Consequences of Shift Work and Night Work: A Literature Review
Abstract
1. Introduction
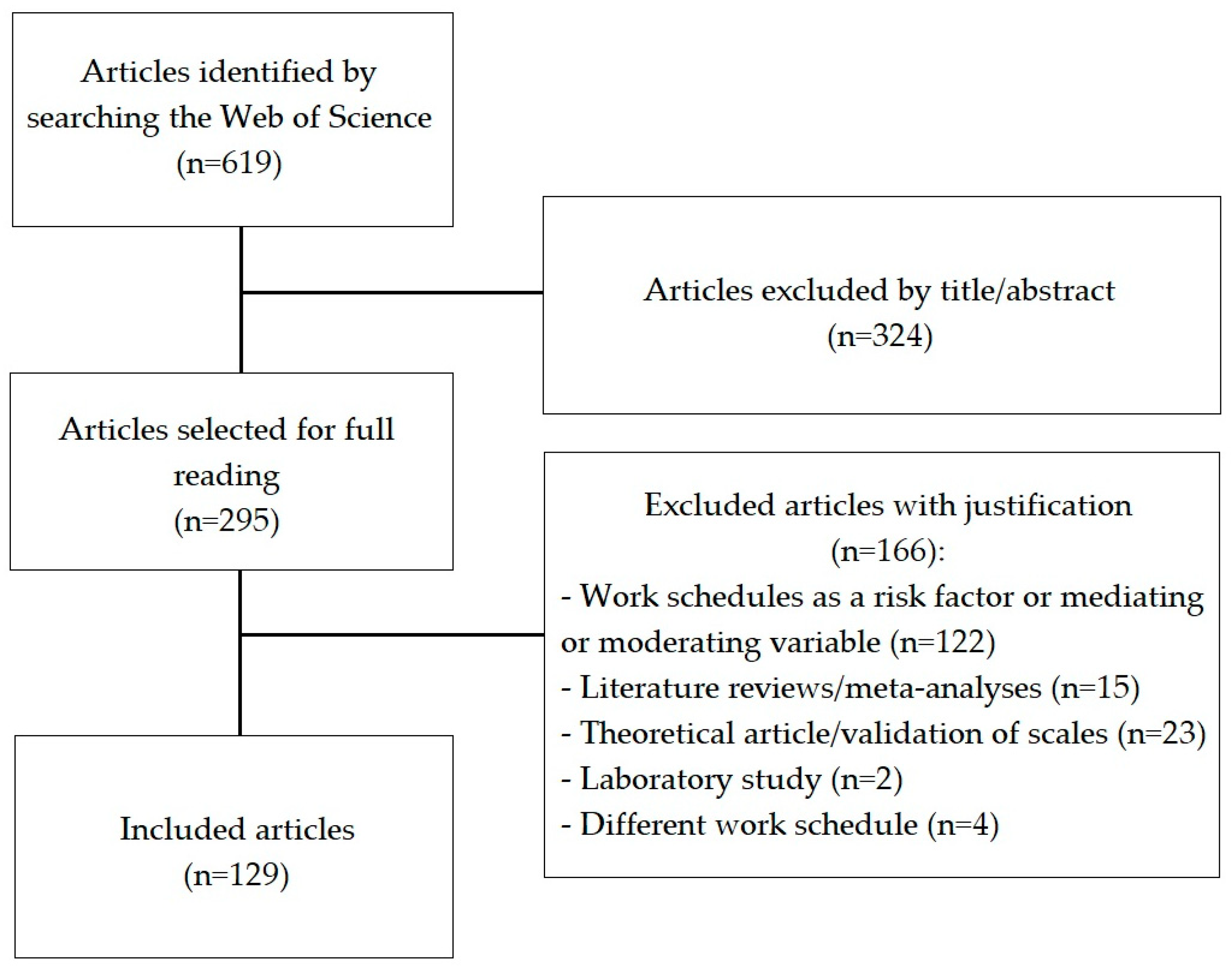
2. Materials and Methods
- Journal articles;
- Studies in Portuguese or English;
- Empirical studies;
- Studies where rotating shift work or a fixed night shift was the main objective.
- Studies not related to shift and night work schedules (first phase of elimination by reading the title and abstract);
- Studies that did not evaluate the effects of shift and night work schedules (different work schedules, for example, rotating without nights);
- Studies in which shift work or night work appeared as a secondary objective (risk factor or mediating variable);
- Theoretical articles (literature reviews, non-empirical articles, or validation of scales);
- Meta-analyses;
- Laboratory studies (in this case, the participants were not shift workers and the work schedule was simulated).
2.1. Analysis and Selection of Studies
2.2. Analysis and Categorization of Variables
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boulin, J. The social organization of time. Futures 1993, 25, 511–520. [Google Scholar] [CrossRef]
- Thierry, H.; Jansen, B. Work time and behaviour at work. In A Handbook of Work and Organizational Psychology, 2nd ed.; Drenth, P.J.D., Thierry, H., de Wolff, C.J., Eds.; Volume 2: Work Psychology; Psychology Press: East Sussex, UK, 1998; pp. 89–119. ISBN 9780863775239. [Google Scholar]
- Costa, G. Shift work and occupational medicine: An overview. Occup. Med. 2003, 53, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Presser, H.B. Toward a 24-hour economy. Science 1999, 11, 1778–1779. [Google Scholar] [CrossRef]
- Costa, G. The problem: Shitwork. Chronobiol. Int. 1997, 14, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Eurofound. Sixth European Working Conditions Survey–Overview Report; Publications Office of the European Union: Luxembourg, 2016; ISBN 978-92-897-1549-2.
- NIOSH. Work Organization Characteristics (NHIS 2015) Charts. Available online: https://wwwn.cdc.gov/NIOSH-WHC/chart/ohs-workorg?OU=*&T=OU&V=R (accessed on 7 December 2022).
- Caruso, C.C. Negative impacts of shiftwork and long work hours. Rehabil. Nurs. 2014, 39, 16–25. [Google Scholar] [CrossRef]
- Åkerstedt, T. Shift work and disturbed sleep/wakefulness. Occup. Med. 2003, 53, 89–94. [Google Scholar] [CrossRef]
- Knutsson, A. Health disorders of shift workers. Occup. Med. 2003, 53, 103–108. [Google Scholar] [CrossRef]
- Bamonde, J.; Pinto, C.; Santos, P.; Couto, G. O Impacto do trabalho por turnos na saúde dos enfermeiros: Revisão integrativa [The impact of shift work on nurse´shealth: Integrative review]. Rev. De Investig. Inovação Em Saúde 2020, 3, 101–110. [Google Scholar] [CrossRef]
- Ahmadi, S.A.; Tranmer, J.E.; Ritonja, J.A.; Flaten, L.; Topouza, D.G.; Duan, Q.L.; Durocher, F.; Aronson, K.J.; Bhatti, P. DNA methylation of circadian genes and markers of cardiometabolic risk in female hospital workers: An exploratory study. Chronobiol. Int. 2022, 39, 735–746. [Google Scholar] [CrossRef]
- Vyas, M.V.; Garg, A.X.; Iansavichus, A.V.; Costella, J.; Donner, A.; Laugsand, L.E.; Janszky, I.; Mrkobrada, M.; Parraga, G.; Hackam, D.G. Shift work and vascular events: Systematic review and meta-analysis. BMJ 2012, 345, e4800. [Google Scholar] [CrossRef]
- Brown, J.P.; Martin, D.; Nagaria, Z.; Verceles, A.C.; Jobe, S.L.; Wickwire, E.M. Mental health consequences of shift work: An updated review. Curr. Psychiatry Rep. 2020, 22, 7. [Google Scholar] [CrossRef]
- Berge, L.A.; Liu, F.C.; Grimsrud, T.K.; Babigumira, R.; Støer, N.C.; Kjærheim, K.; Robsahm, T.E.; Ghiasvand, R.; Hosgood, H.D.; Samuelsen, S.O.; et al. Night shift work and risk of aggressive prostate cancer in the Norwegian Offshore Petroleum Workers (NOPW) cohort. Int. J. Epidemiol. 2022, dyac235. [Google Scholar] [CrossRef]
- Yuan, X.; Zhu, C.; Wang, M.; Mo, F.; Du, W.; Ma, X. Night shift work increases the risks of multiple primary cancers in women: A systematic review and meta-analysis of 61 articles. Cancer Epidemiol. Biomark. Prev. 2018, 27, 25–40. [Google Scholar] [CrossRef]
- Larson, J.M.; Bazalakova, M.H.; Godecker, A.; DelBeccaro, M.; Aagaard, K.M.; Antony, K.M. Shift work and sleep duration are associated with adverse pregnancy outcomes in a predominantly Latinx population with high rates of obesity. PLoS ONE 2022, 17, e0272218. [Google Scholar] [CrossRef]
- Wang, Y.; Gu, F.; Deng, M.; Guo, L.; Lu, C.; Zhou, C.; Chen, S.; Xu, Y. Rotating shift work and menstrual characteristics in a cohort of Chinese nurses. BMC Women’s Health 2016, 16, 24. [Google Scholar] [CrossRef]
- Handy, J.A. Maintaining family life under shiftwork schedules: A case study of a New Zealand petrochemical plant. N. Z. J. Psychol. 2010, 39, 29–37. [Google Scholar]
- Li, J.; Johnson, S.E.; Han, W.J.; Andrews, S.; Kendall, G.; Strazdins, L.; Dockery, A. Parents’ nonstandard work schedules and child well-being: A critical review of the literature. J. Prim. Prev. 2014, 35, 53–73. [Google Scholar] [CrossRef]
- Wöhrmann, A.M.; Müller, G.; Ewert, K. Shift work and work-family conflict: A systematic review. Sozialpolitik.ch 2020, 3, 3.2:1–3.2:26. [Google Scholar] [CrossRef]
- Zhao, Y.; Cooklin, A.R.; Richardson, A.; Strazdins, L.; Butterworth, P.; Leach, L.S. Parents’ shift work in connection with work–family conflict and mental health: Examining the pathways for mothers and fathers. J. Fam. Issues 2021, 42, 445–473. [Google Scholar] [CrossRef]
- Maume, D.J.; Sebastian, R.A. Gender, nonstandard work schedules, and marital quality. J. Fam. Econ. Issues 2012, 33, 477–490. [Google Scholar] [CrossRef]
- Folkard, S.; Tucker, P. Shift work, safety and productivity. Occup. Med. 2003, 53, 95–101. [Google Scholar] [CrossRef]
- Alali, H.; Braeckman, L.; Van Hecke, T.; De Clercq, B.; Janssens, H.; Wahab, M.A. Relationship between non-standard work arrangements and work-related accident absence in Belgium. J. Occup. Health 2017, 59, 177–186. [Google Scholar] [CrossRef]
- Härmä, M.; Koskinen, A.; Sallinen, M.; Kubo, T.; Ropponen, A.; Lombardi, D.A. Characteristics of working hours and the risk of occupational injuries among hospital employees: A case-crossover study. Scand. J. Work Environ. Health 2020, 46, 570–578. [Google Scholar] [CrossRef]
- Dall’Ora, C.; Ball, J.; Recio-Saucedo, A.; Griffiths, P. Characteristics of shift work and their impact on employee performance and wellbeing: A literature review. Int. J. Nurs. Stud. 2016, 57, 12–27. [Google Scholar] [CrossRef]
- Fekedulegn, D.; Burchfiel, C.M.; Hartley, T.A.; Andrew, M.E.; Charles, L.E.; Tinney-Zara, C.A.; Violanti, J.M. Shiftwork and sickness absence among police officers: The BCOPS study. Chronobiol. Int. 2013, 30, 930–941. [Google Scholar] [CrossRef]
- Jacobsen, D.I.; Fjeldbraaten, E.M. Shift work and sickness absence—The mediating roles of work–home conflict and perceived health. Hum. Resour. Manag. 2018, 57, 1145–1157. [Google Scholar] [CrossRef]
- Bastos, J.; Afonso, P. O impacto do trabalho por turnos no sono e saúde psíquica [The impact of shiftwork on sleep and mental health]. Rev. Port. Psiquiatr. Saúde Ment. 2020, 6, 24–30. [Google Scholar] [CrossRef]
- Fonseca, S.; Queirós, C.; Martins, V. Saúde ocupacional na ferrovia: Trabalho por turnos, burnout, sono e interação trabalho-família [Occupational health on the railway: Shift work, burnout, sleep and work-family interaction]. Psicol. Saúde Doenças 2020, 21, 221–228. [Google Scholar] [CrossRef]
- Wight, V.R.; Raley, S.B.; Bianchi, S.M. Time for children, one’s spouse and oneself among parents who work nonstandard hours. Soc. Forces 2008, 87, 243–271. [Google Scholar] [CrossRef]
- Amado, J. A técnica de análise de conteúdo [The content analysis technique]. Rev. Ref. 2000, 5, 53–63. [Google Scholar]
- Burch, J.B.; Alexander, M.; Balte, P.; Sofge, J.; Winstead, J.; Kothandaraman, V.; Ginsberg, J.P. Shift work and heart rate variability coherence: Pilot study among nurses. Appl. Psychophysiol. Biofeedback 2019, 44, 21–30. [Google Scholar] [CrossRef]
- Cerqueira Teixeira, K.R.; de Medeiros, L.A.; Mendes, J.A.; Vaz, E.R.; Cunha, T.M.; de Oliveira, E.P.; Penha-Silva, N.; Crispim, C.A. The erythrocyte membrane stability is associated with sleep time and social jetlag in shift workers. PLoS ONE 2019, 14, e0222698. [Google Scholar] [CrossRef]
- Chang, W.P.; Li, H.B. Differences in workday sleep fragmentation, rest-activity cycle, sleep quality, and activity level among nurses working different shifts. Chronobiol. Int. 2019, 36, 1761–1771. [Google Scholar] [CrossRef]
- Dai, C.; Qiu, H.; Huang, Q.; Hu, P.; Hong, X.; Tu, J.; Xie, Q.; Li, H.; Ren, W.; Ni, S.; et al. The effect of night shift on sleep quality and depressive symptoms among Chinese nurses. Neuropsychiatr. Dis. Treat. 2019, 15, 435–440. [Google Scholar] [CrossRef]
- Di Muzio, M.; Reda, F.; Diella, G.; Di Simone, E.; Novelli, L.; D’Atri, A.; Giannini, A.; De Gennaro, L. Not only a problem of fatigue and sleepiness: Changes in psychomotor performance in Italian nurses across 8-h rapidly rotating shifts. J. Clin. Med. 2019, 8, 47. [Google Scholar] [CrossRef]
- Ferguson, B.; Shoff, H.; Shreffler, J.; McGowan, J.; Huecker, M. Does my emergency department doctor sleep? The trouble with recovery from night shift. J. Emerg. Med. 2019, 57, 162–167. [Google Scholar] [CrossRef]
- Flaa, T.A.; Harris, A.; Bjorvatn, B.; Gundersen, H.; Zakariassen, E.; Pallesen, S.; Waage, S. Sleepiness among personnel in the Norwegian air ambulance service. Int. Arch. Occup. Environ. Health 2019, 92, 1121–1130. [Google Scholar] [CrossRef]
- Fowler, L.A.; Ellis, S. The effect of 12 hour shifts, time of day, and sleepiness on emotional empathy and burnout in medical students. Clocks Sleep 2019, 1, 501–509. [Google Scholar] [CrossRef]
- Ganesan, S.; Magee, M.; Stone, J.E.; Mulhall, M.D.; Collins, A.; Howard, M.E.; Lockley, S.W.; Rajaratnam, S.M.W.; Sletten, T.L. The impact of shift work on sleep, alertness and performance in healthcare workers. Sci. Rep. 2019, 9, 4635. [Google Scholar] [CrossRef]
- Haile, K.K.; Asnakew, S.; Waja, T.; Kerbih, H.B. Shift work sleep disorders and associated factors among nurses at federal government hospitals in Ethiopia: A cross-sectional study. BMJ Open 2019, 9, e029802. [Google Scholar] [CrossRef]
- Härmä, M.; Karhula, K.; Puttonen, S.; Ropponen, A.; Koskinen, A.; Ojajärvi, A.; Kivimäki, M. Shift work with and without night work as a risk factor for fatigue and changes in sleep length: A cohort study with linkage to records on daily working hours. J. Sleep Res. 2019, 28, e12658. [Google Scholar] [CrossRef] [PubMed]
- Hattammaru, M.; Tahara, Y.; Kikuchi, T.; Okajima, K.; Konishi, K.; Nakajima, S.; Sato, K.; Otsuka, K.; Sakura, H.; Shibata, S.; et al. The effect of night shift work on the expression of clock genes in beard hair follicle cells. Sleep Med. 2019, 56, 164–170. [Google Scholar] [CrossRef]
- Hulsegge, G.; Loef, B.; van Kerkhof, L.W.; Roenneberg, T.; van der Beek, A.J.; Proper, K.I. Shift work, sleep disturbances and social jetlag in healthcare workers. J. Sleep Res. 2019, 28, e12802. [Google Scholar] [CrossRef]
- Jeong, K.S.; Ahn, Y.S.; Jang, T.W.; Lim, G.; Kim, H.D.; Cho, S.W.; Sim, C.S. Sleep assessment during shift work in Korean firefighters: A cross-sectional study. Saf. Health Work 2019, 10, 254–259. [Google Scholar] [CrossRef]
- Mulhall, M.D.; Sletten, T.L.; Magee, M.; Stone, J.E.; Ganesan, S.; Collins, A.; Anderson, C.; Lockley, S.W.; Howard, M.E.; Rajaratnam, S.M. Sleepiness and driving events in shift workers: The impact of circadian and homeostatic factors. Sleep 2019, 42, zsz074:1–zsz074:13. [Google Scholar] [CrossRef]
- Pallesen, S.; Jacobsen, D.P.; Nielsen, M.B.; Gjerstad, J. The 5-HTTLPR rs25531 LALA-genotype increases the risk of insomnia symptoms among shift workers. Sleep Med. 2019, 60, 224–229. [Google Scholar] [CrossRef]
- Park, H.; Suh, B.; Lee, S.J. Shift work and depressive symptoms: The mediating effect of vitamin D and sleep quality. Chronobiol. Int. 2019, 36, 689–697. [Google Scholar] [CrossRef]
- Resuehr, D.; Wu, G.; Johnson Jr, R.L.; Young, M.E.; Hogenesch, J.B.; Gamble, K.L. Shift work disrupts circadian regulation of the transcriptome in hospital nurses. J. Biol. Rhythms 2019, 34, 167–177. [Google Scholar] [CrossRef]
- Schuster, M.; Oberlinner, C.; Claus, M. Shift-specific associations between age, chronotype and sleep duration. Chronobiol. Int. 2019, 36, 784–795. [Google Scholar] [CrossRef]
- Uekata, S.; Kato, C.; Nagaura, Y.; Eto, H.; Kondo, H. The impact of rotating work schedules, chronotype, and restless legs syndrome/Willis-Ekbom disease on sleep quality among female hospital nurses and midwives: A cross-sectional survey. Int. J. Nurs. Stud. 2019, 95, 103–112. [Google Scholar] [CrossRef]
- Wilson, M.; Permito, R.; English, A.; Albritton, S.; Coogle, C.; Van Dongen, H.P. Performance and sleepiness in nurses working 12-h day shifts or night shifts in a community hospital. Accid. Anal. Prev. 2019, 126, 43–46. [Google Scholar] [CrossRef]
- Bazazan, A.; Rasoulzadeh, Y.; Dianat, I.; Safaiyan, A.; Mombeini, Z. Occupational fatigue and mental health complaints among 8-hour shift workers of petrochemical industries in Iran. Work 2019, 62, 309–317. [Google Scholar] [CrossRef]
- Chang, Y.H.; Yang, H.H.; Hsu, W.J. Effects of work shifts on fatigue levels of air traffic controllers. J. Air Transp. Manag. 2019, 76, 1–9. [Google Scholar] [CrossRef]
- Yu, F.; Somerville, D.; King, A. Exploring the impact of 12-hour shifts on nurse fatigue in intensive care units. Appl. Nurs. Res. 2019, 50, 151191. [Google Scholar] [CrossRef]
- Arslan, M.; Garipoğlu, G.; Bilek, H. Investigation of nutritional status of security officers working in shifts and correlation with obesity. Prog. Nutr. 2019, 21, 276–284. [Google Scholar] [CrossRef]
- Fradkin, L.; Raz, O.; Boaz, M. Nurses who work rotating shifts consume more energy, macronutrients and calcium when they work the night shift versus day shift. Chronobiol. Int. 2019, 36, 288–295. [Google Scholar] [CrossRef]
- Fröhlich, C.; Garcez, A.; Canuto, R.; Paniz, V.M.V.; Pattussi, M.P.; Olinto, M.T.A. Abdominal obesity and dietary patterns in female shift workers. Cienc. Saude Colet. 2019, 24, 3283–3292. [Google Scholar] [CrossRef]
- Heath, G.; Dorrian, J.; Coates, A. Associations between shift type, sleep, mood, and diet in a group of shift working nurses. Scand. J. Work Environ. Health 2019, 45, 402–412. [Google Scholar] [CrossRef]
- Nogueira, V.C.; Arruda, S.P.M.; Sampaio, H.A.D.C.; Rodrigues, B.C.; Silva, E.B.D.; Farias, B.O.; Sabóia, K.M. Socioeconomic, demographic and lifestyle factors associated with eating patterns of shift workers. Cien. Saude Colet. 2019, 24, 761–769. [Google Scholar] [CrossRef]
- Peplonska, B.; Kaluzny, P.; Trafalska, E. Rotating night shift work and nutrition of nurses and midwives. Chronobiol. Int. 2019, 36, 945–954. [Google Scholar] [CrossRef]
- Shaw, E.; Dorrian, J.; Coates, A.M.; Leung, G.K.; Davis, R.; Rosbotham, E.; Warnock, R.; Huggins, C.E.; Bonham, M.P. Temporal pattern of eating in night shift workers. Chronobiol. Int. 2019, 36, 1613–1625. [Google Scholar] [CrossRef] [PubMed]
- Terada, T.; Mistura, M.; Tulloch, H.; Pipe, A.; Reed, J. Dietary behaviour is associated with cardiometabolic and psychological risk indicators in female hospital nurses-A post-hoc, cross-sectional study. Nutrients 2019, 11, 2054. [Google Scholar] [CrossRef]
- van de Langenberg, D.; Vlaanderen, J.J.; Dollé, M.E.; Rookus, M.A.; van Kerkhof, L.W.; Vermeulen, R.C. Diet, physical activity, and daylight exposure patterns in night-shift workers and day workers. Ann. Work Expo. Health 2019, 63, 9–21. [Google Scholar] [CrossRef]
- Buchvold, H.V.; Pallesen, S.; Waage, S.; Moen, B.E.; Bjorvatn, B. Shift work and lifestyle factors: A 6-year follow-up study among nurses. Front. Public Health 2019, 7, 281. [Google Scholar] [CrossRef]
- Kolbe-Alexander, T.L.; Gomersall, S.; Clark, B.; Torquati, L.; Pavey, T.; Brown, W.J. A hard day’s night: Time use in shift workers. BMC Public Health 2019, 19, 452. [Google Scholar] [CrossRef]
- Pham, T.T.; Park, B. Alcohol use disorder and health-related quality of life in Korean night-shift workers: A cross-sectional study using the KNHANES 2007-2015 data. PLoS ONE 2019, 14, e0214593. [Google Scholar] [CrossRef]
- Cho, Y.M.; Kim, H.R.; Kang, M.Y.; Myong, J.P.; Koo, J.W. Fixed night workers and failed smoking cessation. J. Occup. Med. Toxicol. 2019, 14, 23. [Google Scholar] [CrossRef]
- Kędzierska, A.; Czerepaniak, E.; Stanisławska, M.; Wieder-Huszla, S.; Wesołowska, J.; Jurczak, A. The influence of shift work on health behaviors and self-reported health status of nurses. Pielegniarstwo XXI Wieku 2019, 18, 42–49. [Google Scholar] [CrossRef]
- Navarro, D.J.; Alpert, P.T.; Cross, C. The impact of shift work on diabetes self-management activities. J. Dr. Nurs. Pract. 2019, 12, 66–72. [Google Scholar] [CrossRef]
- Hermansson, J.; Bøggild, H.; Hallqvist, J.; Karlsson, B.; Knutsson, A.; Nilsson, T.; Reuterwall, C.; Gådin, K.G. Interaction between shift work and established coronary risk factors. Int. J. Occup. Environ. Med. 2019, 10, 57–65. [Google Scholar] [CrossRef]
- Holst, M.M.; Wirth, M.D.; Mnatsakanova, A.; Burch, J.B.; Charles, L.E.; Tinney-Zara, C.; Fekedulegn, D.; Andrew, M.E.; Hartley, T.A.; Violanti, J.M. Shift Work and Biomarkers of Subclinical Cardiovascular Disease: The BCOPS Study. J. Occup. Environ. Med. 2019, 61, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Hulsegge, G.; Picavet, H.S.J.; van der Beek, A.J.; Verschuren, W.M.; Twisk, J.W.; Proper, K.I. Shift work, chronotype and the risk of cardiometabolic risk factors. Eur. J. Public Health 2019, 29, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Joo, J.H.; Lee, D.W.; Choi, D.W.; Park, E.C. Association between night work and dyslipidemia in South Korean men and women: A cross-sectional study. Lipids Health Dis. 2019, 18, 75. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.; Kang, S.K.; Choi, W.J.; Lee, S.H.; Lee, J.H.; Kwak, K. Association between shift work and hyperhomocysteinemia in male workers. Ann. Occup. Environ. Med. 2019, 31, e1. [Google Scholar] [CrossRef] [PubMed]
- Kwak, H.S.; Park, H.O.; Kim, Y.O.; Son, J.S.; Kim, C.W.; Lee, J.H.; Shin, Y.H.; Park, S.H.; Chung, E.Y.; Chae, C.H. The effect of shift work on high sensitivity C-reactive protein level among female workers. Ann. Occup. Environ. Med. 2019, 31, e5. [Google Scholar] [CrossRef]
- Ritonja, J.; Tranmer, J.; Aronson, K.J. The relationship between night work, chronotype, and cardiometabolic risk factors in female hospital employees. Chronobiol. Int. 2019, 36, 616–628. [Google Scholar] [CrossRef]
- Skogstad, M.; Mamen, A.; Lunde, L.K.; Ulvestad, B.; Matre, D.; Aass, H.C.D.; Øvstebø, R.; Nielsen, P.; Samuelsen, K.N.; Skare, Ø.; et al. Shift work including night work and long working hours in industrial plants increases the risk of atherosclerosis. Int. J. Environ. Res. Public Health 2019, 16, 521. [Google Scholar] [CrossRef]
- Strzemecka, J.; Skrodziuk, J. The influence of shift work on the occurrence of hypertension, ischemic heart disease and dyslipidemia from the perspective of mine shift workers. Health Probl. Civiliz. 2019, 13, 187–192. [Google Scholar] [CrossRef]
- Tucker, P.; Härmä, M.; Ojajärvi, A.; Kivimäki, M.; Leineweber, C.; Oksanen, T.; Salo, P.; Vahtera, J. Associations between shift work and use of prescribed medications for the treatment of hypertension, diabetes, and dyslipidemia: A prospective cohort study. Scand. J. Work Environ. Health 2019, 45, 465–474. [Google Scholar] [CrossRef]
- Ferguson, J.M.; Costello, S.; Neophytou, A.M.; Balmes, J.R.; Bradshaw, P.T.; Cullen, M.R.; Eisen, E.A. Night and rotational work exposure within the last 12 months and risk of incident hypertension. Scand. J. Work Environ. Health 2019, 45, 256–266. [Google Scholar] [CrossRef]
- Nascimento, J.O.V.; Santos, J.D.; Meira, K.C.; Pierin, A.M.G.; Souza-Talarico, J.N. Shift work of nursing professionals and blood pressure, burnout and common mental disorders. Rev. Esc. Enferm. USP 2019, 53, e03443. [Google Scholar] [CrossRef]
- Park, J.; Shin, S.Y.; Kang, Y.; Rhie, J. Effect of night shift work on the control of hypertension and diabetes in workers taking medication. Ann. Occup. Environ. Med. 2019, 31, e27. [Google Scholar] [CrossRef] [PubMed]
- Arslan, M.; Welcome, M.O.; Dane, S. The effect of sleep deprivation on heart rate variability in shift nurses. J. Res. Med. Dent. Sci. 2019, 7, 45–52. [Google Scholar]
- Hammer, P.; Hageman, I.; Garde, A.; Begtrup, L.; Flachs, E.; Hansen, J.; Hansen, Å.; Hougaard, K.; Kolstad, H.; Larsen, A.; et al. Night work and postpartum depression. Scand. J. Work Environ. Health 2019, 45, 577–587. [Google Scholar] [CrossRef] [PubMed]
- Moreira, H.; Fonseca, A.; Caiado, B.; Canavarro, M.C. Work-family conflict and mindful parenting: The mediating role of parental psychopathology symptoms and parenting stress in a sample of Portuguese employed parents. Front. Psychol. 2019, 10, 635. [Google Scholar] [CrossRef] [PubMed]
- Peterson, S.A.; Wolkow, A.P.; Lockley, S.W.; O’Brien, C.S.; Qadri, S.; Sullivan, J.P.; Czeisler, C.A.; Rajaratnam, S.M.W.; Barger, L.K. Associations between shift work characteristics, shift work schedules, sleep and burnout in North American police officers: A cross-sectional study. BMJ Open 2019, 9, e030302. [Google Scholar] [CrossRef]
- Kim, K.K.; Lee, K.R.; Suh, H.S.; Ko, K.D.; Hwang, I.C. Association between shift work and suicidal ideation: Data from the Korea National Health and Nutrition Examination Survey (2008–2016). Scand. J. Work Environ. Health 2019, 45, 458–464. [Google Scholar] [CrossRef]
- Park, S.M. Effects of work conditions on suicidal ideation among middle-aged adults in South Korea. Int. J. Soc. Psychiatry 2019, 65, 144–150. [Google Scholar] [CrossRef]
- Hall, A.L.; Kecklund, G.; Leineweber, C.; Tucker, P. Effect of work schedule on prospective antidepressant prescriptions in Sweden: A 2-year sex-stratified analysis using national drug registry data. BMJ Open 2019, 9, e023247. [Google Scholar] [CrossRef]
- Tahghighi, M.; Brown, J.A.; Breen, L.J.; Kane, R.; Hegney, D.; Rees, C.S. A comparison of nurse shift workers’ and non-shift workers’ psychological functioning and resilience. J. Adv. Nurs. 2019, 75, 2570–2578. [Google Scholar] [CrossRef]
- Bracci, M.; Copertaro, A.; Ciarapica, V.; Barbaresi, M.; Esposito, S.; Albanesi, A.; Valentino, M.; Ledda, C.; Rapisarda, V.; Santarelli, L. Nocturnin gene diurnal variation in healthy volunteers and expression levels in shift workers. Biomed Res. Int. 2019, 2019, 7582734. [Google Scholar] [CrossRef] [PubMed]
- Gowda, R.H.; Sukumar, G.M.; Gowda, S.H. Association between metabolic risk, oxidative stress and rotating shift work in a tertiary health care facility. Clin. Epidemiol. Glob. Health 2019, 7, 564–570. [Google Scholar] [CrossRef]
- Khosravipour, M.; Shahmohammadi, M.; Athar, H.V. The effects of rotating and extended night shift work on the prevalence of metabolic syndrome and its components. Diabetes Metab. Syndr. 2019, 13, 3085–3089. [Google Scholar] [CrossRef] [PubMed]
- Kiranmala, K.; Aslam, M.; Mishra, B.K.; Jhamb, R.; Madhu, S.V. Association of postprandial triglyceride responses with insulin resistance among rotational night shift healthcare workers. Exp. Physiol. 2019, 104, 819–825. [Google Scholar] [CrossRef] [PubMed]
- Ledda, C.; Cinà, D.; Matera, S.; Mucci, N.; Bracci, M.; Rapisarda, V. High HOMA-IR index in healthcare shift workers. Medicina 2019, 55, 186. [Google Scholar] [CrossRef]
- Loef, B.; Baarle, D.V.; Van Der Beek, A.J.; Beekhof, P.K.; Van Kerkhof, L.W.; Proper, K.I. The association between exposure to different aspects of shift work and metabolic risk factors in health care workers, and the role of chronotype. PLoS ONE 2019, 14, e0211557:1–e0211557:14. [Google Scholar] [CrossRef]
- Nikpour, M.; Tirgar, A.; Hajiahmadi, M.; Hosseini, A.; Heidari, B.; Ghaffari, F.; Ebadi, A.; Nasiri, F.; Firouzbakht, M. Shift work and metabolic syndrome: A multi-center cross-sectional study on females of reproductive age. Biomed. Rep. 2019, 10, 311–317. [Google Scholar] [CrossRef]
- Hanprathet, N.; Lertmaharit, S.; Lohsoonthorn, V.; Rattananupong, T.; Ammaranond, P.; Jiamjarasrangsi, W. Increased risk of type 2 diabetes and abnormal FPG due to shift work differs according to gender: A retrospective cohort study among Thai workers in Bangkok, Thailand. Diabetes Metab. Syndr. Obes. 2019, 12, 2341–2354. [Google Scholar] [CrossRef]
- Silva-Costa, A.; Rotenberg, L.; Baltar, V.T.; Coeli, C.M.; Fonseca, M.D.J.M.D.; Melo, E.C.P.; Griep, R.H. Structural equation modeling of associations between night work and glycemic levels. Arch. Endocrinol. Metab. 2019, 63, 487–494. [Google Scholar] [CrossRef]
- Zoto, E.; Cenko, F.; Doci, P.; Rizza, S. Effect of night shift work on risk of diabetes in healthy nurses in Albania. Acta Diabetol. 2019, 56, 811–813. [Google Scholar] [CrossRef]
- Rabanipour, N.; Roohafza, H.; Feizi, A.; Tirani, S.A.; Sarrafzadegan, N. Association between shift work and obesity in a large sample of Iranian steel industry workers. Arh. Hig. Rada Toksikol. 2019, 70, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Bracci, M.; Ciarapica, V.; Eléxpuru Zabaleta, M.; Tartaglione, M.F.; Pirozzi, S.; Giuliani, L.; Piva, F.; Valentino, M.; Ledda, C.; Rapisarda, V.; et al. BRCA1 and BRCA2 gene expression: Diurnal variability and influence of shift work. Cancers 2019, 11, 1146. [Google Scholar] [CrossRef] [PubMed]
- Bustamante-Montes, L.P.; Flores-Meza, B.; Hernández-Valero, M.A.; Cárdenas-López, A.; Dolores-Velázquez, R.; Borja-Bustamante, P.; Borja-Aburto, V.H. Night shift work and risk of breast cancer in women. Arch. Med. Res. 2019, 50, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Carugno, M.; Maggioni, C.; Crespi, E.; Bonzini, M.; Cuocina, S.; Dioni, L.; Tarantini, L.; Consonni, D.; Ferrari, L.; Pesatori, A.C. Night shift work, DNA methylation and telomere length: An investigation on hospital female nurses. Int. J. Environ. Res. 2019, 16, 2292. [Google Scholar] [CrossRef]
- Jones, M.E.; Schoemaker, M.J.; McFadden, E.C.; Wright, L.B.; Johns, L.E.; Swerdlow, A.J. Night shift work and risk of breast cancer in women: The Generations Study cohort. Br. J. Cancer 2019, 121, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Pahwa, M.; Labrèche, F.; Kim, J.; Harris, M.A.; Song, C.; Peters, C.E.; Arrandale, V.H.; Davies, H.; McLeod, C.B.; Demers, P.A. The impact of night shift work on breast cancer: Results from the Burden of Occupational Cancer in Canada Study. Am. J. Ind. Med. 2019, 62, 635–642. [Google Scholar] [CrossRef]
- Pham, T.T.; Hwang, M.; Lee, E.S.; Kong, S.Y.; Jung, S.Y.; Lee, S.; Kim, J.; Ha, M.; Kim, S.Y.; Park, B. Night-shift work and risk of breast cancer in Korean women. Clin. Epidemiol. 2019, 11, 743–751. [Google Scholar] [CrossRef]
- Barul, C.; Richard, H.; Parent, M.E. Night-shift work and risk of prostate cancer: Results from a Canadian case-control study, the prostate cancer and environment study. Am. J. Epidemiol. 2019, 188, 1801–1811. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.; Park, W.J.; Kang, W.; Lim, D.Y.; Kim, S.; Moon, J.D. Night shiftwork and prostate-specific antigen level in a tire manufacturing factory. Ann. Occup. Environ. Med. 2019, 31, e19. [Google Scholar] [CrossRef]
- Leung, L.; Grundy, A.; Siemiatycki, J.; Arseneau, J.; Gilbert, L.; Gotlieb, W.H.; Provencher, D.M.; Aronson, K.J.; Koushik, A. Shift Work Patterns, chronotype, and epithelial ovarian cancer risk. Cancer Epidemiol. Biomark. Prev. 2019, 28, 987–995. [Google Scholar] [CrossRef] [PubMed]
- El-Zaemey, S.; Carey, R.N. Variations in exposure to carcinogens among shift workers and non-shift workers. Am. J. Ind. Med. 2019, 62, 352–356. [Google Scholar] [CrossRef] [PubMed]
- Hanprathet, N.; Lertmaharit, S.; Lohsoonthorn, V.; Rattananupong, T.; Ammaranond, P.; Jiamjarasrangsi, W. Shift work and leukocyte count changes among workers in Bangkok. Ann. Work Expo. Health 2019, 63, 689–700. [Google Scholar] [CrossRef] [PubMed]
- Loef, B.; Nanlohy, N.M.; Jacobi, R.H.; van de Ven, C.; Mariman, R.; van der Beek, A.J.; Proper, K.I.; van Baarle, D. Immunological effects of shift work in healthcare workers. Sci. Rep. 2019, 9, 18220. [Google Scholar] [CrossRef] [PubMed]
- Nikpour, M.; Tirgar, A.; Hajiahmadi, M.; Ebadi, A.; Ghaffari, F.; Hosseini, A.; Heidari, B. A cross-sectional study on serum high-sensitivity C-reactive protein level and shift work among reproductive age women. Casp. J. Intern. Med. 2019, 10, 402. [Google Scholar] [CrossRef]
- Reinhardt, É.L.; Fernandes, P.A.C.M.; Markus, R.P.; Fischer, F.M. Night work effects on salivary cytokines TNF, IL-1β and IL-6. Chronobiol. Int. 2019, 36, 11–26. [Google Scholar] [CrossRef]
- Teixeira, K.R.; dos Santos, C.P.; de Medeiros, L.A.; Mendes, J.A.; Cunha, T.M.; De Angelis, K.; Penha-Silva, N.; de Oliveira, E.P.; Crispim, C.A. Night workers have lower levels of antioxidant defenses and higher levels of oxidative stress damage when compared to day workers. Sci. Rep. 2019, 9, 4455. [Google Scholar] [CrossRef]
- Haluza, D.; Schmidt, V.M.; Blasche, G. Time course of recovery after two successive night shifts: A diary study among Austrian nurses. J. Nurs. Manag. 2019, 27, 190–196. [Google Scholar] [CrossRef]
- Imes, C.C.; Chasens, E.R. Rotating shifts negatively impacts health and wellness among intensive care nurses. Workplace Health Saf. 2019, 67, 241–249. [Google Scholar] [CrossRef]
- Levin, H.; Lim, R.; Lynch, T.; Sangha, G. Improving resident well-being during shiftwork: Are casino shifts the answer? Pediatr. Emerg. Care 2019, 35, 852–855. [Google Scholar] [CrossRef]
- Turchi, V.; Verzuri, A.; Nante, N.; Napolitani, M.; Bugnoli, G.; Severi, F.M.; Quercioli, C.; Messina, G. Night work and quality of life. A study on the health of nurses. Ann. Ist. Super. Sanita 2019, 55, 161–169. [Google Scholar] [CrossRef]
- Clarkson-Townsend, D.A.; Everson, T.M.; Deyssenroth, M.A.; Burt, A.A.; Hermetz, K.E.; Hao, K.; Chen, J.; Marsit, C.J. Maternal circadian disruption is associated with variation in placental DNA methylation. PLoS ONE 2019, 14, e0215745. [Google Scholar] [CrossRef] [PubMed]
- Specht, I.O.; Hammer, P.E.; Flachs, E.M.; Begtrup, L.M.; Larsen, A.D.; Hougaard, K.S.; Hansen, J.; Hansen, A.M.; Kolstad, H.A.; Rugulies, R.; et al. Night work during pregnancy and preterm birth—A large register-based cohort study. PLoS ONE 2019, 14, e0215748. [Google Scholar] [CrossRef] [PubMed]
- Willis, S.K.; Hatch, E.E.; Wesselink, A.K.; Rothman, K.J.; Mikkelsen, E.M.; Wise, L.A. Female sleep patterns, shift work, and fecundability in a North American preconception cohort study. Fertil. Steril. 2019, 111, 1201–1210. [Google Scholar] [CrossRef]
- Begtrup, L.M.; Specht, I.O.; Hammer, P.E.C.; Flachs, E.M.; Garde, A.H.; Hansen, J.; Hansen, A.M.; Kolstad, H.A.; Larsen, A.D.; Bonde, J.P. Night work and miscarriage: A Danish nationwide register-based cohort study. Occup. Environ. Med. 2019, 76, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Stock, D.; Knight, J.A.; Raboud, J.; Cotterchio, M.; Strohmaier, S.; Willett, W.; Eliassen, A.H.; Rosner, B.; Hankinson, S.E.; Schernhammer, E. Rotating night shift work and menopausal age. Hum. Reprod. 2019, 34, 539–548. [Google Scholar] [CrossRef]
- Choi, Y.I.; Park, D.K.; Chung, J.W.; Kim, K.O.; Kwon, K.A.; Kim, Y.J. Circadian rhythm disruption is associated with an increased risk of sarcopenia: A nationwide population-based study in Korea. Sci. Rep. 2019, 9, 12015. [Google Scholar] [CrossRef] [PubMed]
- Nabe-Nielsen, K.; Hansen, Å.M.; Ishtiak-Ahmed, K.; Grynderup, M.B.; Gyntelberg, F.; Islamoska, S.; Mortensen, E.L.; Phung, T.K.T.; Rod, N.H.; Waldemar, G.; et al. Night shift work, long working hours and dementia: A longitudinal study of the Danish Work Environment Cohort Study. BMJ Open 2019, 9, e027027. [Google Scholar] [CrossRef]
- White, A.J.; Kresovich, J.K.; Xu, Z.; Sandler, D.P.; Taylor, J.A. Shift work, DNA methylation and epigenetic age. Int. J. Epidemiol. 2019, 48, 1536–1544. [Google Scholar] [CrossRef]
- Choi, H.; Oh, H.J.; Shin, J.S.; Lim, M.; Kim, S.K.; Kang, H.T.; Oh, S.S.; Koh, S.B. Relationship between shift work and liver enzymes: A cross-sectional study based on the Korea National Health and Examination Survey (2007–2015). Ann. Occup. Environ. Med. 2019, 31, e15. [Google Scholar] [CrossRef]
- Wang, F.; Zhang, L.; Wu, S.; Li, W.; Sun, M.; Feng, W.; Ding, D.; Wong, S.Y.; Zhu, P.; Evans, G.J.; et al. Night shift work and abnormal liver function: Is non-alcohol fatty liver a necessary mediator? Occup. Environ. Med. 2019, 76, 83–89. [Google Scholar] [CrossRef]
- Abrishami, M.; Fadakar, P.; Mirghorbani, M.; Masoumi, A.; Hassanzadeh, S. Effect of night work on image quality of optical coherence tomography angiography. J. Curr. Ophthalmol. 2019, 31, 438–441. [Google Scholar] [CrossRef] [PubMed]
- Bazazan, A.; Dianat, I.; Bahrampour, S.; Talebian, A.; Zandi, H.; Sharafkhaneh, A.; Maleki-Ghahfarokhi, A. Association of musculoskeletal disorders and workload with work schedule and job satisfaction among emergency nurses. Int. Emerg. Nurs. 2019, 44, 8–13. [Google Scholar] [CrossRef]
- Hannerz, H.; Soll-Johanning, H.; Larsen, A.D.; Garde, A.H. Night-time work and all-cause mortality in the general working population of Denmark. Int. Arch. Occup. Environ. Health 2019, 92, 577–585. [Google Scholar] [CrossRef] [PubMed]
- Katsifaraki, M.; Nilsen, K.B.; Christensen, J.O.; Wærsted, M.; Knardahl, S.; Bjorvatn, B.; Härmä, M.; Matre, D. Sleep duration mediates abdominal and lower-extremity pain after night work in nurses. Int. Arch. Occup. Environ. Health 2019, 92, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Leite, H.M.; Garcez, A.; Nunes, M.A.A.; Pattussi, M.P.; Canuto, R.; Paniz, V.M.V.; Olinto, M.T.A. Shift work, sleep duration, and body image dissatisfaction among female workers in southern Brazil. Arch. Women’s Ment. Health 2019, 22, 583–592. [Google Scholar] [CrossRef]
- Loef, B.; van Baarle, D.; van der Beek, A.J.; Sanders, E.A.; Bruijning-Verhagen, P.; Proper, K.I. Shift work and respiratory infections in health-care workers. Am. J. Epidemiol. 2019, 188, 509–517. [Google Scholar] [CrossRef]
- Lu, F.; Suggs, A.; Ezaldein, H.H.; Ya, J.; Fu, P.; Jamora, J.; Verallo-Rowel, V.; Baron, E.D. The effect of shift work and poor sleep on self-reported skin conditions: A Survey of call center agents in the Philippines. Clocks Sleep 2019, 1, 273–279. [Google Scholar] [CrossRef]
- Papantoniou, K.; Massa, J.; Devore, E.; Munger, K.L.; Chitnis, T.; Ascherio, A.; Schernhammer, E.S. Rotating night shift work and risk of multiple sclerosis in the Nurses’ Health Studies. Occup. Environ. Med. 2019, 76, 733–738. [Google Scholar] [CrossRef]
- Razavi, P.; Devore, E.E.; Bajaj, A.; Lockley, S.W.; Figueiro, M.G.; Ricchiuti, V.; Gauderman, W.J.; Hankinson, S.E.; Willett, W.C.; Schernhammer, E.S. Shift work, chronotype, and melatonin rhythm in nurses. Cancer Epidemiol. Biomark. Prev. 2019, 28, 1177–1186. [Google Scholar] [CrossRef]
- Sigalos, J.T.; Kohn, T.P.; Cartagenova, L.; Dao, Z.; Gondokusumo, J.C.; Santiago, J.; Kohn, J.R.; Pickett, S.M.; Pastuszak, A.W.; Lipshultz, L.I. Shift workers with shift work disorder have worse lower urinary tract symptoms. Urology 2019, 128, 66–70. [Google Scholar] [CrossRef]
- Wang, D.; Zhou, Y.; Ma, J.; Xiao, L.; Cao, L.; Zhou, M.; Kong, W.; Wang, Z.; Li, W.; He, M.; et al. Association between shift work and hearing loss: The Dongfeng-Tongji cohort study. Hear. Res. 2019, 384, 107827:1–107827:7. [Google Scholar] [CrossRef] [PubMed]
- Behrens, T.; Burek, K.; Pallapies, D.; Kösters, L.; Lehnert, M.; Beine, A.; Wichert, K.; Kantermann, T.; Vetter, C.; Brüning, T.; et al. Decreased psychomotor vigilance of female shift workers after working night shifts. PLoS ONE 2019, 14, e0219087:1–e0219087:17. [Google Scholar] [CrossRef] [PubMed]
- Patterson, P.D.; Weaver, M.D.; Markosyan, M.A.; Moore, C.G.; Guyette, F.X.; Doman, J.M.; Sequeira, D.J.; Werman, H.A.; Swanson, D.; Hostler, D.; et al. Impact of shift duration on alertness among air-medical emergency care clinician shift workers. Am. J. Ind. Med. 2019, 62, 325–336. [Google Scholar] [CrossRef] [PubMed]
- Rosa, D.E.; Marot, L.P.; de Mello, M.T.; Narciso, F.V.; Gonçalves, B.D.S.B.; Marqueze, E.C.; Crispim, C.A. Shift rotation, circadian misalignment and excessive body weight influence psychomotor performance: A prospective and observational study under real life conditions. Sci. Rep. 2019, 9, 19333. [Google Scholar] [CrossRef] [PubMed]
- Tummers, F.H.; Huizinga, C.R.; Stockmann, H.B.; Hamming, J.F.; Cohen, A.F.; van der Bogt, K.E. Objective assessment of fitness to perform (FTOP) after surgical night shifts in the Netherlands: An observational study using the validated FTOP self-test in daily surgical practice. Ann. Surg. 2019, 270, 930–936. [Google Scholar] [CrossRef] [PubMed]
- Dall’Ora, C.; Ball, J.; Redfern, O.; Recio-Saucedo, A.; Maruotti, A.; Meredith, P.; Griffiths, P. Are long nursing shifts on hospital wards associated with sickness absence? A longitudinal retrospective observational study. J. Nurs. Manag. 2019, 27, 19–26. [Google Scholar] [CrossRef]
- Hammer, P.; Garde, A.H.; Begtrup, L.M.; Flachs, E.M.; Hansen, J.; Hansen, Å.M.; Hougaard, K.S.; Kolstad, H.A.; Larsen, A.D.; Pinborg, A.B.; et al. Night work and sick leave during pregnancy: A national register-based within-worker cohort study. Occup. Environ. Med. 2019, 76, 163–168. [Google Scholar] [CrossRef]
- Ropponen, A.; Koskinen, A.; Puttonen, S.; Härmä, M. Exposure to working-hour characteristics and short sickness absence in hospital workers: A case-crossover study using objective data. Int. J. Nurs. Stud. 2019, 91, 14–21. [Google Scholar] [CrossRef]
- Vedaa, Ø.; Pallesen, S.; Erevik, E.K.; Svensen, E.; Waage, S.; Bjorvatn, B.; Sivertsen, B.; Harris, A. Long working hours are inversely related to sick leave in the following 3 months: A 4-year registry study. Int. Arch. Occup. Environ. Health 2019, 92, 457–466. [Google Scholar] [CrossRef]
- Donnelly, E.A.; Bradford, P.; Davis, M.; Hedges, C.; Socha, D.; Morassutti, P. Fatigue and safety in paramedicine. Can. J. Emerg. Med. 2019, 21, 762–765. [Google Scholar] [CrossRef]
- Nielsen, H.B.; Dyreborg, J.; Hansen, Å.M.; Hansen, J.; Kolstad, H.A.; Larsen, A.D.; Nabe-Nielsen, K.; Garde, A.H. Shift work and risk of occupational, transport and leisure-time injury. A register-based case-crossover study of Danish hospital workers. Saf. Sci. 2019, 120, 728–734. [Google Scholar] [CrossRef]
- Vedaa, Ø.; Harris, A.; Erevik, E.K.; Waage, S.; Bjorvatn, B.; Sivertsen, B.; Moen, B.E.; Pallesen, S. Short rest between shifts (quick returns) and night work is associated with work-related accidents. Int. Arch. Occup. Environ. Health 2019, 92, 829–835. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, T.; Li, J.; Pollmann-Schult, M. Evening and night work schedules and children’s social and emotional well-being. Community Work Fam. 2019, 22, 167–182. [Google Scholar] [CrossRef]
- Strohmaier, S.; Devore, E.E.; Huang, T.; Vetter, C.; Eliassen, A.H.; Rosner, B.; Okereke, O.I.; Austin, S.B.; Schernhammer, E.S. Maternal rotating night shift work before pregnancy and offspring stress markers. Physiol. Behav. 2019, 207, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Strohmaier, S.; Devore, E.E.; Vetter, C.; Eliassen, A.H.; Rosner, B.; Okereke, O.I.; Schernhammer, E.S. Night shift work before and during pregnancy in relation to depression and anxiety in adolescent and young adult offspring. Eur. J. Epidemiol. 2019, 34, 625–635. [Google Scholar] [CrossRef] [PubMed]
- Wei, C.F.; Chen, M.H.; Lin, C.C.; Guo, Y.L.; Lin, S.J.; Liao, H.F.; Hsieh, W.S.; Chen, P.C. Association between maternal shift work and infant neurodevelopmental outcomes: Results from the Taiwan Birth Cohort Study with propensity-score-matching analysis. Int. J. Epidemiol. 2019, 48, 1545–1555. [Google Scholar] [CrossRef] [PubMed]
- Matheson, A.; O’Brien, L.; Reid, J.A. Women’s experience of shiftwork in nursing whilst caring for children: A juggling act. J. Clin. Nurs. 2019, 28, 3817–3826. [Google Scholar] [CrossRef]
- Costa, D.; Silva, I.S. Social and family life impact of shift work from the perspective of family members. Rev. Adm. Empresas 2019, 59, 108–120. [Google Scholar] [CrossRef]
- Vaghar, M.I.; Masrour, M.J. A comparative study of satisfaction and family conflicts among married nurses with different working hours. J. Family Med. Prim. Care 2019, 8, 472–476. [Google Scholar] [CrossRef]
- Smith, C.S.; Folkard, S.; Fuller, J.A. Shiftwork and working hours. In Handbook of Occupational Health Psychology, 2nd ed.; Quick, J.C., Tetrick, L.E., Eds.; American Psychological Association: Washington, DC, USA, 2003; pp. 163–183. ISBN 978-1-4338-0776-3. [Google Scholar]
- Sweileh, W.M. Analysis and mapping of global research publications on shift work (2012–2021). J. Occup. Med. Toxicol. 2022, 17, 22. [Google Scholar] [CrossRef]
- Garde, A.H.; Begtrup, L.; Bjorvatn, B.; Bonde, J.P.; Hansen, J.; Hansen, Å.M.; Härmä, M.; Jensen, M.A.; Kecklund, G.; Kolstad, H.A.; et al. How to schedule night shift work in order to reduce health and safety risks. Scand. J. Work Environ. Health 2020, 46, 557–569. [Google Scholar] [CrossRef] [PubMed]
- Gadbois, C. Les discordances psychosociales des horaires postés: Questions en suspens [Psychosocial conflicts created by shift work patterns: Pending Questions]. Trav. Hum. 2004, 67, 63–85. [Google Scholar] [CrossRef]
- Bolino, M.C.; Kelemen, T.K.; Matthews, S.H. Working 9-to-5? A review of research on nonstandard work schedules. J. Organ. Behav. 2021, 42, 188–211. [Google Scholar] [CrossRef]
- International Labour Organization. Working Time and Work-Life Balance around the World; International Labour Office: Geneva, Switzerland, 2022; ISBN 978-92-2-037891-5. [Google Scholar]
| Main Category | Subcategories | Variables | Articles | |
|---|---|---|---|---|
| Health (n = 136) | Sleep and fatigue (n = 27) | Sleep (n = 21) | Burch et al. [34] Cerqueira Teixeira et al. [35] Chang and Li [36] Dai et al. [37] Di Muzio et al. [38] B. Ferguson et al. [39] Flaa et al. [40] Fowler and Ellis [41] Ganesan et al. [42] Haile et al. [43] Härmä et al. [44] | Hattammaru et al. [45] Hulsegge, Loef et al. [46] Jeong et al. [47] Mulhall et al. [48] Pallensen et al. [49] H. Park et al. [50] Resuehr et al. [51] Schuster et al. [52] Uekata et al. [53] Wilson et al. [54] |
| Fatigue (n = 6) | Burch et al. [34] Di Muzio et al. [38] Härmä et al. [44] | Bazazan, Rasoulzadeh et al. [55] Chang et al. [56] Yu et al. [57] | ||
| Lifestyle (n = 19) | Eating habits (n = 9) | Müge Arslan et al. [58] Fradkin et al. [59] Fröhlich et al. [60] Heath et al. [61] Nogueira et al. [62] | Peplonska et al. [63] Shaw et al. [64] Terada et al. [65] van de Langenberg et al. [66] | |
| Physical exercise (n = 3) | van de Langenberg et al. [66] Buchvold et al. [67] | Kolbe-Alexander et al. [68] | ||
| Alcoholism (n = 2) | Buchvold et al. [67] | Pham and Park [69] | ||
| Smoking (n = 2) | Buchvold et al. [67] | Y.M. Cho et al. [70] | ||
| Health behaviors (n = 2) | Kędzierska et al. [71] | Navarro et al. [72] | ||
| Caffeine (n = 1) | Buchvold et al. [67] | |||
| Cardiovascular (n = 17) | Cardiometabolic risk factors (n = 11) | Terada et al. [65] Hermansson et al. [73] Holst et al. [74] Hulsegge, Picavet et al. [75] Joo et al. [76] Kang et al. [77] | Kwak et al. [78] Ritonja et al. [79] Skogstad et al. [80] Strzemecka and Skrodziuk [81] Tucker et al. [82] | |
| Hypertension (n = 4) | Strzemecka and Skrodziuk [81] J.M. Ferguson et al. [83] | Nascimento et al. [84] J. Park et al. [85] | ||
| Heart rate (n = 2) | Burch et al. [34] | Muzeyyen Arslan et al. [86] | ||
| Mental health (n = 16) | Depression (n = 5) | Dai et al. [37] H. Park et al. [50] Bazazan, Rasoulzadeh et al. [55] | Hammer, Hageman et al. [87] Moreira et al. [88] | |
| Anxiety (n = 3) | Dai et al. [37] Bazazan, Rasoulzadeh et al. [55] | Moreira et al. [88] | ||
| Burnout (n = 3) | Fowler and Ellis [41] Nascimento et al. [84] | Peterson et al. [89] | ||
| Suicidal ideation (n = 2) | Kim et al. [90] | Park [91] | ||
| Psychological health (n = 1) | Terada et al. [65] | |||
| Antidepressant prescriptions (n = 1) | Hall et al. [92] | |||
| Resilience (n = 1) | Tahghighi et al. [93] | |||
| Metabolic system (n = 13) | System problems (n = 7) | Bracci, Copertaro et al. [94] Gowda et al. [95] Khosravipour et al. [96] Kiranmala et al. [97] Ledda et al. [98] | Loef, van Baarle, van der Beek, Beekhof et al. [99] Nikpour, Tirgar, Hajiahmadi, Hosseini et al. [100] | |
| Diabetes (n = 4) | J. Park et al. [85] Hanprathet et al. [101] | Silva-Costa et al. [102] Zoto et al. [103] | ||
| Obesity (n = 2) | Fröhlich et al. [60] | Rabanipour et al. [104] | ||
| Oncological (n = 10) | Breast cancer (n = 6) | Bracci, Ciarapica et al. [105] Bustamante-Montes et al. [106] Carugno et al. [107] | Jones et al. [108] Pahwa et al. [109] Pham et al. [110] | |
| Prostate cancer (n = 2) | Barul et al. [111] | S. Cho et al. [112] | ||
| Ovarian cancer (n = 1) | Leung et al. [113] | |||
| Carcinogens agents (n = 1) | El-Zaemey and Carey [114] | |||
| Immune system (n = 6) | H. Park et al. [50] Hanprathet et al. [115] Loef, Nanlohy et al. [116] | Nikpour, Tirgar, Hajiahmadi, Ebadi et al. [117] Reinhardt et al. [118] Teixeira et al. [119] | ||
| Well-being and quality of life (n = 6) | Well-being (n = 4) | Kędzierska et al. [71] Haluza et al. [120] | Imes and Chasens [121] Levin et al. [122] | |
| Quality of life (n = 2) | Pham and Park [69] | Turchi et al. [123] | ||
| Female reproductive system (n = 5) | Pregnancy (n = 3) | Clarkson-Townsend et al. [124] Specht et al. [125] | Willis et al. [126] | |
| Miscarriage (n = 1) | Begtrup et al. [127] | |||
| Menopause (n = 1) | Stock et al. [128] | |||
| Aging (n = 3) | Y.I. Choi et al. [129] Nabe-Nielsen et al. [130] | White et al. [131] | ||
| Digestive system (n = 2) | H. Choi et al. [132] | F. Wang et al. [133] | ||
| Others (n = 12) | Hematological system (n = 1) | Cerqueira Teixeira et al. [35] | ||
| Eyesight (n = 1) | Abrishami et al. [134] | |||
| Musculoskeletal diseases (n = 1) | Bazazan, Dianat et al. [135] | |||
| All-cause mortality (n = 1) | Hannerz et al. [136] | |||
| Pain (n = 1) | Katsifaraki et al. [137] | |||
| Body image (n = 1) | Leite et al. [138] | |||
| Respiratory system (n = 1) | Loef, van Baarle, van der Beek, Sanders et al. [139] | |||
| Skin (n = 1) | Lu et al. [140] | |||
| Multiple sclerosis (n = 1) | Papantoniou et al. [141] | |||
| Endocrine system (n = 1) | Razavi et al. [142] | |||
| Urinary system (n = 1) | Sigalos et al. [143] | |||
| Hearing (n = 1) | D. Wang et al. [144] | |||
| Organizational context (n = 15) | Performance (n = 7) | Burch et al. [34] Ganesan et al. [42] Wilson et al. [54] Behrens et al. [145] | Patterson et al. [146] Rosa et al. [147] Tummers et al. [148] | |
| Absenteeism (n = 4) | Dall’Ora et al. [149] Hammer, Garde et al. [150] | Ropponen et al. [151] Vedaa, Pallesen et al. [152] | ||
| Safety (n = 3) | Donnelly et al. [153] Nielsen et al. [154] | Vedaa, Harris et al. [155] | ||
| Workload (n = 1) | Bazazan, Dianat et al. [135] | |||
| Family life (n = 12) | Children (n = 7) | Children’s health or well-being (n = 4) | Kaiser et al. [156] Strohmaier, Devore, Huang et al. [157] | Strohmaier, Devore, Vetter et al. [158] Wei et al. [159] |
| Parenthood (n = 2) | Moreira et al. [88] | Matheson et al. [160] | ||
| Parental relationship (n = 1) | Costa and Silva [161] | |||
| Family (n = 3) | Work–Family Conflict (n = 2) | Moreira et al. [88] | Vaghar and Masrour [162] | |
| Family environment (n = 1) | Costa and Silva [161] | |||
| Partners (n = 2) | Marital relationship (n = 1) | Costa and Silva [161] | ||
| Marital satisfaction (n = 1) | Vaghar and Masrour [162] | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, I.; Costa, D. Consequences of Shift Work and Night Work: A Literature Review. Healthcare 2023, 11, 1410. https://doi.org/10.3390/healthcare11101410
Silva I, Costa D. Consequences of Shift Work and Night Work: A Literature Review. Healthcare. 2023; 11(10):1410. https://doi.org/10.3390/healthcare11101410
Chicago/Turabian StyleSilva, Isabel, and Daniela Costa. 2023. "Consequences of Shift Work and Night Work: A Literature Review" Healthcare 11, no. 10: 1410. https://doi.org/10.3390/healthcare11101410
APA StyleSilva, I., & Costa, D. (2023). Consequences of Shift Work and Night Work: A Literature Review. Healthcare, 11(10), 1410. https://doi.org/10.3390/healthcare11101410






