Barriers and Facilitators of Communication in the Medication Reconciliation Process during Hospital Discharge: Primary Healthcare Professionals’ Perspectives
Abstract
1. Introduction
2. Materials and Method
2.1. Setting and Participants
2.2. Data Collection
2.3. Data Analysis
2.4. Trustworthiness
2.5. Ethical Considerations
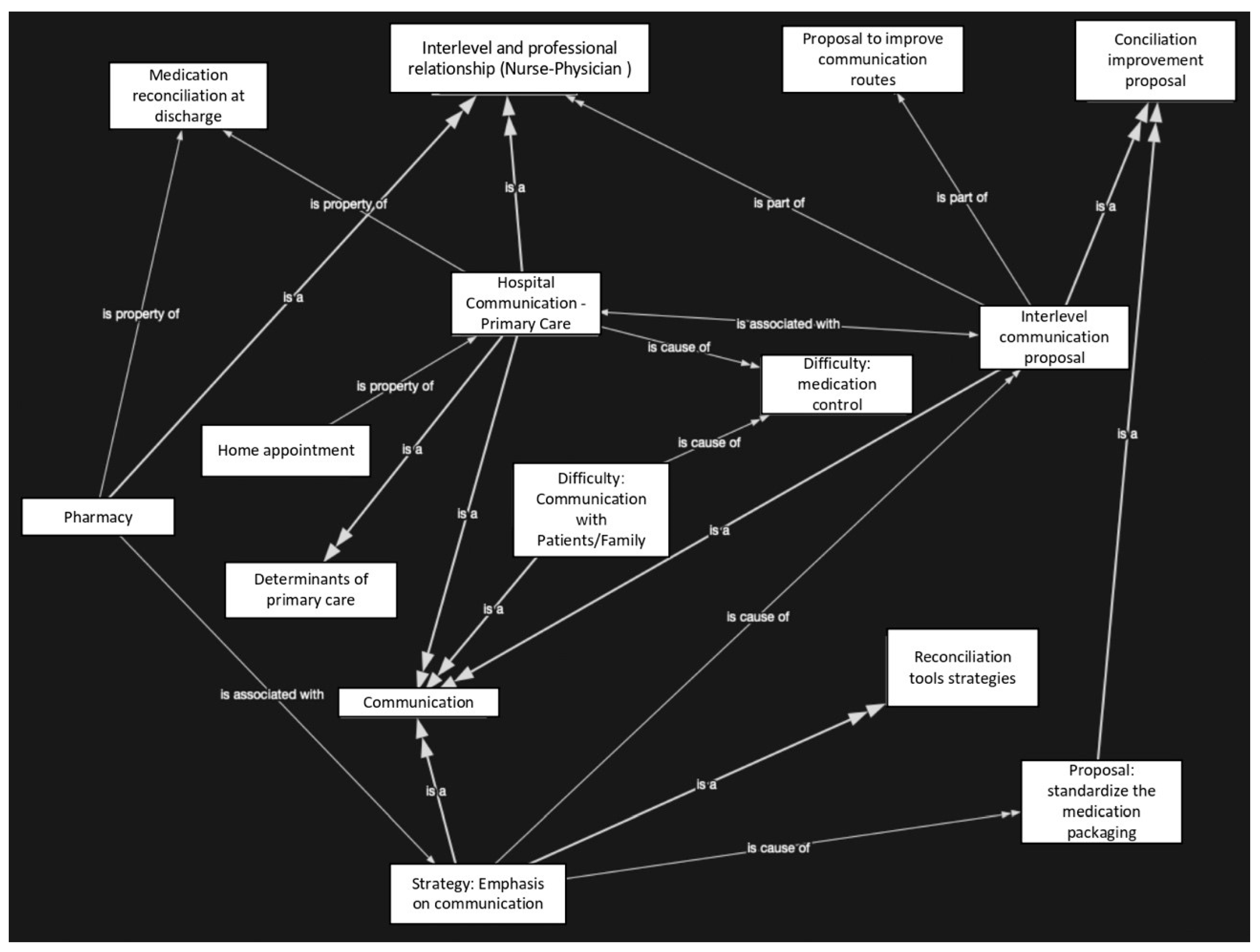
3. Results
3.1. Participants’ Characteristics
3.2. Descriptive Analysis
3.2.1. Barriers to, and Facilitators of, Communication in Interlevel Care
Barriers
“That is the great evil of our health system. There is no such fluidity that should exist between the specialist and primary care. It didn’t exist 30 years ago, or 10 years ago, or today. And I doubt very much that unless things change, it will ever be. You call the number you have thousands of times and there is no way to talk to the specialist”N.12
“The first thing is to improve interlevel communication, especially between primary and specialized, to be more fluid, that there is not that great barrier of communication that we have had; it is true that it is currently somewhat more fluid, although that problems still exist. If it were achieved, that would allow the patients we are both treating at the same time, he from his specialty and I from a more integral medicine, to be much better treated and above all the issue of drug conciliation would be controlled”P.8
“Sometimes we miss greater collaboration from specialists, we see how most of the time, after a consultation with the specialist, the patient receives the discharge report without an explanation to the patient about taking the medication, the dosage, schedules, the possible interactions with other medications, etc. All that is in our hands, the patient comes to his physician with the report so that it is he who interprets it and makes it clear”P.6
“[…] greater connection between hospital and primary care, especially in communication between professionals”N.11
“[…] the pharmacist, if he detects something, the tool for precautionary cancellations is used, but you have to keep in mind that you see that in the mailbox, and if you have 40 patients and you have to read the mailbox while running about in your job, it may escape you, so communication between the pharmacist and the physician should be improved; it is true that there are easier centres for this than others, since some have 13 or 14 physicians and the pharmacist cannot be in contact with everyone, but there should be some mechanism that would allow us to contact the pharmacist more quickly if they detect something that we have not detected”P.7
“I also have a lot of contact with pharmacists to put a kind of signal to the mailbox, to try to link them with something, for example, at the time of the shots, because we put a cup at breakfast, at noon and at dinner, etc.”N.7
“The fundamental problem I observe is that the physicians at the hospital change the treatment, but they do not modify the previous treatment, so the patient comes home with double prescribed treatment and that has to be realized by the primary care physician when he is going to renew the prescription or something like that”N.11
“I emphasize that if they go to the specialist and come back with two or three new drugs that are added to those they already took, it is very difficult for the patient to believe that the physician tells him not to take this or that and listens to him, to trust the primary care physician. They come from the hospital, from the specialist and that the word is law”P.5
“The truth is that if the patient notifies us, then we find out, and if not, to this day I cannot know, with the volume of patients I have, if this patient has been discharged or not. Either the patient contacts us because he needs a cure, or check something, or an analysis or whatever, or I don’t know about his discharge”N.11
“No, neither in those with heart failure, there is no such communication, it is more with diabetics and hypertensives. COPD is when they come to the centre for some other reason or they have a crisis, then we do that work in the emergency room and explain to them, since they do not come to the consultation unless they have a specific problem. Nor does the physician refer me to a COPD patient, it is very rare”N.2
“It would be interesting if, above all, in the most fragile patients there was a more direct communication, from physician to physician, but it is true that within the health system we have, it does not seem insufficient that we learn that they have been discharged”P.1
Facilitators
“Normally the case management nurse at the hospital alerts the case management nurse at my health centre. Then, she is the one who has to call that person in case she needs some kind of assistance from nursing, in that case she already communicates it to us”N.10
“We have a case management nurse, who does exactly that, she is a liaison between the hospital and the primary healthcare centre”P.3
“There are cases where the liaison nurse tells us that this person has just been discharged. Apart from that, we have the Professional Mailbox that when opening the DIRAYA we see people who have entered our quota and who have been discharged from the hospital. So in certain cases of patients who are followed up at home, in those cases we contact them and we see it directly, other times they are referred to us by the liaison nurse who is the one who receives the information directly”N.4
“We have a mailbox where every day we find the discharges, There, I see every day who is discharged, who enters, who goes through emergencies”P.3
“We have the Professional Mailbox where we receive notifications of admissions and discharges that occur with respect to our patients. When we open the computer in the morning, a list appears with the patients who have been admitted, or have gone to the emergency room or have been discharged. In these cases I try to go into the history of that patient and see what has happened to him and the medication”P.2
“We know that in the hospital there is an email for the communication of information about complex chronic patients, and about some help, or some information about these patients you can write it there and after a few days the specialist answers you, but this only works with internal medicine, the ideal would be to do it with the rest of the specialties, there are other patients who are not so chronic or so complex, but also sometimes you have doubts about how to manage them and if you go to the ordinary route of making an appointment, etc., there is a lot of delay in the diagnosis”P.4
3.2.2. Barriers to, and Facilitators of, Communication among Primary Healthcare Professionals
Barriers
“I don’t have a standardized system as such. When I make the home visit to perform a cure or something, I usually take the patient’s medication sheet printed in case they have any doubts and they can be resolved”N.11
“I have my own nurse and we form a team. We would have liked to have had a little more communication, we would have liked to have a few days a week to talk and have feedback on patients. Talk not only about treatments, but also about the evolution of wounds. Unfortunately it has not been possible and with the arrival of COVID well, less, so now when my nurse sees anything, he goes through the consultation or I tell him to stop by at the last minute and we talk more calmly, or we look for a little time”P.1
Facilitators
“From here, we get going, we call him by phone, we look at the history and in the report since we have access to the clinical station of the hospital and we see what has been the evolution and the problems that have been. We ask him if he needs our help for anything, since the medication, being new, needs clarification. We do a review, especially with older patients, by telephone”N.3
“When we formed, the team the physician who was with me previously, we had good communication, for example, if he detected a patient with altered blood glucose and diagnosed him as diabetic and gave him treatment, he immediately called me and told me that the patient had been scheduled for the next day. Just as when a diabetic patient already on time, and it goes wrong, went from oral treatment to insulin, he called me and passed it on me so that I could explain”N.2
“I get along quite well with my functional unit, the nurse I work with explains perfectly to patients how they have to take medication, clears all doubts with them, without the need for them to go through me. On the other hand our relationship is very fluid, we are talking continuously, we transfer any doubts; sometimes the patient tells one thing to the nurse and another to me differently, he wants to tell the same thing, but he doesn’t, and we have to be coordinated to know what to do with him”P.7
3.2.3. Barriers to, and Facilitators of, Communication between Primary Healthcare Professionals and Patients/Caregivers
Barriers
“[…] here there are 22,000 inhabitants and there is no communication like that in the Redondela, for example, which belongs to Isla Cristina and is a small town, and there is a pharmacy and people know each other better, but in Isla Cristina, which is a rural environment, the quotas of physicians are for 1700 or so, and then it can be put at the level of an urban environment”P.8
“[…] They tell the physician that they have understood and then they come to you, and it happens that sometimes we have had many changes of physician, few stable staff; the stable staff were the nurses and they came to us to ask us, since they were in a hurry to go to the physician they did not know, they had more confidence with you and asked you their doubts. Then, you realized that they did not understand the things that were being explained to them”N.8
“[…] I believe that information to patients or relatives should also be improved in some cases, so that when this patient reaches us, it allows us to achieve a better MR. If you come with solid information, what I explain to you will be faster and more efficient”P.5
“In other cases, it is the caregiver or the family member who brings the pills, puts them in front of him, and the patient does not know what is being taken, and when you ask him they do not know what is being taken of each thing”P.2
“We have a native population of the town that has a slightly lower cultural level, so you have to use a simpler vocabulary with them, which is more effective”N.3
“Sometimes it’s a question that they do not understand our explanations well, I try to write them down in a very detailed way, systematically, but sometimes they do not understand well”P.2
Facilitator
“[…] for being a dormitory city, so to speak, for its proximity to Huelva and for being a residential area of villas and residential areas, we have a younger population and with a higher cultural level, so communication with them has other characteristics”N.3
“When it comes with the report, if they have not reconciled the medication there, when it comes with the report, we already take the opportunity to do the review and the MR, at the same address or in the consultation”P.4
4. Discussion
Limitations
5. Conclusions
- Develop a common standardized system for medication reconciliation
- Protocolization of clinical sessions
- Include case management nurses in the medication reconciliation process
- Use up-to-date technologies to save time of the physician, nurse, pharmacist involved in the discharge of patients
- Build collaboration with pharmacists
- Write instructions for patients and caregivers
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Medication Without Harm. WHO Global Patient Safety Challenge; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Alanazi, F.K.; Sim, J.; Lapkin, S. Systematic review: Nurses’ safety attitudes and their impact on patient outcomes in acute-care hospitals. Nurs. Open 2022, 9, 30–43. [Google Scholar] [CrossRef]
- Stark, H.E.; Graudins, L.V.; McGuire, T.M.; Lee, C.Y.Y.; Duguid, M.J. Implementing a sustainable medication reconciliation process in Australian hospitals: The World Health Organization High 5s project. Res. Soc. Adm. Pharm. 2020, 16, 290–298. [Google Scholar] [CrossRef]
- Jakovljevic, M.; Jakab, M.; Gerdtham, U.; McDaid, D.; Ogura, S.; Varavikova, E.; Merrick, J.; Adany, R.; Okunade, A.; Getzen, T.E. Comparative financing analysis and political economy of noncommunicable diseases. J. Med. Econ. 2019, 22, 722–727. [Google Scholar] [CrossRef] [PubMed]
- Jakovljevic, M.; Yamada, T.; Grujic, D. Editorial: Role of health economic data in policy making and reimbursement of new medical technologies, Volume II. Front. Public Health 2023, 11, 1179300. [Google Scholar] [CrossRef]
- Masnoon, N.; Shakib, S.; Kalisch-Ellett, L.; Caughey, G.E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017, 17, 230. [Google Scholar] [CrossRef] [PubMed]
- Mejía, G.; Saiz-Rodríguez, M.; Gómez de Olea, B.; Ochoa, D.; Abad-Santos, F. Urgent Hospital Admissions Caused by Adverse Drug Reactions and Medication Errors—A Population-Based Study in Spain. Front. Pharmacol. 2020, 11, 734. [Google Scholar] [CrossRef] [PubMed]
- Al Rihani, S.B.; Deodhar, M.; Darakjian, L.I.; Dow, P.; Smith, M.K.; Bikmetov, R.; Turgeon, J.; Michaud, V. Quantifying Anticholinergic Burden and Sedative Load in Older Adults with Polypharmacy: A Systematic Review of Risk Scales and Models. Drugs Aging 2021, 38, 977–994. [Google Scholar] [CrossRef]
- Asadi, H.; Habibi Soola, A.; Iranpour, S. Evaluation of the Relationship Between Frailty and Polypharmacy in the Elderly Referred to the Emergency Departments of Ardabil 2019. Salmand Iran. J. Ageing 2022, 16, 550–563. [Google Scholar] [CrossRef]
- Stolldorf, D.P.; Ridner, S.H.; Vogus, T.J.; Roumie, C.L.; Schnipper, J.L.; Dietrich, M.S.; Schlundt, D.G.; Kripalani, S. Implementation strategies in the context of medication reconciliation: A qualitative study. Implement. Sci. Commun. 2021, 2, 63. [Google Scholar] [CrossRef]
- Tobiano, G.; Chaboyer, W.; Teasdale, T.; Raleigh, R.; Manias, E. Patient engagement in admission and discharge medication communication: A systematic mixed studies review. Int. J. Nurs. Stud. 2019, 95, 87–102. [Google Scholar] [CrossRef]
- Alqenae, F.A.; Steinke, D.; Keers, R.N. Prevalence and Nature of Medication Errors and Medication-Related Harm Following Discharge from Hospital to Community Settings: A Systematic Review. Drug Saf. 2020, 43, 517–537. [Google Scholar] [CrossRef] [PubMed]
- Latimer, S.; Hewitt, J.; de Wet, C.; Teasdale, T.; Gillespie, B.M. Medication reconciliation at hospital discharge: A qualitative exploration of acute care nurses’ perceptions of their roles and responsibilities. J. Clin. Nurs. 2023, 32, 1276–1285. [Google Scholar] [CrossRef] [PubMed]
- Latimer, S.; Hewitt, J.; Teasdale, T.; de Wet, C.; Gillespie, B.M. The accuracy, completeness and timeliness of discharge medication information and implementing medication reconciliation: A cross-sectional survey of general practitioners. Aust. J. Gen. Pract. 2020, 49, 854–858. [Google Scholar] [CrossRef] [PubMed]
- van der Nat, D.J.; Huiskes, V.J.B.; Taks, M.; van den Bemt, B.J.F.; van Onzenoort, H.A.W. Barriers and facilitators for the usage of a personal health record for medication reconciliation: A qualitative study among patients. Br. J. Clin. Pharmacol. 2022, 88, 4751–4762. [Google Scholar] [CrossRef] [PubMed]
- Dias Fernandes, B.; Fernandes Almeida, P.H.R.; Foppa, A.A.; Tavares Sousa, C.; Rocha Ayres, L.; Chemello, C. Pharmacist-led medication reconciliation at patient discharge: A scoping review. Res. Soc. Adm. Pharm. 2020, 16, 605–613. [Google Scholar] [CrossRef] [PubMed]
- Hannum, S.M.; Abebe, E.; Xiao, Y.; Brown, R.; Peña, I.M.; Gurses, A.P. Engineering care transitions: Clinician perceptions of barriers to safe medication management during transitions of patient care. Appl. Ergon. 2021, 91, 103299. [Google Scholar] [CrossRef]
- Al Anazi, A. Medication reconciliation process: Assessing value, adoption, and the potential of information technology from pharmacists’ perspective. Health Inform. J. 2021, 27, 1460458220987276. [Google Scholar] [CrossRef] [PubMed]
- Institute of Health Improvement. How-to Guide: Prevent Adverse Drug Events (Medication Reconciliation); Institute for Healthcare Improvement: Cambridge, MA, USA, 2008. [Google Scholar]
- Considine, J.; Berry, D.; Sprogis, S.K.; Newnham, E.; Fox, K.; Darzins, P.; Rawson, H.; Street, M. Understanding the patient experience of early unplanned hospital readmission following acute care discharge: A qualitative descriptive study. BMJ Open 2020, 10, e034728. [Google Scholar] [CrossRef]
- Gionfriddo, M.R.; Duboski, V.; Middernacht, A.; Kern, M.S.; Graham, J.; Wright, E.A. A mixed methods evaluation of medication reconciliation in the primary care setting. PLoS ONE 2021, 16, e0260882. [Google Scholar] [CrossRef]
- Sun, W.; Tahsin, F.; Barakat-Haddad, C.; Turner, J.P.; Haughian, C.R.; Abbass-Dick, J. Exploration of home care nurse’s experiences in deprescribing of medications: A qualitative descriptive study. BMJ Open 2019, 9, e025606. [Google Scholar] [CrossRef]
- Ozavci, G.; Bucknall, T.; Woodward-Kron, R.; Hughes, C.; Jorm, C.; Joseph, K.; Manias, E. A systematic review of older patients’ experiences and perceptions of communication about managing medication across transitions of care. Res. Soc. Adm. Pharm. 2021, 17, 273–291. [Google Scholar] [CrossRef]
- Gionfriddo, M.R.; Hu, Y.; Maddineni, B.; Kern, M.; Hayduk, V.; Kaledas, W.R.; Elder, N.; Border, J.; Frusciante, K.; Kobylinski, M.; et al. Evaluation of a Web-Based Medication Reconciliation Application Within a Primary Care Setting: Cluster-Randomized Controlled Trial. JMIR Form. Res. 2022, 6, e33488. [Google Scholar] [CrossRef] [PubMed]
- Leal-David, M.H.; Martínez-Riera, J.R.; Herraiz-Mallebrera, A.; Lima da Costa, M.F. Case management nurse in Spain: Facing the challenge of chronicity through a comprehensive practice. Cien. Saude. Colet. 2020, 25, 315–324. [Google Scholar] [CrossRef]
- Rangachari, P.; Dellsperger, K.C.; Fallaw, D.; Davis, I.; Sumner, M.; Ray, W.; Fiedler, S.; Nguyen, T.; Rethemeyer, R.K. A Mixed-Method Study of Practitioners’ Perspectives on Issues Related to EHR Medication Reconciliation at a Health System. Qual. Manag. Health Care 2019, 28, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Ocaña, M.J.; García-Navarro, E.B.; García-Navarro, S.; Macías-Colorado, M.E.; Baz-Montero, S.M.; Araujo-Hernández, M. Influence of the COVID-19 Pandemic on Medication Reconciliation in Frail Elderly People at Hospital Discharge: Perception of Healthcare Professionals. Int. J. Environ. Res. Public Health 2022, 19, 10348. [Google Scholar] [CrossRef]
- Macías-Colorado, M.E.; Rodríguez-Pérez, M.; Rojas-Ocaña, M.J.; Teresa-Morales, C. Communication on Safe Caregiving between Community Nurse Case Managers and Family Caregivers. Healthcare 2021, 9, 205. [Google Scholar] [CrossRef]
- Syyrilä, T.; Vehviläinen-Julkunen, K.; Härkänen, M. Healthcare professionals’ perceptions on medication communication challenges and solutions–text mining and manual content analysis-cross-sectional study. BMC Health Serv. Res. 2021, 21, 1226. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Andalusian Regional Governement, Law 2/1998, 15 of June, of Health in Andalusia. 1998. Available online: https://www.boe.es/eli/es-an/l/1998/06/15/2/con (accessed on 15 March 2023).
- Andalusian Health System. Typology of Health Centers in the Analytical Accounting System; SE-1871-2012; Andalusian Regional Governement: Sevilla, Spain, 2012.
- Naderifar, M.; Goli, H.; Ghaljaie, F. Snowball Sampling: A Purposeful Method of Sampling in Qualitative Research. Strides Dev. Med. Educ. 2017, 14, e67670. [Google Scholar] [CrossRef]
- Sandelowski, M. Sample size in qualitative research. Res. Nurs. Health 1995, 18, 179–183. [Google Scholar] [CrossRef]
- Graneheim, U.H.; Lundman, B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ. Today 2004, 24, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Lincoln, Y.; Guba, E. Naturaliztic Inquiry; SAGE Publications: London, UK, 1985. [Google Scholar]
- Manias, E.; Cranswick, N.; Newall, F.; Rosenfeld, E.; Weiner, C.; Williams, A.; Wong, I.C.; Borrott, N.; Lai, J.; Kinney, S. Medication error trends and effects of person-related, environment-related and communication-related factors on medication errors in a paediatric hospital. J. Paediatr. Child Health 2019, 55, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Mendizabal Olaizola, A.; Valverde, E.; Goienetxea, E.; Oñatibia, A.; Ezcurra, M. Reconciliation of medication in coordination between primary care professionals and the community pharmacy. Int. J. Integr. Care 2019, 19, A44. [Google Scholar] [CrossRef]
- Wheeler, A.J.; Scahill, S.; Hopcroft, D.; Stapleton, H. Reducing medication errors at transitions of care is everyone’s business. Aust. Prescr. 2018, 41, 73–77. [Google Scholar] [CrossRef]
- Bucknall, T.; Fossum, M.; Hutchinson, A.M.; Botti, M.; Considine, J.; Dunning, T.; Hughes, L.; Weir-Phyland, J.; Digby, R.; Manias, E. Nurses’ decision-making, practices and perceptions of patient involvement in medication administration in an acute hospital setting. J. Adv. Nurs. 2019, 75, 1316–1327. [Google Scholar] [CrossRef]
- Pinelli, V.; Stuckey, H.L.; Gonzalo, J.D. Exploring challenges in the patient’s discharge process from the internal medicine service: A qualitative study of patients’ and providers’ perceptions. J. Interprofessional Care 2017, 31, 566–574. [Google Scholar] [CrossRef] [PubMed]
- Waldron, C.; Cahill, J.; Cromie, S.; Delaney, T.; Kennelly, S.P.; Pevnick, J.M.; Grimes, T. Personal Electronic Records of Medications (PERMs) for medication reconciliation at care transitions: A rapid realist review. BMC Med. Inform. Decis. Mak. 2021, 21, 307. [Google Scholar] [CrossRef] [PubMed]
- Errasti-Ibarrondo, B.; Choperena, A.; Wilson, D.M. Reading and reflecting on experiential accounts of hospital patients to foster a person-centered care approach: A novel educational method. Teach. Learn. Nurs. 2022, 18, 166–175. [Google Scholar] [CrossRef]
- Daliri, S.; Bekker, C.L.; Buurman, B.M.; Scholte op Reimer, W.J.M.; van den Bemt, B.J.F.; Karapinar-Çarkit, F. Barriers and facilitators with medication use during the transition from hospital to home: A qualitative study among patients. BMC Health Serv. Res. 2019, 19, 204. [Google Scholar] [CrossRef]
- Penm, J.; Vaillancourt, R.; Pouliot, A. Defining and identifying concepts of medication reconciliation: An international pharmacy perspective. Res. Soc. Adm. Pharm. 2019, 15, 632–640. [Google Scholar] [CrossRef]
- Fournier, R.; Kachachi, S.; Mouchoux, C.; Gervais, F. From medication reconciliation to shared medication review: Pilot study integrating support for community pharmacists within a pharmaceutical care pathway. Ann. Pharm. Fr. 2022, 80, 950–960. [Google Scholar] [CrossRef] [PubMed]
- Marinovic, I.; Bacic Vrca, V.; Samardzic, I.; Marusic, S.; Grgurevic, I.; Papic, I.; Grgurevic, D.; Brkic, M.; Jambrek, N.; Mesaric, J. Impact of an integrated medication reconciliation model led by a hospital clinical pharmacist on the reduction of post-discharge unintentional discrepancies. J. Clin. Pharm. Ther. 2021, 46, 1326–1333. [Google Scholar] [CrossRef] [PubMed]
- Cerda, A.A.; García, L.Y.; Rivera-Arroyo, J.; Riquelme, A.; Teixeira, J.P.; Jakovljevic, M. Comparison of the healthcare system of Chile and Brazil: Strengths, inefficiencies, and expenditures. Cost Eff. Resour. Alloc. 2022, 20, 71. [Google Scholar] [CrossRef]
- Welk, B.; Killin, L.; Reid, J.N.; Anderson, K.K.; Shariff, S.Z.; Appleton, A.; Kearns, G.; Garg, A.X. Effect of electronic medication reconciliation at the time of hospital discharge on inappropriate medication use in the community: An interrupted time-series analysis. CMAJ Open 2021, 9, E1105–E1113. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, S.; Laurens, V.; Weigel, G.; Hirschman, K.; Scott, A.; Nguyen, H. Care transitions from patient and caregiver perspectives. Ann. Fam. Med. 2018, 16, 225–231. [Google Scholar] [CrossRef]
- Astier-Peña, M.P.; Torijano-Casalengua, M.L.; Olivera-Cañadas, G. Setting priorities for patient safety in Primary Care. Aten. Primaria. 2016, 48, 3–7. [Google Scholar] [CrossRef]
- Kattel, S.; Manning, D.M.; Erwin, P.J.; Wood, H.; Kashiwagi, D.T.; Murad, M.H. Information Transfer at Hospital Discharge: A Systematic Review. J. Patient Saf. 2020, 16, e25–e33. [Google Scholar] [CrossRef] [PubMed]
- Allen, J.; Hutchinson, A.M.; Brown, R.; Livingston, P.M. User experience and care for older people transitioning from hospital to home: Patients’ and carers’ perspectives. Health Expect. 2018, 21, 518–527. [Google Scholar] [CrossRef]
- Miguélez-Chamorro, A.; Casado-Mora, M.I.; Company-Sancho, M.C.; Balboa-Blanco, E.; Font-Oliver, M.A.; Román-Medina Isabel, I. Advanced practice in case management: An essential element in the new complex chronicity care model. Enfermería Clínica 2019, 29, 99–106. [Google Scholar] [CrossRef]
- Duarte-Climents, G.; Sánchez-Gómez, M.B.; Rodríguez-Gómez, J.; Rodríguez-Álvarez, C.; Sierra-López, A.; Aguirre-Jaime, A.; Gómez-Salgado, J. Impact of the Case Management Model through Community Liaison Nurses. Int. J. Environ. Res. Public Health 2019, 16, 1894. [Google Scholar] [CrossRef]
- Bosque, D.; Forbes, S.; Ward, E.N.; Delaney, J.; Meyers, G.T. Reconciliation and Disposal of Oral Medication: Creating a Safe Process for Clinical Research Personnel. Clin. J. Oncol. Nurs. 2021, 25, 587–590. [Google Scholar] [CrossRef] [PubMed]
- Lane-Fall, M.B.; Pascual, J.L.; Peifer, H.G.; Di Taranti, L.J.; Collard, M.L.; Jablonski, J.; Gutsche, J.T.; Halpern, S.D.; Barg, F.K.; Fleisher, L.A. A Partially Structured Postoperative Handoff Protocol Improves Communication in 2 Mixed Surgical Intensive Care Units: Findings From the Handoffs and Transitions in Critical Care (HATRICC) Prospective Cohort Study. Ann. Surg. 2020, 271, 484–493. [Google Scholar] [CrossRef]
- Aires-Moreno, G.T.; Silvestre, C.C.; Araujo, D.; Matos, V.T.G.; Marcon de Oliveira, V.; Ferreira, C.M.; Vasconcelos-Pereira, E.F.; Lira, A.R.P.; Chemello, C.; Oliveira, L.M.S.; et al. Perceptions of nurses, pharmacists and physicians about medication reconciliation: A multicenter study. Saudi. Pharm. J. 2020, 28, 1435–1439. [Google Scholar] [CrossRef]
- Kim, J.M.; Suarez-Cuervo, C.; Berger, Z.; Lee, J.; Gayleard, J.; Rosenberg, C.; Nagy, N.; Weeks, K.; Dy, S. Evaluation of Patient and Family Engagement Strategies to Improve Medication Safety. Patient 2018, 11, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Moral-Fernández, L.; Frías-Osuna, A.; Moreno-Cámara, S.; Palomino-Moral, P.A.; del-Pino-Casado, R. The first moments of the carer: The process of becoming a caregiver of a dependent elderly relative. Atención Primaria 2018, 50, 282–290. [Google Scholar] [CrossRef] [PubMed]
| B/F | Category | Operational Definition | |
|---|---|---|---|
| B | Non-existence or ineffectiveness of communication channels | Refers to the existence and functionality that healthcare professionals find when communicating | |
| Cross-level collaboration | Lack of collaboration on the part of specialists in the hospital field in medication reconciliation | ||
| Lack of relationship with pharmacist | Lack of relationship with pharmacists and valuation of their work in communication. Element that they contemplate as necessary (that they refer to as non-existent or absent) but also referred to as facilitator | ||
| Non-comprehensive care | Unique care within an area of specialization without attending to other pathologies or previous treatments, generating problems in medication reconciliation | ||
| Use of the patient/informal caregivers as a link between levels | Give the patient responsibility for bringing the information relating to discharge to the healthcare professionals of other levels of care | ||
| Chronic multi-pathological patients | Difficulty typical of patients who have multiple pathologies, and the interaction of many and diverse professionals | ||
| F | Figure of the case management nurse | Case management nurse who serves as liaison between levels. Work of the nurse as mediator between both care spaces | |
| Technological tools | Professional mailbox | Information through these computer communication resources that informs of, and gives access to, patients and their processes | |
| Diraya | Communication tool to know the care processes between levels | ||
| Telemedicine | Telematic and internal communication at various levels of specialization for specific consultations of multidisciplinary patients | ||
| B/F | Categories | Operational Definition |
|---|---|---|
| B | Non-existence/ignorance or lack of use of a common standardized system for medication reconciliation | Non-existence/ignorance or lack of use of common standardized systems for medication reconciliation. Each healthcare professional acts differently. |
| Lack of time for communication between healthcare professionals | Lack of time for communication between nurse and physician, and to manage cases of highly complex patients in medication reconciliation. | |
| F | Protocols | Knowledge and use of action protocols, where the interventions and the form of action between healthcare professionals involved in medication reconciliation are unified. |
| Close relationship/Teamwork | Close relationship between the two healthcare professionals involved in medication reconciliation. Fluid communication and strategies aimed at responding to the same problem. |
| B/F | Categories | Operational Definition |
|---|---|---|
| B | Geographical distribution of the health centre (urban or rural) | The number of patients to be treated, according to the characteristics of the geographical space in which they are treated. |
| Unstable job conditions of the staff | Lack of contact, knowledge and fluid and effective communication caused by staff turnover. They do not know the patients and their circumstances. | |
| Patient is unaware of the need for medication reconciliation. | The patient in hospital care is not made to participate in the need for medication reconciliation at discharge. | |
| Informal caregiver characteristics: knowledge, skill and attitudes | Lack of knowledge and skills of caregivers in the communication process. It hinders communication and transfer of information from the healthcare professional to these mediators. | |
| Low sociocultural level | Difficulty observed in communication for medication reconciliation with people of low sociocultural level. | |
| F | Medium/high sociocultural level | The medium/high sociocultural level facilitates and improves the effectiveness of communication for medication reconciliation. |
| Proximity of the primary healthcare centre to the home space | Knowledge acquired by the healthcare professional of the patient and family environment, and knowledge of their communication channels and intra-family relationship. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rojas-Ocaña, M.J.; Teresa-Morales, C.; Ramos-Pichardo, J.D.; Araujo-Hernández, M. Barriers and Facilitators of Communication in the Medication Reconciliation Process during Hospital Discharge: Primary Healthcare Professionals’ Perspectives. Healthcare 2023, 11, 1495. https://doi.org/10.3390/healthcare11101495
Rojas-Ocaña MJ, Teresa-Morales C, Ramos-Pichardo JD, Araujo-Hernández M. Barriers and Facilitators of Communication in the Medication Reconciliation Process during Hospital Discharge: Primary Healthcare Professionals’ Perspectives. Healthcare. 2023; 11(10):1495. https://doi.org/10.3390/healthcare11101495
Chicago/Turabian StyleRojas-Ocaña, María Jesús, Cristina Teresa-Morales, Juan Diego Ramos-Pichardo, and Miriam Araujo-Hernández. 2023. "Barriers and Facilitators of Communication in the Medication Reconciliation Process during Hospital Discharge: Primary Healthcare Professionals’ Perspectives" Healthcare 11, no. 10: 1495. https://doi.org/10.3390/healthcare11101495
APA StyleRojas-Ocaña, M. J., Teresa-Morales, C., Ramos-Pichardo, J. D., & Araujo-Hernández, M. (2023). Barriers and Facilitators of Communication in the Medication Reconciliation Process during Hospital Discharge: Primary Healthcare Professionals’ Perspectives. Healthcare, 11(10), 1495. https://doi.org/10.3390/healthcare11101495






