Intentional Replantation of Single-Rooted and Multi-Rooted Teeth: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
- P (Population): Subjects undergone Intentional Replantation of permanent teeth
- I (Intervention): Intentional Replantation of permanent teeth
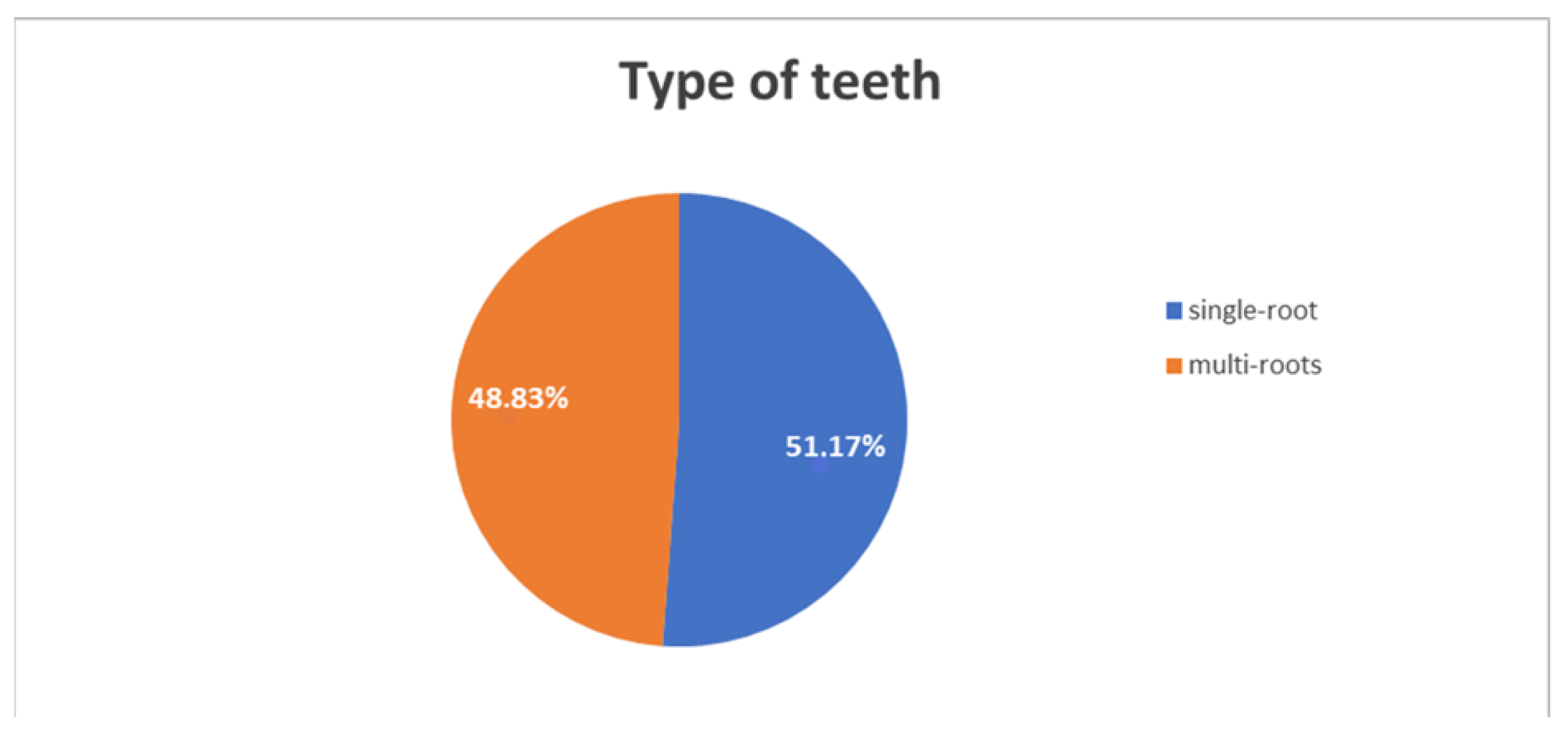
- C (Comparison): Single-rooted vs Multi-rooted replanted teeth
- O (Outcome): Intentional Replantation survival rate
2.1. Search Strategy and Study Selection
- Source: studies published in the English language from January 1996 to 1 July 2022;
- Study design: case reports, case series, analytical observational studies, trials;
- Study population: subjects undergone IR (no age nor gender restrictions);
- Study intervention: IR of single-rooted and/or multi-rooted permanent teeth; and
- Study outcomes: IR reported clinical and/or patient-related outcomes.
2.2. Data Extraction
2.3. Data Synthesis and Statistical Analysis
2.4. Quality Assessment
3. Results
3.1. Study Selection
3.2. Studies Characteristics and Synthesis of the Reported Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grossman, L.I. Intentional replantation of teeth. J. Am. Dent. Assoc. 1966, 72, 1111–1118. [Google Scholar] [CrossRef] [PubMed]
- Emmertsen, E.; Andreasen, J.O. Replantation of extracted molars. A radiographic and histological study. Acta Odontol. Scand. 1966, 24, 327–346. [Google Scholar] [CrossRef] [PubMed]
- Demiralp, B.; Nohutcu, R.M.; Tepe, D.I.; Eratalay, K. Intentional replantation for periodontally involved hopeless teeth. Dent. Traum. 2003, 19, 45–51. [Google Scholar] [CrossRef]
- Kratchman, S. Intentional replantation. Dent. Clin. N. Am. 1997, 41, 603–617. [Google Scholar] [CrossRef] [PubMed]
- Dumsha, T.C.; Gutmann, J.L. Clinical guidelines for intentional replantation. Compend. Contin. Educ. Dent. 1985, 6, 606–608. [Google Scholar]
- Iandolo, A.; Pisano, M.; Scelza, G.; Abdellatif, D.; Martina, S. Three-Dimensional Evaluation of the Root Apex of Permanent Maxillary Premolars: A Multicentric Study. Appl. Sci. 2022, 12, 6159. [Google Scholar] [CrossRef]
- Raghoebar, G.M.; Vissink, A. Results of intentional replantation of molars. J. Oral Maxillofac. Surg. 1999, 57, 240–244. [Google Scholar] [CrossRef]
- Andreasen, J. Effect of extra-alveolar period and storage media upon periodontal and periapical healing after replantation of mature permanent incisors in monkeys. Int. J. Oral Surg. 1981, 10, 43–45. [Google Scholar] [CrossRef]
- Kvint, S.; Lindsten, R.; Magnusson, A.; Nilsson, P.; Bjerklin, K. Autotransplantation of Teeth in 215 Patients. A follow-up study. Angle Orthod. 2010, 80, 446–451. [Google Scholar] [CrossRef]
- Andreasen, J.O. Relationship Between Cell Damage in the Periodontal Ligament After Replantation and Subsequent Development of Root Resorption. Acta Odontol. Scand. 1981, 39, 15–25. [Google Scholar] [CrossRef]
- Kingsbury, B.C., Jr.; Wiesenbaugh, J.M., Jr. Intentional replantation of mandibular premolars and molars. J. Am. Dent. Assoc. 1971, 1053–1057. [Google Scholar] [CrossRef] [PubMed]
- Becker, B.D. Intentional Replantation Techniques: A Critical Review. J. Endod. 2018, 44, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Guy, S.C.; Goerig, A.C. Intentional replantation: Technique and rationale. Quintessence Int. Dent. Dig. 1984, 15, 595–603. [Google Scholar] [PubMed]
- Tewari, A.; Chawla, H. Intentional replantation of pulpal or periapically involved permanent posterior teeth. J. Indian Dent. Assoc. 1974, 46, 385–389. [Google Scholar]
- Bender, I.; Rossman, L.E. Intentional replantation of endodontically treated teeth. Oral Surg. Oral Med. Oral Pathol. 1993, 76, 623–630. [Google Scholar] [CrossRef]
- Messkoub, M. Intentional replantation: A successful alternative for hopeless teeth. Oral Surg. Oral Med. Oral Pathol. 1991, 71, 743–747. [Google Scholar] [CrossRef]
- D’Angelo, M.; Zanza, A.; Testarelli, L.; Valenti Obino, F.; Cicconetti, A. In Silico Novel Drug Design Targeting the Oral Microbiome: Endodontic and Periodontal Pathogenic Bacteria. Microorganisms 2021, 9, 2400. [Google Scholar] [CrossRef]
- Kharouf, N.; Sauro, S.; Jmal, H.; Eid, A.; Karrout, M.; Bahlouli, N.; Haikel, Y.; Mancino, D. Does Multi-Fiber-Reinforced Composite-Post Influence the Filling Ability and the Bond Strength in Root Canal? Bioengineering 2021, 8, 195. [Google Scholar] [CrossRef]
- Peer, M. Intentional replantation—A ‘last resort’ treatment or a conventional treatment procedure? Nine case reports. Dent. Traumatol. 2004, 20, 48–55. [Google Scholar] [CrossRef]
- Kharouf, N.; Pedullà, E.; La Rosa, G.R.M.; Bukiet, F.; Sauro, S.; Haikel, Y.; Mancino, D. In Vitro Evaluation of Different Irrigation Protocols on Intracanal Smear Layer Removal in Teeth with or without Pre-Endodontic Proximal Wall Restoration. J. Clin. Med. 2020, 9, 3325. [Google Scholar] [CrossRef]
- Barnett, R.J.; Burton, W.E.; Nuckles, D.B. Intentional replantation: Report of a successful case. Quintessence Int. 1992, 23, 755–757. [Google Scholar] [PubMed]
- Iandolo, A.; Amato, A.; Martina, S.; Latif, D.A.; Pantaleo, G. Management of Severe Curvatures in Root Canal Treatment with the New Generation of Rotating Files Using a Safe and Predictable Protocol. Open Dent. J. 2020, 14, 421–425. [Google Scholar] [CrossRef]
- Martina, S.; Pisano, M.; Amato, A.; Abdellatif, D.; Iandolo, A. Modern rotary files in minimally invasive endodontics: A case report. Front. Biosci. 2021, 13, 299. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, 7. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.-L.; Wang, Y.-Y.; Yang, Z.-H.; Huang, D.; Weng, H.; Zeng, X.-T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Mil. Med. Res. 2020, 7, 7. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Tang, P.M.; Chan, C.P.; Huang, S.K.; Huang, C.C. Intentional replantation for iatrogenic perforation of the furcation: A case report. Quintessence Int. 1996, 27, 691–696. [Google Scholar]
- Poi, W.R.; Sonoda, C.K.; Salineira, S.L.; Martin, S.C. Treatment of root perforation by intentional reimplantation: A case report. Dent. Traumatol. 1999, 15, 132–134. [Google Scholar] [CrossRef]
- Aqrabawi, J. Five-year Follow-up of Successful Intentional Replantation. Dent. Update 1999, 26, 388–390. [Google Scholar] [CrossRef]
- Benenati, F.W. Intentional replantation of a mandibular second molar with long-term follow-up: Report of a case. Dent. Traumatol. 2003, 19, 233–236. [Google Scholar] [CrossRef] [PubMed]
- Fariniuk, L.F.; Ferreira, E.L.; Soresini, G.C.; Cavali, A.E.; BarattoFilho, F. Intentional replantation with 180 degrees rotation of a crown-root fracture: A case report. Dent. Traumatol. 2003, 19, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Ward, J. Intentional Replantation of A Lower Premolar. Aust. Endod. J. 2004, 30, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Shintani, S.; Tsuji, M.; Toyosawa, S.; Ooshima, T. Intentional replantation of an immature permanent lower incisor because of a refractory peri-apical lesion: Case report and 5-year follow-up. Int. J. Paediatr. Dent. 2004, 14, 218–222. [Google Scholar] [CrossRef] [PubMed]
- BarattoFilho, F.; Vanni, J.R.; Limongi, O.; Farinuk, L.F.; Travassos, R.S.; Albuquerque, D. Intentional replantation: Case report of an alternative treatment for endodontic therapy failure. RSBO Rev. Sul-Bras. Odontol. 2004, 1, 36–40. [Google Scholar]
- Cotter, M.R.; Panzarino, J. Intentional Replantation: A Case Report. J. Endod. 2006, 32, 579–582. [Google Scholar] [CrossRef]
- Herrera, H.; Leonardo, M.R.; Herrera, H.; Miralda, L.; Bezerra da Silva, R.A. Intentional replantation of a mandibular molar: Case report and 14-year follow-up. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 102, e85-7. [Google Scholar] [CrossRef]
- Martins, W.D.; Westphalen, V.P.D.; Perin, C.P.; Neto, U.X.D.S.; Westphalen, F.H. Treatment of extrusive luxation by intentional replantation. Int. J. Paediatr. Dent. 2007, 17, 134–138. [Google Scholar] [CrossRef]
- Peñarrocha, M.; García, B.; Martí, E.; Palop, M.; von Arx, T. Intentional replantation for the management of maxillary sinusitis. Int. Endod. J. 2007, 40, 891–899. [Google Scholar] [CrossRef]
- Demir, B.; Demiralp, B.; Güncü, G.N.; Uyanık, M.; Caglayan, F. Intentional replantation of a hopeless tooth with the combination of platelet rich plasma, bioactive glass graft material and non-resorbable membrane: A case report. Dent. Traumatol. 2007, 23, 190–194. [Google Scholar] [CrossRef]
- Sivolella, S.; Bressan, E.; Mirabal, V.; Stellini, E.; Berengo, M. Extraoral endodontic treatment, odontotomy and intentional replantation of a double maxillary lateral permanent incisor: Case report and 6-year follow-up. Int. Endod. J. 2008, 41, 538–546. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Heffernan, M.; Vann, W.F. Management of a complicated crown-root fracture in a young permanent incisor using intentional replantation. Dent. Traumatol. 2008, 24, 100–103. [Google Scholar] [CrossRef] [PubMed]
- Al-Hezaimi, K.; Naghshbandi, J.; Simon, J.H.; Rotstein, I. Successful treatment of a radicular groove by intentional replantation and Emdogain therapy: Four years follow-up. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2009, 107, e82–e85. [Google Scholar] [CrossRef]
- Bittencourt, G.; Almeida, F.; Roldi, A.; Graziella, S.; Bittencourt, F.; Avio, X.; Almeida, A. Intentional replantation with tooth rotation as indication for treatment of crown-root fractures. Braz. J. Dent. Traumatol. 2009, 1824, 2–657. [Google Scholar]
- Özer, S.Y.; Ünlü, G.; Değer, Y. Diagnosis and treatment of endodontically treated teeth with vertical root fracture: Three case reports with two-year follow-up. J. Endod. 2011, 37, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.H.; Lu, H.C.; Ke, J.H.; Lan, W.H. Laser assisted tooth replantation—Case report. Laser Ther. 2011, 20, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Unver, S.; Onay, E.O.; Ungor, M. Intentional re-plantation of a vertically fractured tooth repaired with an adhesive resin. Int. Endod. J. 2011, 44, 1069–1078. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.-S.; Shin, D.R.; Choi, G.-W.; Park, S.H.; Lee, J.W.; Kim, S.-Y. Management of complicated crown-root fractures using intentional replantation: Two case reports. Dent. Traumatol. 2011, 29, 334–337. [Google Scholar] [CrossRef] [PubMed]
- Moura, L.F.A.D.; Lima, M.D.M.; Moura, M.S.; Carvalho, P.V.; Cravinhos, J.C.P.; Carvalho, C.M.R.S. Treatment of a crown-root fracture with intentional replantation—Case report with 16-year follow-up. Int. Endod. J. 2012, 45, 955–960. [Google Scholar] [CrossRef]
- Dogan, M.C.; Akgun, E.O.; Yoldaş, H.O. Adhesive tooth fragment reattachment with intentional replantation: 36-month follow-up. Dent. Traumatol. 2012, 29, 238–242. [Google Scholar] [CrossRef]
- Shin, Y.; Kim, Y.; Roh, B.-D. Maxillary first molar with an O-shaped root morphology: Report of a case. Int. J. Oral Sci. 2013, 5, 242–244. [Google Scholar] [CrossRef] [PubMed]
- Yuan, L.-T.; Duan, D.-M.; Tan, L.; Wang, X.-J.; Wu, L.-A. Treatment for a complicated crown-root fracture with intentional replantation: A case report with a 3.5-year follow up. Dent. Traumatol. 2012, 29, 474–478. [Google Scholar] [CrossRef] [PubMed]
- Nagappa, G.; Aspalli, S.; Devanoorkar, A.; Shetty, S.; Parab, P. Intentional replantation of periodontally compromised hopeless tooth. J. Indian Soc. Periodontol. 2013, 17, 665–669. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Logani, A.; Shah, N. Intentional replantation: A viable alternative for management of palatogingival groove. Saudi Endod. J. 2013, 3, 90. [Google Scholar] [CrossRef]
- Moradi Majd, N.; Akhtari, F.; Araghi, S.; Homayouni, H. Treatment of a vertical root fracture using dual-curing resin cement: A case report. Case Rep. Dent. 2012, 2012, 985215. [Google Scholar] [CrossRef]
- Sübay, R.K.; Sübay, M.O.; Balkaya, C.M. Intentional replantation of a mandibular canine with multiple iatrogenic endodontic complications. Oral Health Dent. Manag. 2014, 13, 811–814. [Google Scholar]
- Asgary, S.; AlimMarvasti, L.; Kolahdouzan, A. Indications and case series of intentional replantation of teeth. Iran Endod. J. 2014, 9, 71–78. [Google Scholar]
- Asgary, S.; Nosrat, A. Concurrent intentional replantation of maxillary molars using a novel root-end filling. Gen. Dent. 2014, 62. [Google Scholar]
- Majd, N.M.; Arvin, A.; Darvish, A.; Aflaki, S.; Homayouni, H. Treatment of Necrotic Calcified Tooth Using Intentional Replantation Procedure. Case Rep. Dent. 2014, 2014, 793892. [Google Scholar] [CrossRef]
- Peñarrocha-Diago, M.A.; Aloy-Prósper, A.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M. Replantation of a maxillary second molar after removal of a third molar with a dentigerous cyst: Case report and 12-month follow-up. J. Clin. Exp. Dent. 2014, 6, 185–188. [Google Scholar] [CrossRef]
- Tsesis, I.; Taschieri, S.; Rosen, E.; Corbella, S.; Fabbro, M. Treatment of paraesthesia following root canal treatment by intentional tooth replantation: A review of the literature and a case report. Indian J. Dent. Res. 2014, 25, 231–235. [Google Scholar] [PubMed]
- Keceli, H.G.; Hendek, M.K. Fifteen months follow-up of a hopeless tooth treated with two-step procedure involving intentional replantation and free gingival graft. Eur. J. Dent. 2014, 8, 559–562. [Google Scholar] [CrossRef] [PubMed]
- Pruthi, P.J.; Dharmani, U.; Roongta, R.; Talwar, S. Management of external perforating root resorption by intentional replantation followed by Biodentine restoration. Dent. Res. J. 2015, 12, 488–493. [Google Scholar] [CrossRef]
- Dua, D. Reconstruction and Intentional Replantation of a Maxillary Central Incisor with A Complete Vertical Root Fracture: A Rare Case Report with Three Years Follow up. J. Clin. Diagn. Res. 2015, 9, ZD06–9. [Google Scholar] [CrossRef] [PubMed]
- Forero-López, J.; Gamboa-Martínez, L.; Pico-Porras, L.; Niño-Barrera, J.L. Surgical management with intentional replantation on a tooth with palato-radicular groove. Restor. Dent. Endod. 2015, 40, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Garrido, I.; Abella, F.; Ordinola-Zapata, R.; Duran-Sindreu, F.; Roig, M. Combined Endodontic Therapy and Intentional Replantation for the Treatment of Palatogingival Groove. J. Endod. 2015, 42, 324–328. [Google Scholar] [CrossRef]
- Muhamad, A.H.; Azzaldeen, A. Intentional replantation of maxillary second molar; case report and 15-year follow-up. IOSR J. Dent. Med. 2016, 15, 67–73. [Google Scholar]
- Oishi, A. Intentional Replantation of an Immature Incisor with a Transverse Root Fracture and Endo-Perio Condition: 4 Year Follow-Up. J. Clin. Pediatr. Dent. 2017, 41, 187–192. [Google Scholar] [CrossRef]
- Grzanich, D.; Rizzo, G.; Silva, R.M. Saving Natural Teeth: Intentional Replantation—Protocol and Case Series. J. Endod. 2017, 43, 2119–2124. [Google Scholar] [CrossRef]
- Eshghi, A.; Faghihian, R.; Mosleh, H.; Akhlaghi, N. Management of complicated crown-root fracture in central incisors using intentional replantation with 180° rotation: A case report. Dent. Hypotheses 2017, 8, 113. [Google Scholar] [CrossRef]
- Maniglia-Ferreira, C.; Gomes, F.D.A.; Vitoriano, M.D.M. Intentional Replantation of an Avulsed Immature Permanent Incisor: A Case Report. J. Endod. 2017, 43, 1383–1386. [Google Scholar] [CrossRef] [PubMed]
- Thaore, S.; Desai, N.; Srinidhi, S.R.; Balsaraf, O. Intentional Replantation of an Endodontically Treated Tooth with Separated Instrument: A Case Report. Saudi J. Oral. Dent. Res. 2017, 2, 59–62. [Google Scholar]
- Asgary, S.; Roghanizadeh, L. Rapid Bone Healing after Intentional Replantation of a Molar with Apical Actinomycosis. Iran Endod. J. 2018, 13, 135–138. [Google Scholar] [PubMed]
- Zafar, K.; Badar, S.B.; Khan, F.R. Intentional Replantation in a Maxillary Molar with Undesirable Root Fracture: A Case Report. J. Pak. Dent. Assoc. 2018, 26, 132–136. [Google Scholar] [CrossRef]
- Yaqoob, S.K.M. Intentional Replantation of Endodontically Treated Tooth—A Case Report. Open Access J. Dent. Sci. 2018, 3, 1. [Google Scholar] [CrossRef]
- Krug, R.; Soliman, S.; Krastl, G. Intentional Replantation with an Atraumatic Extraction System in Teeth with Extensive Cervical Resorption. J. Endod. 2019, 45, 1390–1396. [Google Scholar] [CrossRef]
- Deshpande, N.M.; Shah, D.; Wadekar, S. Maintenance of cell viability in extraoral conditions for a case of intentional replantation to retrieve a separated endodontic instrument. J. Conserv. Dent. 2019, 22, 207–212. [Google Scholar] [CrossRef]
- Ong, T.K. Non-surgical Retreatment after Failed Intentional Replantation: A Case Report. Eur. Endod. J. 2019, 4, 145–149. [Google Scholar] [CrossRef]
- Yan, H.; Xu, N.; Wang, H.; Yu, Q. Intentional Replantation with a 2-segment Restoration Method to Treat Severe Palatogingival Grooves in the Maxillary Lateral Incisor: A Report of 3 Cases. J. Endod. 2019, 45, 1543–1549. [Google Scholar] [CrossRef]
- Cunliffe, J.; Ayub, K.; Darcey, J.; Foster-Thomas, E. Intentional replantation—A clinical review of cases undertaken at a major UK dental school. Br. Dent. J. 2020, 229, 230–238. [Google Scholar] [CrossRef]
- Asgary, S.; Talebzadeh, B. Intentional replantation of a molar with several endodontic complications. J. Stomatol. Oral Maxillofac. Surg. 2018, 120, 489–492. [Google Scholar] [CrossRef] [PubMed]
- Fujii, R.; Morinaga, K.; Asai, T.; Aida, N.; Yamada, M.; Sako, R.; Furusawa, M. Intentional Replantation to Treat Apical Periodontitis of Maxillary First Molar with Foreign Body Located Outside Apical Foramen Using CBCT: A Case Report. Bull. Tokyo Dent. Coll. 2020, 61, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Ganapathy, S.; Vedam, V.; Rajeev, V.; Nair, S.V. Intentional replantation with 180° rotation of a complicated crown-root fracture: A Case Report. Trauma Case Rep. 2020, 27, 100306. [Google Scholar] [CrossRef] [PubMed]
- Lodha, S.S.; Nanda, Z.; Deore, R.; Reddy, K.; Raghavendra, S.S.; Mundada, A. An endodontic challenge managed by intentional replantation: A case report. Int. J. Appl. Dent. Sci. 2020, 6, 10–13. [Google Scholar]
- Yang, Y.; Zhang, B.; Huang, C.; Ye, R. Intentional Replantation of a Second Premolar with Internal Resorption and Root Fracture: A Case Report. J. Contemp. Dent. Pract. 2021, 22, 562–567. [Google Scholar] [CrossRef]
- Shekhawat, D.; Sharma, N.; Emmanuel, B.J.; Narwat, S. Intentional replantation of a tooth with separated instrument: A case report. Int. J. Med. Dent. Case Rep. 2021, 11, 1–3. [Google Scholar] [CrossRef]
- Plotino, G.; Abella Sans, F.; Duggal, M.; Grande, N.; Krastl, G.; Nagendrababu, V.; Gambarini, G. Clinical procedures and outcome of surgical extrusion, intentional replantation and tooth autotransplantation—A narrative review. Int. Endod. J. 2020, 53, 1636–1652. [Google Scholar] [CrossRef]
- Torabinejad, M.; Dinsbach, N.A.; Turman, M.; Handysides, R.; Bahjri, K.; White, S.N. Survival of Intentionally Replanted Teeth and Implant-supported Single Crowns: A Systematic Review. J. Endod. 2015, 41, 992–998. [Google Scholar] [CrossRef]
- Jang, Y.; Lee, S.-J.; Yoon, T.-C.; Roh, B.-D.; Kim, E. Survival Rate of Teeth with a C-shaped Canal after Intentional Replantation: A Study of 41 Cases for up to 11 Years. J. Endod. 2016, 42, 1320–1325. [Google Scholar] [CrossRef]
- Sangiovanni, G.; Scelza, G.; Giordano, F.; Chiacchio, A.; Ferrigno, R.; Rengo, C.; Pisano, M. Intentional replantation in Endodontics: Review of literature. G. Ital. Endod. 2022, 36, 97–102. [Google Scholar] [CrossRef]
- Pantaleo, G.; Amato, A.; Iandolo, A.; Abdellatif, D.; Di Spirito, F.; Caggiano, M.; Pisano, M.; Blasi, A.; Fornara, R.; Amato, M. Two-Year Healing Success Rates after Endodontic Treatment Using 3D Cleaning Technique: A Prospective Multicenter Clinical Study. J. Clin. Med. 2022, 11, 6213. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.-Y.; Chen, G. A long-term treatment outcome of intentional replantation in Taiwanese population. J. Formos. Med. Assoc. 2020, 120, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Rohof, E.C.M.; Kerdijk, W.; Jansma, J.; Livas, C.; Ren, Y. Autotransplantation of teeth with incomplete root formation: A systematic review and meta-analysis. Clin. Oral Investig. 2018, 22, 1613–1624. [Google Scholar] [CrossRef] [PubMed]
- Shahbazian, M.; Jacobs, R.; Wyatt, J.; Denys, D.; Lambrichts, I.; Vinckier, F.; Willems, G. Validation of the cone beam computed tomography–based stereolithographic surgical guide aiding autotransplantation of teeth: Clinical case–control study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 115, 667–675. [Google Scholar] [CrossRef]
- Di Spirito, F.; Pelella, S.; Argentino, S.; Sisalli, L.; Sbordone, L. Oral manifestations and the role of the oral healthcare workers in COVID-19. Oral Dis. 2020, 28, 1003–1004. [Google Scholar] [CrossRef]
- Di Spirito, F.; Iacono, V.J.; Alfredo, I.; Alessandra, A.; Sbordone, L.; Lanza, A. Evidence-based Recommendations on Periodontal Practice and the Management of Periodontal Patients During and After the COVID-19 Era: Challenging Infectious Diseases Spread by Airborne Transmission. Open Dent. J. 2021, 15, 325–336. [Google Scholar] [CrossRef]
- Di Spirito, F.; Pisano, M.; Caggiano, M.; Bhasin, P.; Giudice, R.L.; Abdellatif, D. Root Canal Cleaning after Different Irrigation Techniques: An Ex Vivo Analysis. Medicina 2022, 58, 193. [Google Scholar] [CrossRef]
- Kaku, M.; Shimasue, H.; Ohtani, J.; Kojima, S.; Sumi, H.; Shikata, H.; Kojima, S.; Motokawa, M.; Abonti, T.R.; Kawata, T.; et al. A case of tooth autotransplantation after long-term cryopreservation using a programmed freezer with a magnetic field. Angle Orthod. 2015, 85, 518–524. [Google Scholar] [CrossRef]
- Iandolo, A.; Abdellatif, D.; Amato, A.; Calapaj, M.; Pisano, M. A novel modified obturation technique using biosealers: An ex vivo study. J. Conserv. Dent. 2021, 24, 369. [Google Scholar] [CrossRef]
- Dioguardi, M.; Stellacci, C.; La Femina, L.; Spirito, F.; Sovereto, D.; Laneve, E.; Manfredonia, M.F.; D’Alessandro, A.; Ballini, A.; Cantore, S.; et al. Comparison of Endodontic Failures between Nonsurgical Retreatment and Endodontic Surgery: Systematic Review and Meta-Analysis with Trial Sequential Analysis. Medicina 2022, 58, 894. [Google Scholar] [CrossRef]
- Iandolo, A.; Abdellatif, D.; Pantaleo, G.; Sammartino, P.; Amato, A. Conservative shaping combined with three-dimensional cleaning can be a powerful tool: Case series. J. Conserv. Dent. 2020, 23, 648–652. [Google Scholar] [CrossRef] [PubMed]


| Source | Participants’ Gender Age | Treated Teeth | Extra-Alveolar Time Stay | Extra-Alveolar Conditions Management | IR Indication(s) | IR Outcomes | IR Follow-Up |
|---|---|---|---|---|---|---|---|
| Tang 1996 [28] | Male 29 y.o. | 3.6 MR | - | - | Iatrogenic root furcation perforation | Survival | 17 months |
| Poi 1999 [29] | Male 30 y.o. | 4.5 SR | - | - | Instrument separation/Root perforation | Survival | 8 years |
| Aqrabawi 1999 [30] Case 1 | Female 46 y.o. | 3.7 MR | 15 min | - | Endodontic failure/Apical periodontitis | Survival | 5 years |
| Aqrabawi Case 2 | Female 38 y.o. | 3.7 MR | 20 min | - | Endodontic failure/Apical periodontitis | Survival | 5 years |
| Benenati 2003 [31] | Female 45 y.o. | 4.7 MR | - | - | Pain | Survival | 16 years |
| Fariniuk 2003 [32] | Male 11 y.o. | 1.1 SR | - | - | Crown-root fracture | Survival | 3 years |
| Ward 2004 [33] | Female 68 y.o. | 3.4 SR | 15 min | - | Apical periodontitis | Survival | 18 months |
| Shintani 2004 [34] | Male 7 y.o. | 3.1 SR | 10 min | - | Apical periodontitis with coronal fracture | Survival | 5 years |
| Peer 2004 Case 1 [19] | Male 47 y.o. | 3.5 SR | - | - | Apical periodontitis | Survival | 30 months |
| Peer 2004 Case 3 | Male 70 y.o. | 3.2 SR | - | - | Apical periodontitis/sinus tract | Survival | 4 years |
| Peer 2004 Case 4 | Male 40 y.o. | 3.7 MR | - | - | Apical periodontitis/sinus tract | Failure | 7 years |
| BarattoFilho 2004 [35] | Male 36 y.o. | 2.7 MR | 15 min | - | Apical periodontitis/Instrument separation | Survival | 5 years |
| Cotter 2006 [36] | Female 47 y.o. | 3.1 SR | 5 min | - | Apical periodontitis | Survival | 1 years |
| Herrera 2006 [37] | Female 56 y.o. | 4.6 MR | 30 min | - | Apical periodontitis/endodontic failure | Survival | 14 years |
| Martins [38] | Female 15 y.o. | 2.1 SR | 10 min | - | Traumatic avulsion | Survival | 3 years |
| Penarrocha 2007 [39] | Female 20 y.o. | 2.6 MR | 5 min | - | Odontogenic maxillary sinusitis | Survival | 2 years |
| Demir 2007 [40] | Male 45 y.o. | 4.1 SR | - | - | Severe periodontitis | Survival | 1 year |
| Sivolella 2008 [41] | Male 9 y.o. | 1.2 SR | 20 min | - | Double tooth | Survival | 6 years |
| Wang 2008 [42] | Female 8 y.o. | 1.1 SR | 15 min | - | Complicated crown-root fracture | Failure | 3 months |
| Al-Hezaimi 2009 [43] | Female 15 y.o. | 1.2 SR | - | - | Pulp necrosis with suppurative apical periodontitis | Survival | 4 years |
| Bittencourt 2009 [44] | Male 9 y.o. | 2.1 SR | - | - | Complicated crown-root fracture | Survival | 2 years |
| Ozer 2010 [45] Case 1 | Male 36 y.o. | 1.1 SR 1.2 SR | (1.1) 12 min (1.2) 16 min | - | Vertical root fracture | Survival | 2 years |
| Ozer Case 2 | Female 25 y.o. | 2.2 SR | 18 min | - | Vertical root fracture | Survival | 2 years |
| Ozer Case 3 | Male 32 y.o. | 1.3 SR | 24 min | - | Vertical root fracture | Survival | 2 years |
| Hsiang Lu 2011 [46] | Male 50 y.o. | 4.6 MR | 13 min | - | Apical periodontitis | Survival | 3 months |
| Unver 2011 [47] | Female 41 y.o. | 1.4 MR | 25 min | - | Vertical fracture | Survival | 36 months |
| Kim 2011 [48] Case 1 | Female 23 y.o. | 1.1 SR 2.1 SR 2.2 SR | - | - | Complicated crown-root fractures | Failure Survival Survival | 90 months |
| Kim 2011 Case 2 | Female 27 y.o. | 2.1 SR | - | - | Complicated crown-root fracture | Survival | 24 months |
| Moura 2012 [49] | Female 11 y.o. | 1.1 SR | - | - | Complicated crown-root fracture | Failure | 2 years |
| Dogan 2013 [50] | Female 9 y.o | 2.1 SR | 28 min | - | complicated crown-root fracture | Survival | 3 years |
| Shin 2013 [51] | Male 39 y.o. | 4.6 MR | 17 min | - | Apical periodontitis | Survival | 9 months |
| Yuan 2013 [52] | Female 11 y.o. | 2.1 SR | - | - | Complicated crown-root fracture | Survival | 3.5 years+ |
| Nagappa 2013 [53] Case 1 | Female 18 y.o. | 1.1 SR | - | - | Severe periodontitis | Failure | 3 months |
| Nagappa Case2 | Male 24 y.o. | 2.1 SR | - | - | Severe periodontitis | Survival | 14 months |
| Kumar 2013 [54] | Male 26 y.o. | 2.2 SR | 8 min | - | Apical periodontitis/endodontic failure | Survival | 1 year |
| MoradiMajd 2012 [55] | Female 44 y.o. | 3.5 SR | - | - | Apical periodontitis/necrotic tooth | Survival | 1 year |
| Subay 2014 [56] | Female 45 y.o. | 4.3 SR | 14 min | - | Apical periodontitis/Instrument separation | Survival | 24 months |
| Asgary 2014 [57] Case 1 | Male 25 y.o. | 4.6 MR | 14 min | - | Apical periodontitis | Survival | 23 months |
| Asgary Case 2 | Male 45 y.o. | 3.4 SR | 10 min | - | Apical periodontitis | Survival | 30 months |
| Asgary Case 3 | Male 41 y.o. | 4.7 MR | 8 min | - | Apical periodontitis | Survival | 24 months |
| Asgary Case 4 | Male 23 y.o. | 4.6 MR | 12 min | - | Apical periodontitis | Survival | 15 months |
| Asgary Case 5 | Female 46 y.o. | 4.7 MR | 8 min | - | Apical periodontitis | Survival | 27 months |
| Asgary Case 6 | Female 31 y.o. | 4.7 MR | 9 min | - | Apical periodontitis | Survival | 12 months |
| Asgary Case 7 | Female 30 y.o. | 1.4 MR | 10 min | - | Apical periodontitis | Failure | 18 months |
| Asgary Case 8 | Female 36 y.o. | 3.6 MR | 13 min | - | Apical periodontitis | Survival | 14 months |
| Asgary Case 9 | Male 48 y.o. | 4.7 MR | 14 min | - | Apical periodontitis | Survival | 16 months |
| Asgary Case 10 | Female 24 y.o. | 4.6 MR | 14 min | - | Apical periodontitis | Survival | 8 months |
| Asgary Case 11 | Female 43 y.o. | 2.6 MR | 14 min | - | Apical periodontitis | Survival | 17 months |
| Asgary Case 12 | Male 34 y.o. | 3.4 SR | 12 min | - | Apical periodontitis | Survival | 15 months |
| Asgary Case 13 | Female 29 y.o. | 3.6 MR | 10 min | - | Apical periodontitis | Survival | 11 months |
| Asgary Case 14 | Male 63 y.o. | 3.6 MR | 14 min | - | Apical periodontitis | Survival | 12 months |
| Asgary Case 15 | Male 31 y.o. | 1.7 MR | 13 min | - | Apical periodontitis | Survival | 10 months |
| Asgary Case 16 | Female 46 y.o. | 4.6 MR | 14 min | - | Apical periodontitis | Survival | 8 months |
| Asgary Case 17 | Female 40 y.o. | 4.6 MR | 12 min | - | Apical periodontitis | Failure | 8 months |
| Asgary Case 18 | Female 27 y.o. | 4.7 MR | 13 min | - | Apical periodontitis | Survival | 20 months |
| Asgary Case 19 | Female 41 y.o. | 3.6 MR | 10 min | - | Apical periodontitis | Survival | 12 months |
| Asgary Case 20 | Male 37 y.o. | 4.7 MR | 10 min | - | Apical periodontitis | Survival | 9 months |
| Asgari 2014 [58] | Female 28 y.o. | 1.4 MR 1.5 SR | 8 min | - | Apical periodontitis | Survival | 2 years |
| MoradiMajd 2014 [59] | Female 44 y.o. | 4.5 SR | - | - | Iatrogenic perforation | Failure | 1 year |
| Penarrocha Diego 2014 [60] | Male 51 y.o. | 1.7 MR | 30 min | - | Follicular cyst | Survival | 12 months |
| Tsesis 2014 [61] | Female 20 y.o. | 4.7 MR | 8 min | - | Paraesthesia | Survival | 4 years |
| Keceli 2014 [62] | Female 20 y.o. | 3.2 SR | 6 min | - | Severe periodontitis | Survival | 15 months |
| Pruthi 2015 [63] | Male 28 y.o. | 1.1 SR | 15 min | - | External root resorption | Survival | 18 months |
| DeeptiDua 2015 [64] | Male 23 y.o. | 1.1 SR | 20 min | - | Complicated crown-root fracture | Survival | 3 years |
| Forero-Lopez 2015 [65] | Male 25 y.o. | 1.2 SR | 8 min | - | Apical periodontitis | Survival | 3 months |
| Garrido 2016 [66] | Female 50 y.o. | 1.1 SR | 4 min | - | Endo-periodontal disease | Survival | 1 year |
| Abu-Hussein Muhamad 2016 [67] | Female 45 y.o. | 1.7 SR | 20 min | - | Apical periodontitis/Instrument separation | Survival | 15 years |
| Oishi 2017 [68] | Male 7 y.o. | 1.1 SR | - | - | Transverse root fracture/Endo-periodontal disease | Survival | 5 years |
| Grzanich 2017 [69] Case 1 | Female 64 y.o. | 3.1 SR | - | - | Apical periodontitis/Instrument separation | Survival | 28 months |
| Grzanich Case 2 | Male 35 y.o. | 1.4 MR | - | - | Apical periodontitis/endodontic | Survival | 2 years |
| Grzanich Case 3 | Female 86 y.o. | 1.8 SR | - | - | Apical periodontitis/vertical root fracture | Survival | 2 years |
| Faghihian 2017 [70] | Male 10 y.o. | 1.1 SR | 4 min | - | complicated crown-root fracture | Survival | 18 months |
| Maniglia-Ferreira 2017 [71] | Male 7 y.o. | 1.1 SR | 15 min | - | Traumatic avulsion | Survival | 3 years |
| Thaore 2017 [72] | Male 23 y.o. | 3.7 MR | 10 min | - | Apical periodontitis/Instrument separation | Survival | 1 year |
| Asgari 2018 [73] | Female 22 y.o. | 4.6 MR | 7 min | - | Apical periodontitis | Survival | 2 months |
| Zafar 2018 [74] | Female 30 y.o. | 2.6 MR | 15 min | - | Apical periodontitis/Instrument separation | questionable | 4 weeks |
| Saeed Kazi 2018 [75] | Male 35 y.o. | 4.7 MR | 10 min | - | Root perforation | Survival | 4 months |
| Krug 2019 [76] | Male 37 y.o. | 1.1 SR | 12 min | - | External cervical resorption | Survival | 2.5 years |
| Deshpande 2019 [77] | Female 23 y.o. | 1.6 MR | 10 min | - | Apical periodontitis/Instrument separation | Survival | 2 years |
| Teng Kai Ong 2019 [78] | Male 27 y.o. | 1.7 MR | 15 min | - | Symptomatic periradicular periodontitis | Failure | 10 months |
| Hao Yan 2019 [79] case1 | Male 37 y.o. | 2.2 SR | 7 min | - | Apical periodontitis | Survival | 18 months |
| Hao Yan 2019 case2 | Male 30 y.o. | 1.2 SR | 6 min | - | Apical periodontitis | Survival | 15 months |
| Hao Yan 2019 case3 | Female 27 y.o. | 1.2 SR | 6 min | - | Apical periodontitis | Survival | 12 months |
| Cunliffe 2020 [80] Case 1 | Male 33 y.o. | 4.1 SR | 15 min | - | Instrument separation/Root perforation | Survival | 6 months |
| Cunliffe Case 2 | Female 45 y.o. | 3.4 SR | 15 min | - | Apical periodontitis with missed anatomy | Failure | 3 months |
| Cunliffe Case 3 | Female 52 y.o. | 4.6 MR | 15 min | - | Apical periodontitis with over-filled | Failure | 3 months |
| Cunliffe Case 4 | Female 57 y.o. | 4.4 SR | 4 min | - | Apical periodontitis/pain | Survival | 1 year |
| Cunliffe Case 5 | Female 42 y.o. | 3.6 MR | - | - | Apical periodontitis | Survival | 3 months |
| Cunliffe Case 6 | Male 64 y.o. | 2.1 SR | 15 min | - | External root resorption | Survival | 4 months |
| Cunliffe Case 7 | Female 76 y.o. | 3.7 MR | - | - | Apical periodontitis with sclerosed canals | Failure | 1 year |
| Cunliffe Case 8 | Male 53 y.o. | 3.7 MR | - | - | Pulpal floor perforation | Survival | 3 months |
| Cunliffe Case 9 | Male 50 y.o. | 2.1 SR | - | - | Internal root resorption | Survival | 15 months |
| Cunliffe Case 10 | Female 64 y.o. | 3.7 MR | 15 min | - | Instrument separation | Survival | 6 months |
| Cunliffe Case 11 | Female 45 y.o. | 3.7 MR | - | - | Apical periodontitis with over-filled | Survival | 28 months |
| Cunliffe Case 12 | Male 45 y.o. | 4.5 SR | - | - | Apical periodontitis | Survival | 9 months |
| Cunliffe Case 13 | Female 39 y.o. | 3.6 MR | - | - | Apical periodontitis with procedural errors | Failure | 3 months |
| Asgary 2019 [81] | Female 28 y.o. | 3.7 MR | 10 min | - | Apical periodontitis/endodontic failure | Survival | 1 year |
| Fujii 2020 [82] | Female 30 y.o. | 1.6 MR | 15 min | - | Instrument separation | Survival | 1 year |
| Ganapathy 2020 [83] | Male 10 y.o. | 2.1 SR | - | - | Complicated crown-root fracture | Survival | 2 years |
| Lodha 2020 [84] | Female 28 y.o. | 4.6 MR | 10 min | - | Apical periodontitis/Instrument separation | Survival | 8 months |
| Yang 2021 [85] | Male 20 y.o. | 1.5 SR | 15 min | - | Apical periodontitis with internal root resorption and root fracture | Survival | 2 years |
| Shekhawat 2021 [86] | Male 13 y.o. | 3.6 MR | 15 min | - | Apical periodontitis | Survival | 12 months |
| Source | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | %Yes | Risk |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tang 1996 | x | √ | √ | √ | x | √ | √ | √ | ? | x | x | 55% | moderate |
| Poi 1999 | x | ? | x | x | x | √ | √ | √ | x | x | x | 27% | high |
| Aqrabawi 1999 | √ | √ | ? | x | x | √ | √ | √ | x | x | ? | 45% | high |
| Benenati 2003 | x | √ | √ | x | √ | √ | √ | √ | ? | x | x | 55% | moderate |
| Fariniuk 2003 | √ | √ | √ | x | x | √ | √ | √ | ? | x | x | 55% | moderate |
| Ward 2004 | x | √ | √ | x | x | √ | √ | √ | ? | x | √ | 55% | moderate |
| Shintani 2004 | x | √ | √ | √ | x | √ | √ | √ | x | x | ? | 55% | moderate |
| Peer 2004 | √ | √ | √ | ? | x | √ | √ | √ | x | x | x | 55% | moderate |
| BarattoFilho 2004 | √ | ? | √ | √ | √ | √ | √ | √ | √ | x | √ | 81% | low |
| Cotter 2006 | x | x | √ | √ | x | √ | √ | √ | √ | x | ? | 55% | moderate |
| Herrera 2006 | √ | √ | ? | x | x | √ | √ | √ | ? | x | x | 45% | high |
| Martins | √ | √ | x | ? | x | √ | √ | √ | x | x | ? | 45% | high |
| Penarrocha 2007 | √ | √ | √ | √ | ? | √ | √ | √ | √ | x | √ | 81% | low |
| Demir 2007 | √ | ? | √ | √ | √ | √ | √ | √ | √ | x | √ | 81% | low |
| Sivolella 2008 | x | ? | x | x | x | √ | √ | √ | x | x | x | 27% | high |
| Wang 2008 | x | x | √ | √ | x | √ | √ | √ | ? | x | √ | 55% | moderate |
| Al-Hezaimi 2009 | x | ? | √ | √ | x | √ | √ | √ | √ | x | x | 55% | moderate |
| Bittencourt 2009 | x | x | √ | √ | x | √ | √ | √ | √ | x | ? | 55% | moderate |
| Ozer 2010 | x | x | √ | √ | x | √ | √ | √ | ? | x | √ | 55% | moderate |
| Hsiang Lu 2011 | x | ? | √ | √ | x | √ | √ | √ | √ | x | x | 55% | moderate |
| Unver 2011 | √ | √ | ? | √ | √ | √ | √ | √ | √ | x | √ | 81% | low |
| Kim 2011 | √ | √ | x | ? | x | √ | √ | √ | x | x | ? | 45% | high |
| Moura 2012 | √ | √ | ? | x | x | √ | √ | √ | x | x | ? | 45% | high |
| Dogan 2013 | x | x | ? | x | x | √ | √ | √ | x | x | x | 27% | high |
| Shin 2013 | x | x | √ | √ | x | √ | √ | √ | ? | x | √ | 55% | moderate |
| Yuan 2013 | x | x | √ | √ | x | √ | √ | √ | ? | x | √ | 55% | moderate |
| Nagappa 2013 | x | x | √ | √ | x | √ | √ | √ | ? | x | √ | 55% | moderate |
| Kumar 2013 | √ | √ | √ | √ | ? | √ | √ | √ | √ | x | √ | 81% | low |
| Moradi Majd 2014 | x | x | √ | x | √ | √ | √ | √ | ? | x | √ | 55% | moderate |
| Subay 2014 | x | √ | x | √ | x | √ | √ | √ | √ | x | ? | 55% | moderate |
| Asgary 2014 | x | x | √ | √ | x | √ | √ | √ | ? | x | √ | 55% | moderate |
| Asgari 2014 | x | ? | x | x | x | √ | √ | √ | x | x | x | 27% | high |
| Moradi Majd 2014 | x | x | √ | x | √ | √ | √ | √ | ? | x | √ | 55% | moderate |
| Penarrocha Diego 2014 | x | √ | x | √ | x | √ | √ | √ | √ | x | ? | 55% | moderate |
| Tsesis 2014 | x | x | √ | √ | x | √ | √ | √ | ? | x | √ | 55% | moderate |
| Keceli 2014 | x | x | ? | x | x | √ | √ | √ | x | x | x | 27% | high |
| Pruthi 2015 | x | √ | x | √ | x | √ | √ | √ | √ | x | ? | 55% | moderate |
| Deepti Dua 2015 | x | x | √ | √ | x | √ | √ | √ | ? | x | √ | 55% | moderate |
| Forero-Lopez 2015 | x | ? | x | x | x | √ | √ | √ | x | x | x | 27% | high |
| Garrido 2016 | x | x | √ | x | √ | √ | √ | √ | ? | x | √ | 55% | moderate |
| Abu-Hussein Muhamad 2016 | x | √ | x | √ | x | √ | √ | √ | √ | x | ? | 55% | moderate |
| Oishi 2017 | x | x | √ | x | √ | √ | √ | √ | ? | x | √ | 55% | moderate |
| Grzanich 2017 | x | ? | x | x | x | √ | √ | √ | x | x | x | 27% | high |
| Faghihian 2017 | √ | √ | √ | √ | ? | √ | √ | √ | √ | x | √ | 81% | low |
| Maniglia-Ferreira 2017 | √ | √ | ? | X | x | √ | √ | √ | x | x | ? | 45% | high |
| Thaore 2017 | x | x | √ | x | √ | √ | √ | √ | ? | x | √ | 55% | moderate |
| Asgari 2018 | x | √ | x | √ | x | √ | √ | √ | √ | x | ? | 55% | moderate |
| Zafar 2018 | √ | √ | x | ? | x | √ | √ | √ | x | x | ? | 45% | high |
| Saeed Kazi 2018 | x | x | √ | x | √ | √ | √ | √ | ? | x | √ | 55% | moderate |
| Krug 2019 | √ | √ | √ | √ | x | √ | √ | √ | √ | ? | √ | 81% | low |
| Deshpande 2019 | √ | √ | √ | ? | √ | √ | √ | √ | √ | x | √ | 81% | low |
| Teng Kai Ong 2019 | √ | √ | x | ? | x | √ | √ | √ | x | x | ? | 45% | high |
| Hao Yan 2019 | √ | √ | ? | x | x | √ | √ | √ | x | x | ? | 45% | high |
| Cunliffe 2020 | √ | √ | √ | √ | ? | √ | √ | √ | √ | x | √ | 81% | low |
| Asgary 2019 | √ | x | √ | ? | x | √ | √ | √ | x | x | ? | 45% | high |
| Fujii 2020 | x | √ | x | √ | x | √ | √ | √ | √ | x | ? | 55% | moderate |
| Ganapathy 2020 | x | x | x | x | ? | √ | √ | √ | x | x | x | 27% | High |
| Lodha 2020 | x | x | ? | x | x | √ | √ | √ | x | x | x | 27% | high |
| Yang 2021 | x | √ | x | √ | x | √ | √ | √ | √ | x | ? | 55% | moderate |
| Shekhawat 2021 | √ | √ | √ | √ | ? | √ | √ | √ | √ | x | √ | 81% | low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pisano, M.; Di Spirito, F.; Martina, S.; Sangiovanni, G.; D’Ambrosio, F.; Iandolo, A. Intentional Replantation of Single-Rooted and Multi-Rooted Teeth: A Systematic Review. Healthcare 2023, 11, 11. https://doi.org/10.3390/healthcare11010011
Pisano M, Di Spirito F, Martina S, Sangiovanni G, D’Ambrosio F, Iandolo A. Intentional Replantation of Single-Rooted and Multi-Rooted Teeth: A Systematic Review. Healthcare. 2023; 11(1):11. https://doi.org/10.3390/healthcare11010011
Chicago/Turabian StylePisano, Massimo, Federica Di Spirito, Stefano Martina, Giuseppe Sangiovanni, Francesco D’Ambrosio, and Alfredo Iandolo. 2023. "Intentional Replantation of Single-Rooted and Multi-Rooted Teeth: A Systematic Review" Healthcare 11, no. 1: 11. https://doi.org/10.3390/healthcare11010011
APA StylePisano, M., Di Spirito, F., Martina, S., Sangiovanni, G., D’Ambrosio, F., & Iandolo, A. (2023). Intentional Replantation of Single-Rooted and Multi-Rooted Teeth: A Systematic Review. Healthcare, 11(1), 11. https://doi.org/10.3390/healthcare11010011











