Mental Health in Coronary Heart Disease (CHD) Patients: Findings from the UK Household Longitudinal Study (UKHLS)
Abstract
1. Introduction
2. Methods
2.1. Data
2.2. Measures
2.2.1. CHD
2.2.2. Mental Health
2.2.3. Demographic Variables
2.3. Analysis
2.3.1. Factor Model
2.3.2. Linear Models
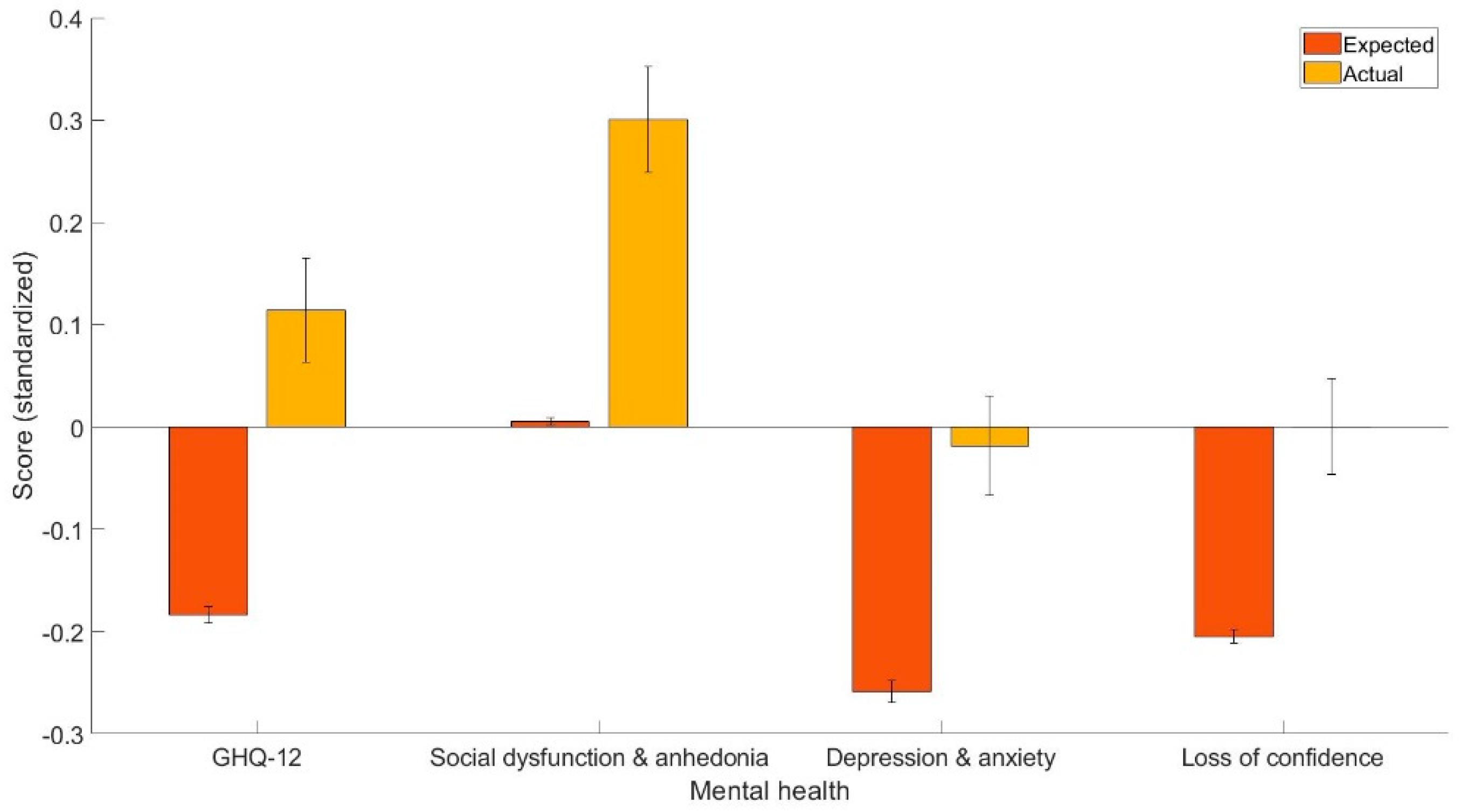
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, H.; Naghavi, M.; Allen, C.; Barber, R.M.; Bhutta, Z.A.; Carter, A.; Li, Y.; Wang, L.; Liu, Y.; Yin, P.; et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1459–1544. [Google Scholar] [CrossRef] [PubMed]
- Hanna, I.R.; Wenger, N.K. Secondary prevention of coronary heart disease in elderly patients. Am. Fam. Physician 2005, 71, 2289–2296. [Google Scholar]
- Chaddha, A.; Robinson, E.A.; Kline-Rogers, E.; Alexandris-Souphis, T.; Rubenfire, M. Mental health and cardiovascular disease. Am. J. Med. 2016, 129, 1145–1148. [Google Scholar] [CrossRef] [PubMed]
- Gostoli, S.; Buzzichelli, S.; Guidi, J.; Sirri, L.; Marzola, E.; Roncuzzi, R.; Abbate-Daga, G.; Fava, G.A.; Rafanelli, C. An innovative approach to the assessment of mood disturbances in patients with acute coronary syndrome. CNS Spectr. 2023, 28, 78–89. [Google Scholar] [CrossRef]
- Vaccarino, V.; Badimon, L.; Bremner, J.D.; Cenko, E.; Cubedo, J.; Dorobantu, M.; Duncker, D.J.; Koller, A.; Manfrini, O.; Milicic, D.; et al. Depression and coronary heart disease: 2018 position paper of the ESC working group on coronary pathophysiology and microcirculation. Eur. Heart J. 2019, 41, 1687–1696. [Google Scholar] [CrossRef]
- Bashiri, Z.; Aghajani, M.; Alavi, N.M. Effects of psychoeducation on mental health in patients with coronary heart disease. Iran. Red Crescent Med. J. 2016, 18, e25089. [Google Scholar] [CrossRef] [PubMed]
- Ono, M.; Serruys, P.W.; Garg, S.; Kawashima, H.; Gao, C.; Hara, H.; Lunardi, M.; Wang, R.; O’leary, N.; Wykrzykowska, J.J.; et al. Effect of patient-reported preprocedural physical and mental health on 10-year mortality after percutaneous or surgical coronary revascularization. Circulation 2022, 146, 1268–1280. [Google Scholar] [CrossRef] [PubMed]
- Mayer, O., Jr.; Bruthans, J.; Seidlerová, J.; Karnosová, P.; Mateřánková, M.; Gelžinský, J.; Rychecká, M.; Cífková, R.; Filipovský, J. Mood disorders impaired quality of life but not the mortality or morbidity risk in stable coronary heart disease patients. Acta Cardiol. 2020, 75, 667–675. [Google Scholar] [CrossRef]
- Fan, Y.; Ho, M.R.; Shen, B. Loneliness predicts physical and mental health-related quality of life over 9 months among patients with coronary heart disease. Appl. Psychol. Health Well Being 2023, 15, 152–171. [Google Scholar] [CrossRef]
- Barth, J.; Schumacher, M.; Herrmann-Lingen, C. Depression as a risk factor for mortality in patients with coronary heart disease: A meta-analysis. Psychosom. Med. 2004, 66, 802–813. [Google Scholar] [CrossRef] [PubMed]
- Dehdari, T.; Heidarnia, A.; Ramezankhani, A.; Sadeghian, S.; Ghofranipour, F. Effects of progressive muscular relaxation training on quality of life in anxious patients after coronary artery bypass graft surgery. Indian J. Med. Res. 2009, 129, 603. [Google Scholar] [PubMed]
- Carney, R.M.; Freedland, K.E. Depression and coronary heart disease. Nat. Rev. Cardiol. 2017, 14, 145–155. [Google Scholar] [CrossRef]
- Bahall, M. Prevalence and associations of depression among patients with cardiac diseases in a public health institute in Trinidad and Tobago. BMC Psychiatry 2019, 19, 4. [Google Scholar] [CrossRef] [PubMed]
- Haddad, M.; Walters, P.; Phillips, R.; Tsakok, J.; Williams, P.; Mann, A.; Tylee, A. Detecting depression in patients with coronary heart disease: A diagnostic evaluation of the PHQ-9 and HADS-D in primary care, findings from the UPBEAT-UK study. PLoS ONE 2013, 8, e78493. [Google Scholar]
- Organisation, W.H. Depression. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/depression (accessed on 23 March 2023).
- Gu, G.; Zhou, Y.; Zhang, Y.; Cui, W. Increased prevalence of anxiety and depression symptoms in patients with coronary artery disease before and after percutaneous coronary intervention treatment. BMC Psychiatry 2016, 16, 259. [Google Scholar] [CrossRef] [PubMed]
- Silarova, B.; Nagyova, I.; Van Dijk, J.P.; Rosenberger, J.; Reijneveld, S.A. Anxiety and sense of coherence in Roma and non-Roma coronary heart disease patients. Ethn. Health 2014, 19, 500–511. [Google Scholar] [CrossRef] [PubMed]
- Cohen, B.E.; Panguluri, P.; Na, B.; Whooley, M.A. Psychological risk factors and the metabolic syndrome in patients with coronary heart disease: Findings from the Heart and Soul Study. Psychiatry Res. 2010, 175, 133–137. [Google Scholar] [CrossRef]
- Ruo, B.; Rumsfeld, J.S.; Hlatky, M.A.; Liu, H.; Browner, W.S.; Whooley, M.A. Depressive symptoms and health-related quality of life: The Heart and Soul Study. JAMA 2003, 290, 215–221. [Google Scholar] [CrossRef]
- Whooley, M.A.; De Jonge, P.; Vittinghoff, E.; Otte, C.; Moos, R.; Carney, R.M.; Sadia, A.; Sunaina, D.; Beeya, N.; Feldman, M.D.; et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA 2008, 300, 2379–2388. [Google Scholar] [CrossRef] [PubMed]
- Currier, M.B.; Nemeroff, C.B. Inflammation and mood disorders: Proinflammatory cytokines and the pathogenesis of depression. Anti Inflamm. Anti Allergy Agents Med. Chem. 2010, 9, 212–220. [Google Scholar]
- Nemeroff, C.B.; Goldschmidt-Clermont, P.J. Heartache and heartbreak—The link between depression and cardiovascular disease. Nat. Rev. Cardiol. 2012, 9, 526–539. [Google Scholar] [CrossRef]
- Raedler, T.J. Inflammatory mechanisms in major depressive disorder. Curr. Opin. Psychiatry 2011, 24, 519–525. [Google Scholar] [CrossRef]
- Shimokawa, H. Primary endothelial dysfunction: Atherosclerosis. J. Mol. Cell. Cardiol. 1999, 31, 23–37. [Google Scholar] [CrossRef]
- Broadley, A.J.M.; Korszun, A.; Jones, C.J.H.; Frenneaux, M.P. Arterial endothelial function is impaired in treated depression. Heart 2002, 88, 521–523. [Google Scholar] [CrossRef] [PubMed]
- Cooper, D.C.; Tomfohr, L.M.; Milic, M.S.; Natarajan, L.; Bardwell, W.A.; Ziegler, M.G.; Dimsdale, J.E. Depressed mood and flow-mediated dilation: A systematic review and meta-analysis. Psychosom. Med. 2011, 73, 360. [Google Scholar] [CrossRef] [PubMed]
- Rajagopalan, S.; Brook, R.; Rubenfire, M.; Pitt, E.; Young, E.; Pitt, B. Abnormal brachial artery flow-mediated vasodilation in young adults with major depression. Am. J. Cardiol. 2001, 88, 196–198. [Google Scholar] [CrossRef] [PubMed]
- Rybakowski, J.K.; Wykretowicz, A.; Heymann-Szlachcinska, A.; Wysocki, H. Impairment of endothelial function in unipolar and bipolar depression. Biol. Psychiatry 2006, 60, 889–891. [Google Scholar] [CrossRef] [PubMed]
- Sherwood, A.; Hinderliter, A.L.; Watkins, L.L.; Waugh, R.A.; Blumenthal, J.A. Impaired endothelial function in coronary heart disease patients with depressive symptomatology. J. Am. Coll. Cardiol. 2005, 46, 656–659. [Google Scholar] [CrossRef] [PubMed]
- El-Metwally, A.; Javed, S.; Razzak, H.A.; Aldossari, K.K.; Aldiab, A.; Al-Ghamdi, S.H.; Househ, M.; Mamdouh, M.S.; Al-Zahrani, J.M. The factor structure of the general health questionnaire (GHQ12) in Saudi Arabia. BMC Health Serv. Res. 2018, 18, 595. [Google Scholar] [CrossRef]
- Fernandes, H.M.; Vasconcelos-Raposo, J. Factorial validity and invariance of the GHQ-12 among clinical and nonclinical samples. Assessment 2012, 20, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Hankins, M. The factor structure of the twelve-item general health questionnaire (GHQ-12): The result of negative phrasing? Clin. Pract. Epidemiol. Ment. Health 2008, 4, 10. [Google Scholar] [CrossRef]
- López, M.P.S.; Dresch, V. The 12-item general health questionnaire (GHQ-12): Reliability, external validity and factor structure in the Spanish population. Psicothema 2008, 20, 839–843. [Google Scholar]
- Salama-Younes, M.; Montazeri, A.; Ismaïl, A.; Roncin, C. Factor structure and internal consistency of the 12-item general health questionnaire (GHQ-12) and the subjective vitality scale (VS), and the relationship between them: A study from France. Health Qual. Life Outcomes 2009, 7, 22. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.B.; Fallowfield, L.J.; Stark, D.P.; Velikova, G.; Jenkins, V. A Rasch and confirmatory factor analysis of the general health questionnaire (GHQ)-12. Health Qual. Life Outcomes 2010, 8, 45. [Google Scholar] [CrossRef] [PubMed]
- Daradkeh, T.K.; Ghubash, R.; El-Rufaie, O.E.F. Reliability, validity, and factor structure of the Arabic version of the 12-item general health questionnaire. Psychol. Rep. 2001, 89, 85–94. [Google Scholar] [CrossRef]
- Endsley, P.; Weobong, B.; Nadkarni, A. The psychometric properties of GHQ for detecting common mental disorder among community-dwelli men in Goa, India. Asian J. Psychiatr. 2017, 28, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.; Knowles, S. A confirmatory factor analysis of the GHQ12 using a large Australian sample. Eur. J. Psychol. Assess. 2007, 23, 2–8. [Google Scholar] [CrossRef]
- Gao, W.; Stark, D.; Bennett, M.I.; Siegert, R.J.; Murray, S.; Higginson, I.J. Using the 12-item general health questionnaire to screen psychological distress from survivorship to end-of-life care: Dimensionality and item quality. Psycho Oncol. 2011, 21, 954–961. [Google Scholar] [CrossRef]
- Graetz, B. Multidimensional properties of the general health questionnaire. Soc. Psychiatry Psychiatr. Epidemiol. 1991, 26, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.M.; Leff, M.; Calonge, N.; Garrett, C.; Nelson, D.E. Validation of self-reported chronic conditions and health services in a managed care population. Am. J. Prev. Med. 2000, 18, 215–218. [Google Scholar] [PubMed]
- Padrón, A.; Galán, I.; Durbán, M.; Gandarillas, A.; Rodríguez-Artalejo, F. Confirmatory factor analysis of the general health questionnaire (GHQ-12) in Spanish adolescents. Qual. Life Res. 2011, 21, 1291–1298. [Google Scholar] [CrossRef]
- Penninkilampi-Kerola, V.; Miettunen, J.; Ebeling, H. Health and disability: A comparative assessment of the factor structures and psychometric properties of the GHQ-12 and the GHQ-20 based on data from a Finnish population-based sample. Scand. J. Psychol. 2006, 47, 431–440. [Google Scholar] [CrossRef]
- Rajabi, G.; Sheykhshabani, S.H. Factor structure of the 12-item general health questionnaire. J. Educ. Psychol. 2009, 3, 81–94. [Google Scholar]
- Marsh, H.W.; Morin, A.J.; Parker, P.D.; Kaur, G. Exploratory structural equation modeling: An integration of the best features of exploratory and confirmatory factor analysis. Annu. Rev. Clin. Psychol. 2014, 10, 85–110. [Google Scholar] [CrossRef]
- Griffith, G.J.; Jones, K. Understanding the population structure of the GHQ-12: Methodological considerations in dimensionally complex measurement outcomes. Soc. Sci. Med. 2019, 243, 112638. [Google Scholar] [CrossRef] [PubMed]
- University of Essex, Institute for Social and Economic Research. Understanding Society: Waves 1-11, 2009-2020 and Harmonised BHPS: Waves 1–18, 1991–2009, 15th ed.; UK Data Service: Manchester, UK, 2022. [Google Scholar] [CrossRef]
- Bhatnagar, P.; Wickramasinghe, K.; Wilkins, E.; Townsend, N. Trends in the epidemiology of cardiovascular disease in the UK. Heart 2016, 102, 1945–1952. [Google Scholar] [CrossRef]
- Barr, E.L.; Tonkin, A.M.; Welborn, T.A.; Shaw, J.E. Validity of self-reported cardiovascular disease events in comparison to medical record adjudication and a statewide hospital morbidity database: The AusDiab study. Intern. Med. J. 2009, 39, 49–53. [Google Scholar] [CrossRef]
- Goldberg, D.; Williams, P. A User’s Guide to the General Health Questionnaire; Nfer-Nelson: Windsor, UK, 1988. [Google Scholar]
- Davidson, K.W.; Burg, M.M.; Kronish, I.M.; Shimbo, D.; Dettenborn, L.; Mehran, R.; Vorchheimer, D.; Clemow, L.; Schwartz, J.E.; Rieckmann, N. Association of anhedonia with recurrent major adverse cardiac events and mortality 1 year after acute coronary syndrome. Arch. Gen. Psychiatry 2010, 67, 480–488. [Google Scholar] [CrossRef]
- Denollet, J.; Pedersen, S.S.; Daemen, J.; De Jaegere, P.; Serruys, P.W.; Van Domburg, R.T. Reduced positive affect (anhedonia) predicts major clinical events following implantation of coronary-artery stents. J. Intern. Med. 2008, 263, 203–211. [Google Scholar] [CrossRef] [PubMed]
- López Castro, J.; Cid Conde, L.; Fernández Rodríguez, V.; Failde Garrido, J.M.; Almazán Ortega, R. Analysis of quality of life using the generic SF-36 questionnaire in patients with heart failure. Rev. Calid. Asist. Organo Soc. Esp. Calid. Asist. 2013, 28, 355–360. [Google Scholar]
- Farquhar, J.M.; Stonerock, G.L.; Blumenthal, J.A. Treatment of anxiety in patients with coronary heart disease: A systematic review. Psychosomatics 2018, 59, 318–332. [Google Scholar] [CrossRef]
| Healthy Controls | CHD Patients | |||
|---|---|---|---|---|
| Mean | S.D. | Mean | S.D. | |
| Age | 68.47 | 8.22 | 68.29 | 11.60 |
| Income (monthly) | £1832.58 | £1570.07 | £1699.32 | £1170.78 |
| N | % | N | % | |
| Sex | ||||
| Male | 4167 | 67.89 | 308 | 68.44 |
| Female | 1971 | 32.11 | 142 | 31.56 |
| Education | ||||
| Below college | 4330 | 70.54 | 351 | 78.00 |
| College | 1808 | 29.46 | 99 | 22.00 |
| Legal marital status | ||||
| Single | 2048 | 33.37 | 178 | 39.56 |
| Married | 4090 | 66.63 | 272 | 60.44 |
| Residence | ||||
| Urban | 4348 | 70.84 | 323 | 71.78 |
| Rural | 1790 | 29.16 | 127 | 28.22 |
| GHQ-12 Items | Social Dysfunction and Anhedonia | Depression and Anxiety | Loss of Confidence |
|---|---|---|---|
| Concentration | 0.53 | 0.25 | −0.10 |
| Loss of sleep | 0.00 | 0.66 | 0.05 |
| Playing a useful role | 0.67 | −0.16 | 0.16 |
| Constantly under strain | 0.79 | −0.14 | 0.00 |
| Problem overcoming difficulties | −0.01 | 0.88 | −0.07 |
| Unhappy or depressed | 0.08 | 0.56 | 0.21 |
| Losing confidence | 0.68 | 0.22 | −0.125 |
| Believe worthless | 0.71 | −0.03 | 0.04 |
| General happiness | 0.013 | 0.53 | 0.34 |
| Capable of making decisions | 0.00 | 0.23 | 0.70 |
| Ability to face problems | 0.10 | 0.02 | 0.74 |
| Enjoy day-to-day activities | 0.56 | 0.10 | 0.10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, W.; Malvaso, A. Mental Health in Coronary Heart Disease (CHD) Patients: Findings from the UK Household Longitudinal Study (UKHLS). Healthcare 2023, 11, 1364. https://doi.org/10.3390/healthcare11101364
Kang W, Malvaso A. Mental Health in Coronary Heart Disease (CHD) Patients: Findings from the UK Household Longitudinal Study (UKHLS). Healthcare. 2023; 11(10):1364. https://doi.org/10.3390/healthcare11101364
Chicago/Turabian StyleKang, Weixi, and Antonio Malvaso. 2023. "Mental Health in Coronary Heart Disease (CHD) Patients: Findings from the UK Household Longitudinal Study (UKHLS)" Healthcare 11, no. 10: 1364. https://doi.org/10.3390/healthcare11101364
APA StyleKang, W., & Malvaso, A. (2023). Mental Health in Coronary Heart Disease (CHD) Patients: Findings from the UK Household Longitudinal Study (UKHLS). Healthcare, 11(10), 1364. https://doi.org/10.3390/healthcare11101364







