Reasons for Non-Attendance in the German National Mammography Screening Program: Which Barriers Can Be Overcome Using Telephone Counseling?—A Randomized Controlled Trial
Abstract
1. Introduction
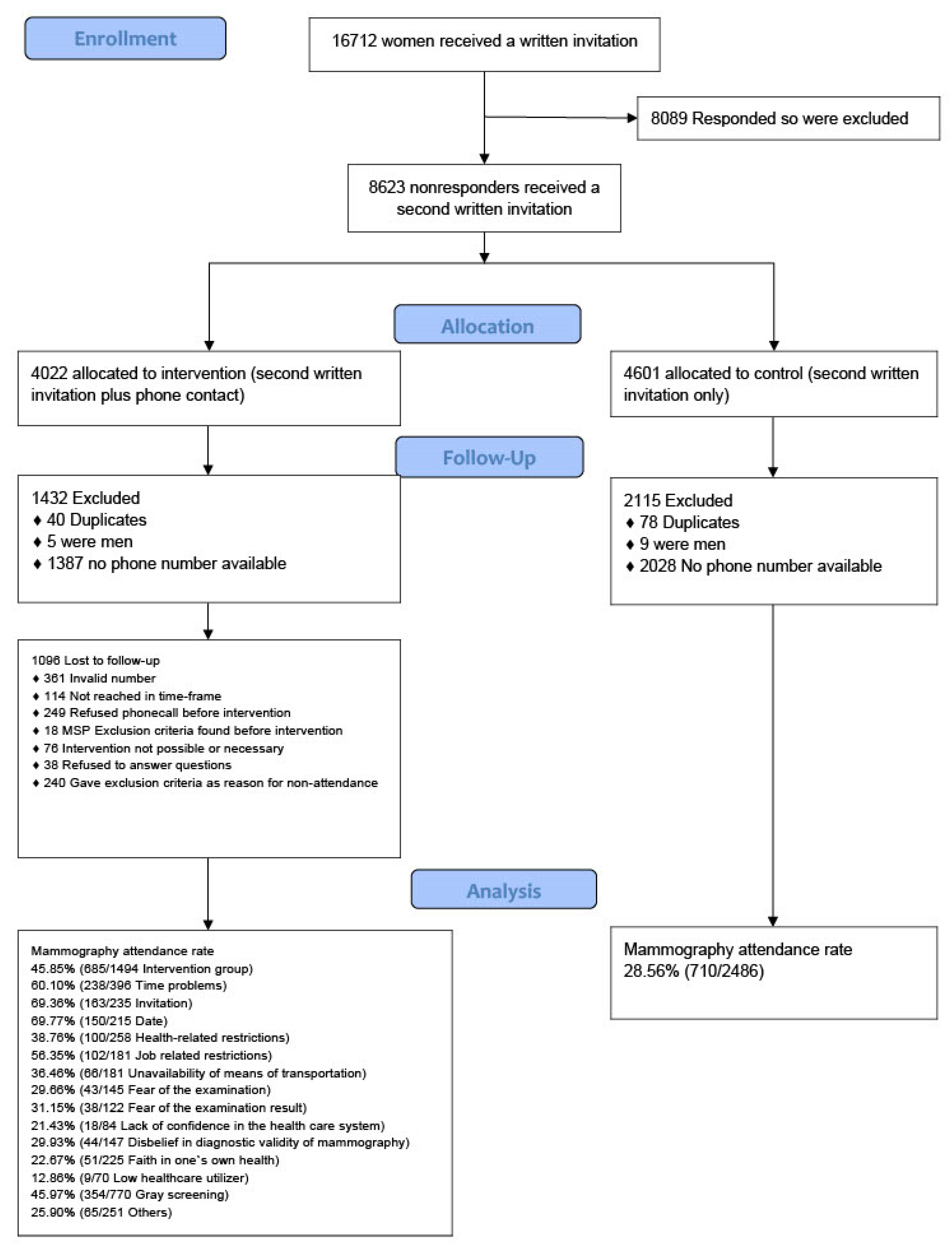
2. Methods
2.1. Study Population
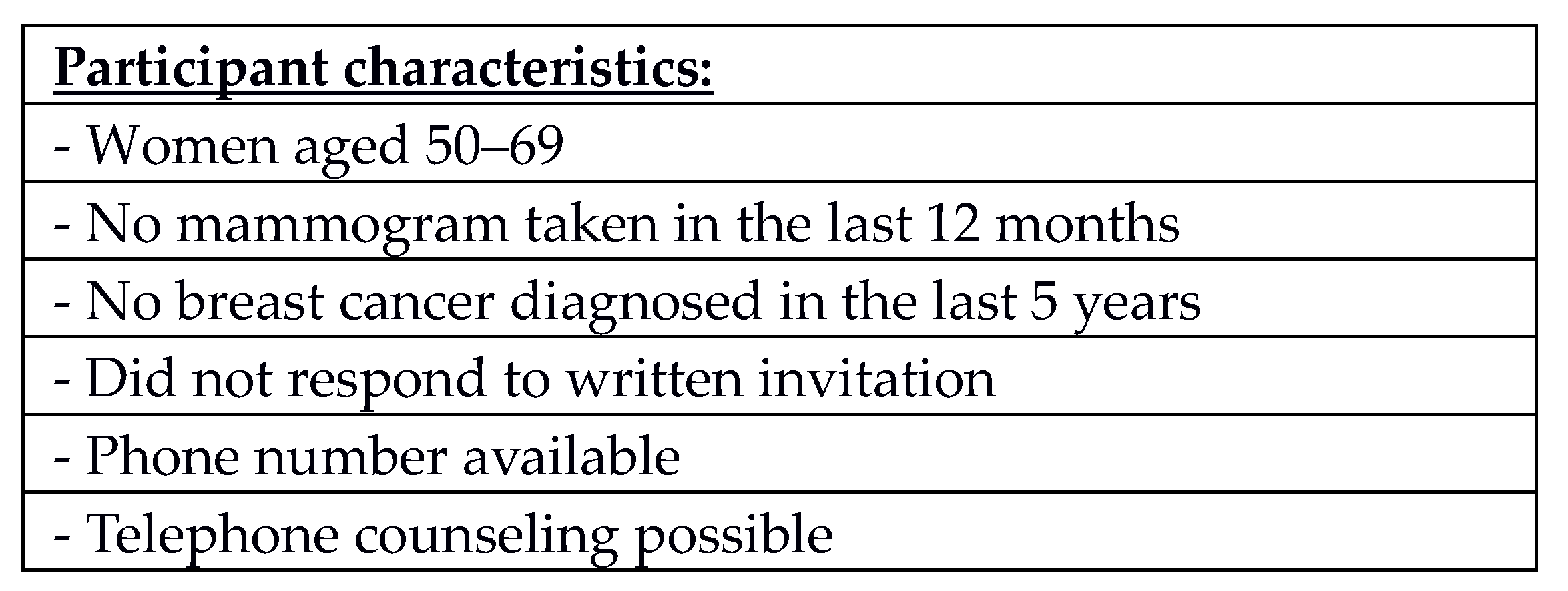
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Study Procedure
2.4.1. Consultation
2.4.2. Objectives
2.5. Statistical Analysis
3. Results
3.1. Control Group
3.2. Individual Reasons
3.3. Categories in Detail
Block 1: Organizational ProblemsProblems surrounding the organizational aspect of screening
Block 2: Limited resources
Problems originating in the client’s limited ability to attend
Block 3: Negative perception
Barriers resulting from preconceptions
Block 4: Other
Other reasons
4. Discussion
4.1. Summary
4.2. Context
4.3. Key Findings
4.4. Implications for Future Research
4.5. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tabar, L.; Gad, A.; Holmberg, L.H.; Ljungquist, U.; Group, K.C.P.; Fagerberg, C.J.G.; Baldetorp, L.; Gröntoft, O.; Lundström, B.; Månson, J.C.; et al. Reduction in mortality from breast cancer after mass screening with mammography. Randomised trial from the Breast Cancer Screening Working Group of the Swedish National Board of Health and Welfare. Lancet 1985, 829–832. [Google Scholar] [CrossRef] [PubMed]
- Andersson, I.; Aspegren, K.; Janzon, L.; Landberg, T.; Lindholm, K.; Linell, F.; Ljungberg, O.; Ranstam, J.; Sigfusson, B. Mammographic screening and mortality from breast cancer: The Malmö mammographic screening trial. BMJ 1988, 297, 943–948. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, S. Periodic screening for breast cancer: The HIP randomized controlled trial. Health Insurance Plan. J. Natl. Cancer Inst. Monogr. 1997, 27–30. [Google Scholar] [CrossRef] [PubMed]
- Nyström, L.; Wall, S.; Rutqvist, L.E.; Lindgren, A.; Lindqvist, M.; Rydén, S.; Andersson, J.; Bjurstam, N.; Fagerberg, G.; Frisell, J.; et al. Breast cancer screening with mammography: Overview of Swedish randomised trials. Lancet 1993, 341, 973–978. [Google Scholar] [CrossRef]
- Frisell, J.; Lidbrink, E.; Hellström, L.; Rutqvist, L.E. Followup after 11 years--update of mortality results in the Stockholm mammographic screening trial. Breast Cancer Res. Treat. 1997, 45, 263–270. [Google Scholar] [CrossRef]
- Alexander, F.E.; Anderson, T.J.; Brown, H.K.; Forrest, A.P.M.; Hepburn, W.; Kirkpatrick, A.E.; Muir, B.B.; Prescott, R.J.; Smith, A. 14 years of follow-up from the Edinburgh randomised trial of breast-cancer screening. Lancet 1999, 353, 1903–1908. [Google Scholar] [CrossRef]
- Malek, D.; Rabe, P.; Bock, K. Ergebnisse des Mammographie-Screening-Programms in Deutschland; Evaluationsbericht 2005–2007. Koop. Mammographie 2014, 1–156. Available online: https://www.g-ba.de/downloads/17-98-2731/2009-09-21-Evaluationsbericht.pdf (accessed on 15 December 2014).
- Perry, N.; Broeders, M.; de Wolf, C.; Törnberg, S.; Holland, R.; von Karsa, L. European guidelines for quality assurance in breast cancer screening and diagnosis. Fourth edition--summary document. Oncol. Clin. Pract. 2008, 19, 614–622. [Google Scholar] [CrossRef]
- Lee, K.; Lim, H.T.; Park, S.M. Factors associated with use of breast cancer screening services by women aged ≥ 40 years in Korea: The Third Korea National Health and Nutrition Examination Survey 2005 (KNHANES III). BMC Cancer 2010, 10, 144. [Google Scholar] [CrossRef]
- Esteva, M.; Ripoll, J.; Leiva, A.; Sánchez-Contador, C.; Collado, F. Determinants of non attendance to mammography program in a region with high voluntary health insurance coverage. BMC Public Health 2008, 8, 387. [Google Scholar] [CrossRef] [PubMed]
- Kjellén, M.; von Euler-Chelpin, M. Socioeconomic status as determinant for participation in mammography screening: Assessing the difference between using women’s own versus their partner’s. Int. J. Public Health 2010, 55, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Banks, E.; Beral, V.; Cameron, R.; Hogg, A.; Langley, N.; Barnes, I.; Bull, D.; Reeves, G.; English, R.; Taylor, S.; et al. Comparison of various characteristics of women who do and do not attend for breast cancer screening. Breast Cancer Res. 2002, 4, R1. [Google Scholar] [CrossRef] [PubMed]
- Lagerlund, M.; Maxwell, A.E.; Bastani, R.; Thurfjell, E.; Ekbom, A.; Lambe, M. Sociodemographic predictors of non-attendance at invitational mammography screening--a population-based register study (Sweden). Cancer Causes Control 2002, 13, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Bulliard, J.-L.; de Landtsheer, J.-P.; Levi, F. Profile of women not attending in the Swiss Mammography Screening Pilot Programme. Breast 2004, 13, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Dundar, P.E.; Ozyurt, B.C.; Erdurak, K. Sociodemographic Determinants of Nonattendance in a Population-Based Mammography Screening Program in the City of Manisa, Turkey. Sci. World J. 2012. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zackrisson, S.; Andersson, I.; Manjer, J.; Janzon, L. Non-attendance in breast cancer screening is associated with unfavourable socio-economic circumstances and advanced carcinoma. Int. J. Cancer. 2004, 108, 754–760. [Google Scholar] [CrossRef]
- Kinnear, H.; Connolly, S.; Rosato, M.; Hall, C.; Mairs, A.; O’Reilly, D. Are caregiving responsibilities associated with non-attendance at breast screening? BMC Public Health 2010, 10, 749. [Google Scholar] [CrossRef]
- Flamant, C.; Gauthier, E.; Clavel-Chapelon, F. Determinants of non-compliance to recommendations on breast cancer screening among women participating in the French E3N cohort study. Eur. J. Cancer Prev. 2006, 15, 27–33. [Google Scholar] [CrossRef][Green Version]
- Baré, M.L.; Montes, J.; Florensa, R.; Sentís, M.; Donoso, L. Factors related to non-participation in a population-based breast cancer screening programme. Eur. J. Cancer Prev. 2003, 12, 487–494. [Google Scholar] [CrossRef]
- Aro, A.R.; de Koning, H.J.; Absetz, P.; Schreck, M. Two distinct groups of non-attenders in an organized mammography screening program. Breast Cancer Res. Treat. 2001, 70, 145–153. [Google Scholar] [CrossRef]
- Fleming, P.; O’Neill, S.; Owens, M.; Mooney, T.; Fitzpatrick, P. Intermittent Attendance at Breast Cancer Screening. J. Public Health Res. 2013. [Google Scholar] [CrossRef] [PubMed]
- Duijm, L.E.; Guit, G.L.; Zaat, J.O. Mammographic surveillance of asymptomatic breast cancer relatives in general practice: Rate of re-attendance and GP- and patient-related barriers. Fam. Pract. 1997, 14, 450–454. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Munn, E.M. Nonparticipation in mammography screening: Apathy, anxiety or cost? N. Z. Med. J. 1993, 106, 284–286. [Google Scholar] [PubMed]
- Lostao, L.; Joiner, T.E.; Pettit, J.W.; Chorot, P.; Sandín, B. Health beliefs and illness attitudes as predictors of breast cancer screening attendance. Eur. J. Public Health 2001, 11, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Donato, F.; Bollani, A.; Spiazzi, R.; Soldo, M.; Pasquale, L.; Monarca, S.; Lucini, L.; Nardi, G. Factors associated with non-participation of women in a breast cancer screening programme in a town in northern Italy. J. Epidemiol. Community Health 1991, 45, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Kee, F.; Telford, A.M.; Donaghy, P.; O’Doherty, A. Attitude or access: Reasons for not attending mammography in Northern Ireland. Eur. J. Cancer Prev. 1992, 1, 311–315. [Google Scholar] [CrossRef] [PubMed]
- McNoe, B.; Richardson, A.K.; Elwood, J.M. Factors affecting participation in mammography screening. N. Z. Med. J. 1996, 109, 359–361. [Google Scholar]
- Hegenscheid, K.; Hoffmann, W.; Fochler, S.; Domin, M.; Weiss, S.; Hartmann, B.; Bick, U.; Hosten, N. Telephone counseling and attendance in a national mammography-screening program a randomized controlled trial. Am. J. Prev. Med. 2011, 41, 421–427. [Google Scholar] [CrossRef]
- Cosp, X.B.; Castillejo, M.M.; Vila, M.P.; Marti, J.; Emparanza, J.I. Strategies for increasing the participation of women in community breast cancer screening. In Cochrane Database of Systematic Reviews; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2001; Available online: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002943/abstract (accessed on 15 June 2015).
- Davis, N.A.; Lewis, M.J.; Rimer, B.K.; Harvey, C.M.; Koplan, J.P. Evaluation of a phone intervention to promote mammography in a managed care plan. Am. J. Health Promot. 1997, 11, 247–249. [Google Scholar] [CrossRef]
- Janz, N.K.; Schottenfeld, D.; Doerr, K.M.; Selig, S.M.; Dunn, R.L.; Strawderman, M.; Levine, P.A. A two-step intervention of increase mammography among women aged 65 and older. Am. J. Public Health 1997, 87, 1683–1686. [Google Scholar] [CrossRef][Green Version]
- Costanza, M.E.; Stoddard, A.M.; Luckmann, R.; White, M.J.; Spitz Avrunin, J.; Clemow, L. Promoting mammography: Results of a randomized trial of telephone counseling and a medical practice intervention. Am. J. Prev. Med. 2000, 19, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Lipkus, I.M.; Rimer, B.K.; Halabi, S.; Strigo, T.S. Can tailored interventions increase mammography use among HMO women? Am. J. Prev. Med. 2000, 18, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Champion, V.; Maraj, M.; Hui, S.; Perkins, A.J.; Tierney, W.; Menon, U.; Skinner, C.S. Comparison of tailored interventions to increase mammography screening in nonadherent older women. Prev. Med. 2003, 36, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Vogt, T.M.; Glass, A.; Glasgow, R.E.; La Chance, P.A.; Lichtenstein, E. The safety net: A cost-effective approach to improving breast and cervical cancer screening. J. Women Health 2003, 12, 789–798. [Google Scholar] [CrossRef]
- Saywell, R.M.; Champion, V.L.; Zollinger, T.W.; Maraj, M.; Skinner, C.S.; Zoppi, K.A.; Muegge, C.M. The cost effectiveness of 5 interventions to increase mammography adherence in a managed care population. Am. J. Manag. Care. 2003, 9, 33–44. [Google Scholar] [PubMed]
- Luckmann, R.; Savageau, J.A.; Clemow, L.; Stoddard, A.M.; Costanza, M.E. A randomized trial of telephone counseling to promote screening mammography in two HMOs. Cancer Detect. Prev. 2003, 27, 442–450. [Google Scholar] [CrossRef]
- Carney, P.A.; Harwood, B.G.; Greene, M.A.; Goodrich, M.E. Impact of a telephone counseling intervention on transitions in stage of change and adherence to interval mammography screening (United States). Cancer Causes Control 2005, 16, 799–807. [Google Scholar] [CrossRef]
- King, E.S.; Rimer, B.K.; Seay, J.; Balshem, A.; Engstrom, P.F. Promoting mammography use through progressive interventions: Is it effective? Am. J. Public Health 1994, 84, 104–106. [Google Scholar] [CrossRef][Green Version]
- John, U.; Hensel, E.; Lüdemann, J.; Piek, M.; Sauer, S.; Adam, C.; Born, G.; Alte, D.; Greiser, E.; Haertel, U.; et al. Study of Health In Pomerania (SHIP): A health examination survey in an east German region: Objectives and design. Soz. Präventivmedizin 2001, 46, 186–194. [Google Scholar] [CrossRef]
- Völzke, H.; Alte, D.; Schmidt, C.O.; Radke, D.; Lorbeer, R.; Friedrich, N.; Aumann, N.; Lau, K.; Piontek, M.; Born, G.; et al. Cohort Profile: The Study of Health in Pomerania. Int. J. Epidemiol. 2011, 40, 294–307. [Google Scholar] [CrossRef]
- Prochaska, J.O.; DiClemente, C.C. Transtheoretical therapy: Toward a more integrative model of change. Psychother. Theory Res. Pract. 1982, 19, 276–288. [Google Scholar] [CrossRef]
- Rakowski, W.; Andersen, M.R.; Stoddard, A.M.; Urban, N.; Rimer, B.K.; Lane, D.S.; Fox, S.A.; Costanza, M.E. Confirmatory analysis of opinions regarding the pros and cons of mammography. Health Psychol. 1997, 16, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Rakowski, W.; Dube, C.E.; Marcus, B.H.; Prochaska, J.O.; Velicer, W.F.; Abrams, D.B. Assessing elements of women’s decisions about mammography. Health Psychol. 1992, 11, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Das Mammographie Screening-Programm. July 2015. Available online: http://www.mammo-programm.de/ (accessed on 15 October 2015).
- Gierisch, J.M.; DeFrank, J.T.; Bowling, J.M.; Rimer, B.K.; Matuszewski, J.M.; Farrell, D.; Skinner, C.S. Finding the Minimal Intervention Needed for Sustained Mammography Adherence. Am. J. Prev. Med. 2010, 39, 334–344. [Google Scholar] [CrossRef]
- Taplin, S.H.; Barlow, W.E.; Ludman, E.; MacLehos, R.; Meyer, D.M.; Seger, D.; Herta, D.; Chin, C.; Curry, S. Testing reminder and motivational telephone calls to increase screening mammography: A randomized study. J. Natl. Cancer Inst. 2000, 92, 233–242. [Google Scholar] [CrossRef]
- Baron, R.C.; Rimer, B.K.; Coates, R.J.; Kerner, J.; Kalra, G.P.; Melillo, S.; Habarta, N.; Wilson, K.M.; Chattopadhyay, S.; Leeks, K.; et al. Client-directed interventions to increase community access to breast, cervical, and colorectal cancer screening a systematic review. Am. J. Prev. Med. 2008, 35, S56–S66. [Google Scholar] [CrossRef]
- Moutel, G.; Duchange, N.; Darquy, S.; de Montgolfier, S.; Papin-Lefebvre, F.; Jullian, O.; Viguier, J.; Sancho-Garnier, H. Women’s participation in breast cancer screening in France—An ethical approach. BMC Med. Ethics 2014, 15, 64. [Google Scholar] [CrossRef]
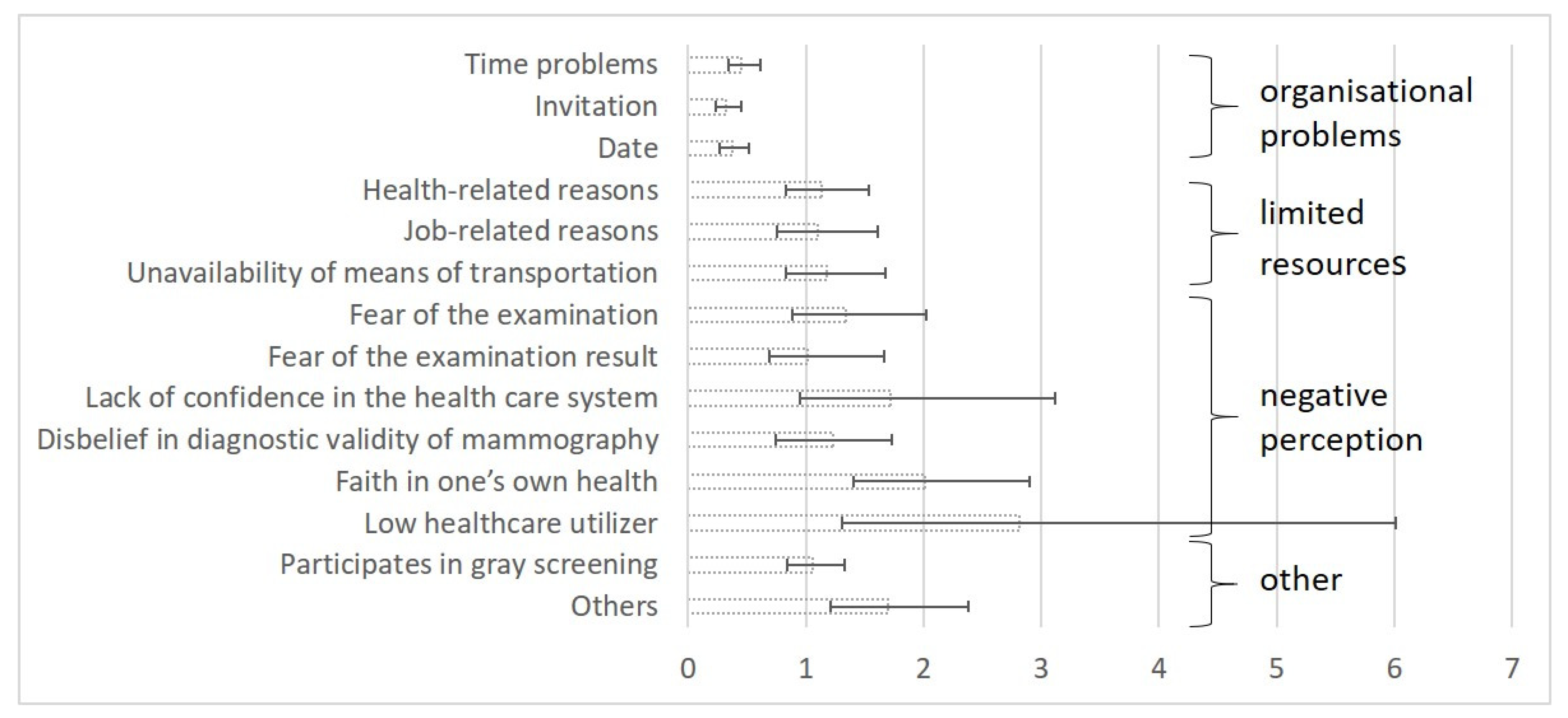
| n | % | Participants | Non-Participants | Participation Rate | OR | 95%CI | p Value | ||
|---|---|---|---|---|---|---|---|---|---|
| Controls | 2486 | 710 | 1776 | 28.56% | |||||
| Intervention group | 1494 | 685 | 809 | 45.85% | |||||
| Block 1: Organizational problems | |||||||||
| Time problems | 396 | 26.51% | 238 | 158 | 60.10% | 0.45 | 0.34 | 0.61 | <0.0001 |
| Invitation | 235 | 15.73% | 163 | 72 | 69.36% | 0.32 | 0.23 | 0.45 | <0.0001 |
| Date | 215 | 14.39% | 150 | 65 | 69.77% | 0.38 | 0.27 | 0.52 | <0.0001 |
| Block 2: Limited resources | |||||||||
| Health-related restrictions | 258 | 17.27% | 100 | 158 | 38.76% | 1.13 | 0.83 | 1.54 | 0.4229 |
| Job-related restrictions | 181 | 12.12% | 102 | 79 | 56.35% | 1.10 | 0.75 | 1.61 | 0.6372 |
| Unavailability of means of transportation | 181 | 12.12% | 66 | 115 | 36.46% | 1.18 | 0.83 | 1.68 | 0.3481 |
| Block 3: Negative perception | |||||||||
| Fear of the examination | 145 | 9.71% | 43 | 102 | 29.66% | 1.34 | 0.89 | 2.02 | 0.1628 |
| Fear of the examination result | 122 | 8.17% | 38 | 84 | 31.15% | 1.01 | 0.69 | 1.67 | 0.7554 |
| Lack of confidence in the health care system | 84 | 5.62% | 18 | 66 | 21.43% | 1.72 | 0.95 | 3.12 | 0.0730 |
| Disbelief in diagnostic validity of mammography | 147 | 9.84% | 44 | 103 | 29.93% | 1.23 | 0.74 | 1.73 | 0.5835 |
| Faith in one’s own health | 225 | 15.06% | 51 | 174 | 22.67% | 2.01 | 1.40 | 2.90 | 0.0002 |
| Low healthcare utilizer | 70 | 4.69% | 9 | 61 | 12.86% | 2.81 | 1.31 | 6.01 | 0.0078 |
| Block 4: Others | |||||||||
| Participates in gray screening | 770 | 51.54% | 354 | 416 | 45.97% | 1.06 | 0.84 | 1.33 | 0.5974 |
| Others | 251 | 16.80% | 65 | 186 | 25.90% | 1.70 | 1.21 | 2.38 | 0.0020 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fochler, S.; Weitmann, K.; Domin, M.; Hoffmann, W. Reasons for Non-Attendance in the German National Mammography Screening Program: Which Barriers Can Be Overcome Using Telephone Counseling?—A Randomized Controlled Trial. Healthcare 2023, 11, 17. https://doi.org/10.3390/healthcare11010017
Fochler S, Weitmann K, Domin M, Hoffmann W. Reasons for Non-Attendance in the German National Mammography Screening Program: Which Barriers Can Be Overcome Using Telephone Counseling?—A Randomized Controlled Trial. Healthcare. 2023; 11(1):17. https://doi.org/10.3390/healthcare11010017
Chicago/Turabian StyleFochler, Sebastian, Kerstin Weitmann, Martin Domin, and Wolfgang Hoffmann. 2023. "Reasons for Non-Attendance in the German National Mammography Screening Program: Which Barriers Can Be Overcome Using Telephone Counseling?—A Randomized Controlled Trial" Healthcare 11, no. 1: 17. https://doi.org/10.3390/healthcare11010017
APA StyleFochler, S., Weitmann, K., Domin, M., & Hoffmann, W. (2023). Reasons for Non-Attendance in the German National Mammography Screening Program: Which Barriers Can Be Overcome Using Telephone Counseling?—A Randomized Controlled Trial. Healthcare, 11(1), 17. https://doi.org/10.3390/healthcare11010017





