Occupational Therapy Interventions for Dementia Caregivers: Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Review Criteria
- Experimental studies (randomized or non-randomized intervention studies, exploratory studies, pilot studies and quasi-experimental studies). Rationale: we have included these study designs because they provide us with the greatest number of intervention characteristics, and therefore contribute to answering our research question. We have only included experimental studies at Joanna Briggs Institute (JBI) levels of evidence 1 and 2 [21] seeking to include only those study designs with the highest level of evidence;
- Experimental studies in which an occupational therapy intervention for caregivers (over 18 years old) of people with dementia (Alzheimer’s disease, Lewy body dementia, frontotemporal dementia, vascular dementia, Huntington’s disease, Pick’s disease dementia, Parkinson’s disease) was carried out. Rationale: caregivers of people with dementia should be included in the study population, as the aim of our study is to describe occupational therapy interventions directed at them;
- Experimental studies written in English or Spanish. Rationale: English is the most widely used language in research and therefore the language through which we can obtain most information in relation to our study objective. Although it is unusual to find articles published only in Spanish, we have added this language since it is our native language and if necessary, we will be able to complement the articles in English.
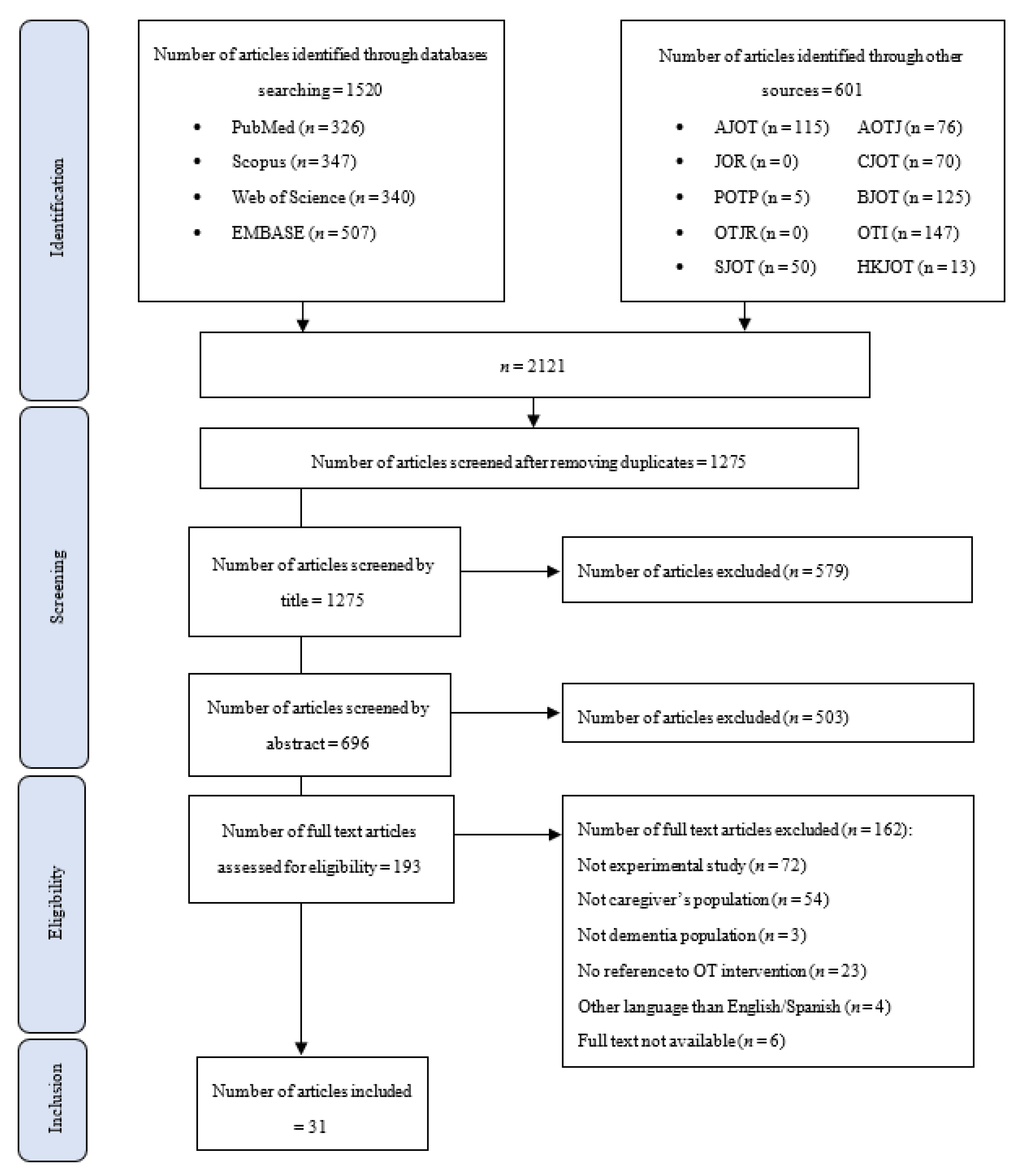
2.3. Study Selection
2.4. Data Extraction and Synthesis
2.5. Quality Assessment
3. Results
3.1. Main Characteristics of the Included Studies
3.2. Study Population in the Included Studies
3.3. Main Intervention Characteristics of the Included Studies
3.4. Occupational Therapy Interventions for Caregivers
3.5. Home-Based Intervention: Tailored Activity Program (TAP)
3.6. Home-Based Intervention: The Environmental Skill-Building Program (ESP)
3.7. Home-Based Intervention: Advancing Caregiver Training (ACT)
3.8. Home-Based Intervention: Other Household Interventions
3.9. Other Interventions
3.10. Variables of Study and Measurement Instruments
3.11. Main Limitations of Included Studies
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- About dementia-Alzheimer’s Disease and Dementia. Available online: https://alz.org/inicio (accessed on 15 November 2021).
- Neurological Disorders: Public Health Challenges. Available online: https://www.who.int/publications-detail-redirect/9789241563369 (accessed on 15 November 2021).
- Galende, A.V.; Ortiz, M.E.; Velasco, S.L.; Luque, M.L.; de Miguel, C.L.d.S.; Jurczynska, C.P. Informe de la Fundación del Cerebro. Impacto social de la enfermedad de Alzheimer y otras demencias. Neurol. Publi. Soc. Esp. Neurol. 2021, 36, 39–49. [Google Scholar]
- Mahoney, R.; Regan, C.; Katona, C.; Livingston, G. Anxiety and Depression in Family Caregivers of People with Alzheimer Disease: The LASER-AD Study. Am. J. Geriatr. Psychiatry 2005, 13, 795–801. [Google Scholar] [CrossRef]
- Peña-Longobardo, L.M.; Oliva-Moreno, J. Caregiver Burden in Alzheimer’s Disease Patients in Spain. J. Alzheimer’s Dis. 2015, 43, 1293–1302. [Google Scholar] [CrossRef]
- Herrera Merchán, E.J. Eficacia de un Programa de Intervención Psicológica para Cuidadores Familiares de Personas con Demencia. Ph.D. Thesis, Universidad de Salamanca, Salamanca, Spain, 2014. [Google Scholar] [CrossRef]
- Sörensen, S.; Pinquart, M.; Duberstein, P. How Effective Are Interventions with Caregivers? An Updated Meta-Analysis. Gerontologist 2002, 42, 356–372. [Google Scholar] [CrossRef]
- García Mateos, F.; Alonso Sanchez, J. Aquaterapia para familiares y cuidadores de personas con demencia. Ress. Rev. Educ. Soc. 2016. Available online: https://eduso.net/res/revista/23/resenas/aquaterapia-para-familiares-y-cuidadores-de-personas-con-demencia (accessed on 15 November 2021).
- Madruga-Vicente, M.; Gozalo-Delgado, M.; Gusi-Fuertes, N.; Prieto-Prieto, J. Efectos de un programa de ejercicio físico a domicilio en cuidadores de pacientes de alzheimer: Un estudio piloto. Rev. Psicol. Deporte 2009, 18, 255–270. [Google Scholar]
- Kuo, L.-M.; Huang, H.-L.; Huang, H.-L.; Liang, J.; Chiu, Y.-C.; Chen, S.-T.; Kwok, Y.-T.; Hsu, W.-C.; Shyu, Y.-I.L. A Home-Based Training Program Improves Taiwanese Family Caregivers’ Quality of Life and Decreases Their Risk for Depression: A Randomized Controlled Trial. Int. J. Geriatr. Psychiatry 2013, 28, 504–513. [Google Scholar] [CrossRef]
- Signe, A.; Elmståhl, S. Psychosocial Intervention for Family Caregivers of People with Dementia Reduces Caregiver’s Burden: Development and Effect after 6 and 12 Months. Scand. J. Caring Sci. 2008, 22, 98–109. [Google Scholar] [CrossRef]
- Yong, A.S.L.; Price, L. The human occupational impact of partner and close family caregiving in dementia: A meta-synthesis of the qualitative research, using a bespoke quality appraisal tool. Br. J. Occup. Ther. 2014, 77, 410–421. [Google Scholar] [CrossRef]
- Donovan, M.L.; Corcoran, M.A. Description of Dementia Caregiver Uplifts and Implications for Occupational Therapy. Am. J. Occup. Ther. 2010, 64, 590–595. [Google Scholar] [CrossRef]
- Gitlin, L.; Corcoran, M.; Winter, L.; Boyce, A.; Hauck, W. A Randomized, Controlled Trial of a Home Environmental Intervention Effect on Efficacy and Upset in Caregivers and on Daily Function of Persons with Dementia. Gerontologist 2001, 41, 4–14. [Google Scholar] [CrossRef]
- Dooley, N.R.; Hinojosa, J. Improving Quality of Life for Persons with Alzheimer’s Disease and Their Family Caregivers: Brief Occupational Therapy Intervention. Am. J. Occup. Ther. 2004, 58, 561–569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Draper, B. Occupational Therapy Is Cost-Effective for Older People with Dementia and Their Caregivers. Evid. Based Ment. Health 2008, 11, 83. [Google Scholar] [CrossRef] [PubMed]
- 2020 Alzheimer’s Disease Facts and Figures. Alzheimer’s Dement. 2020. Available online: https://www.researchgate.net/publication/342411751_2020_Alzheimer’s_disease_facts_and_figures (accessed on 15 November 2021). [CrossRef]
- Higgins, J.; Thomas, J. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0; The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Bramer, W.M.; Rethlefsen, M.L.; Kleijnen, J.; Franco, O.H. Optimal Database Combinations for Literature Searches in Systematic Reviews: A Prospective Exploratory Study. Syst. Rev. 2017, 6, 245. [Google Scholar] [CrossRef]
- Joanna Briggs Institute JBI Levels of Evidence. Developed by the Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party October 2013. Available online: https://joannabriggs.org/sites/default/files/2019-05/JBI-Levels-of-evidence_2014_0.pdf (accessed on 12 January 2022).
- Li, T.; Higgins, J.; Deeks, J.J. Chapter 5: Collecting Data. Cochrane Handbook for Systematic Reviews of Interventions Version 6.3, 2022th ed.; Cochrane: London, UK, 2022. [Google Scholar]
- Arksey, H.; O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Pynoos, J.; Ohta, R.J. In-Home Interventions for Persons with Alzheimer’s Disease and Their Caregivers. Phys. Occup. Ther. Geriatr. 1991, 9, 83–92. [Google Scholar] [CrossRef]
- Gitlin, L.; Corcoran, M.; Winter, L.; Boyce, A.; Marcus, S. Predicting Participation and Adherence to a Home Environmental Intervention among Family Caregivers of Persons with Dementia. Fam. Relat. 1999, 48, 363–372. [Google Scholar] [CrossRef]
- Mitchell, E. Managing Carer Stress: An Evaluation of a Stress Management Programme for Carers of People with Dementia. Br. J. Occup. Ther. 2000, 63, 179–184. [Google Scholar] [CrossRef]
- Corcoran, M.A.; Gitlin, L. Family Caregiver Acceptance and Use of Environmental Strategies Provided in an Occupational Therapy Intervention. Phys. Occup. Ther. Geriatr. 2001, 19, 1–20. [Google Scholar] [CrossRef]
- Gitlin, L.N.; Winter, L.; Corcoran, M.; Dennis, M.P.; Schinfeld, S.; Hauck, W.W. Effects of the Home Environmental Skill-Building Program on the Caregiver-Care Recipient Dyad: 6-Month Outcomes from the Philadelphia REACH Initiative. Gerontologist 2003, 43, 532–546. [Google Scholar] [CrossRef] [Green Version]
- Gitlin, L.N.; Hauck, W.W.; Dennis, M.P.; Winter, L. Maintenance of Effects of the Home Environmental Skill-Building Program for Family Caregivers and Individuals with Alzheimer’s Disease and Related Disorders. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 368–374. [Google Scholar] [CrossRef]
- Hilgeman, M.M.; Allen, R.S.; DeCoster, J.; Burgio, L.D. Positive Aspects of Caregiving as a Moderator of Treatment Outcome Over 12 Months. Psychol. Aging 2007, 22, 361–371. [Google Scholar] [CrossRef]
- Chee, Y.K.; Gitlin, L.N.; Dennis, M.P.; Hauck, W.W. Predictors of Adherence to a Skill-Building Intervention in Dementia Caregivers. J. Gerontol. A Biol. Sci. Med. Sci. 2007, 62, 673–678. [Google Scholar] [CrossRef]
- Gitlin, L.N.; Winter, L.; Burke, J.; Chernett, N.; Dennis, M.P.; Hauck, W.W. Tailored Activities to Manage Neuropsychiatric Behaviors in Persons with Dementia and Reduce Caregiver Burden: A Randomized Pilot Study. Am. J. Geriatr. Psychiatry 2008, 16, 229–239. [Google Scholar] [CrossRef]
- Gitlin, L.N.; Winter, L.; Dennis, M.P.; Hodgson, N.; Hauck, W.W. A Biobehavioral Home-Based Intervention and the Well-Being of Patients with Dementia and Their Caregivers: The COPE Randomized Trial. JAMA 2010, 304, 983–991. [Google Scholar] [CrossRef]
- Gitlin, L.N.; Winter, L.; Dennis, M.P.; Hodgson, N.; Hauck, W.W. Targeting and Managing Behavioral Symptoms in Individuals with Dementia: A Randomized Trial of a Nonpharmacological Intervention. J. Am. Geriatr. Soc. 2010, 58, 1465–1474. [Google Scholar] [CrossRef]
- DiZazzo-Miller, R.; Samuel, P.S.; Barnas, J.M.; Welker, K.M. Addressing Everyday Challenges: Feasibility of a Family Caregiver Training Program for People With Dementia. Am. J. Occup. Ther. 2014, 68, 212–220. [Google Scholar] [CrossRef]
- Gitlin, L.N.; Arthur, P.; Piersol, C.; Hessels, V.; Wu, S.S.; Dai, Y.; Mann, W.C. Targeting Behavioral Symptoms and Functional Decline in Dementia: A Randomized Clinical Trial. J. Am. Geriatr. Soc. 2018, 66, 339–345. [Google Scholar] [CrossRef]
- DiZazzo-Miller, R.; Pociask, F.D.; Adamo, D.E. The Role of Confidence in Family Caregiving for People with Dementia. Phys. Occup. Ther. Geriatr. 2020, 38, 355–369. [Google Scholar] [CrossRef]
- Graff, M.J.L.; Vernooij-Dassen, M.J.M.; Thijssen, M.; Dekker, J.; Hoefnagels, W.H.L.; Rikkert, M.G.M.O. Community Based Occupational Therapy for Patients with Dementia and Their Care Givers: Randomised Controlled Trial. BMJ 2006, 333, 1196. [Google Scholar] [CrossRef] [Green Version]
- Graff, M.J.L.; Vernooij-Dassen, M.J.M.; Thijssen, M.; Dekker, J.; Hoefnagels, W.H.L.; Olderikkert, M.G.M. Effects of Community Occupational Therapy on Quality of Life, Mood, and Health Status in Dementia Patients and Their Caregivers: A Randomized Controlled Trial. J. Gerontol. A Biol. Sci. Med. Sci. 2007, 62, 1002–1009. [Google Scholar] [CrossRef]
- Sturkenboom, I.H.; Graff, M.J.; Borm, G.F.; Veenhuizen, Y.; Bloem, B.R.; Munneke, M.; Nijhuis-van der Sanden, M.W. The Impact of Occupational Therapy in Parkinson’s Disease: A Randomized Controlled Feasibility Study. Clin. Rehabil. 2013, 27, 99–112. [Google Scholar] [CrossRef]
- Sturkenboom, I.H.W.M.; Graff, M.J.L.; Hendriks, J.C.M.; Veenhuizen, Y.; Munneke, M.; Bloem, B.R.; Nijhuis-van der Sanden, M.W. OTiP study group Efficacy of Occupational Therapy for Patients with Parkinson’s Disease: A Randomised Controlled Trial. Lancet Neurol. 2014, 13, 557–566. [Google Scholar] [CrossRef]
- Tang, S.-H.; Chio, O.-I.; Chang, L.-H.; Mao, H.-F.; Chen, L.-H.; Yip, P.-K.; Hwang, J.-P. Caregiver Active Participation in Psychoeducational Intervention Improved Caregiving Skills and Competency. Geriatr. Gerontol. Int. 2018, 18, 750–757. [Google Scholar] [CrossRef]
- Lau, W.M.; Chan, T.Y.; Szeto, S.L. Effectiveness of a Home-Based Missing Incident Prevention Program for Community-Dwelling Elderly Patients with Dementia. Int. Psychogeriatr. 2019, 31, 91–99. [Google Scholar] [CrossRef]
- Lai, F.H.-Y.; Yan, E.W.-H.; Tsui, W.-S.; Yu, K.K.-Y. A Randomized Control Trial of Activity Scheduling for Caring for Older Adults with Dementia and Its Impact on Their Spouse Care-Givers. Arch. Gerontol. Geriatr. 2020, 90, 104167. [Google Scholar] [CrossRef]
- Brodaty, H.; Low, L.F. Making Memories: Pilot Evaluation of a New Program for People with Dementia and Their Caregivers. Australas. J. Ageing 2004, 23, 144–146. [Google Scholar] [CrossRef]
- O’Connor, C.M.; Clemson, L.; Brodaty, H.; Low, L.-F.; Jeon, Y.-H.; Gitlin, L.N.; Piguet, O.; Mioshi, E. The Tailored Activity Program (TAP) to Address Behavioral Disturbances in Frontotemporal Dementia: A Feasibility and Pilot Study. Disabil. Rehabil. 2019, 41, 299–310. [Google Scholar] [CrossRef]
- Laver, K.; Liu, E.; Clemson, L.; Davies, O.; Gray, L.; Gitlin, L.N.; Crotty, M. Does Telehealth Delivery of a Dyadic Dementia Care Program Provide a Noninferior Alternative to Face-To-Face Delivery of the Same Program? A Randomized, Controlled Trial. Am. J. Geriatr. Psychiatry 2020, 28, 673–682. [Google Scholar] [CrossRef]
- Nobili, A.; Riva, E.; Tettamanti, M.; Lucca, U.; Liscio, M.; Petrucci, B.; Porro, G.S. The Effect of a Structured Intervention on Caregivers of Patients with Dementia and Problem Behaviors: A Randomized Controlled Pilot Study. Alzheimer Dis. Assoc. Disord. 2004, 18, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Onor, M.L.; Trevisiol, M.; Negro, C.; Signorini, A.; Saina, M.; Aguglia, E. Impact of a Multimodal Rehabilitative Intervention on Demented Patients and Their Caregivers. Am. J. Alzheimer’s Dis. Other Demen. 2007, 22, 261–272. [Google Scholar] [CrossRef] [PubMed]
- Novelli, M.M.P.C.; Machado, S.C.B.; Lima, G.B.; Cantatore, L.; Sena, B.P.; Rodrigues, R.S.; Rodrigues, C.I.B.; Canon, M.B.F.; Piersol, C.V.; Nitrini, R.; et al. Effects of the Tailored Activity Program in Brazil (TAP-BR) for Persons with Dementia. Alzheimer Dis. Assoc. Disord. 2018, 32, 339–345. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, A.M.; Radanovic, M.; Homem de Mello, P.C.; Buchain, P.C.; Dias Vizzotto, A.; Harder, J.; Stella, F.; Piersol, C.V.; Gitlin, L.N.; Forlenza, O.V. An Intervention to Reduce Neuropsychiatric Symptoms and Caregiver Burden in Dementia: Preliminary Results from a Randomized Trial of the Tailored Activity Program-Outpatient Version. Int. J. Geriatr. Psychiatry 2019, 34, 1301–1307. [Google Scholar] [CrossRef]
- Voigt-Radloff, S.; Graff, M.; Leonhart, R.; Schornstein, K.; Jessen, F.; Bohlken, J.; Metz, B.; Fellgiebel, A.; Dodel, R.; Eschweiler, G.; et al. A Multicentre RCT on Community Occupational Therapy in Alzheimer’s Disease: 10 Sessions Are Not Better than One Consultation. BMJ Open 2011, 1, e000096. [Google Scholar] [CrossRef]
- Wenborn, J.; O’Keeffe, A.G.; Mountain, G.; Moniz-Cook, E.; King, M.; Omar, R.Z.; Mundy, J.; Burgess, J.; Poland, F.; Morris, S.; et al. Community Occupational Therapy for People with Dementia and Family Carers (COTiD-UK) versus Treatment as Usual (Valuing Active Life in Dementia [VALID]) Study: A Single-Blind, Randomised Controlled Trial. PLoS Med. 2021, 18, e1003433. [Google Scholar] [CrossRef]
- Man, D.W.K.; Tsang, W.S.F.; Lu, E.Y.; Tsang, H.W.H. Bibliometric Study of Research Productivity in Occupational Therapy and Physical Therapy/Physiotherapy in Four Western Countries and Five Asian Countries/Regions. Aust. Occup. Ther. J. 2019, 66, 690–699. [Google Scholar] [CrossRef]
- WHO. Dementia. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 16 November 2021).
- Spillman, B.C.; Wolff, J.L.; Freedman, V.; Kasper, J.D. Informal Caregiving for Older Americans: An Analysis of the 2011 National Study of Caregiving. Available online: https://www.urban.org/research/publication/informal-caregiving-older-americans-analysis-2011-national-study-caregiving (accessed on 16 November 2021).
- Gitlin, L.N.; Corcoran, M.A. Occupational Therapy and Dementia Care. In The Home Environmental Skill-Building Program for Individuals and Families; American Occupational Therapy Association: Bethesda, ML, USA, 2005. [Google Scholar]
- Maresova, P.; Hruska, J.; Klimova, B.; Barakovic, S.; Krejcar, O. Activities of Daily Living and Associated Costs in the Most Widespread Neurodegenerative Diseases: A Systematic Review. Clin. Interv. Aging 2020, 15, 1841–1862. [Google Scholar] [CrossRef]
- Lord, K.; Gill, L.; Robertson, S.; Cooper, C. How People with Dementia and Their Families Decide about Moving to a Care Home and Support Their Needs: Development of a Decision Aid, a Qualitative Study. BMC Geriatr. 2016, 16, 68. [Google Scholar] [CrossRef]
- López, J.; Losada, A.; Romero-Moreno, R.; Márquez-González, M.; Martínez-Martín, P. Factores asociados a la consideración de ingresar a un familiar con demencia en una residencia. Neurologia 2012, 27, 83–89. [Google Scholar] [CrossRef]
- Law, M.; Cooper, B.; Strong, S.; Stewart, D.; Rigby, P.; Letts, L. The Person-Environment-Occupation Model: A Transactive Approach to Occupational Performance. Can. J. Occup. Ther. 1996, 63, 9–23. [Google Scholar] [CrossRef]
- Occupational Therapy Practice Guidelines for Adults With Alzheimer’s Disease and Related Major Neurocognitive Disorders. Available online: https://myaota.aota.org/shop_aota/product/900402 (accessed on 16 November 2021).
- Gitlin, L.N.; Kales, H.C.; Lyketsos, C.G. Nonpharmacologic Management of Behavioral Symptoms in Dementia. JAMA 2012, 308, 2020–2029. [Google Scholar] [CrossRef] [PubMed]
- Gitlin, L.N.; Piersol, C.V.; Hodgson, N.; Marx, K.; Roth, D.L.; Johnston, D.; Samus, Q.; Pizzi, L.; Jutkowitz, E.; Lyketsos, C.G. Reducing Neuropsychiatric Symptoms in Persons with Dementia and Associated Burden in Family Caregivers Using Tailored Activities: Design and Methods of a Randomized Clinical Trial. Contemp. Clin. Trials 2016, 49, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Gitlin, L.N.; Hodgson, N.; Jutkowitz, E.; Pizzi, L. The Cost-Effectiveness of a Nonpharmacologic Intervention for Individuals with Dementia and Family Caregivers: The Tailored Activity Program. Am. J. Geriatr. Psychiatry 2010, 18, 510–519. [Google Scholar] [CrossRef]
- Peeters, J.M.; Van Beek, A.P.; Meerveld, J.H.; Spreeuwenberg, P.M.; Francke, A.L. Informal Caregivers of Persons with Dementia, Their Use of and Needs for Specific Professional Support: A Survey of the National Dementia Programme. BMC Nurs. 2010, 9, 9. [Google Scholar] [CrossRef]
- Livingston, G.; Sommerlad, A.; Orgeta, V.; Costafreda, S.G.; Huntley, J.; Ames, D.; Ballard, C.; Banerjee, S.; Burns, A.; Cohen-Mansfield, J.; et al. Dementia Prevention, Intervention, and Care. Lancet 2017, 390, 2673–2734. [Google Scholar] [CrossRef]
- Lyketsos, C.; Miller, D. Addressing the Alzheimer’s Disease Crisis through Better Understanding, Treatment, and Eventual Prevention of Associated Neuropsychiatric Syndromes. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2012, 8, 60–64. [Google Scholar] [CrossRef]
- Kales, H.C.; Gitlin, L.N.; Lyketsos, C.G. When Less Is More, but Still Not Enough: Why Focusing on Limiting Antipsychotics in People With Dementia Is the Wrong Policy Imperative. J. Am. Med. Dir. Assoc. 2019, 20, 1074–1079. [Google Scholar] [CrossRef]
- Oliveira, A.M.; Radanovic, M.; de Mello, P.C.H.; Buchain, P.C.; Vizzotto, A.D.B.; Harder, J.; Stella, F.; Gitlin, L.N.; Piersol, C.V.; Valiengo, L.L.C.; et al. Adjunctive Therapy to Manage Neuropsychiatric Symptoms in Moderate and Severe Dementia: Randomized Clinical Trial Using an Outpatient Version of Tailored Activity Program. J. Alzheimer’s Dis. 2021, 83, 475–486. [Google Scholar] [CrossRef]
| Database | Search Strategy |
|---|---|
| PubMed | ((alzheimer OR dementia OR parkinson) AND caregiver AND “occupational therapy”) |
| Scopus | ((alzheimer OR dementia OR parkinson) AND caregiver AND “occupational therapy”) |
| EMBASE | (alzheimer OR ‘dementia’/exp OR dementia OR parkinson) AND (‘caregiver’/exp OR caregiver) AND (‘occupational therapy’/exp OR ‘occupational therapy’) |
| WOS | ((alzheimer OR dementia OR parkinson) AND caregiver AND “occupational therapy”) |
| AJOT | (alzheimer OR dementia OR parkinson) AND caregiver AND “occupational therapy” |
| JOR | (alzheimer OR dementia OR parkinson) AND caregiver AND “occupational therapy” |
| POTP | [All: alzheimer] OR [All: dementia] OR [All: parkinson] AND [All: caregiver] AND [All: “occupational therapy”] AND [in Journal: Physical & Occupational Therapy In Pediatrics] |
| OTJR | (alzheimer OR dementia OR parkinson) AND caregiver AND “occupational therapy” |
| SJOT | [[All: alzheimer] OR [All: dementia] OR [All: parkinson]] AND [All: caregiver] AND [All: “occupational therapy”] AND [in Journal: Scandinavian Journal of Occupational Therapy] |
| AOTJ | [[All: alzheimer] OR [All: dementia] OR [All: parkinson]] AND [All: caregiver] AND [All: “occupational therapy”] |
| CJOT | [[All alzheimer] OR [All dementia] OR [All parkinson]] AND [All caregiver] AND [All “occupational therapy”] within Canadian Journal of Occupational Therapy |
| BJOT | [[All alzheimer] OR [All dementia] OR [All parkinson]] AND [All caregiver] AND [All “occupational therapy”] within British Journal of Occupational Therapy |
| OTI | dementia and alzheimer and parkinson and caregiver and occupational therapy |
| HKJOT | [[All alzheimer] OR [All dementia] OR [All parkinson]] AND [All caregiver] AND [All “occupational therapy”] within Hong Kong Journal of Occupational |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Campos, A.; Compañ-Gabucio, L.-M.; Torres-Collado, L.; Garcia-de la Hera, M. Occupational Therapy Interventions for Dementia Caregivers: Scoping Review. Healthcare 2022, 10, 1764. https://doi.org/10.3390/healthcare10091764
Martínez-Campos A, Compañ-Gabucio L-M, Torres-Collado L, Garcia-de la Hera M. Occupational Therapy Interventions for Dementia Caregivers: Scoping Review. Healthcare. 2022; 10(9):1764. https://doi.org/10.3390/healthcare10091764
Chicago/Turabian StyleMartínez-Campos, Alberto, Laura-María Compañ-Gabucio, Laura Torres-Collado, and Manuela Garcia-de la Hera. 2022. "Occupational Therapy Interventions for Dementia Caregivers: Scoping Review" Healthcare 10, no. 9: 1764. https://doi.org/10.3390/healthcare10091764
APA StyleMartínez-Campos, A., Compañ-Gabucio, L.-M., Torres-Collado, L., & Garcia-de la Hera, M. (2022). Occupational Therapy Interventions for Dementia Caregivers: Scoping Review. Healthcare, 10(9), 1764. https://doi.org/10.3390/healthcare10091764





