Cardiorespiratory Response to Six-Minute Step Test in Post COVID-19 Patients—A Cross Sectional Study
Abstract
1. Introduction
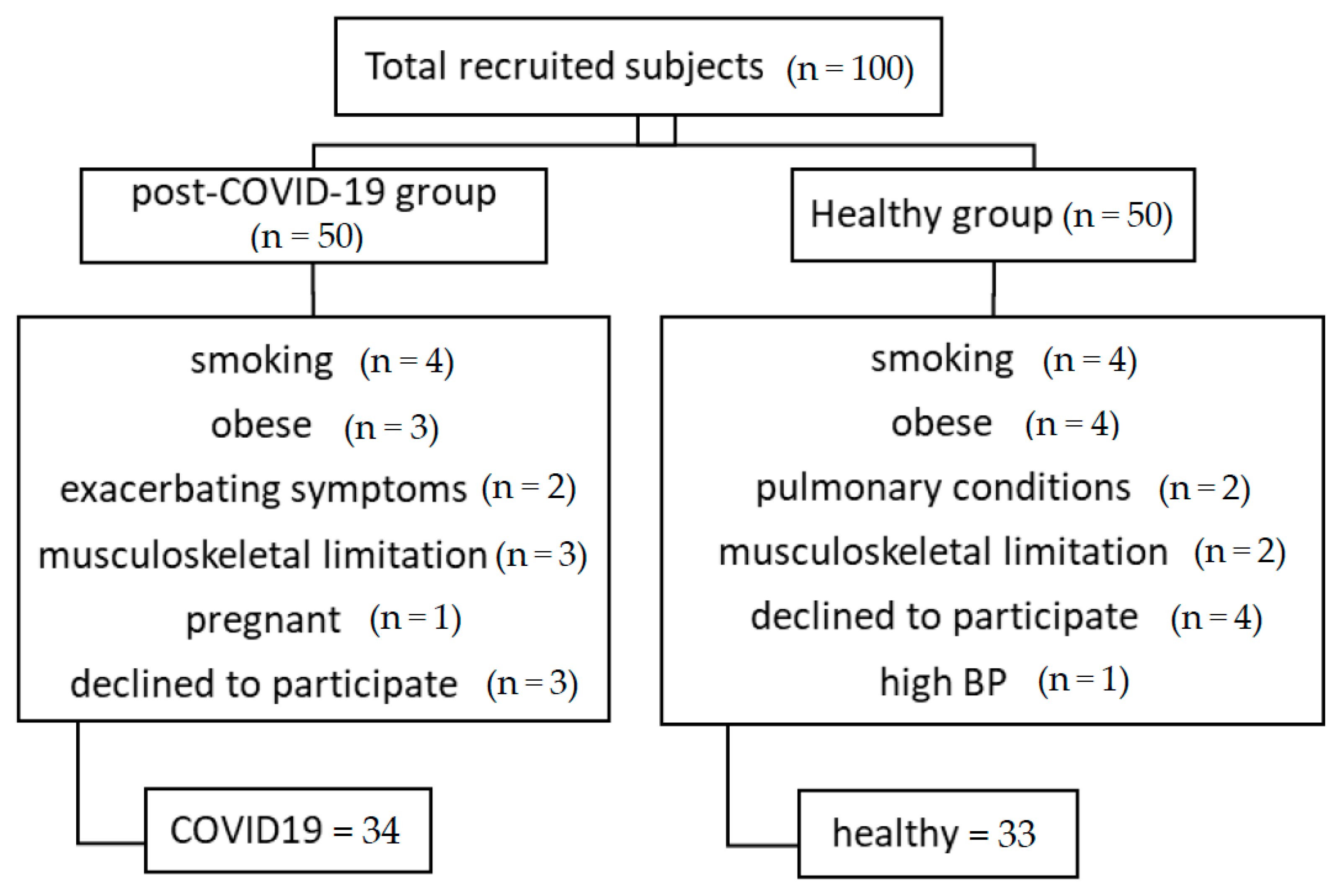
2. Methodology
2.1. Inclusion Criteria
- -
- Patients with a positive polymerase chain reaction (PCR) test for COVID-19 which was confirmed by a physician.
- -
- Past 4 weeks from the onset of acute illness (post-recovery phase).
- -
- Mild to moderate condition of COVID-19 based on the COVID-19 severity index [16] (mild conditions score 0–2 and moderate score 3–5)
- -
- Age (above 18) and gender-matched subjects will be recruited from the community for a healthy group.
2.2. Exclusion Criteria
- -
- Subjects with a history of pulmonary or cardiac conditions such as asthma, TB, and acute myocardial infarction.
- -
- History of musculoskeletal conditions that interfere with the ability to perform the test such as a recent fracture or severe osteoarthritis.
- -
- History of recurrent hemoptysis.
- -
- Obesity, smoking, cancer, and uncontrolled diabetes mellitus.
- -
- Subjects who are unable to perform the test for any reason such as mental illness or neuromuscular disorders.
- -
- Subjects who are on oxygen therapy.
- -
- Subjects who use orthosis or prosthesis.
- -
- Subjects who have exacerbating symptoms during data collection.
2.3. Study Procedure
2.4. Six-Minute Walk Test
2.5. Six-Minute Step Test
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alandijany, T.A.; Faizo, A.A.; Azhar, E.I. Coronavirus disease of 2019 (COVID-19) in the Gulf Cooperation Council (GCC) countries: Current status and management practices. J. Infect. Public Health 2020, 13, 839–842. [Google Scholar] [CrossRef]
- Korompoki, E.; Gavriatopoulou, M.; Hicklen, R.S.; Ntanasis-Stathopoulos, I.; Kastritis, E.; Fotiou, D.; Stamatelopoulos, K.; Terpos, E.; Kotanidou, A.; Hagberg, C.A.; et al. Epidemiology and Organ Specific Sequelae of Post-Acute COVID19: A Narrative Review. J. Infect. 2021, 83, 1–16. [Google Scholar] [CrossRef]
- Adil, M.T.; Rahman, R.; Whitelaw, D.; Jain, V.; Al-Taan, O.; Rashid, F.; Munasinghe, A.; Jambulingam, P. SARS-CoV-2 and the Pandemic of COVID-19. Postgrad. Med. J. 2021, 97, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Reina, J. The SARS-CoV-2, a New Pandemic Zoonosis That Threatens the World. Vacunas 2020, 21, 17–22. [Google Scholar] [CrossRef]
- Wang, F.; Kream, R.M.; Stefano, G.B. Long-Term Respiratory and Neurological Sequelae of COVID-19. Med. Sci. Monit. 2020, 26, e928996. [Google Scholar] [CrossRef] [PubMed]
- So, M.K.P.; Chu, A.M.Y.; Tiwari, A. Persistent Symptoms after SARS-CoV-2 Infection: Long-Term Implications for Health and Quality of Life. Lancet Reg. Health Eur. 2022, 17, 100373. [Google Scholar] [CrossRef] [PubMed]
- Malkova, A.; Kudryavtsev, I.; Starshinova, A.; Kudlay, D.; Zinchenko, Y.; Glushkova, A.; Yablonskiy, P.; Shoenfeld, Y. Post COVID-19 Syndrome in Patients with Asymptomatic/Mild Form. Pathogens 2021, 10, 1408. [Google Scholar] [CrossRef] [PubMed]
- Schwendinger, F.; Knaier, R.; Radtke, T.; Schmidt-Trucksäss, A. Low Cardiorespiratory Fitness Post-COVID-19: A Narrative Review. Sport. Med. 2023, 53, 51–74. [Google Scholar] [CrossRef]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS Statement: Guidelines for the Six-Minute Walk Test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- Hansen, H.; Beyer, N.; Frølich, A.; Godtfredsen, N.; Bieler, T. Intra- and Inter-Rater Reproducibility of the 6-Minute Walk Test and the 30-Second Sit-to-Stand Test in Patients with Severe and Very Severe COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 2018, 13, 3447–3457. [Google Scholar] [CrossRef]
- Hernandes, N.A.; Wouters, E.F.M.; Meijer, K.; Annegarn, J.; Pitta, F.; Spruit, M.A. Reproducibility of 6-Minute Walking Test in Patients with COPD. Eur. Respir. J. 2011, 38, 261–267. [Google Scholar] [CrossRef]
- Grosbois, J.M.; Riquier, C.; Chehere, B.; Coquart, J.; Béhal, H.; Bart, F.; Wallaert, B.; Chenivesse, C. Six-Minute Stepper Test: A Valid Clinical Exercise Tolerance Test for COPD Patients. Int. J. Chron. Obstruct. Pulmon. Dis. 2016, 11, 657–663. [Google Scholar] [CrossRef] [PubMed]
- Munari, A.B.; Venâncio, R.S.; Klein, S.R.; Gulart, A.A.; Silva, I.J.C.S.; Sonza, A.; Dal Lago, P.; Mayer, A.F. Physiological Responses to the 6-Min Step Test in Patients with Chronic Obstructive Pulmonary Disease. J. Cardiopulm. Rehabil. Prev. 2020, 40, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Arcuri, J.F.; da Costa, J.N.F.; Gonçalves, L.L.; Davi, S.F.; Pessoa, B.V.; Jamami, M.; Di Lorenzo, V.A.P. Six minute step test reproducibility in COPD patients: Cross-sectional study. Eur. Respir. J. 2013, 42, P3171. [Google Scholar]
- Pessoa, B.V.; Arcuri, J.F.; Labadessa, I.G.; Costa, J.N.F.; Sentanin, A.C.; Di Lorenzo, V.A.P. Validity of the Six-Minute Step Test of Free Cadence in Patients with Chronic Obstructive Pulmonary Disease. Braz. J. Phys. Ther. 2014, 18, 228–236. [Google Scholar] [CrossRef]
- Huespe, I.; Carboni Bisso, I.; Di Stefano, S.; Terrasa, S.; Gemelli, N.A.; Las Heras, M. COVID-19 Severity Index: A Predictive Score for Hospitalized Patients. Med. Intensiv. 2020, 46, 98–101. [Google Scholar] [CrossRef]
- Graham, B.L.; Steenbruggen, I.; Miller, M.R.; Barjaktarevic, I.Z.; Cooper, B.G.; Hall, G.L.; Hallstrand, T.S.; Kaminsky, D.A.; McCarthy, K.; McCormack, M.C.; et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am. J. Respir. Crit. Care Med. 2019, 200, e70–e88. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.R.; Hankinson, J.; Brusasco, V.; Burgos, F.; Casaburi, R.; Coates, A.; Crapo, R.; Enright, P.; van der Grinten, C.P.M.; Gustafsson, P.; et al. ATS/ERS Task Force. Standardisation of Spirometry. Eur. Respir. J. 2005, 26, 319–338. [Google Scholar] [CrossRef]
- da Costa, J.N.; Arcuri, J.F.; Gonçalves, I.L.; Davi, S.F.; Pessoa, B.V.; Jamami, M.; Di Lorenzo, V.A. Reproducibility of Cadence-Free 6-Minute Step Test in Subjects with COPD. Respir. Care 2014, 59, 538–542. [Google Scholar] [CrossRef]
- Finney, L.J.; Doughty, R.; Lovage, S.; Spurr, L.; Mehta, B.; Kemp, S.V.; Chua, F.; Price, L.C.; Singh, S.; Man, W.D.C. Lung Function Deficits and Symptom Burden in Survivors of COVID-19 Requiring Mechanical Ventilation. Ann. Am. Thorac. Soc. 2021, 18, 1740–1743. [Google Scholar] [CrossRef]
- Kovalski, B.S.; Vergel, L.G.; Galhardo, F.D.M.; Marques, S.F.D.; Heidmann, A.M.; Gonçales, E.S.L. Physical Capacity Assessment in Patients Hospitalized with COVID-19 Diagnose. Fisioter. Pesqui. 2022, 29, 216–222. [Google Scholar] [CrossRef]
- Torres-Castro, R.; Vasconcello-Castillo, L.; Alsina-Restoy, X.; Solis-Navarro, L.; Burgos, F.; Puppo, H.; Vilaró, J. Respiratory Function in Patients Post-Infection by COVID-19: A Systematic Review and Meta-Analysis. Pulmonology 2021, 27, 328–337. [Google Scholar] [CrossRef] [PubMed]
- Mo, X.; Jian, W.; Su, Z.; Chen, M.; Peng, H.; Peng, P.; Lei, C.; Chen, R.; Zhong, N.; Li, S. Abnormal Pulmonary Function in COVID-19 Patients at Time of Hospital Discharge. Eur. Respir. J. 2020, 55, 2001217. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Tan, C.; Wu, J.; Chen, M.; Wang, Z.; Luo, L.; Zhou, X.; Liu, X.; Huang, X.; Yuan, S.; et al. Impact of Coronavirus Disease 2019 on Pulmonary Function in Early Convalescence Phase. Respir. Res. 2020, 21, 163. [Google Scholar] [CrossRef]
- Chen, R.; Gao, Y.; Chen, M.; Jian, W.; Lei, C.; Zheng, J.; Li, S. Impaired Pulmonary Function in Discharged Patients with COVID-19: More Work Ahead. Eur. Respir. J. 2020, 56, 2002194. [Google Scholar] [CrossRef] [PubMed]
- Hasan, L.K.; Deadwiler, B.; Haratian, A.; Bolia, I.K.; Weber, A.E.; Petrigliano, F.A. Effects of COVID-19 on the Musculoskeletal System: Clinician’s Guide. Orthop. Res. Rev. 2021, 13, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro Baptista, B.; d’Humières, T.; Schlemmer, F.; Bendib, I.; Justeau, G.; Al-Assaad, L.; Hachem, M.; Codiat, R.; Bardel, B.; Abou Chakra, L.; et al. Identification of Factors Impairing Exercise Capacity after Severe COVID-19 Pulmonary Infection: A 3-Month Follow-up of Prospective COVulnerability Cohort. Respir. Res. 2022, 23, 68. [Google Scholar] [CrossRef]
- Tuttle, C.S.L.; Thang, L.A.N.; Maier, A.B. Markers of Inflammation and Their Association with Muscle Strength and Mass: A Systematic Review and Meta-Analysis. Ageing Res. Rev. 2020, 64, 101185. [Google Scholar] [CrossRef]
- Fernández-de-Las-Peñas, C.; Palacios-Ceña, D.; Gómez-Mayordomo, V.; Palacios-Ceña, M.; Rodríguez-Jiménez, J.; de-la-Llave-Rincón, A.I.; Velasco-Arribas, M.; Fuensalida-Novo, S.; Ambite-Quesada, S.; Guijarro, C.; et al. Fatigue and Dyspnoea as Main Persistent Post-COVID-19 Symptoms in Previously Hospitalized Patients: Related Functional Limitations and Disability. Respiration 2022, 101, 132–141. [Google Scholar] [CrossRef]
- Sperling, S.; Fløe, A.; Leth, S.; Hyldgaard, C.; Gissel, T.; Topcu, A.; Kristensen, L.; Sønderskov, L.D.; Schmid, J.M.; Jensen-Fangel, S.; et al. Fatigue Is a Major Symptom at COVID-19 Hospitalization Follow-Up. J. Clin. Med. 2022, 11, 2411. [Google Scholar] [CrossRef]
- Townsend, A. Autoimmunity to ACE2 as a Possible Cause of Tissue Inflammation in COVID-19. Med. Hypotheses 2020, 144, 110043. [Google Scholar] [CrossRef] [PubMed]
- Bottemanne, H.; Gouraud, C.; Hulot, J.-S.; Blanchard, A.; Ranque, B.; Lahlou-Laforêt, K.; Limosin, F.; Günther, S.; Lebeaux, D.; Lemogne, C. Do Anxiety and Depression Predict Persistent Physical Symptoms after a Severe COVID-19 Episode? A Prospective Study. Front. Psychiatry 2021, 12, 757685. [Google Scholar] [CrossRef] [PubMed]
- Wensink, M.; Schaap, G.; Ten Klooster, P.M.; Doggen, C.J.M.; van der Palen, J.; Vonkeman, H.E.; Bode, C. Physical and mental fatigue in post-COVID syndrome and their associations over time: A small-sample ESM-study to explore fatigue, quality of sleep and behaviours. J. Psychosom. Res. 2023, 164, 111084. [Google Scholar] [CrossRef]
- Mukrikakkada, A.H.; Arnold, G.; Abboud, R.; Wang, W. Correlation Analysis of Oxygen Consumptions between Stepper and Treadmill Movements and Implication for Rehabilitation. Res. Sq. 2020, 2, 1–26. [Google Scholar] [CrossRef]
- Dani, M.; Dirksen, A.; Taraborrelli, P.; Torocastro, M.; Panagopoulos, D.; Sutton, R.; Lim, P.B. Autonomic Dysfunction in “Long COVID”: Rationale, Physiology and Management Strategies. Clin. Med. 2021, 21, e63–e67. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Healthy (N = 33) | Post-COVID-19 (N = 34) | p Value |
|---|---|---|---|
| Gender: | 0.690 | ||
| Female (N%) | 19 (57.6%) | 16 (47.1%) | |
| Male (N%) | 14 (42.4%) | 18 (52.9%) | |
| Age (years) | 34.8 ± 8.85 | 36.3 ± 9.29 | 0.808 |
| Body height (cm) | 166.4 ± 10.6 | 166.6 ± 8.4 | 0.993 |
| Body weight (kg) | 70.8 ± 12.5 | 72.9 ± 13.3 | 0.800 |
| BMI (kg/m2) | 25.5 ± 3.18 | 26.1 ± 3.12 | 0.747 |
| COVID-19 severity: | |||
| Mild (N%) | NA | 23 (67.6%) | - |
| Moderate (N%) | NA | 11 (32.4%) | - |
| PCFS (score): | |||
| Grade 0 (N%) | NA | 15 (44.1%) | - |
| Grade 1 (N%) | NA | 12 (35.3%) | - |
| Grade 2 (N%) | NA | 7 (20.6%) | - |
| Grade 3–4 (N%) | NA | 0 (0%) | - |
| Pulmonary Functional Test: | |||
| FEV1 (L) | 3.21 ± 0.761 | 2.81 ± 0.655 | 0.080 |
| FVC (L) | 3.91 ± 0.950 | 3.42 ± 0.858 | 0.094 |
| FEV1/FVC (%) | 82.3 ± 5.72 | 83.5 ± 10.0 | 0.849 |
| PEF (L/S) | 6.58 ± 1.95 | 5.81 ± 1.75 | 0.236 |
| Variables | Healthy (N = 33) (Mean ± SD) | Post-COVID-19 (N = 34) (Mean ± SD) | Mean Difference ± S.E | p-Value |
|---|---|---|---|---|
| 6MST: | ||||
| Number of steps | 156 ± 31.7 | 121 ± 35.6 | 34.6 ± 8.2 | <0.001 * |
| Post-HR | 114.2 ± 16.1 | 121.4 ± 12.1 | −7.2 ± 3.5 | 0.042 * |
| Post-RR | 24.4 ± 2.3 | 27.8 ± 1.9 | −3.4 ± 0.5 | <0.001 * |
| Post-SpO2 | 98.5 ± 0.9 | 98.2 ± 0.8 | 0.2 ± 0.2 | 0.239 |
| Post-Systolic BP | 139 ± 11.5 | 144.4 ± 10.1 | −5.4 ± 2.6 | 0.046 * |
| Post-Diastolic BP | 81.7 ± 8.4 | 86.1 ± 9.4 | −4.4 ± 2.2 | 0.048 * |
| Borg scale (dyspnea) | 0.061 ± 0.24 | 0.62 ± 0.7 | −0.557 ± 0.13 | <0.001 * |
| Borg scale (fatigue) | 2.12 ± 1.2 | 3.44 ± 1.6 | −1.32 ± 0.35 | <0.001 * |
| 6MWT: | ||||
| Distance (m) | 518 ± 90 | 423 ± 68 | 94.1 ± 19.4 | <0.001 * |
| Post-HR | 98.0 ± 13.1 | 104 ± 10.3 | −5.9 ± 2.9 | 0.043 * |
| Post-RR | 22 ± 2 | 24.4 ± 1.9 | −2.4 ± 0.5 | <0.001 * |
| Post-SpO2 | 98.7 ± 0.8 | 98.5 ± 0.9 | 0.2 ± 0.2 | 0.272 |
| Post-Systolic BP | 126.7 ± 14.5 | 127.5 ± 9.4 | −0.7 ± 3 | 0.805 |
| Post-Diastolic BP | 79.8 ± 6.9 | 82.4 ± 10.4 | −2.6 ± 2.1 | 0.238 |
| Borg scale (dyspnea) | 0 ± 0 | 0.235 ± 0.55 | −0.24 ± 0.1 | 0.017 * |
| Borg scale (fatigue) | 0.76 ± 0.83 | 1.35 ± 1.2 | −0.59 ± 0.25 | 0.022 * |
| Correlation between: | Healthy (N = 33) | Post-COVID 19 (N = 34) | ||
|---|---|---|---|---|
| r | p Value | r | p Value | |
| (6MWT distance vs. 6MST steps) | r = 0.360 95% CI 0.019 to 0.626 | 0.039 * | r = 0.552 95% CI 0.262 to 0.750 | 0.001 * |
| Post-HR of 6MWT vs. post-HR of 6MST | r = 0.606 95% CI 0.331 to 0.786 | <0.001 * | r = 0.051 95% CI −0.292 to 0.382 | 0.776 |
| Post-RR of 6MWT vs. post-RR of 6MST | r = 0.549 95% CI 0.253 to 0.751 | 0.001 * | r = 0.129 95% CI −0.219 to 0.447 | 0.468 |
| Post-SpO2 of 6MWT vs. post-SpO2 of 6MST | r = 0.539 95% CI 0.240 to 0.745 | 0.001 * | r = 0.228 95% CI −0.119 to 0.526 | 0.194 |
| Post-SBP of 6MWT vs. post-SBP of 6MST | r = 0.647 95% CI 0.391 to 0.810 | <0.001 * | r = 0.628 95% CI 0.368 to 0.797 | <0.001 * |
| Post-DBP of 6MWT vs. post-DBP of 6MST | r = 0.558 95% CI 0.266 to 0.757 | 0.001 * | r = 0.832 95% CI 0.688 to 0.913 | <0.001 * |
| Borg (dyspnea) of 6MWT vs. dyspnea of 6MST | - | - | r = 0.633 95% CI 0.375 to 0.800 | <0.001 * |
| Borg (fatigue) of 6MWT vs. fatigue of 6MST | r = 0.63 95% CI 0.366 to 0.800 | <0.001 * | r = 0.547 95% CI 0.256 to 0.747 | 0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Omar, A.; Ferreira, A.d.S.; Hegazy, F.A.; Alaparthi, G.K. Cardiorespiratory Response to Six-Minute Step Test in Post COVID-19 Patients—A Cross Sectional Study. Healthcare 2023, 11, 1386. https://doi.org/10.3390/healthcare11101386
Omar A, Ferreira AdS, Hegazy FA, Alaparthi GK. Cardiorespiratory Response to Six-Minute Step Test in Post COVID-19 Patients—A Cross Sectional Study. Healthcare. 2023; 11(10):1386. https://doi.org/10.3390/healthcare11101386
Chicago/Turabian StyleOmar, Amna, Arthur de Sá Ferreira, Fatma A. Hegazy, and Gopala Krishna Alaparthi. 2023. "Cardiorespiratory Response to Six-Minute Step Test in Post COVID-19 Patients—A Cross Sectional Study" Healthcare 11, no. 10: 1386. https://doi.org/10.3390/healthcare11101386
APA StyleOmar, A., Ferreira, A. d. S., Hegazy, F. A., & Alaparthi, G. K. (2023). Cardiorespiratory Response to Six-Minute Step Test in Post COVID-19 Patients—A Cross Sectional Study. Healthcare, 11(10), 1386. https://doi.org/10.3390/healthcare11101386







