Current Healthcare Systems in Light of Hyperendemic NCDs and the COVID-19 Pandemic: Time to Change
Abstract
1. Introduction
2. The Bright Side of Current Healthcare Systems
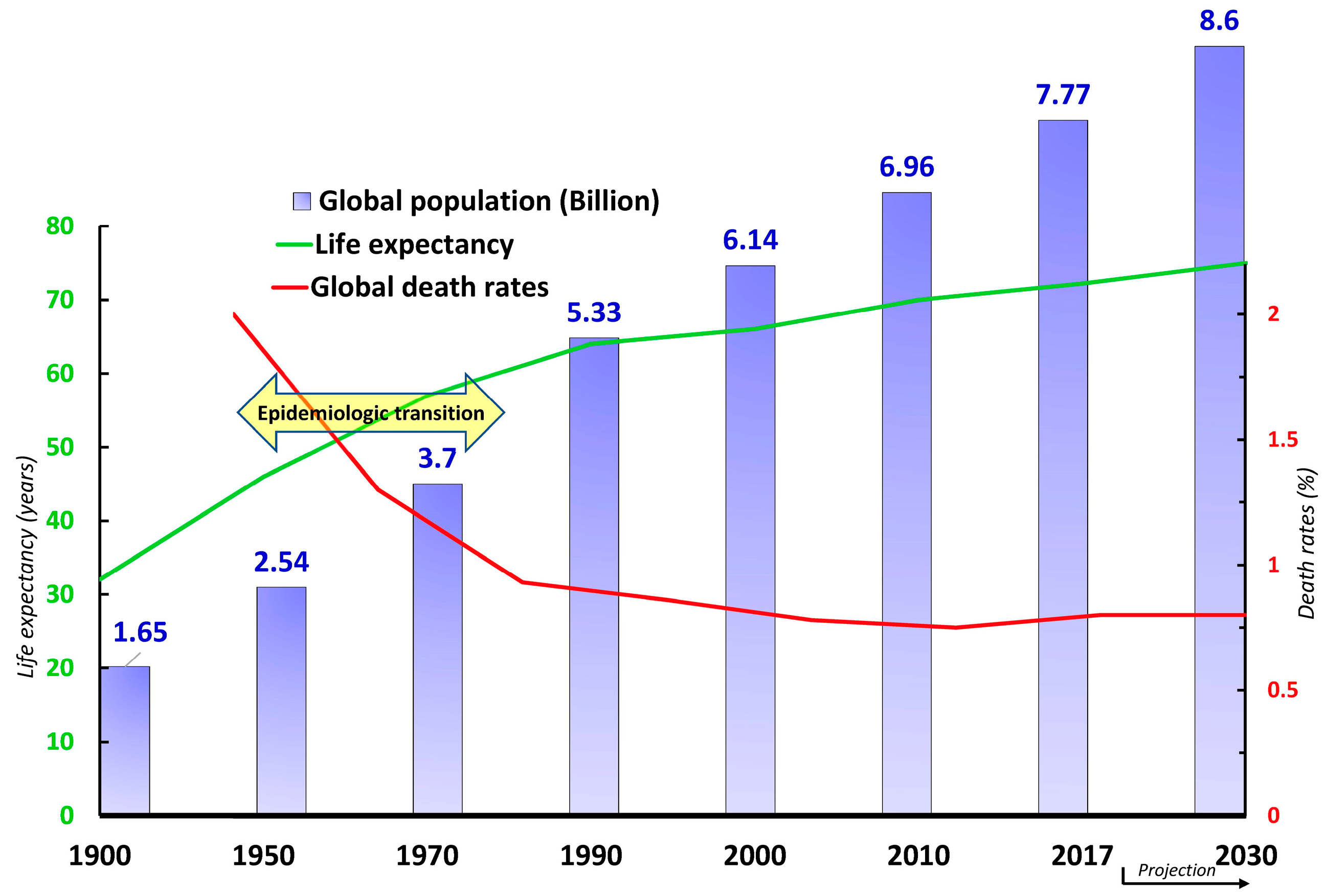
3. Epidemiologic Transition and the Emergence of Healthcare Challenges
4. The Invisible Hyperendemic NCDs
5. The Fragmented “Illness Care” System
6. Healthcare Commodification
7. Skyrocketing Healthcare Expenditure
8. Unfilled Quality Gap
9. CHCS Shortcomings in Response to the COVID-19 Pandemic
10. Additional Challenges of CHCSs
11. The Promise of Health-Determinant-Oriented Care
12. Conclusion and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Duffy, T.P. The Flexner report―100 years later. Yale J. Biol. Med. 2011, 84, 269. [Google Scholar] [PubMed]
- Flexner, A. Medical education in the United States and Canada. Bull. World Health Organ. 2002, 80, 594–602. [Google Scholar] [CrossRef] [PubMed]
- Nightingale, F. Notes on Hospitals; Longman, Green, Longman, Roberts, and Green: London, UK, 1863. [Google Scholar]
- Pasteur, L.; Chamberland, R. Summary report of the experiments conducted at Pouilly-le-Fort, near Melun, on the anthrax vaccination, 1881. Yale J. Biol. Med. 2002, 75, 59. [Google Scholar] [PubMed]
- Oedingen, C.; Staerk, J.W. First cure for diphtheria by antitoxin as early as 1891. Ann. Sci. 1997, 54, 607–610. [Google Scholar] [CrossRef]
- Strebhardt, K.; Ullrich, A. Paul Ehrlich’s magic bullet concept: 100 years of progress. Nat. Rev. Cancer 2008, 8, 473–480. [Google Scholar] [CrossRef]
- Kauffman, G.B. The discovery of penicillin: Twentieth century wonder drug. J. Chem. Educ. 1979, 56, 454. [Google Scholar] [CrossRef]
- Aminov, R.I. A brief history of the antibiotic era: Lessons learned and challenges for the future. Front. Microbiol. 2010, 1, 134. [Google Scholar] [CrossRef]
- Oates, S.B. Woman of Valor: Clara Barton and the Civil War; Simon and Schuster: New York, NY, USA, 1995. [Google Scholar]
- Cavaillon, J.-M.; Legout, S. Duclaux, Chamberland, Roux, Grancher, and Metchnikoff: The five musketeers of Louis Pasteur. Microbes Infect. 2019, 21, 192–201. [Google Scholar] [CrossRef]
- Sheingold, B.H.; Hahn, J.A. The history of healthcare quality: The first 100 years 1860–1960. Int. J. Afr. Nurs. Sci. 2014, 1, 18–22. [Google Scholar] [CrossRef]
- Evens, R.; Kaitin, K. The Evolution Of Biotechnology And Its Impact On Health Care. Health Aff. 2015, 34, 210–219. [Google Scholar] [CrossRef]
- Chew, M.; Sharrock, K. Medical Milestones: Celebrating Key Advances Since 1840; British Medical Association: London, UK, 2007. [Google Scholar]
- WHO. Vaccines and Immunization. Available online: https://www.who.int/health-topics/vaccines-and-immunization#tab=tab_1 (accessed on 17 April 2023).
- Adedeji, W. The treasure called antibiotics. Ann. Ib. Postgrad. Med. 2016, 14, 56. [Google Scholar]
- Bigelow, H.J. Insensibility During Surgical Operations Produced by Inhalation; Classics of Medicine Library: Boston, MA, USA, 1846. [Google Scholar]
- Lister, J. Antiseptic principle in the practice of surgery. Br. Med. J. 1967, 2, 9. [Google Scholar] [CrossRef]
- Röntgen, W.C. Discovery of X-rays. In A Century of X-Rays and Radioactivity in Medicine; CRC Press: Boca Raton, FL, USA, 2018; pp. 1–9. [Google Scholar]
- Feinstein, A.R. Clinical epidemiology: I. The populational experiments of nature and of man in human illness. Ann. Intern. Med. 1968, 69, 807–820. [Google Scholar] [CrossRef]
- Concato, J.; Shah, N.; Horwitz, R.I. Randomized, controlled trials, observational studies, and the hierarchy of research designs. New Engl. J. Med. 2000, 342, 1887–1892. [Google Scholar] [CrossRef]
- Omran, A.R. The epidemiologic transition theory revisited thirty years later. World Health Stat. Q. 1998, 53, 99–119. [Google Scholar]
- Mackenbach, J.P. The epidemiologic transition theory. J. Epidemiol. Community Health 1994, 48, 329–331. [Google Scholar] [CrossRef]
- Wahdan, M.H. The epidemiological transition. EMHJ-East. Mediterr. Health J. 1996, 2, 8–20. [Google Scholar] [CrossRef]
- Assidi, M.; Buhmeida, A.; Budowle, B. Medicine and health of 21st Century: Not just a high biotech-driven solution. npj Genom. Med. 2022, 7, 67. [Google Scholar] [CrossRef]
- World Health Organization. Health Inequities and Their Causes; World Health Organisation: Geneva, Switzerland, 2018; Available online: https://www.who.int/news-room/facts-in-pictures/detail/health-inequities-and-their-causes (accessed on 5 February 2023).
- HELEN. He Reference for HELEN is: Health Equity Leadership & Exchange Network (HELEN). Available online: https://www.nationalcollaborative.org/our-programs/health-equity-leadership-exchange-network-helen/ (accessed on 13 April 2023).
- McCartney, G.; Popham, F.; McMaster, R.; Cumbers, A. Defining health and health inequalities. Public Health 2019, 172, 22–30. [Google Scholar] [CrossRef]
- Baciu, A.; Negussie, Y.; Geller, A.; Weinstein, J.N.; National Academies of Sciences, Engineering, and Medicine. The state of health disparities in the United States. In Communities in Action: Pathways to Health Equity; National Academies Press: Washington, DC, USA, 2017. [Google Scholar]
- Roser, M.; Ortiz-Ospina, E.; Ritchie, H. Life Expectancy. Available online: https://ourworldindata.org/life-expectancy (accessed on 20 June 2021).
- United Nations—Department of Economic and Social Affair—Population Division. World Population Prospects: The 2017 Revision, DVD Edition. Available online: https://ourworldindata.org/grapher/crude-death-rate-the-share-of-the-population-that-dies-per-year (accessed on 7 June 2020).
- Office of Disease, P.; Health, P. US Department of Health and Human Services: Healthy People 2010. Available online: http://www/health/gov/healthypeople/ (accessed on 5 May 2021).
- Naghavi, M.; Abajobir, A.A.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Adetokunboh, O.; Afshin, A.; Agrawal, A. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1151–1210. [Google Scholar] [CrossRef]
- Ritchie, H. Causes of Death. Available online: https://ourworldindata.org/causes-of-death (accessed on 10 December 2021).
- Bloom, D.E.; Cafiero, E.; Jané-Llopis, E.; Abrahams-Gessel, S.; Bloom, L.R.; Fathima, S.; Feigl, A.B.; Gaziano, T.; Hamandi, A.; Mowafi, M. The Global Economic Burden of Noncommunicable Diseases; Program on the Global Demography of Aging: Cambridge, MA, USA, 2012. [Google Scholar]
- European Commission. Knowledge for Policy: Noncommunicable Diseases—NCDs. Available online: https://ec.europa.eu/knowledge4policy/foresight/topic/shifting-health-challenges/non-communicable-diseases-ncds_en (accessed on 20 July 2020).
- Clark, J. Medicalization of global health 3: The medicalization of the non-communicable diseases agenda. Glob. Health Action 2014, 7, 24002. [Google Scholar] [CrossRef] [PubMed]
- Monaco, A.; Palmer, K.; Marengoni, A.; Maggi, S.; Hassan, T.A.; Donde, S. Integrated care for the management of ageing-related non-communicable diseases: Current gaps and future directions. Aging Clin. Exp. Res. 2020, 32, 1353–1358. [Google Scholar] [CrossRef] [PubMed]
- Fani Marvasti, F.; Stafford, R.S. From sick care to health care—Reengineering prevention into the U.S. system. New Engl. J. Med. 2012, 367, 889–891. [Google Scholar] [CrossRef] [PubMed]
- Mills, D.A. Chronic disease: The epidemic of the twentieth century. Maine Policy Rev. 2000, 9, 50–65. [Google Scholar]
- WHO Europe. Better Non-Communicable Disease Outcomes: Challenges and Opportunities for Health Systems; WHO Europe: Geneva, Switzerland, 2014. [Google Scholar]
- Allen, L. Are we facing a noncommunicable disease pandemic? J. Epidemiol. Glob. Health 2017, 7, 5–9. [Google Scholar] [CrossRef]
- Stuckler, D.; Siegel, K.; Kishore, S.; Duffany, K.O.C.; Stevens, D.; Basu, S. Comprehensive strategies to reduce the burden of chronic diseases. Management 2011, 2, 1. [Google Scholar]
- Leitzmann, M.F.; Jochem, C.; Schmid, D. Sedentary Behaviour Epidemiology; Springer: Berlin/Heidelberg, Germany, 2017. [Google Scholar]
- Karavasiloglou, N.; Pannen, S.T.; Jochem, C.; Kuhn, T.; Rohrmann, S. Sustainable Diets and Cancer: A Systematic Review. Curr. Nutr. Rep. 2022, 11, 742–752. [Google Scholar] [CrossRef]
- Albreht, T.; Dyakova, M.; Schellevis, F.G.; Van den Broucke, S. Many diseases, one model of care? J. Comorbidity 2016, 6, 12–20. [Google Scholar] [CrossRef]
- Henderson, D.A. The eradication of smallpox—An overview of the past, present, and future. Vaccine 2011, 29, D7–D9. [Google Scholar] [CrossRef]
- Larson, H.J.; Ghinai, I. Lessons from polio eradication. Nature 2011, 473, 446–447. [Google Scholar] [CrossRef]
- Fries, J.F. Aging, natural death, and the compression of morbidity. N. Engl. J. Med. 1980, 303, 130–135. [Google Scholar] [CrossRef]
- Mor, V. The compression of morbidity hypothesis: A review of research and prospects for the future. J. Am. Geriatr. Soc. 2005, 53, S308–S309. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Vos, T.; Lozano, R.; Naghavi, M.; Flaxman, A.D.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2197–2223. [Google Scholar] [CrossRef]
- Clark, J. Do the solutions for global health lie in healthcare? BMJ 2014, 349, g5457. [Google Scholar] [CrossRef]
- Pizzorno, J.; Stephenson, S. Health Care System and Addressing the Determinants of Health. Integr. Med. 2017, 16, 16–18. [Google Scholar]
- Duran, A.; Kutzin, J. Financing of public health services and programmes: Time to look into the black box. In Implementing Health Financing Reform; Observatory Studies Series No. 21; European Observatory on Health Systems and Policies: Brussels, Belgium, 2010; ISBN 978 92 890 4211 6. Available online: https://www.researchgate.net/profile/Dina-Balabanova-2/publication/48909782_What_role_for_voluntary_health_insurance/links/0a85e532acc2225454000000/What-role-for-voluntary-health-insurance.pdf#page=262, (accessed on 5 May 2022).
- Edmondson, A.C.; Nembhard, I.M. Product development and learning in project teams: The challenges are the benefits. J. Prod. Innov. Manag. 2009, 26, 123–138. [Google Scholar] [CrossRef]
- Donini-Lenhoff, F.G.; Hedrick, H.L. Increasing awareness and implementation of cultural competence principles in health professions education. J. Allied Health 2000, 29, 241–245. [Google Scholar]
- Mann, L. From “silos” to seamless healthcare: Bringing hospitals and GPs back together again. Med. J. Aust. 2005, 182, 34–37. [Google Scholar] [CrossRef]
- Hajek, A.M. Breaking down clinical silos in healthcare. Front. Health Serv. Manag. 2013, 29, 45–50. [Google Scholar] [CrossRef]
- Elhauge, E. The Fragmentation of US Health Care: Causes and Solutions; Oxford University Press on Demand: Oxford, UK, 2010. [Google Scholar]
- Harper, P.R.; Shahani, A. Modelling for the planning and management of bed capacities in hospitals. J. Oper. Res. Soc. 2002, 53, 11–18. [Google Scholar] [CrossRef]
- Chokshi, D.A.; Farley, T.A. Changing behaviors to prevent noncommunicable diseases. Science 2014, 345, 1243. [Google Scholar] [CrossRef] [PubMed]
- Carlson, R.J. Holism and reductionism as perspectives in medicine and patient care. West. J. Med. 1979, 131, 466–470. [Google Scholar] [PubMed]
- Lysaght, M. ‘Your Wealth is your Health’: A Study of the Commodification of Health Services in Ireland. In Critical Social Thinking: Policy and Practice; Dept. of Applied Social Studies, University College Cork: Cork, Ireland, 2009; Volume 1, Available online: https://www.ucc.ie/en/appsoc/resconf/conf/cst/vol1/health/MargaretLysaght.pdf (accessed on 20 March 2021).
- Baudrillard, J. The Consumer Society: Myths and Structures; Sage: Newcastle upon Tyne, UK, 2016. [Google Scholar]
- Pellegrino, E.D. The commodification of medical and health care: The moral consequences of a paradigm shift from a professional to a market ethic. J. Med. Philos. 1999, 24, 243–266. [Google Scholar] [CrossRef] [PubMed]
- Lown, B. The commodification of health care. Physicians A National Health Program. 2007. Available online: http://www.pnhp.org/publications/the_commodification_of_health_care.php?page=all (accessed on 17 April 2021).
- Christiansen, I. Commodification of healthcare and its consequences. World Rev. Political Econ. 2017, 8, 82–103. [Google Scholar] [CrossRef]
- Institute of Medicine Committee on Preventing the Global Epidemic of Cardiovascular Disease: Meeting the Challenges in Developing, C. The National Academies Collection: Reports funded by National Institutes of Health. In Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health; Fuster, V., Kelly, B.B., Eds.; National Academies Press: Washington, DC, USA, 2010. [Google Scholar]
- Butler, D. Agency gets a grip on budget: Reforms increase flexibility and shift spending towards non-communicable disorders. Nature 2013, 498, 18–20. [Google Scholar]
- Deas, T.M., Jr. Health care value-based purchasing. Gastrointest. Endosc. Clin. N. Am. 2006, 16, 643–656. [Google Scholar] [CrossRef]
- Orszag, P.R. Health Care and the Budget: Issues and Challenges for Reform; CBO Testimony Before the Committee on the Budget, United States Senate, Ed.; Congressional Budget Office: Washington, DC, USA, 2007. [Google Scholar]
- Callahan, D. Health care costs and medical technology. In From Birth to Death and Bench to Clinic: The Hastings Center Bioethics Briefing Book for Journalists, Policymakers, and Campaigns; The Hastings Center: Garrison, NY, USA, 2008; pp. 79–82. Available online: https://www.thehastingscenter.org/briefingbook/health-care-costs-and-medical-technology/ (accessed on 10 February 2022).
- Michelson, K. Trust: Can it exist in today’s healthcare system? Pediatr. Crit. Care Med. 2010, 11, 432–433. [Google Scholar] [CrossRef]
- Guharoy, R. Time to stop skyrocketing drug costs. Am. J. Health-Syst. Pharm. 2018, 75, 91–92. [Google Scholar] [CrossRef]
- Hicks, L.K.; O’Brien, P.; Sholzberg, M.; Veloce, N.; Trafford, A.; Sinclair, D. Tackling overutilization of hospital tests and treatments: Lessons learned from a grassroots approach. Healthc. Manag. Forum 2018, 31, 186–190. [Google Scholar] [CrossRef]
- Chan, B.; Cochrane, D. What can be done to improve patient safety? In Measuring Patient Harm in Canadian Hospitals; CIHI: Toronto, ON, Canada; Ottawa, ON, Canada, 2016. [Google Scholar]
- Canadian Institute for Health Information. Unnecessary Care in Canada; CIHI: Toronto, ON, Canada; Ottawa, ON, Canada, 2017. [Google Scholar]
- Gapanenko, K.; Lam, D.; Parker, M.; D’Silva, J.; Johnson, T. Unnecessary Care in Canada. Healthc. Q. 2017, 20, 10. [Google Scholar] [CrossRef]
- Makary, M.A.; Daniel, M. Medical error—The third leading cause of death in the US. BMJ 2016, 353, i2139. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century; National Academies Press: Washington, DC, USA, 2001. [Google Scholar]
- World Health Organization. Declaration of Alma-Ata: International Conference on Primary Health Care, Alma-Ata, USSR, 6–12 September 1978. Retrieved Febr. 1978, 14, 2006. [Google Scholar]
- Donaldson, M.S.; Corrigan, J.M.; Kohn, L.T. To Err is Human: Building a Safer Health System; National Academies Press: Washington, DC, USA, 2000; Volume 6. [Google Scholar]
- Epping-Jordan, J.E.; Pruitt, S.D.; Bengoa, R.; Wagner, E.H. Improving the quality of health care for chronic conditions. Qual. Saf. Health Care 2004, 13, 299. [Google Scholar] [CrossRef]
- Fonarow, G.C. Unintended harm associated with the hospital readmissions reduction program. JAMA J. Am. Med. Assoc. 2018, 320, 2539–2541. [Google Scholar] [CrossRef]
- Bulger, J.; Nickel, W.; Messler, J.; Goldstein, J.; O’Callaghan, J.; Auron, M.; Gulati, M. Choosing wisely in adult hospital medicine: Five opportunities for improved healthcare value. J. Hosp. Med. 2013, 8, 486–492. [Google Scholar] [CrossRef]
- Gandhi, T.K.; Feeley, D.; Schummers, D. Zero Harm in Health Care. NEJM Catal. Innov. Care Deliv. 2020, 1. [Google Scholar] [CrossRef]
- Fernandopulle, R.; Ferris, T.; Epstein, A.; McNeil, B.; Newhouse, J.; Pisano, G.; Blumenthal, D. A research agenda for bridging the ‘quality chasm’. Health Aff. 2003, 22, 178–190. [Google Scholar] [CrossRef]
- World Health Organization. Improving Healthcare Quality in Europe: Characteristics, Effectiveness and Implementation of Different Strategies; World Health Organization. Regional Office for Europe: Geneva, Switzerland, 2019. [Google Scholar]
- McGinnis, J.M.; Williams-Russo, P.; Knickman, J.R. The case for more active policy attention to health promotion. Health Aff. 2002, 21, 78–93. Available online: https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.21.2.78 (accessed on 11 February 2021). [CrossRef]
- WHO. WHO COVID-19 Dashboard; World Health Organization: Geneva, Switzerland, 2023; Available online: https://covid19.who.int/ (accessed on 5 April 2023).
- Hebbar, P.B.; Sudha, A.; Dsouza, V.; Chilgod, L.; Amin, A. Healthcare delivery in India amid the COVID-19 pandemic: Challenges and opportunities. Indian J. Med. Ethics 2020. ahead of print. [Google Scholar] [CrossRef]
- Bansal, P.; Bingemann, T.A.; Greenhawt, M.; Mosnaim, G.; Nanda, A.; Oppenheimer, J.; Sharma, H.; Stukus, D.; Shaker, M. Clinician wellness during the COVID-19 pandemic: Extraordinary times and unusual challenges for the allergist/immunologist. J. Allergy Clin. Immunol. Pract. 2020, 8, 1781–1790.e3. [Google Scholar] [CrossRef]
- Dorsett, M. Point of no return: COVID-19 and the U.S. healthcare system: An emergency physician’s perspective. Sci. Adv. 2020, 6, eabc5354. [Google Scholar] [CrossRef] [PubMed]
- Miller, G. Social Distancing Prevents Infections, but it Can Have Unintended Consequences, Science Magazine, 20 March 2020. Available online: https://www.science.org/content/article/we-are-social-species-how-will-social-distancing-affect-us (accessed on 30 March 2021).
- Cohen, J. Pandemic vaccines are about to face the real test. Science 2020, 368, 1295–1296. [Google Scholar] [CrossRef] [PubMed]
- Contandriopoulos, D.; Brousselle, A. Reliable in their failure: An analysis of healthcare reform policies in public systems. Health Policy 2010, 95, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Cundiff, D.; McCarthy, M.E. The Right Medicine How to Make Health Care Reform Work Today; Humana Press: Totowa, NJ, USA, 1994. [Google Scholar]
- Cell Editorial Team. Embracing the Landscape of Therapeutics. Cell 2020, 181, 1–3. [Google Scholar] [CrossRef]
- McGovern, L.; Miller, G.; Hughes-Cromwick, P. Health Policy Briefs: The Relative Contribution of Multiple Determinants to Health, Health Affairs, 21 August 2014. Available online: https://www.healthaffairs.org/do/10.1377/hpb20140821.404487/ (accessed on 6 February 2023).
- McGinnis, J.M.; Foege, W.H. Actual Causes of Death in the United States. JAMA J. Am. Med. Assoc. 1993, 270, 2207–2212. [Google Scholar] [CrossRef]
- Lantz, P.M.; House, J.S.; Lepkowski, J.M.; Williams, D.R.; Mero, R.P.; Chen, J. Socioeconomic factors, health behaviors, and mortality: Results from a nationally representative prospective study of US adults. JAMA J. Am. Med. Assoc. 1998, 279, 1703–1708. [Google Scholar] [CrossRef]
- Mokdad, A.H.; Marks, J.S.; Stroup, D.F.; Gerberding, J.L. Actual causes of death in the United States, 2000. JAMA J. Am. Med. Assoc. 2004, 291, 1238–1245. [Google Scholar] [CrossRef]
- Danaei, G.; Ding, E.L.; Mozaffarian, D.; Taylor, B.; Rehm, J.; Murray, C.J.; Ezzati, M. The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009, 6, e1000058. [Google Scholar] [CrossRef]
- World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks; WHO: Geneva, Switzerland, 2009; Available online: https://apps.who.int/iris/handle/10665/44203 (accessed on 12 May 2021).
- Booske, B.C.; Athens, J.K.; Kindig, D.A.; Park, H.; Remington, P.L. Different Perspectives for Assigning Weights to Determinants of Health; Population Health Institute, University of Wisconsin: Madison, WI, USA, 2010; Available online: https://www.countyhealthrankings.org/sites/default/files/differentPerspectivesForAssigningWeightsToDeterminantsOfHealth.pdf (accessed on 31 October 2021).
- Stringhini, S.; Sabia, S.; Shipley, M.; Brunner, E.; Nabi, H.; Kivimaki, M.; Singh-Manoux, A. Association of socioeconomic position with health behaviors and mortality. JAMA J. Am. Med. Assoc. 2010, 303, 1159–1166. [Google Scholar] [CrossRef]
- Thoits, P.A. Stress and health: Major findings and policy implications. J. Health Soc. Behav. 2010, 51, S41–S53. [Google Scholar] [CrossRef]
- Schroeder, S.A. We can do better—Improving the health of the American people. N. Engl. J. Med. 2007, 357, 1221–1228. [Google Scholar] [CrossRef]
- Ansari, Z.; Carson, N.J.; Ackland, M.J.; Vaughan, L.; Serraglio, A. A public health model of the social determinants of health. Soz.-Und Prav. 2003, 48, 242–251. [Google Scholar] [CrossRef]
- Choi, E.; Sonin, J. Determinants of Health. Available online: https://www.goinvo.com/vision/determinants-of-health/ (accessed on 18 April 2020).
- Pellmar, T.C.; Brandt, E.N., Jr.; Baird, M.A. Health and behavior: The interplay of biological, behavioral, and social influences: Summary of an Institute of Medicine report. Am. J. Health Promot. 2002, 16, 206–219. [Google Scholar] [CrossRef]
- WHO. Chapter 4: More Health for the Money; World Health Organization: Geneva, Switzerland, 2010. Available online: https://www.moph.gov.lb/userfiles/files/Publications/HealthReformInLebanon/Chap4(lebanonBox4_2).pdf (accessed on 20 July 2020).
- Beaglehole, R.; Bonita, R.; Horton, R.; Adams, C.; Alleyne, G.; Asaria, P.; Baugh, V.; Bekedam, H.; Billo, N.; Casswell, S.; et al. Priority actions for the non-communicable disease crisis. Lancet 2011, 377, 1438–1447. [Google Scholar] [CrossRef]
- NCD Alliance. Shaping the Health Systems of the Future: Case Studies and Recommendations for Integrated NCD Care; NCD Alliance: Geneva, Switzerland, 2018; Available online: https://ncdalliance.org/sites/default/files/resource_files/ShapingTheHealthSystemsOfTheFuture_FINAL_WEB_0.pdf (accessed on 6 May 2020).
- Rathbone, A.L.; Prescott, J. The Use of Mobile Apps and SMS Messaging as Physical and Mental Health Interventions: Systematic Review. J. Med. Internet Res. 2017, 19, e295. [Google Scholar] [CrossRef]
- Ahmad, S.S.; Khan, S.; Kamal, M.A. What is Blockchain Technology and its Significance in the Current Healthcare System? A Brief Insight. Curr. Pharm. Des. 2019, 25, 1402–1408. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buhmeida, A.; Assidi, M.; Budowle, B. Current Healthcare Systems in Light of Hyperendemic NCDs and the COVID-19 Pandemic: Time to Change. Healthcare 2023, 11, 1382. https://doi.org/10.3390/healthcare11101382
Buhmeida A, Assidi M, Budowle B. Current Healthcare Systems in Light of Hyperendemic NCDs and the COVID-19 Pandemic: Time to Change. Healthcare. 2023; 11(10):1382. https://doi.org/10.3390/healthcare11101382
Chicago/Turabian StyleBuhmeida, Abdelbaset, Mourad Assidi, and Bruce Budowle. 2023. "Current Healthcare Systems in Light of Hyperendemic NCDs and the COVID-19 Pandemic: Time to Change" Healthcare 11, no. 10: 1382. https://doi.org/10.3390/healthcare11101382
APA StyleBuhmeida, A., Assidi, M., & Budowle, B. (2023). Current Healthcare Systems in Light of Hyperendemic NCDs and the COVID-19 Pandemic: Time to Change. Healthcare, 11(10), 1382. https://doi.org/10.3390/healthcare11101382







