRef] [PubMed]
- Abel, T.; Havekes, R.; Saletin, J.M.; Walker, M.P. Sleep, plasticity and memory from molecules to whole-brain networks. Curr. Biol. 2013, 23, R774–R788. [Google Scholar] [CrossRef] [PubMed]
- Xie, L.; Kang, H.; Xu, Q.; Chen, M.J.; Liao, Y.; Thiyagarajan, M.; O’Donnell, J.; Christensen, D.J.; Nicholson, C.; Iliff, J.J.; et al. Sleep drives metabolite clearance from the adult brain. Science 2013, 342, 373–377. [Google Scholar] [CrossRef]
- Bishop, D. An applied research model for the sport sciences. Sports Med. 2008, 38, 253–263. [Google Scholar] [CrossRef] [PubMed]
- Drust, B.; Waterhouse, J.; Atkinson, G.; Edwards, B.; Reilly, T. Circadian rhythms in sports performance: An update. Chronobiol. Int. 2005, 22, 21–44. [Google Scholar] [CrossRef] [PubMed]
- Beersma, D.G.; Gordijn, M.C. Circadian control of the sleep-wake cycle. Physiol. Behav. 2007, 90, 190–195. [Google Scholar] [CrossRef]
- Fullagar, H.H.; Skorski, S.; Duffield, R.; Hammes, D.; Coutts, A.J.; Meyer, T. Sleep and athletic performance: The effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med. 2015, 45, 161–186. [Google Scholar] [CrossRef]
- Czeisler, C.A.; Allan, J.S.; Strogatz, S.H.; Ronda, J.M.; Sánchez, R.; Ríos, C.D.; Freitag, W.O.; Richardson, G.S.; Kronauer, R.E. Bright light resets the human circadian pacemaker independent of the timing of the sleep-wake cycle. Science 1986, 233, 667–671. [Google Scholar] [CrossRef]
- Reilly, T.; Edwards, B. Altered sleep-wake cycles and physical performance in athletes. Physiol. Behav. 2007, 90, 274–284. [Google Scholar] [CrossRef]
- Lack, L.C.; Wright, H.R. Chronobiology of sleep in humans. Cell. Mol. Life Sci. 2007, 64, 1205–1215. [Google Scholar] [CrossRef]
- Halson, S.L. Nutrition, sleep and recovery. Eur. J. Sport Sci. 2008, 8, 119–126. [Google Scholar] [CrossRef]
- Goel, N.; Rao, H.; Durmer, J.S.; Dinges, D.F. Neurocognitive consequences of sleep deprivation. Semin. Neurol. 2009, 29, 320–339. [Google Scholar] [CrossRef] [PubMed]
- Banks, S.; Dinges, D.F. Behavioral and physiological consequences of sleep restriction. J. Clin. Sleep Med. 2007, 3, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Robey, E.; Dawson, B.; Halson, S.; Gregson, W.; Goodman, C.; Eastwood, P. Sleep quantity and quality in elite youth soccer players: A pilot study. Eur. J. Sport Sci. 2014, 14, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Samuels, C. Sleep, recovery, and performance: The new frontier in high-performance athletics. Phys. Med. Rehabil. Clin. N. Am. 2009, 20, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Caia, J.; Kelly, V.G.; Halson, S.L. The role of sleep in maximising performance in elite athletes. In Sport, Recovery, and Performance, 1st ed.; Routledge: New York, NY, USA, 2017; pp. 151–167. [Google Scholar] [CrossRef]
- Walsh, N.P.; Halson, S.L.; Sargent, C.; Roach, G.D.; Nédélec, M.; Gupta, L.; Leeder, J.; Fullagar, H.H.; Coutts, A.J.; Edwards, B.J.; et al. Sleep and the athlete: Narrative review and 2021 expert consensus recommendations. Br. J. Sports Med. 2021, 55, 356–368. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.M.; Carskadon, M.A.; Guilleminault, C.; Vitiello, M.V. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep 2004, 27, 1255–1273. [Google Scholar] [CrossRef] [PubMed]
- Fullagar, H.H.; Duffield, R.; Skorski, S.; Coutts, A.J.; Julian, R.; Meyer, T. Sleep and recovery in team sport: Current sleep-related issues facing professional team-sport athletes. Int. J. Sports Physiol. Perform. 2015, 10, 950–957. [Google Scholar] [CrossRef]
- Gupta, L.; Morgan, K.; Gilchrist, S. Does elite sport degrade sleep quality? A systematic review. Sports Med. 2017, 47, 1317–1333. [Google Scholar] [CrossRef] [PubMed]
- Fietze, I.; Strauch, J.; Holzhausen, M.; Glos, M.; Theobald, C.; Lehnkering, H.; Penzel, T. Sleep quality in professional ballet dancers. Chronobiol. Int. 2009, 26, 1249–1262. [Google Scholar] [CrossRef]
- Swinbourne, R.; Gill, N.; Vaile, J.; Smart, D. Prevalence of poor sleep quality, sleepiness and obstructive sleep apnoea risk factors in athletes. Eur. J. Sport Sci. 2016, 16, 850–858. [Google Scholar] [CrossRef] [PubMed]
- Tuomilehto, H.; Vuorinen, V.P.; Penttilä, E.; Kivimäki, M.; Vuorenmaa, M.; Venojärvi, M.; Airaksinen, O.; Pihlajamäki, J. Sleep of professional athletes: Underexploited potential to improve health and performance. J. Sports Sci. 2017, 35, 704–710. [Google Scholar] [CrossRef] [PubMed]
- Knufinke, M.; Nieuwenhuys, A.; Geurts, S.A.E.; Coenen, A.M.L.; Kompier, M.A.J. Self-reported sleep quantity, quality and sleep hygiene in elite athletes. J. Sleep Res. 2018, 27, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Monma, T.; Ando, A.; Asanuma, T.; Yoshitake, Y.; Yoshida, G.; Miyazawa, T.; Ebine, N.; Takeda, S.; Omi, N.; Satoh, M.; et al. Sleep disorder risk factors among student athletes. Sleep Med. 2018, 44, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Lastella, M.; Roach, G.D.; Halson, S.L.; Sargent, C. Sleep/wake behaviours of elite athletes from individual and team sports. Eur. J. Sport Sci. 2015, 15, 94–100. [Google Scholar] [CrossRef]
- Leeder, J.; Glaister, M.; Pizzoferro, K.; Dawson, J.; Pedlar, C. Sleep duration and quality in elite athletes measured using wristwatch actigraphy. J. Sports Sci. 2012, 30, 541–545. [Google Scholar] [CrossRef]
- Sargent, C.; Halson, S.; Roach, G.D. Sleep or swim? Early-morning training severely restricts the amount of sleep obtained by elite swimmers. Eur. J. Sport Sci. 2014, 14 (Suppl. 1), S310–S315. [Google Scholar] [CrossRef]
- Samuels, C.; James, L.; Lawson, D.; Meeuwisse, W. The Athlete Sleep Screening Questionnaire: A new tool for assessing and managing sleep in elite athletes. Br. J. Sports Med. 2016, 50, 418–422. [Google Scholar] [CrossRef]
- Bender, A.M.; Samuels, C.H. Comment on: “Does elite sport degrade sleep quality? A systematic review”. Sports Med. 2017, 47, 1453–1454. [Google Scholar] [CrossRef]
- Driller, M.W.; Mah, C.D.; Halson, S.L. Development of the athlete sleep behavior questionnaire: A tool for identifying maladaptive sleep practices in elite athletes. Sleep Sci. 2018, 11, 37–44. [Google Scholar] [CrossRef]
- Bender, A.M.; Lawson, D.; Werthner, P.; Samuels, C.H. The clinical validation of the athlete sleep screening questionnaire: An instrument to identify athletes that need further sleep assessment. Sports Med. Open 2018, 4, 23. [Google Scholar] [CrossRef]
- Gouttebarge, V.; Bindra, A.; Blauwet, C.; Campriani, N.; Currie, A.; Engebretsen, L.; Hainline, B.; Kroshus, E.; McDuff, D.; Mountjoy, M.; et al. International Olympic Committee (IOC) Sport Mental Health Assessment Tool 1 (SMHAT-1) and Sport Mental Health Recognition Tool 1 (SMHRT-1): Towards better support of athletes’ mental health. Br. J. Sports Med. 2021, 55, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Huskey, A.; Kim, K.; Emert, S.; Auerbach, A.; Webb, R.; Skog, M.; Grandner, M.; Taylor, D. 315 athlete sleep and mental health: Differences by gender, race, and ethnicity. Sleep 2021, 44 (Suppl. 2), A125–A126. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef] [PubMed]
- Chan, L.L.; Idris, N. Validity and reliability of the instrument using exploratory factor analysis and Cronbach’s alpha. Int. J. Acad. Res. Bus. Soc. Sci. 2017, 7, 400–410. [Google Scholar] [CrossRef]
- De Winter, J.C.; Dodou, D.; Wieringa, P.A. Exploratory factor analysis with small sample sizes. Multivar. Behav. Res. 2009, 44, 147–181. [Google Scholar] [CrossRef]
- Omachi, T.A. Measures of sleep in rheumatologic diseases: Epworth Sleepiness Scale (ESS), Functional Outcome of Sleep Questionnaire (FOSQ), Insomnia Severity Index (ISI), and Pittsburgh Sleep Quality Index (PSQI). Arthritis Care Res. 2011, 63 (Suppl. 11), S287–S296. [Google Scholar] [CrossRef]
- Terwee, C.B.; Bot, S.D.; de Boer, M.R.; van der Windt, D.A.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef]
- Portney, M.P.W.; Gross, L. Foundations of Clinical Research: Applications to Practice, 3rd ed.; Prentice Hall: Upper Saddle River, NJ, USA, 2014. [Google Scholar]
- De Vet, H.C.W.; Terwee, C.B.; Mokkink, L.B.; Knol, D.L. Measurement in Medicine: A Practical Guide; Cambridge University Press: Cambridge, UK, 2011. [Google Scholar] [CrossRef]
- Zhang, B.; Bender, A.; Tan, X.; Wang, X.; Le, S.; Cheng, S. Assessment of sleep disturbances with the athlete sleep screening questionnaire in Chinese athletes. Sports Med. Health Sci. 2022, 4, 133–139. [Google Scholar] [CrossRef]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef]
- Tan, C.; Lu, J.; Qiu, J. Revision and validation of the Chinese version of the athlete sleeping screening questionnaire. Sports Sci. Res. 2021, 3, 1006–1207. [Google Scholar]


| Gender | |
|---|---|
| Male (n = 64) | 28.9% |
| Female (n = 26) | 71.1% |
| Hight (mean ± SD) | 170.08 ± 7.7 |
| Wight (mean ± SD) | 71.01 ± 9.01 |
| BMI (mean ± SD) | 22.03 ± 3.30 |
| Smokers, yes (n, %) | 10, (10.09%) |
| ASSQ-SDS | ASSQ-Chronotype | |
|---|---|---|
| First test | 6.49 ± 2.72 | 7.63 ± 2.98 |
| Second test | 6.12 ± 2.69 | 7.56 ± 3.00 |
| Mean difference | 0.37 | 0.07 |
| ICC (95% CI) | 0.84 (0.75–0.89) | 0.93 (0.90–0.96) |
| SEM | 1.91 | 2.11 |
| SDCindividual | 5.30 | 5.86 |
| SDCgroup | 0.59 | 0.65 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhowimel, A.S.; Alenazi, A.M.; Alshehri, M.M.; Alqahtani, B.A.; Al-Jamaan, A.; Alodaibi, F.; Alshehri, Y.S.; Charest, J. Translation and Validation of the Arabic Version of the Athlete Sleep Screening Questionnaire. Healthcare 2023, 11, 1501. https://doi.org/10.3390/healthcare11101501
Alhowimel AS, Alenazi AM, Alshehri MM, Alqahtani BA, Al-Jamaan A, Alodaibi F, Alshehri YS, Charest J. Translation and Validation of the Arabic Version of the Athlete Sleep Screening Questionnaire. Healthcare. 2023; 11(10):1501. https://doi.org/10.3390/healthcare11101501
Chicago/Turabian StyleAlhowimel, Ahmed S., Aqeel M. Alenazi, Mohammed M. Alshehri, Bader A. Alqahtani, Abdulaziz Al-Jamaan, Faris Alodaibi, Yasir S. Alshehri, and Jonathan Charest. 2023. "Translation and Validation of the Arabic Version of the Athlete Sleep Screening Questionnaire" Healthcare 11, no. 10: 1501. https://doi.org/10.3390/healthcare11101501
APA StyleAlhowimel, A. S., Alenazi, A. M., Alshehri, M. M., Alqahtani, B. A., Al-Jamaan, A., Alodaibi, F., Alshehri, Y. S., & Charest, J. (2023). Translation and Validation of the Arabic Version of the Athlete Sleep Screening Questionnaire. Healthcare, 11(10), 1501. https://doi.org/10.3390/healthcare11101501







