Cost-Effectiveness of Cerebrolysin after Ischemic Stroke: Secondary Analysis of the CARS Study
Abstract
1. Introduction
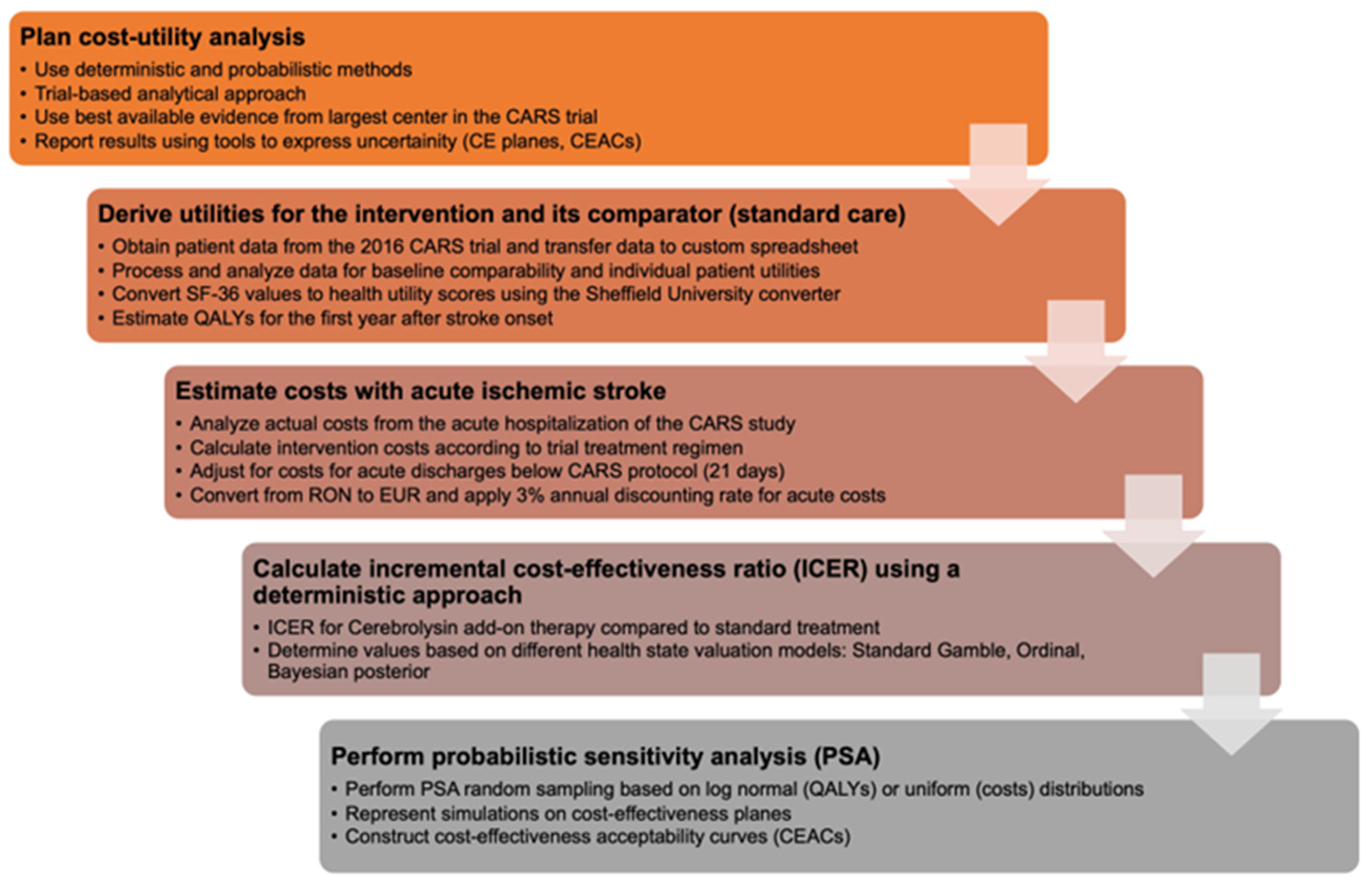
2. Materials and Methods
2.1. Deriving Utilities for the Intervention and Standard of Care
2.2. Extracting Costs with Acute Ischemic Stroke
2.3. Calculating the Incremental Cost-Effectiveness Ratio of Cerebrolysin Add-on Therapy for Ischemic Stroke Using a Deterministic Approach
2.4. Probabilistic Sensitivity Analysis
3. Results
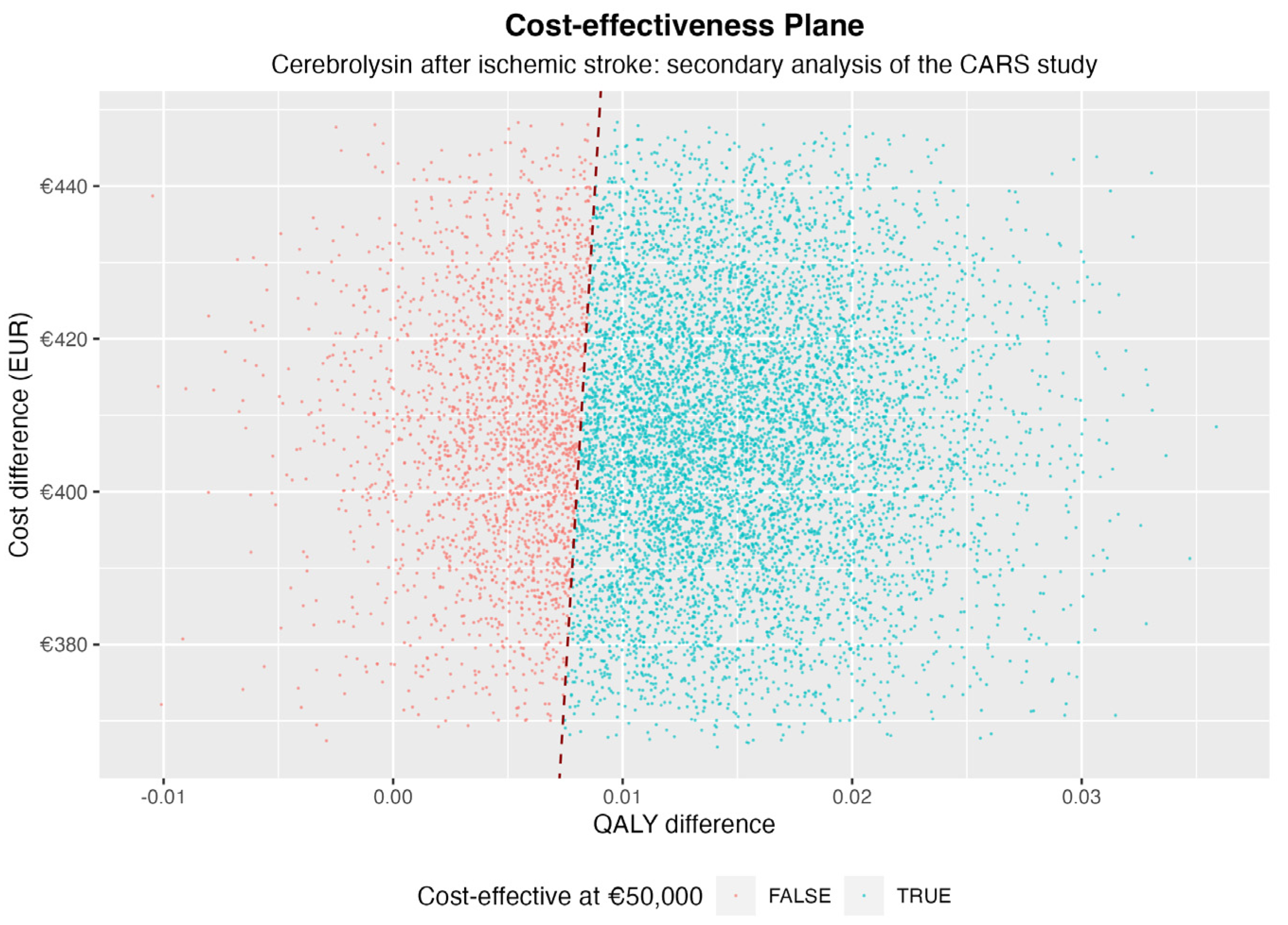
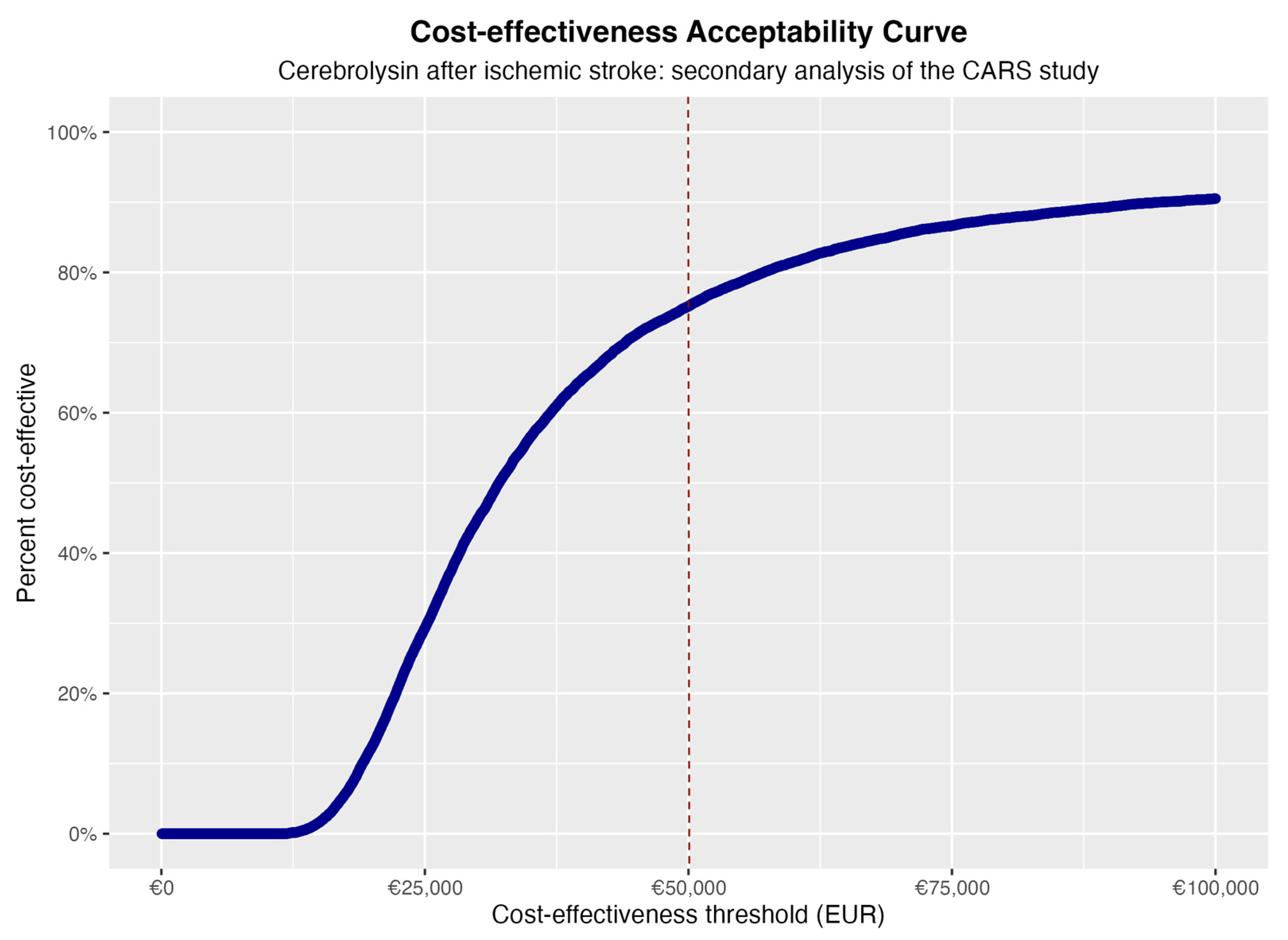
Probabilistic Sensitivity Analysis
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Feigin, V.L.; Stark, B.A.; Johnson, C.O.; Roth, G.A.; Bisignano, C.; Abady, G.G.; Abbasifard, M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abedi, V.; et al. Global, Regional, and National Burden of Stroke and Its Risk Factors, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef] [PubMed]
- Foreman, K.J.; Marquez, N.; Dolgert, A.; Fukutaki, K.; Fullman, N.; McGaughey, M.; Pletcher, M.A.; Smith, A.E.; Tang, K.; Yuan, C.-W.; et al. Forecasting Life Expectancy, Years of Life Lost, and All-Cause and Cause-Specific Mortality for 250 Causes of Death: Reference and Alternative Scenarios for 2016–40 for 195 Countries and Territories. Lancet 2018, 392, 2052–2090. [Google Scholar] [CrossRef]
- Herpich, F.; Rincon, F. Management of Acute Ischemic Stroke. Crit. Care Med. 2020, 48, 1654–1663. [Google Scholar] [CrossRef]
- Stinear, C.M.; Lang, C.E.; Zeiler, S.; Byblow, W.D. Advances and Challenges in Stroke Rehabilitation. Lancet Neurol. 2020, 19, 348–360. [Google Scholar] [CrossRef]
- Al-Jishi, A.; Saluja, R.S.; Al-Jehani, H.; Lamoureux, J.; Maleki, M.; Marcoux, J. Primary or Secondary Decompressive Craniectomy: Different Indication and Outcome. Can. J. Neurol. Sci. 2011, 38, 612–620. [Google Scholar] [CrossRef] [PubMed]
- Diener, H.C.; Rothwell, P.M. Antithrombotic Drugs in Secondary Stroke Prevention: Still Some Way to Go. Lancet 2022, 400, 974–975. [Google Scholar] [CrossRef] [PubMed]
- Kalseth, J.; Halvorsen, T. Health and Care Service Utilisation and Cost over the Life-Span: A Descriptive Analysis of Population Data. BMC Health Serv. Res. 2020, 20, 435. [Google Scholar] [CrossRef]
- Jayawardana, S.; Cylus, J.; Mossialos, E. It’s Not Ageing, Stupid: Why Population Ageing Won’t Bankrupt Health Systems. Eur. Heart J. Qual. Care Clin. Outcomes 2019, 5, 195–201. [Google Scholar] [CrossRef]
- Webb, E.; Hernández-Quevedo, C.; Williams, G.; Scarpetti, G.; Reed, S.; Panteli, D. Providing Health Services Effectively during the First Wave of COVID-19: A Cross-Country Comparison on Planning Services, Managing Cases, and Maintaining Essential Services. Health Policy 2022, 126, 382–390. [Google Scholar] [CrossRef]
- Winkelmann, J.; Webb, E.; Williams, G.A.; Hernández-Quevedo, C.; Maier, C.B.; Panteli, D. European Countries’ Responses in Ensuring Sufficient Physical Infrastructure and Workforce Capacity during the First COVID-19 Wave. Health Policy 2022, 126, 362–372. [Google Scholar] [CrossRef]
- Second Round of the National Pulse Survey on Continuity of Essential Health Services during the COVID-19 Pandemic. Available online: https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-EHS-continuity-survey-2021.1 (accessed on 6 January 2022).
- White, T.G.; Martinez, G.; Wang, J.; Gribko, M.; Boltyenkov, A.; Arora, R.; Katz, J.M.; Woo, H.H.; Sanelli, P.C. Impact of the COVID-19 Pandemic on Acute Ischemic Stroke Presentation, Treatment, and Outcomes. Stroke Res. Treat. 2021, 2021, e8653396. [Google Scholar] [CrossRef] [PubMed]
- Meza, H.T.; Lambea Gil, Á.; Saldaña, A.S.; Martínez-Zabaleta, M.; Juez, P.D.L.R.; Martínez, E.L.C.; Apilánez, M.C.; Isasi, M.H.; Enguita, J.M.; Alfonso, M.D.L.; et al. Impact of COVID-19 Outbreak on Ischemic Stroke Admissions and in-Hospital Mortality in North-West Spain. Int. J. Stroke 2020, 15, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, R.G.; Qureshi, M.M.; Abdalkader, M.; Martins, S.O.; Yamagami, H.; Qiu, Z.; Mansour, O.Y.; Sathya, A.; Czlonkowska, A.; Tsivgoulis, G.; et al. Global Impact of COVID-19 on Stroke Care and IV Thrombolysis. Neurology 2021, 96, e2824–e2838. [Google Scholar] [CrossRef]
- Zhao, J.; Li, H.; Kung, D.; Fisher, M.; Shen, Y.; Liu, R. Impact of the COVID-19 Epidemic on Stroke Care and Potential Solutions. Stroke 2020, 51, 1996–2001. [Google Scholar] [CrossRef]
- Nawabi, N.L.A.; Duey, A.H.; Kilgallon, J.L.; Jessurun, C.; Doucette, J.; Mekary, R.A.; Aziz-Sultan, M.A. Effects of the COVID-19 Pandemic on Stroke Response Times: A Systematic Review and Meta-Analysis. J. NeuroInterv. Surg. 2022, 14, 642–649. [Google Scholar] [CrossRef]
- The Territorial Impact of COVID-19: Managing the Crisis and Recovery across Levels of Government. Available online: https://www.oecd.org/coronavirus/policy-responses/the-territorial-impact-of-covid-19-managing-the-crisis-and-recovery-across-levels-of-government-a2c6abaf/ (accessed on 7 January 2022).
- McKee, M.; Suhrcke, M.; Nolte, E.; Lessof, S.; Figueras, J.; Duran, A.; Menabde, N. Health Systems, Health, and Wealth: A European Perspective. Lancet 2009, 373, 349–351. [Google Scholar] [CrossRef] [PubMed]
- Langhorne, P.; Ramachandra, S. Stroke Unit Trialists’ Collaboration Organised Inpatient (Stroke Unit) Care for Stroke: Network Meta-Analysis. Cochrane Database Syst. Rev. 2020, 4, CD000197. [Google Scholar] [CrossRef]
- Neumann, P.J.; Ganiats, T.G.; Russell, L.B.; Sanders, G.D.; Siegel, J.E.; Neumann, P.J.; Ganiats, T.G.; Russell, L.B.; Sanders, G.D.; Siegel, J.E. (Eds.) Cost-Effectiveness in Health and Medicine, 2nd ed.; Oxford University Press: Oxford, UK, 2016; ISBN 978-0-19-049293-9. [Google Scholar]
- Drummond, M.F.; Sculpher, M.J.; Claxton, K.; Stoddart, G.L.; Torrance, G.W. Methods for the Economic Evaluation of Health Care Programmes, 4th ed.; Oxford University Press: Oxford, UK, 2015; ISBN 978-0-19-966588-4. [Google Scholar]
- Bettger, J.P.; Cadilhac, D.A. Stroke Care Costs and Cost-Effectiveness to Inform Health Policy. Stroke 2022, 53, 2078–2081. [Google Scholar] [CrossRef]
- Beghi, E.; Binder, H.; Birle, C.; Bornstein, N.; Diserens, K.; Groppa, S.; Homberg, V.; Lisnic, V.; Pugliatti, M.; Randall, G.; et al. European Academy of Neurology and European Federation of Neurorehabilitation Societies Guideline on Pharmacological Support in Early Motor Rehabilitation after Acute Ischaemic Stroke. Eur. J. Neurology 2021, 28, 2831–2845. [Google Scholar] [CrossRef]
- Platz, T. Rehabilitative Therapy for Arm Paresis Following a Stroke. 2020. Available online: https://www.awmf.org/leitlinien/detail/ll/080-001.html (accessed on 6 January 2022).
- Teasell, R.; Hussein, N.; Mirkowski, M.; Vanderlaan, D.; Saikaley, M.; Longval, M.; Iruthayarajah, J. Stroke Rehabilitation Clinician Handbook; Evidence-Based Review of Stroke Rehabilitation: London, ON, Canada, 2020. [Google Scholar]
- Muresanu, D.F. Neuroplasticity and Neurorecovery. Stroke 2009, 37–49. [Google Scholar] [CrossRef]
- Strilciuc, S. Safety of Cerebrolysin for Neurorecovery after Acute Ischemic Stroke: A Systematic Review and Meta-Analysis of Twelve Randomized-Controlled Trials. Pharmaceuticals 2021, 14, 1297. [Google Scholar] [CrossRef] [PubMed]
- Bornstein, N.M.; Guekht, A.; Vester, J.; Heiss, W.-D.; Gusev, E.; Hömberg, V.; Rahlfs, V.W.; Bajenaru, O.; Popescu, B.O.; Muresanu, D. Safety and Efficacy of Cerebrolysin in Early Post-Stroke Recovery: A Meta-Analysis of Nine Randomized Clinical Trials. Neurol. Sci. 2018, 39, 629–640. [Google Scholar] [CrossRef]
- Alvarez, X.A.; Sampedro, C.; Figueroa, J.; Tellado, I.; González, A.; García-Fantini, M.; Cacabelos, R.; Muresanu, D.; Moessler, H. Reductions in QEEG Slowing over 1 Year and after Treatment with Cerebrolysin in Patients with Moderate-Severe Traumatic Brain Injury. J. Neural. Transm. 2008, 115, 683–692. [Google Scholar] [CrossRef]
- Muresanu, D.F.; Florian, S.; Hömberg, V.; Matula, C.; von Steinbüchel, N.; Vos, P.E.; von Wild, K.; Birle, C.; Muresanu, I.; Slavoaca, D.; et al. Efficacy and Safety of Cerebrolysin in Neurorecovery after Moderate-Severe Traumatic Brain Injury: Results from the CAPTAIN II Trial. Neurol. Sci. 2020, 41, 1171–1181. [Google Scholar] [CrossRef]
- Poon, W.; Matula, C.; Vos, P.E.; Muresanu, D.F.; von Steinbüchel, N.; von Wild, K.; Hömberg, V.; Wang, E.; Lee, T.M.C.; Strilciuc, S.; et al. Safety and Efficacy of Cerebrolysin in Acute Brain Injury and Neurorecovery: CAPTAIN I-a Randomized, Placebo-Controlled, Double-Blind, Asian-Pacific Trial. Neurol. Sci. 2019, 41, 281–293. [Google Scholar] [CrossRef] [PubMed]
- Kulikov, A.; Abdrashitova, G. Cost-Effectiveness Analysis of Cerebrolysin In The Treatment of Patients With Acute Ischemic Stroke Moderate and Severe Degrees of Severity In The Russian Federation. Value Health 2015, 18, A705. [Google Scholar] [CrossRef]
- Walter, E.; Bauer, M.; Ressl, S. Cost-Effectiveness Of Combined Treatment With Alteplase (Rt-Pa) And Cerebrolysin In Acute Ischemic Hemispheric Stroke In Austria. Value Health 2015, 18, A390. [Google Scholar] [CrossRef]
- Vladescu, C.; Scintee, S.G.; Olsavszky, V.; Hernandez-Quevedo, C.; Sagan, A. Romania: Health System Review. Health Syst. Transit. 2016, 18, 1–170. [Google Scholar]
- GDP per Capita (Current US$)—Romania, Data. Available online: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=RO (accessed on 16 February 2022).
- Muresanu, D.F.; Heiss, W.-D.; Hoemberg, V.; Bajenaru, O.; Popescu, C.D.; Vester, J.C.; Rahlfs, V.W.; Doppler, E.; Meier, D.; Moessler, H.; et al. Cerebrolysin and Recovery After Stroke (CARS): A Randomized, Placebo-Controlled, Double-Blind, Multicenter Trial. Stroke 2016, 47, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Calculating QALYs from the SF-36 and SF-12, Available from University of Sheffield. Available online: https://licensing.sheffield.ac.uk/product/SF-6D (accessed on 7 January 2022).
- Bernhardt, J.; Hayward, K.S.; Kwakkel, G.; Ward, N.S.; Wolf, S.L.; Borschmann, K.; Krakauer, J.W.; Boyd, L.A.; Carmichael, S.T.; Corbett, D.; et al. Agreed Definitions and a Shared Vision for New Standards in Stroke Recovery Research: The Stroke Recovery and Rehabilitation Roundtable Taskforce. Int. J. Stroke 2017, 12, 444–450. [Google Scholar] [CrossRef]
- Mauskopf, J.A.; Sullivan, S.D.; Annemans, L.; Caro, J.; Mullins, C.D.; Nuijten, M.; Orlewska, E.; Watkins, J.; Trueman, P. Principles of Good Practice for Budget Impact Analysis: Report of the ISPOR Task Force on Good Research Practices—Budget Impact Analysis. Value Health 2007, 10, 336–347. [Google Scholar] [CrossRef] [PubMed]
- Winstein, C.J.; Stein, J.; Arena, R.; Bates, B.; Cherney, L.R.; Cramer, S.C.; Deruyter, F.; Eng, J.J.; Fisher, B.; Harvey, R.L.; et al. Guidelines for Adult Stroke Rehabilitation and Recovery. Stroke 2016, 47, e98–e169. [Google Scholar] [CrossRef]
- Ringelstein, E.B.; Chamorro, A.; Kaste, M.; Langhorne, P.; Leys, D.; Lyrer, P.; Thijs, V.; Thomassen, L.; Toni, D. European Stroke Organisation Recommendations to Establish a Stroke Unit and Stroke Center. Stroke 2013, 44, 828–840. [Google Scholar] [CrossRef]
- Acțiunea Prioritară Pentru Tratamentul Intervențional Al Pacienților Cu Avc Acut Procedură Operațională Standard Privind Traseul Pacientului Și Protocolul Terapeutic; Romanian Society of Neurology: Bucharest, Romania, 2018.
- Strilciuc, S.; Grad, D.A.; Mixich, V.; Stan, A.; Buzoianu, A.D.; Vladescu, C.; Vintan, M.A. Societal Cost of Ischemic Stroke in Romania: Results from a Retrospective County-Level Study. Brain Sci. 2021, 11, 689. [Google Scholar] [CrossRef]
- Norrving, B.; Barrick, J.; Davalos, A.; Dichgans, M.; Cordonnier, C.; Guekht, A.; Kutluk, K.; Mikulik, R.; Wardlaw, J.; Richard, E.; et al. Action Plan for Stroke in Europe 2018–2030. Eur. Stroke J. 2018, 3, 309–336. [Google Scholar] [CrossRef] [PubMed]
- Vester, J.; Bornstein, N.; Heiss, W.-D.; Vosko, M.; Moessler, H.; Jech, M.; Winter, S.; Brainin, M. C-REGS 2—Design and Methodology of a High-Quality Comparative Effectiveness Observational Trial. J. Med. Life 2021, 14, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Tiu, C.; Terecoasă, E.O.; Tuță, S.; Bălașa, R.; Simu, M.; Sabău, M.; Stan, A.; Radu, R.A.; Tiu, V.; Cășaru, B.; et al. Quality of Acute Stroke Care in Romania: Achievements and Gaps between 2017 and 2022. Eur. Stroke J. 2023, 8, 44–51. [Google Scholar] [CrossRef]
- Lorenzovici, L.; Székely, A.; Csanádi, M.; Gaál, P. Cost Assessment of Inpatient Care Episodes of Stroke in Romania. Front. Public Health 2020, 8, 605919. [Google Scholar] [CrossRef]
- Strilciuc, S.; Grad, D.A.; Radu, C.; Chira, D.; Stan, A.; Ungureanu, M.; Gheorghe, A.; Muresanu, F.-D. The Economic Burden of Stroke: A Systematic Review of Cost of Illness Studies. J. Med. Life 2021, 14, 606–619. [Google Scholar] [CrossRef]
- Thokala, P.; Ochalek, J.; Leech, A.A.; Tong, T. Cost-Effectiveness Thresholds: The Past, the Present and the Future. Pharmacoeconomics 2018, 36, 509–522. [Google Scholar] [CrossRef]
- Wafa, H.A.; Wolfe, C.D.A.; Emmett, E.; Roth, G.A.; Johnson, C.O.; Wang, Y. Burden of Stroke in Europe. Stroke 2020, 51, 2418–2427. [Google Scholar] [CrossRef] [PubMed]
- Value Assessment Framework. Available online: https://icer.org/our-approach/methods-process/value-assessment-framework/ (accessed on 12 April 2023).
- Lopert, R.; Ruiz, F.; Gheorghe, A.; Chanturidze, T. Technical Assistance for institution building of Health Technology Assessment structure, including training for the National Agency for Medicines & Medical Devices. In Situational Analysis of Romanian HTA; Romanian Ministry of Health: Bucharest, Romania, 2017. [Google Scholar]
- Radu, C.-P.; Chiriac, N.D.; Pravat, A.M. The Development of the Romanian Scorecard HTA System. Value Health Reg. Issues 2016, 10, 41–47. [Google Scholar] [CrossRef] [PubMed]
- McDougall, J.A.; Furnback, W.E.; Wang, B.C.M.; Mahlich, J. Understanding the Global Measurement of Willingness to Pay in Health. J. Mark. Access Health Policy 2020, 8, 1717030. [Google Scholar] [CrossRef] [PubMed]
| Total Medical Cost Estimates | Cerebrolysin | Standard Treatment |
|---|---|---|
| Sample size | 100 | 93 |
| Mean | 1458 EUR | 1050 EUR |
| Median | 1466 EUR | 1767 EUR |
| Lower threshold (95%) | 1437 EUR | 1029 EUR |
| Upper threshold (95%) | 1478 EUR | 1070 EUR |
| Standard deviation | 106 EUR | 101 EUR |
| Valuation Technique | QALYs Derived from CARS | Deterministic ICER (EUR) | |
|---|---|---|---|
| Cerebrolysin | Standard Treatment | ||
| Bayesian posterior | 0.166 | 0.156 | €26,981 |
| Ordinal | 0.182 | 0.168 | €18,788 |
| Standard gamble | 0.186 | 0.171 | €20,618 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strilciuc, S.; Radu, C.; Grad, D.-A.; Stan, A.D.; Vladescu, C.; Buzoianu, A.D.; Muresanu, D. Cost-Effectiveness of Cerebrolysin after Ischemic Stroke: Secondary Analysis of the CARS Study. Healthcare 2023, 11, 1497. https://doi.org/10.3390/healthcare11101497
Strilciuc S, Radu C, Grad D-A, Stan AD, Vladescu C, Buzoianu AD, Muresanu D. Cost-Effectiveness of Cerebrolysin after Ischemic Stroke: Secondary Analysis of the CARS Study. Healthcare. 2023; 11(10):1497. https://doi.org/10.3390/healthcare11101497
Chicago/Turabian StyleStrilciuc, Stefan, Constantin Radu, Diana-Alecsandra Grad, Adina Dora Stan, Cristian Vladescu, Anca Dana Buzoianu, and Dafin Muresanu. 2023. "Cost-Effectiveness of Cerebrolysin after Ischemic Stroke: Secondary Analysis of the CARS Study" Healthcare 11, no. 10: 1497. https://doi.org/10.3390/healthcare11101497
APA StyleStrilciuc, S., Radu, C., Grad, D.-A., Stan, A. D., Vladescu, C., Buzoianu, A. D., & Muresanu, D. (2023). Cost-Effectiveness of Cerebrolysin after Ischemic Stroke: Secondary Analysis of the CARS Study. Healthcare, 11(10), 1497. https://doi.org/10.3390/healthcare11101497







