The Effects of a Scenario-Based Spiritual Care Course on Spiritual Care Competence among Clinical Nurses: A Quasi-Experimental Study
Abstract
1. Introduction
1.1. Background
1.2. Program Design
2. Materials and Methods
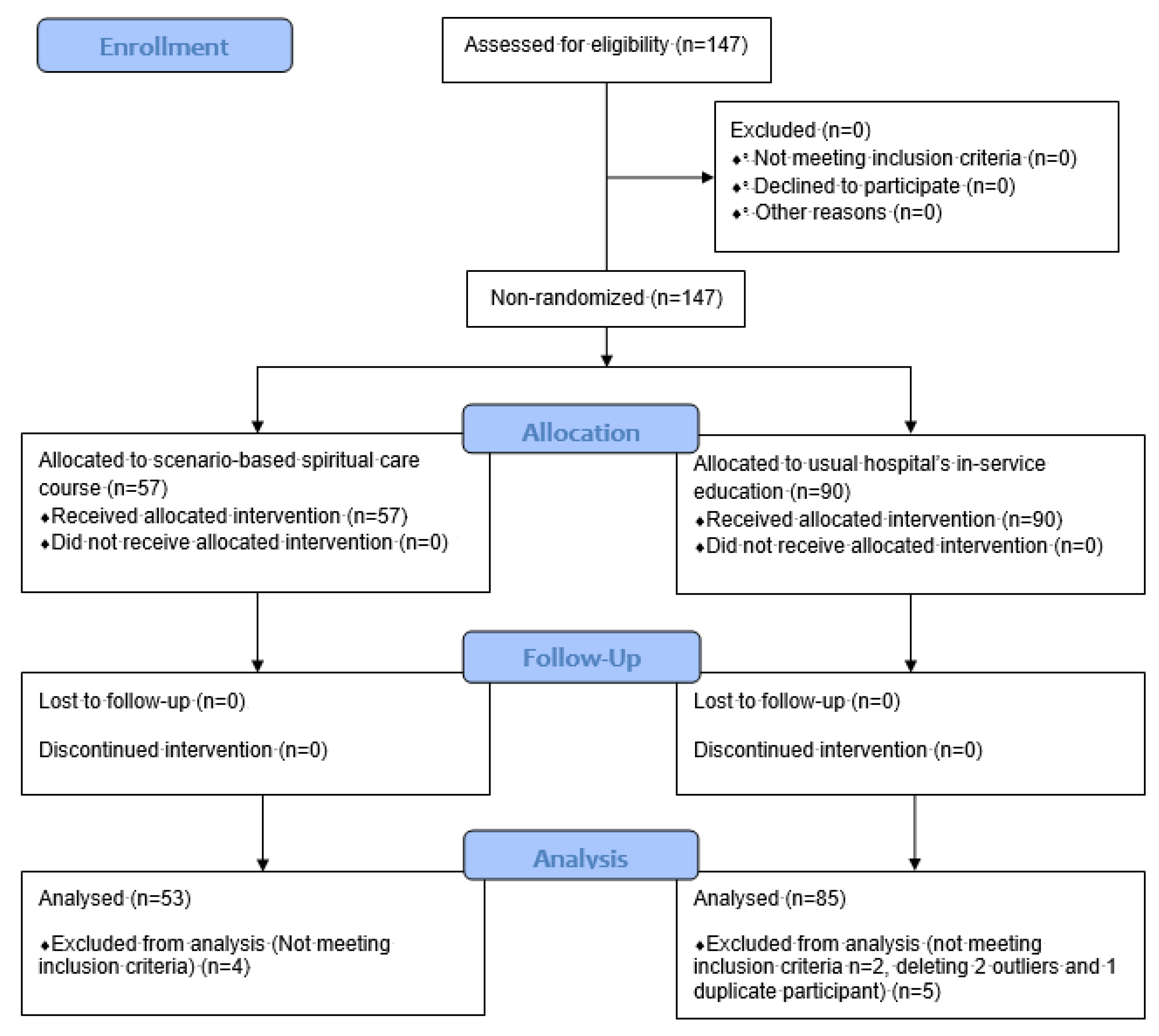
2.1. Study Design
2.2. Participants and Setting
2.3. Intervention
2.4. Instruments
2.5. Data Collection
2.6. Data Analysis
2.7. Ethical Considerations
3. Results
3.1. Background Information
3.2. SPS, SCPS-R, and Self- and HN-Evaluated SCCS at Baseline
3.3. Between-Subject Effects of the SPS, SCPS-R, and Self- and HN-Evaluated SCCS
3.4. Within-Subject Effects on the SPS, SCPS-R, and Self- and HN-Evaluated SCCS
3.5. Course Satisfaction, OSCE, and SPFS of the Experimental Group
3.6. Reflection Logs
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Instrument | Source and Purpose | Operational Definition | Validity | Reliability |
|---|---|---|---|---|
| Spiritual Perspective Scale (SPS) | Reed (1987) Measures extent to which individuals hold certain spiritual beliefs and engage in spiritually relevant behaviors |
|
|
|
| Spiritual Care Perspective Scale-Revised (SCPS-R) | Taylor et al. (1994) developed for measuring spiritual care perspective |
| CVI 0.96 |
|
| Spiritual Care Competence Scale (SCCS) | van Leeuwen & Cursveller (2004) developed for measuring spiritual care competence |
|
|
|
| Course Satisfaction Scale (CSS) | Refer to Hsu, Huang, & Hsieh (2014) developed for measuring satisfaction on communication competence training course satisfaction |
| CVI 1.00 |
|
| OSCE Checklist | Principal investigator developed for assessing spiritual assessment performance through literature review [52,53] |
| CVI 0.94 PAF using varimax rotation verified 2 factors explained 47.91% of cumulative variances | Cronbach’s α 0.84 for this study |
| Standardized Patient Feedback Scale (SPFS) | Refer to Hsu, Chang, & Hsieh (2015) developed for giving feedback to clinical nurses on spiritual assessment performance |
| CVI 1.00 | Cronbach’s α 0.91 for this study |
| Coefficients | ANOVA | Model Summary | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | IV & Covariate | b (SE) | Std b | t Value | p Value | 95% CI | F Value | p Value | R2 | Adjusted R2 |
| SPS | Constant | 10.09 (2.76) | NA | 3.66 | <0.001 | 4.63–15.56 | F(3,134) = 48.07 | <0.001 | 0.518 | 0.508 |
| Group | 2.86 (1.13) | 0.17 | 2.54 | 0.012 | 0.63–5.09 | |||||
| Interest in attending spirituality/spiritual care | 2.66 (0.92) | 0.23 | 2.90 | 0.004 | 0.85–4.47 | |||||
| SPS at T1 | 0.51 (0.07) | 0.52 | 7.17 | <0.001 | 0.37–0.65 | |||||
| SCPS-R | Constant | 20.72 (2.98) | NA | 6.96 | <0.001 | 14.83–26.60 | F(3,134) = 44.49 | <0.001 | 0.499 | 0.488 |
| Group | −0.98 (0.40) | −0.17 | −2.46 | 0.015 | −1.77–−0.19 | |||||
| Interest in attending spirituality/spiritual care | −0.77 (0.30) | −0.19 | −2.61 | 0.010 | −1.35–−0.19 | |||||
| SCPS-R at T1 | 0.53 (0.06) | 0.56 | 8.42 | <0.001 | 0.41–0.66 | |||||
| Self-evaluated SCCS | Constant | 21.94 (7.13) | NA | 3.08 | 0.003 | 7.83–36.05 | F(3,134) = 40.56 | <0.001 | 0.476 | 0.464 |
| Group | 7.05 (2.18) | 0.23 | 3.23 | 0.002 | 2.74–11.37 | |||||
| Interest in attending spirituality/spiritual care | 4.06 (1.52) | 0.19 | 2.67 | 0.008 | 1.06–7.07 | |||||
| Self-evaluated SCCS at T1 | 0.63 (0.07) | 0.59 | 9.16 | <0.001 | 0.49–0.76 | |||||
| HN-evaluated SCCS | Constant | 35.13 (8.49) | NA | 4.14 | <0.001 | 18.34–51.93 | F(3, 130) = 21.65 | <0.001 | 0.333 | 0.318 |
| Group | −0.98 (2.50) | −0.03 | −0.39 | 0.695 | −5.92–3.96 | |||||
| Interest in attending spirituality/spiritual care | 5.87 (1.72) | 0.27 | 3.41 | 0.001 | 2.47–9.28 | |||||
| HN-evaluated SCCS at T1 | 0.45 (0.07) | 0.46 | 6.18 | <0.001 | 0.31–0.60 | |||||
| Outcome | T1 (n = 53) | T2 (n = 53) | T3 (n = 53) | F Value | p Value | Partial Eta2 | Post Hoc Analysis | ||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | F Value | p Value | |||||
| SPS | 37.60 (10.25) | 41.21 (9.57) | 42.45 (9.73) | F(1.57,81.48) = 17.12 | <0.001 | 0.248 | T2 > T1 | F(1,52) = 24.50 | <0.001 |
| T3 > T1 | F(1,52) = 20.81 | <0.001 | |||||||
| SCPS-R | 38.45 (2.78) | 35.91 (2.78) | 37.17 (2.48) | F(2,104) = 29.93 | <0.001 | 0.365 | T1 > T2 | F(1,52) = 56.03 | <0.001 |
| T1 > T3 | F(1,52) = 19.66 | <0.001 | |||||||
| T3 > T2 | F(1,52) = 12.72 | 0.001 | |||||||
| Self-evaluated SCCS | 86.15 (15.33) | 96.85 (16.13) | 98.85 (16.14) | F(2,104) = 36.68 | <0.001 | 0.414 | T2 > T1 | F(1,52) = 47.54 | <0.001 |
| T3 > T1 | F(1,52) = 49.11 | <0.001 | |||||||
| Group/Outcome | Baseline | T3 | t Value | p Value | 95% CI | ||
|---|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | ||||
| Experimental group | |||||||
| HN-evaluated SCCS | 51 | 102.39 (15.76) | 51 | 103.75 (14.92) | −0.61 | 0.542 | −5.78–3.08 |
| Control group | |||||||
| SPS | 85 | 36.51 (6.85) | 85 | 37.42 (6.32) | −1.44 | 0.154 | −2.19–0.35 |
| SCPS-R | 85 | 39.28 (3.13) | 85 | 39.06 (2.90) | 0.79 | 0.434 | −0.34–0.79 |
| Self-evaluated SCCS | 85 | 89.15 (13.58) | 85 | 91.21 (13.87) | −1.62 | 0.109 | −4.58–0.47 |
| HN-evaluated SCCS | 83 | 93.78 (14.25) | 83 | 97.17 (14.57) | −2.14 | 0.035 | −6.54–−0.24 |
| Not Done | Partially Done | Completely Done | Range | Mean (SD) | Rank | ||
|---|---|---|---|---|---|---|---|
| Item | n (%) | n (%) | n (%) | ||||
| 2. Encourage patients to express their thoughts and feelings about having cancer. | 1 (1.9) | 14 (26.4) | 38 (71.7) | 0–2 | 1.70 (0.50) | H2 | |
| 3. Demonstrate eye contact and listening behaviors. | 0 (0.0) | 10 (18.9) | 43 (81.1) | 1–2 | 1.81 (0.40) | H1 | |
| 4. Can apply body language to interact with patients. | 28 (52.8) | 14 (26.4) | 11 (20.8) | 0–2 | 0.68 (0.80) | L2 | |
| 5. Can respond appropriately to patient questions. | 4 (7.5) | 25 (47.2) | 24 (45.3) | 0–2 | 1.38 (0.63) | ||
| 7. Demonstrate attitude of accepting patients. (e.g., caring, compassion, inspiring trust and confidence, empathy, sincere, sensitive or cordial) | 1 (1.9) | 24 (45.3) | 28 (52.8) | 0–2 | 1.51 (0.54) | ||
| 8. Can soothe the patient’s emotions in timely manner. | 1 (1.9) | 21 (39.6) | 31 (58.5) | 0–2 | 1.57 (0.54) | H3 | |
| 9. Can adequately use care experience to share with patients. | 7 (13.2) | 19 (35.8) | 27 (50.9) | 0–2 | 1.38 (0.71) | ||
| 10. Can relate to loss as a normal reaction. | 34 (64.2) | 13 (24.5) | 6 (11.3) | 0–2 | 0.47 (0.70) | L1 | |
| 11. Can assess relevant data of the spiritual aspect. | 11 (20.8) | 39 (73.6) | 3 (5.7) | 0–2 | 0.85 (0.50) | L3 | |
| Grand mean of percent/mean(SD) | 18.2 | 37.5 | 44.3 | 1–17 | 11.34 (3.58) | ||
| 1 (Failed) | 2 (Passing edge) | 3 (Passed) | 4 (Good) | 5 (Excellent) | Range | Mean (SD) | |
| Item | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Global performance | 1 (1.9) | 6 (11.3) | 23 (43.4) | 19 (35.8) | 4 (7.5) | 1–5 | 3.40 (0.91) |
Appendix B

References
- International Council of Nurses [ICN]. Nursing Definitions. 2022. Available online: https://www.icn.ch/nursing-policy/nursing-definitions (accessed on 16 November 2022).
- Gallison, B.S.; Xu, Y.; Jurgens, C.Y.; Boyle, S.M. Acute Care Nurses’ Spiritual Care Practices. J. Holist. Nurs. 2013, 31, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.-F.; Koo, M.; Liao, Y.-C.; Chen, Y.-M.; Yeh, D.-C. Development and Validation of the Spiritual Care Needs Inventory for Acute Care Hospital Patients in Taiwan. Clin. Nurs. Res. 2015, 25, 590–606. [Google Scholar] [CrossRef]
- Shih, F.-J.; Lin, H.-R.; Gau, M.-L.; Chen, C.-H.; Hsiao, S.-M.; Shih, S.-N.; Sheu, S.-J. Spiritual Needs of Taiwan’s Older Patients With Terminal Cancer. Oncol. Nurs. Forum 2009, 36, E31–E38. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, S.-M.; Gau, M.-L.; Ingleton, C.; Ryan, T.; Shih, F.-J. An exploration of spiritual needs of Taiwanese patients with advanced cancer during the therapeutic processes. J. Clin. Nurs. 2011, 20, 950–959. [Google Scholar] [CrossRef] [PubMed]
- Thuné-Boyle, I.C.; Stygall, J.A.; Keshtgar, M.R.; Newman, S.P. Do religious/spiritual coping strategies affect illness adjustment in patients with cancer? A systematic review of the literature. Soc. Sci. Med. 2006, 63, 151–164. [Google Scholar] [CrossRef]
- Charles, E.J. Effects of Spirituality on Patients’ Health Outcomes. Master’s Thesis, Rhode Island College, New York, NY, USA, 2018. Available online: http://digitalcommons.ric.edu/etd/289 (accessed on 4 December 2022).
- Seybold, K.S.; Hill, P.C. The Role of Religion and Spirituality in Mental and Physical Health. Curr. Dir. Psychol. Sci. 2001, 10, 21–24. [Google Scholar] [CrossRef]
- O’Shea, E.R.; Wallace, M.; Griffin, M.Q.; Fitzpatrick, J.J. The Effect of an Educational Session on Pediatric Nurses’ Perspectives Toward Providing Spiritual Care. J. Pediatr. Nurs. 2011, 26, 34–43. [Google Scholar] [CrossRef]
- The Joint Commission. Standards FAQ. 2022. Available online: https://www.jointcommission.org/search/#q=spiritual%20care&t=_Tab_All&sort=relevancy&f:_SitesOrganizations=[The%20Joint%20Commission] (accessed on 16 November 2022).
- American Nurse Association [ANA]. Nursing: Scope and Standards of Practice (2nd ed.). 2010. ANA. Available online: https://www.bethelu.edu/uploads/general/Nursing-Program-ApplicationProcess_Scope-and-Standards.pdf (accessed on 16 November 2022).
- International Council of Nurses [ICN]. The ICN Code of Ethics for Nurses. 2021. Available online: https://www.icn.ch/system/files/2021-10/ICN_Code-of-Ethics_EN_Web_0.pdf (accessed on 16 November 2022).
- Attard, J.; Baldacchino, D. The demand for competencies in spiritual care in nursing and midwifery education: A literature review. Rev. Pist. Prax. 2014, 6, 671. [Google Scholar] [CrossRef]
- Hsieh, S.; Hsu, L.; Kao, C.; Breckenridge-Sproat, S.; Lin, H.; Tai, H.; Huang, T.; Chu, T. Factors associated with spiritual care competencies in Taiwan’s clinical nurses: A descriptive correlational study. J. Clin. Nurs. 2020, 29, 1599–1613. [Google Scholar] [CrossRef]
- Wu, L.-F.; Tseng, H.-C.; Liao, Y.-C. Nurse education and willingness to provide spiritual care. Nurse Educ. Today 2016, 38, 36–41. [Google Scholar] [CrossRef]
- Cetinkaya, B.; Dundar, S.A.; Azak, A. Nurses’ Perceptions of Spirituality and Spiritual Care. AJAN 2013, 31, 5–10. [Google Scholar]
- Ruder, S. Spirituality in Nursing: Nurses’ Perceptions about Providing Spiritual Care. Home Healthc. Nurse J. Home Care Hosp. Prof. 2013, 31, 356–367. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.F.; Hsiao, Y.C. A Study of the Correlation between the Spiritual Health Status and Spiritual Care Abilities of Nurses. J. Nurs. Healthc. Res. 2009, 5, 68–78. [Google Scholar] [CrossRef]
- Zehtab, S.; Hajbaghery, M.A. The Importance of Spiritual Care in Nursing. Nurs. Midwifery Stud. 2014, 3, e22261. [Google Scholar] [CrossRef]
- Green, A.; Kim-Godwin, Y.S.; Jones, C.W. Perceptions of Spiritual Care Education, Competence, and Barriers in Providing Spiritual Care Among Registered Nurses. J. Holist. Nurs. 2020, 38, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Azarsa, T.; Davoodi, A.; Markani, A.K.; Gahramanian, A.; Vargaeei, A. Spiritual wellbeing, Attitude toward Spiritual Care and its Relationship with Spiritual Care Competence among Critical Care Nurses. J. Caring Sci. 2015, 4, 309–320. [Google Scholar] [CrossRef]
- Baldacchino, D. Spiritual Care Education of Health Care Professionals. Religions 2015, 6, 594–613. [Google Scholar] [CrossRef]
- Hawthorne, D.M.; Gordon, S.C. The Invisibility of Spiritual Nursing Care in Clinical Practice. J. Holist. Nurs. 2020, 38, 147–155. [Google Scholar] [CrossRef]
- Keall, R.; Clayton, J.; Butow, P. How do Australian palliative care nurses address existential and spiritual concerns? Facilitators, barriers and strategies. J. Clin. Nurs. 2014, 23, 3197–3205. [Google Scholar] [CrossRef]
- Paal, P.; Helo, Y.; Frick, E. Spiritual Care Training Provided to Healthcare Professionals: A Systematic Review. J. Pastor. Care Couns. 2015, 69, 19–30. [Google Scholar] [CrossRef]
- Van Leeuwen, R.; Tiesinga, L.J.; Middel, B.; Post, D.; Jochemsen, H. The validity and reliability of an instrument to assess nursing competencies in spiritual care. J. Clin. Nurs. 2009, 18, 2857–2869. [Google Scholar] [CrossRef] [PubMed]
- Cahn, P.S.; Smoller, S.L. Experiential Learning and Cultural Competence: What Do Participants in Short-Term Experiences in Global Health Learn About Culture? Health Prof. Educ. 2020, 6, 230–237. [Google Scholar] [CrossRef]
- Jacob, S.A.; Power, A.; Portlock, J.; Jebara, T.; Cunningham, S.; Boyter, A.C. Competency-Based Assessment in Experiential Learning in Undergraduate Pharmacy Programmes: Qualitative Exploration of Facilitators’ Views and Needs (ACTp Study). Pharmacy 2022, 10, 90. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.F.; Paal, P.; Symons, X.; Best, M.C. The Content, Teaching Methods and Effectiveness of Spiritual Care Training for Healthcare Professionals: A Mixed-Methods Systematic Review. J. Pain Symptom Manag. 2021, 62, e261–e278. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Jiao, M.; Li, F. Effectiveness of spiritual care training to enhance spiritual health and spiritual care competency among oncology nurses. BMC Palliat. Care 2019, 18, 104. [Google Scholar] [CrossRef]
- Vlasblom, J.P.; van der Steen, J.T.; Knol, D.L.; Jochemsen, H. Effects of a spiritual care training for nurses. Nurse Educ. Today 2011, 31, 790–796. [Google Scholar] [CrossRef]
- Amoah, V.A. The Effect of Spiritual Care Education on Hospice Nurses’ Competence in the Assessment and Implementation of Spiritual Care with Their Patients: A Quasi-Experimental Study. Master’s Thesis, Cedarville University, Cedarville, OH, USA, 2015. [Google Scholar]
- Linegang, B.F. A Quasi-Experimental Pilot Study Examining the Effects of Spiritual Nursing Care Education Based in Biblical Truth on Pediatric Nurses’ Competence in Providing Spiritual Nursing Care. Master’s Thesis, Cedarville University, Cedarville, OH, USA, 2014. Available online: https://digitalcommons.cedarville.edu/nursing_theses/9/ (accessed on 16 November 2022).
- Petersen, C.L.; Callahan, M.F.; McCarthy, N.O.; Hughes, R.G.; White-Traut, R.; Bansal, N.K. An Online Educational Program Improves Pediatric Oncology Nurses’ Knowledge, Attitudes, and Spiritual Care Competence. J. Pediatr. Oncol. Nurs. 2017, 34, 130–139. [Google Scholar] [CrossRef]
- Narayanasamy, A. ASSET: A Model for Actioning Spirituality and Spiritual Care Education and Training in Nursing. Nurse Educ. Today 1999, 19, 274–285. [Google Scholar] [CrossRef]
- Petersen, C.L. Effects of Spiritual Care Education on Pediatric Nurses’ Knowledge, Attitudes, and Competence. Ph.D. Thesis, Marquette University, Milwaukee, WI, USA, 2015. Available online: https://epublications.marquette.edu/dissertations_mu/654/ (accessed on 16 November 2022).
- Narayanasamy, A. The impact of empirical studies of spirituality and culture on nurse education. J. Clin. Nurs. 2006, 15, 840–851. [Google Scholar] [CrossRef]
- Jeffries, P.R. A framework for designing, implementing, and evaluating simulations used as teaching strategies in nursing. Nurs. Educ. Perspect. 2005, 26, 96–103. [Google Scholar]
- Jeffries, P.R.; Rogers, K.J. Theoretical Framework for Simulation Design. In Simulation in Nursing Education. From Conceptualization to Evaluation, 3rd ed.; Jeffries, P.R., Ed.; Wolters Kluwer: Philadelphia, PA, USA, 2020; pp. 25–42. [Google Scholar]
- Jeffries, P.R.; Rodgers, B.; Adamson, K. NLN Jeffries Simulation Theory: Brief Narrative Description. Nurs. Educ. Perspect. 2015, 36, 292–293. [Google Scholar] [CrossRef] [PubMed]
- Aebersold, M.; Titler, M.G. A Simulation Model for Improving Learner and Health Outcomes. Nurs. Clin. N. Am. 2014, 49, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Cowperthwait, A. NLN/Jeffries Simulation Framework for Simulated Participant Methodology. Clin. Simul. Nurs. 2020, 42, 12–21. [Google Scholar] [CrossRef]
- Ross, S. Simulation-Based Learning: From Learning Theory to Pedagogical Application. Internet J. Allied Health Sci. Pract. 2021, 19, 15. [Google Scholar] [CrossRef]
- McMahon, E.; Jimenez, F.A.; Lawrence, K.; Victor, J.; INACSL Standards Committee. Healthcare Simulation Standards of Best PracticeTM Evaluation of Learning and Performance. Clin. Simul. Nurs. 2021, 58, 54–56. [Google Scholar] [CrossRef]
- Zenios, M. Educational theory in technology enhanced learning revisited: A model for simulation-based learning in higher education. Stud. Technol. Enhanc. Learn. 2020, 1, 191–207. [Google Scholar] [CrossRef]
- Clarke, S.; Rainey, D.; Traynor, M. Using the Objective Structured Clinical Examination (OSCE) to assess orthopaedic clinical skills for the registered nurse. Int. J. Orthop. Trauma Nurs. 2011, 15, 92–101. [Google Scholar] [CrossRef]
- Khan, K.Z.; Ramachandran, S.; Gaunt, K.; Pushkar, P. The Objective Structured Clinical Examination (OSCE): AMEE Guide No. 81. Part I: An historical and theoretical perspective. Med. Teach. 2013, 35, e1437–e1446. [Google Scholar] [CrossRef]
- Zayyan, M. Objective Structured Clinical Examination: The Assessment of Choice. Oman Med. J. 2011, 26, 219–222. [Google Scholar] [CrossRef]
- Taylor, E.J.; Mamier, I.; Bahjri, K.; Anton, T.; Petersen, F. Efficacy of a self-study programme to teach spiritual care. J. Clin. Nurs. 2008, 18, 1131–1140. [Google Scholar] [CrossRef]
- Ross, L.; van Leeuwen, R.; Baldacchino, D.; Giske, T.; McSherry, W.; Narayanasamy, A.; Downes, C.; Jarvis, P.; Schep-Akkerman, A. Student nurses perceptions of spirituality and competence in delivering spiritual care: A European pilot study. Nurse Educ. Today 2014, 34, 697–702. [Google Scholar] [CrossRef] [PubMed]
- Ross, L.; Giske, T.; van Leeuwen, R.; Baldacchino, D.; McSherry, W.; Narayanasamy, A.; Jarvis, P.; Schep-Akkerman, A. Factors contributing to student nurses’/midwives’ perceived competency in spiritual care. Nurse Educ. Today 2016, 36, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Van Leeuwen, R.; Schep-Akkerman, A. Nurses’ Perception of Spirituality and Spiritual Care in Different Health Care Settings in the Netherland. Religions 2015, 6, 1346–1357. [Google Scholar] [CrossRef]
- McSherry, W. Spiritual Care in Nursing Practice: An Interactive Approach; Jessica Kingsley Publishers: Philadelphia, PA, USA, 2006. [Google Scholar]
- Hsiao, H.E.; Chen, S.L.; Tsai, G.S.; Lai, S.Y.; Kao, M.L.; Huang, S.C.; Tseng, L.C.; Wu, L.F.; Chou, C.C. Spiritual Care; Farseeing Publishing Group: Taipei, Taiwan, 2009. [Google Scholar]
- Ku, Y.L. Spirituality in Nursing: Theory, Practice, Education & Research; Farseeing Publishing Group: Taipei, Taiwan, 2010. [Google Scholar]
- Bennett, V.; Thompson, M.L. Teaching spirituality to student nurses. J. Nurs. Educ. Pract. 2015, 5, 26. [Google Scholar] [CrossRef]
- Taiwan Nurses Association [TNA]. Planning Guideline of Basic Nursing Competence Ladder. 2021. Available online: https://www.twna.org.tw/WebPad/WebPad.aspx?1x8jyHnXeNSHfBGHev4mkg%3D%3D (accessed on 5 December 2022).
- Farajpour, A.; Amini, M.; Pishbin, E.; Mostafavian, Z.; Farmad, S.A. Using modified Direct Observation of Procedural Skills (DOPS) to assess undergraduate medical students. J. Adv. Med. Educ. Prof. 2018, 6, 130–136. [Google Scholar] [CrossRef]
- Albritton, M. Body Language and Hand Gestures in Different Cultures. 2022. Available online: https://study.com/learn/lesson/body-language-different-cultures-gestures-examples-importance.html (accessed on 7 December 2022).
- Miller, G.E. The Assessment of Clinical Skills/Competence/Performance. Acad. Med. 1990, 65 (Suppl. 9), S63–S67. [Google Scholar] [CrossRef]
- Dailey, D.E.; Stewart, A.L. Psychometric characteristics of the spiritual perspective scale in pregnant African-American women. Res. Nurs. Health 2007, 30, 61–71. [Google Scholar] [CrossRef]
- Meezenbroek, E.D.J.; Garssen, B.; Berg, M.V.D.; Tuytel, G.; Van Dierendonck, D.; Visser, A.; Schaufeli, W. Measuring Spirituality as a Universal Human Experience: Development of the Spiritual Attitude and Involvement List (SAIL). J. Psychosoc. Oncol. 2012, 30, 141–167. [Google Scholar] [CrossRef]
- Hsu, L.-L.; Huang, Y.-H.; Hsieh, S.-I. The effects of scenario-based communication training on nurses’ communication competence and self-efficacy and myocardial infarction knowledge. Patient Educ. Couns. 2014, 95, 356–364. [Google Scholar] [CrossRef]
- Hsu, L.-L.; Chang, W.-H.; Hsieh, S.-I. The Effects of Scenario-Based Simulation Course Training on Nurses’ Communication Competence and Self-Efficacy: A Randomized Controlled Trial. J. Prof. Nurs. 2015, 31, 37–49. [Google Scholar] [CrossRef]
- Monod, S.; Brennan, M.; Rochat, E.; Martin, E.; Rochat, S.; Büla, C.J. Instruments Measuring Spirituality in Clinical Research: A Systematic Review. J. Gen. Intern. Med. 2012, 26, 1345. [Google Scholar] [CrossRef] [PubMed]
| NR | O1 | X | O2 | O3 |
|---|---|---|---|---|
| NR | O1 | O2 | ||
| Measures | Time 1 | Time 2 | Time 3 | |
| 1. Background information | √(EG) | √(CG) | ||
| 2. Self-evaluated SCCS (PO) | √(EG) | √(EG & CG) | √(EG & CG) | |
| 3. HN-evaluated SCCS (PO) | √(EG & CG) | √(EG & CG) | ||
| 4. SPS (PO) | √(EG) | √(EG & CG) | √(EG & CG) | |
| 5. SCPS-R (PO) | √(EG) | √(EG & CG) | √(EG & CG) | |
| 6. Reflection log (PO) | √(EG) | √(EG & CG) | ||
| 7. Course Satisfaction (SO) | √(EG) | |||
| 8. SPFS (SO) | √(EG) | |||
| 9. OSCE Checklist (SO) | √(EG) |
| Content | |
|---|---|
| Learning objectives | 1. Differentiate the definitions of spirituality, religion, and spiritual care. 2. Understand the impact of illness. 3. Understand clues of patient or family conversation about spirituality. 4. Perform spiritual care assessment. 5. Clarify spiritual distress and well-being. 6. Execute the nursing process of spiritual care. 7. Write individual spiritual reflection logs. 8. Understand skills of looking for life’s meaning and purpose. |
| Content and related teaching strategies | Morning Session 1. Lecture with PowerPoint, handout, and shared cases.
1. OSCE
|
| Course Offerings and Participants | 1. 17 August 2019–11 January 2020 (7 times): held 5 times on 17 August (n = 4); 28 September (n = 5); 2 November (n = 5); 23 November 2019 (n = 8); & 11 January 2020 (n = 5) 2. 22 February 2020–13 June 2020 (5 times): held 2 times on 18 April (n = 3); & 16 May (n = 1) 3. 29 August 2020–28 November 2020 (3 times): held 3 times on 29 August (n = 11); 31 October (n = 9); & 28 November (n = 6) |
| Course Schedule | 08:00–08:20 (20 min) Check in and completion of baseline measures 08:21–10:10 (110 min) Lecture of spiritual care 10:11–10:20 (10 min) Rest/Break 10:21–11:20 (60 min) Scenario-based spiritual care video watching and debriefing 11:21–11:30 (10 min) Rest/Break 11:31–12:00 (30 min) Completion of 1st posttest measures 12:01–13:00 (60 min) Rest and lunch 13:01–16:00 OSCE (15 min examination and 5 min SP feedback) 16:01 Check out and distribute gift card (NT 500 dollars) |
| Control | Experimental | ||||
|---|---|---|---|---|---|
| (n = 85) | (n = 53) | t/χ2 Test | p Value | ||
| Variable | Category | n (%) | n (%) | ||
| Age in years a | t(136) = −0.62 | 0.535 | |||
| Range | 22–55 | 23–56 | |||
| Mean (SD) | 32.01 (7.45) | 31.17 (8.19) | |||
| Gender b | Male | 2 (2.4) | 0 (0.0) | NA | 0.523 |
| Female | 83 (97.6) | 53 (100.0) | |||
| Marital status c | Single | 61 (71.8) | 40 (75.5) | χ2(1) = 0.23 | 0.633 |
| Married | 24 (28.2) | 13 (24.5) | |||
| Education c | 2-year/5-year diploma | 4 (4.7) | 7 (13.2) | χ2(3) = 4.00 | 0.261 |
| 2-year college | 39 (45.9) | 21 (39.6) | |||
| 4-year college | 8 (9.4) | 7 (13.2) | |||
| ≥University/master’s programme | 34 (40.0) | 18 (34.0) | |||
| Religion b | None identified | 38 (44.7) | 19 (35.8) | 8.18 | 0.135 |
| Buddhist | 6 (7.1) | 8 (15.1) | |||
| Christian/Catholic | 4 (4.7) | 7 (13.2) | |||
| Taoist | 23 (27.1) | 8 (15.1) | |||
| I-Kuan Tao | 2 (2.4) | 2 (3.8) | |||
| Folk beliefs | 12 (14.1) | 9 (17.0) | |||
| Working years a | t(136) = −0.65 | 0.519 | |||
| Range | 0.1–35.8 | 0.3–34.1 | |||
| Mean (SD) | 9.42 (7.62) | 8.55 (7.85) | |||
| Nursing clinical ladder c | N0 | 7 (8.2) | 3 (5.7) | χ2(4) = 4.94 | 0.294 |
| N1 | 7 (8.2) | 10 (18.9) | |||
| N2 | 21 (24.7) | 16 (30.2) | |||
| N3 | 17 (20.2) | 7 (13.2) | |||
| ≥N4 | 33 (38.8) | 17 (32.1) | |||
| Physical health status c | Very poor/poor | 9 (10.6) | 1 (1.9) | χ2(2) = 4.12 | 0.128 |
| Common | 58 (68.2) | 37 (69.8) | |||
| Good/very good | 18 (21.2) | 15 (28.3) | |||
| Interest in spirituality and spiritual care a | t(136) = −5.40 | <0.001 | |||
| Range | 2–5 | 3–5 | |||
| Mean (SD) | 3.32 (0.60) | 3.92 (0.70) |
| Control | Experimental | t/Fisher’s | ||
|---|---|---|---|---|
| (n = 85) | (n = 53) | Exact Test | p Value | |
| Variable | n (%) | n (%) | ||
| SPS a | t(81.1) = 0.69 | 0.492 | ||
| Range | 20–57 | 19–59 | ||
| Mean (SD) | 36.51 (6.85) | 37.60 (10.25) | ||
| SCPS-R a | t(136) = 1.58 | 0.116 | ||
| Range | 32–48 | 33–44 | ||
| Mean (SD) | 39.28 (3.13) | 38.45 (2.78) | ||
| Self-evaluated SCCS a | t(136) = 1.20 | 0.232 | ||
| Range | 55–125 | 52–109 | ||
| Mean (SD) | 89.15 (13.58) | 86.15 (15.33) | ||
| Self-evaluated SCCS b | 2.09 | 0.381 | ||
| Low competence (<64) | 2 (2.4) | 4 (7.5) | ||
| Moderate competence (64–98) | 60 (70.6) | 36 (67.9) | ||
| High competence (99–135) | 23 (27.1) | 13 (24.5) | ||
| HN-evaluated SCCS a | t(133) = −3.04 | 0.003 | ||
| Range | 63–131 | 66–129 | ||
| Mean (SD) | 94.23 (14.74) | 102.39 (15.76) | ||
| HN-evaluated SCCS b | 4.48 | 0.072 | ||
| Low competence (<64) | 1 (1.2) | 0 (0.0) | ||
| Moderate competence (64–98) | 52 (61.9) | 23 (45.1) | ||
| High competence (99–135) | 31 (36.9) | 28 (54.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsieh, S.-I.; Hsu, L.-L.; Hinderer, K.A.; Lin, H.-L.; Tseng, Y.-P.; Kao, C.-Y.; Lee, C.-Y.; Kao, S.-H.; Chou, Y.-F.; Szu, L.-Y.; et al. The Effects of a Scenario-Based Spiritual Care Course on Spiritual Care Competence among Clinical Nurses: A Quasi-Experimental Study. Healthcare 2023, 11, 36. https://doi.org/10.3390/healthcare11010036
Hsieh S-I, Hsu L-L, Hinderer KA, Lin H-L, Tseng Y-P, Kao C-Y, Lee C-Y, Kao S-H, Chou Y-F, Szu L-Y, et al. The Effects of a Scenario-Based Spiritual Care Course on Spiritual Care Competence among Clinical Nurses: A Quasi-Experimental Study. Healthcare. 2023; 11(1):36. https://doi.org/10.3390/healthcare11010036
Chicago/Turabian StyleHsieh, Suh-Ing, Li-Ling Hsu, Katherine A. Hinderer, Hui-Ling Lin, Yi-Ping Tseng, Chen-Yi Kao, Ching-Yun Lee, Shu-Hua Kao, Yen-Fang Chou, Li-Yun Szu, and et al. 2023. "The Effects of a Scenario-Based Spiritual Care Course on Spiritual Care Competence among Clinical Nurses: A Quasi-Experimental Study" Healthcare 11, no. 1: 36. https://doi.org/10.3390/healthcare11010036
APA StyleHsieh, S.-I., Hsu, L.-L., Hinderer, K. A., Lin, H.-L., Tseng, Y.-P., Kao, C.-Y., Lee, C.-Y., Kao, S.-H., Chou, Y.-F., Szu, L.-Y., & Ho, L.-H. (2023). The Effects of a Scenario-Based Spiritual Care Course on Spiritual Care Competence among Clinical Nurses: A Quasi-Experimental Study. Healthcare, 11(1), 36. https://doi.org/10.3390/healthcare11010036





