Abstract
Parametric and non-parametric frontier applications are typical for measuring the efficiency and productivity of many healthcare units. Due to the current COVID-19 pandemic, hospital efficiency is the center of academic discussions and the most desired target for many public authorities under limited resources. Investigating the state of the art of such applications and methodologies in the healthcare sector, besides uncovering strategical managerial prospects, can expand the scientific knowledge on the fundamental differences among efficiency models, variables and applications, drag research attention to the most attractive and recurrent concepts, and broaden a discussion on the specific theoretical and empirical gaps still to be addressed in future research agendas. This work offers a systematic bibliometric review to explore this complex panorama. Hospital efficiency applications from 1996 to 2022 were investigated from the Web of Science base. We selected 65 from the 203 most prominent works based on the Core Publication methodology. We provide core and general classifications according to the clinical outcome, bibliographic coupling of concepts and keywords highlighting the most relevant perspectives and literature gaps, and a comprehensive discussion of the most attractive literature and insights for building a research agenda in the field.
1. Introduction
Hospitals are the largest cost factor in health care systems worldwide and are experiencing increasing pressure to improve the efficiency and quality of their services. Healthcare is one of the job sectors with the highest levels of complexity in business models, given the customers′ uniqueness. One way to better manage the nature of healthcare is through the incorporation of information technologies, medical innovations and new technologies, web platforms, data storage, analytical software, telecommunications systems and blockchain implementation to help deliver information and improve information security, speed of dissemination of information for administrators, professionals and decision-makers in healthcare organizations and improve the effectiveness of treatments [1,2]. According to Dwivedi et al. [3], the COVID-19 pandemic challenges the capabilities of health managers to make timely decisions to handle the pandemic efficiently and effectively.
At the same time, it forces the latter to rethink the essential elements of their operational processes in order to meet the new needs associated with the pandemic. Leite et al. [4] state that the COVID-19 pandemic has affected the operations of healthcare organizations in several aspects. These elements relate, for instance, to the refocusing of healthcare supply chain practices, the ability to maximize resource utilization and operations management practices. Understanding the impact of these factors allows health managers and policy makers to identify how to balance demand, resources and capacity properly. Therefore, according to Kamel and Mousa [5], hospitals can reappraise and restructure their existing plans to meet the organizational challenges brought by the pandemic through efficiency evaluation.
Hospitals consume several inputs (e.g., human resources, pharmaceuticals, equipment, etc.) to produce high-value outputs (e.g., outpatient visits, surgical operations, etc.). Hence, hospital efficiency analysis is about measuring the competence with which inputs are converted into valuable outputs. However, Kohl et al. [6] point out that estimating hospital efficiency is not straightforward. In this regard, one can emphasize that there are several methodologies to evaluate the efficiency of hospitals. According to Cordero et al. [7], efficiency scores of healthcare institutions can be estimated using either parametric or non-parametric methods. Both methodologies aim to assess production units and are based on productivity indicators, also known as technical efficiency (TE), that offer measures that characterize the operations of the units analyzed. Every econometric estimation of parametric functions has a definite mathematical form that is not very easy to identify [8]. Hence, the Stochastic Frontier (SF) is the most used parametric approach. It assumes that it is not possible to fully specify the function and allows for random noise. SF, therefore, takes into account the random component.
In relation to non-parametric methodologies, Data Envelopment Analysis (DEA) is the most widely used. DEA models allow the assessment of the relative efficiency of decision-making units (DMUs) by creating a production frontier using the best practice of the observed data [9]. It was developed by Charnes et al. [10]. In addition, it is used to rank and compare the efficiency of various entities. Thus, according to O’Neill et al. [11], DEA overcomes the weaknesses of parametric analysis because it does not require any assumption related to the functional form of the relationship between outputs and inputs. In addition, DEA can not only identify inefficient units but can also assess the degree of inefficiency. DEA uses linear programming to construct a piecewise convex linear segmented efficiency frontier, making it more flexible than econometric frontier analysis [12]. Moreover, DEA can include multiple inputs and outputs.
Despite these identified benefits, DEA presents some shortcomings. It attributes every deviation from the best practice frontier to inefficiency. Such deviations might be due to statistical noise. In addition, it is highly susceptible to the selection of variables and data errors. However, according to Kohl et al. [6], the most widely used tools for analyzing the efficiency of hospitals include DEA and other closely related tools. Furthermore, an important feature of the analysis of hospital efficiency through DEA concerns the fact that many authors (among others, Nayar and Ozcan [13]; Ferrier and Trivitt and [14], Wu et al. [15]) focused on the relationship between efficiency and quality. Indeed, according to Kohl et al. [6], the proportion of studies that include quality variables is likely to increase further and the inclusion of quality indicators should become the standard procedure in the future. However, it should be noted that the scientific community has not agreed on a common standard in dealing with hospital variables, and not all models are suitable to produce meaningful results from quality data processing.
Given the necessity to improve the performance of hospitals, this article aims to provide an overview of past, present and future research directions in the field of hospital efficiency assessment through DEA. More in detail, our study seeks to address the following collection of research questions (RQs):
- RQ1: Who are the most prominent contributions to the core literature of the DEA for the efficiency evaluation of hospitals?
- RQ2: What are the main quantity and quality variables used in the literature on hospital efficiency evaluation through DEA?
- RQ3: What are the main models and support approaches used in the literature on hospital efficiency evaluation through DEA? Which of these are most suitable for including different inputs and outputs combinations?
- RQ4: What are the main gaps and overlaps in the literature on hospital efficiency evaluation through DEA? How can we use this perspective to construct and address future research agendas in the field?
While previous research (e.g., Kohl et al. [6]) has attempted to analyze this topic through a literature study, we use bibliometric analysis [16,17] to reveal statistical patterns and provide an informative overview of key topical perspectives in the field of DEA application in hospital settings. Accordingly, this article not only sets out the most important issues in this field but also highlights those areas of research that have not been sufficiently developed, creating points of support for future research.
2. Systematic Review Design
On 13 January 2022, a systematic search was conducted at 10:48 a.m. (UTC+03:00) in the Web of Science™ database (https://www.webofscience.com/, accessed on 22 January 2022) [18]. Despite having less content than other bibliographic bases, the Web of Science (WoS) was chosen because it is recognized in the scientific community as the world’s most important repository for scientific literature. It contains more than 34 thousand journals and more than 171 million records in all fields of knowledge from 1900 to the present day on a global scale. Four query strings with three refinements were applied using the search tools provided by the website to retrieve the most relevant contributions in the field of healthcare efficiency. The results were extracted at 10:49 a.m., 10:53 a.m., 10:58 a.m., and 11:01 a.m. on the same day. At first, all searchable fields (such as topic, title, abstract, author keywords) in all collections (A&HCI, ESCI, CPCI-SSH, CPCI-S, SCI-EXPANDED, SSCI) were considered from 1980 (the first record) to 2022 using a straightforward query string Q1 “ALL = (healthcare AND efficiency)” resulting 15,594 records. Then refinements were made to those results.
Table 1 reports all the query strings used in the systematic search design. The query links in this table directly address this review′s content on each specific instance. The second query string was applied to restrict the broad results, which included documents, such as bibliographies, corrections, database reviews, creative proses, meeting abstracts, and record reviews, among others, to articles only. The third query string was elaborated to meet research questions RQ2, RQ3 and RQ4, restricting the results to parametric and non-parametric frontier applications only (DEA and SFA). The last string and refinement were elaborated to meet the research question RQ1 restricting to hospital applications only.

Table 1.
Strings used in the Web of Science systematic search.
Figure 1, panels a, b, c and d, illustrate the document distribution with bar charts per author (panel a), year (panel b), geographic region (panel c) and Web of Science categories (panel d). The most recurrent contributors are Michael D. Rosko (reported in the first and eighth bars of panel a) [23,24,25,26,27,28,29,30,31,32,33], Yasar A. Ozcan [34,35,36,37,38,39], Vivian G. Valdmanis [23,24,31,40,41,42], Ali Emrouznejad [43,44,45,46,47], Ryan L. Mutter [23,25,26,27,33], Kristina Kocisova [48,49,50,51], Paolo Mancuso [40,42,52,53], Yoshinori Nakata [54,55,56,57], Hongbing Tao [58,59,60,61], and Yuichi Watanabe [54,55,56,57]. The number of publications per year reported in the second panel (panel b) has a decreasing increase (increase with a decreasing rate), especially over the past six years. The higher growth in the number of publications is from 2014 to 2015, a 100% increase from five to 10 publications. There was a particular tendency for COVID-19-related publications over the past years in hospital applications. The mean growth rate is 0.1739 over the past decade (2020–2021: 0.0645, 2019–2020: 0.1481, 2018–2019: 0.2857, 2017–2018: 0.2352, 2016–2017: 0.4166, 2015–2016: 0.2000, 2014–2015: 1.0000, 2013–2014: −0.2857, 2012–2013: −0.1250, 2011–2012: −0.2000).
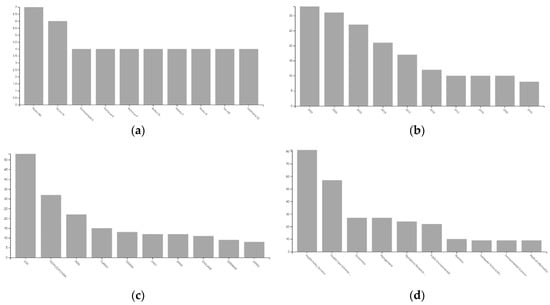
Figure 1.
Results sorted by authors, year, country and field. Panels (a–d), illustrate the document distribution with bar charts per author (panel a), year (panel b), geographic region (panel c) and Web of Science categories (panel d).
After the third refinement, we applied the Core Publication methodology [62,63] for selecting the most relevant records strictly related to the field of efficiency analysis in hospitals. Sixty-five papers out of the 15,954 documents from the general search (Q1) were identified as core publications in this exercise. After classifying, filtering and investigating this network, we retrieved the twelve documents identified as the most relevant based on citation scores. They are discussed in the following section. Figure 2 illustrates the Prisma Diagram for this systematic review application.
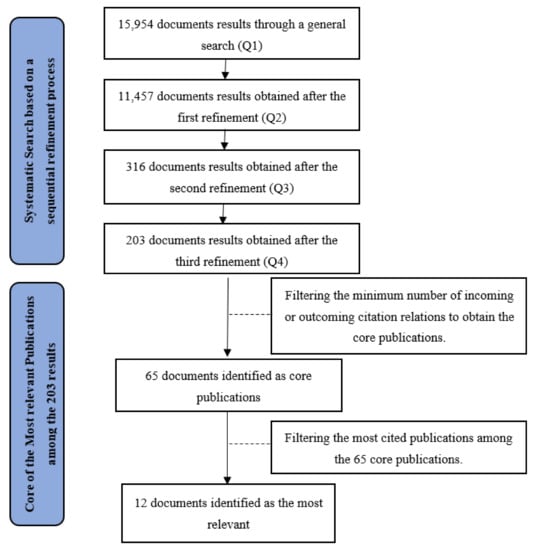
Figure 2.
Flow Diagram with the different phases of the systematic review (according to Moher et al. [64] PRISMA scheme).
The Web of Science Systematic Search based on a sequential refinement procedure departed from 15,954 document results applying the general search query Q1. Then, 11,457 documents results were obtained after the first refinement applying the query string Q2, 316 documents results appeared after the second refinement applying the third query string Q3, and finally, 203 documents results were obtained after the third refinement applying the fourth query string Q4. From this point, we resort to the Core Publication Methodology of van Eck and Waltman [62], by filtering the minimum number of incoming or outcoming citation relations, resulting in 65 documents identified as core publications. Lastly, 12 documents were ranked as the most relevant based on their citation score. Figure 2 summarizes the systematic search.
3. Core Publications and Research Impact
The Core Publication Methodology is an interesting approach for selecting the core, i.e., the most important publications related to a specific field. Many networks of scientific literature may include publications that, despite their importance in terms of content quality or citations, are weak related or completely unrelated to the investigated field [65]. According to van Eck and Waltman [62,66], a Core Publication is a paper with (at least) a certain minimum number of interactions with other core publications. These interactions are counted in the number of incoming and outgoing citations. This methodology keeps in the core of a network of scientific literature only the relevant contributions to the investigated area, regardless of the van Eck and Waltman citation scores [62,66].
By definition, at least one core publication must be related to another core publication (by citing or being cited). Thus, the minimum number of core publications for any bibliometric network is two. Following Nepomuceno et al.’s [65] approach for selecting the most relevant and restricted network, we define four as the maximum–minimum threshold of citation links in which at least two core publications can be identified. This means that each core publication in this network has citation relations with at least four other core publications. Above this threshold, no core publications can be identified (i.e., there is no core publication with five incoming or outgoing citation relations with another core publication).
3.1. Classification
After applying the maximum–minimum threshold of citation links, 65 documents were identified as core publications in the field of hospital efficiency analysis. Table 2 reports the core publications classified into two groups using the clustering technique from van Eck and Waltman [62,66]. The most common inputs, outputs, frontier models and methods are highlighted for each group. Figure 3 illustrates the timeline-based citation network of the 65 core publications represented in blue, mainly located on the right side of the visualization (left side of the reader) and green (mainly located on the left side of the visualization (right side of the reader).

Table 2.
Core-publications clusters, variables and models.
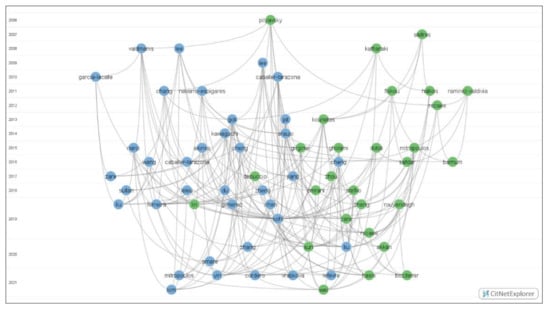
Figure 3.
Timeline-based network visualization for the core publications.
The most commonly used inputs in more than 80% of the core publications are hospital beds (intensive care unit beds, emergency beds, psychiatric, chronic, tuberculosis and leprosy beds [47,74]), physicians (specialists and non-specialists), nurses and other medical and non-medical staff (such as ancillary services personnel, pharmacists, laboratory and other technicians, administrative personnel, radiological technologists, midwives, and dietitians [43,47]). They are often measured in Full Time Equivalent (FTE) [1,41,52,60,67]. Another common but less recurrent input is expenditures. Salaries and other financial or administrative expenditures, such as interest costs [72], spending on medicines and on purchase of goods and services [73], rural medical and general healthcare expenditures [74] are often reported in local currency. Municipal subsidies to cover deficits are also reported in the work of Kawaguchi, Tone and Tsutsui [72] as an input related to healthcare expenditures.
Instead of the total number of beds (aggregate or by medical specialties), some works employ the number of available beds or “the actual number of open beds” [60,85,88], which according to the authors, represent a better proxy for capital inputs in the healthcare production system. The hospital area, medical business area, the number of doctor’s offices and surgical rooms are examples of physical inputs related to the building where the healthcare services are provided in the works of Araújo [77] and Liu [88]. The works of Tao Du [81] and Tao Liu et al. [74] are macro-efficiency evaluations rather than hospital institutional assessments using the number of healthcare institutions in 31 provinces of China as input. Lastly, two unusual and interesting inputs are the service complexity reported in the work of Lee, Yang and Choi [71], defined as the total number of diagnostic and special services provided by the hospital, and the unmet medical needs reported in the work of Mitropoulos [89] exhibiting the population seeking healthcare but which cannot have access to it due to financial and service barriers in the healthcare system.
The outputs are more diversified than inputs in the applications. The most common healthcare products regarded in the hospital efficiency core applications are the number of discharges [7,70,71,75,83], the number of surgeries [67,77,78,79,83,86], and the total number of inpatient and outpatient treatments, diagnoses and healthcare income [68,77,81]. Childbirth-related outputs are antenatal checkups, deliveries (such as cesarean-section deliveries), abortions, post-natal care, and the number of male and female sterilizations [83,84,86]. Two interesting outputs related to hospital bed management are bed utilization and turnover rate [81]. Case-mix adjusted healthcare admissions and discharges [70,71,75,78,79], mostly based on diagnosis-related group (DRG) systems, are another interesting output integration used to consider the complexity of diseases and clinical specialties. The complexity and differences among medical specialties impact any efficiency analysis based on quantitative outputs, making it easier or more difficult to expand that related product [117]. This is a relevant topic for consideration in this field.
Efficiency analyses of hospitals are filled with applications containing undesirable outputs composing healthcare units’ production technology, which aims to be reduced instead of expanded in the DEA linear formulation. Examples are in-hospital mortality, inpatient days (length of hospitalization stays) and readmissions [65,66,83,85,86]. Other outputs present in Network DEA models are known as links (intermediate products), i.e., an output that is at the same time an input for another department of the service unit. This is the case of Kawaguchi et al. [72] Dynamic-Network Data Envelopment Analysis model which uses “number of beds” as a link variable from Division 1 (administration) to Division 2 (medical examination) in the efficiency estimation of Japanese hospitals. Other studies, such as Amare et al. [76] and Du [81] are two-stage approaches used to evaluate the impact of quality environment variables or exogenous (independent) factors, such as the CEO’s administrative service years, educational status, the distance of the CEO’s residence from the facility, incentive packages for the employee, patient waiting time, among others. Another interesting work
Some controversial outputs found in the literature implicate using exogenously determined variables that are not sufficiently under the control of healthcare units and limit the scope of the production possibilities of hospitals. Exogenous outputs, such as outpatient visits, ambulatory and emergency room visits, number of ordinary admissions, ICU inpatients, emergency inpatients, first consultations and successive consultations [67,68,70,71,75,78,79,84,85,86] are some examples. They depend on social, demographic, spatial and economic covariates that affect people’s health conditions that hospitals do not control to expand. It is possible that, in a comparative perspective, efficient hospitals produce many consultations or admissions compared to others with similar production structures because they are faced with a bigger population (demographic factor) or poorer, less-educated regions (socioeconomic factor). When control variables are not included in such analysis, results might bias the distribution of inefficiencies. According to Nepomuceno et al. [118], such analysis can jeopardize the objective measure of technical efficiency and the inclusion of exogenously determined outputs as non-discretionary inputs are suggested.
3.2. Discussion on the Most Relevant Contribution
This subsection is dedicated to a comprehensive discussion on the most relevant contributions based on the attractiveness metric of the 12 top-cited core publications. The attractiveness of a publication is defined as the number of Google Scholar citations divided by the publication period. This bibliometric measure provides a fairer comparison between old and new publications by offering a number of citations per unit of time. For instance, the work of Valdmanis, Rosko and Mutter (2008) [23] has the second-highest number of Google Scholar citations (until January 2022) with 152 citations, but it is the sixth-ranked core publication with about 0.96 citations per month (paper published on 20 September 2008) compared to the work of Gok and Sezen (2013) [83] with fewer citations (136 citations) but published more recently (on August 2013), reporting about 1.35 citations per month. Figure 4 and Table 3 report the most relevant core contributions in the efficiency analysis of hospitals.
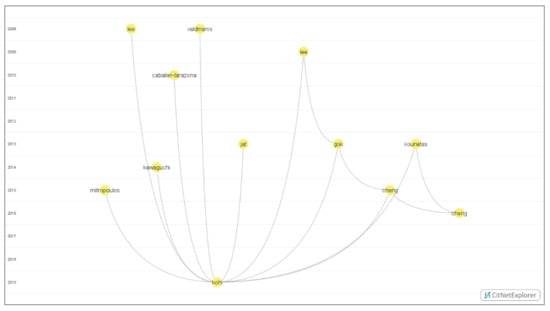
Figure 4.
Timeline-based network visualization for the most relevant contributions.

Table 3.
Most relevant contributions.
Kohl et al. (2019) [6] developed a literature review covering 262 papers with DEA applications in hospitals to discover gaps not covered in a timeline from 2005 to 2016. Their literature search was performed on Google Scholar, Science Direct, and PubMed, including works only in English, detecting an increasing trend in the number of articles published along the defined timeline, with the peak occurring in 2016. In terms of the geographical distribution of the publications, it was detected that most studies came from Europe (with 96), followed by Asia (66), in the second rank, and North America (64), in the third rank, and these three regions presented a tendency in increasing the number of papers. Africa (with 21) appeared in the fourth rank and was the only region presenting a decline. About the types of research questions, the authors detected the following distribution: 100 publications related to “specific management questions”, 99 related to “performing DEA”, 48 related to questions on “new applications or methodologies, and 36 related to the “effects of reforms”. There was a tendency to increase the number of papers in the timeline for each question cluster. In terms of model specification, it was noted a remarkable trend for the use of quality parameters, and related to the DEA model selection, two basic models–CCR (Charnes, Cooper, and Rhodes model) and BCC (Banker, Charnes, and Cooper and model)–appeared with most of the applications (112 and 144, respectively).
Gok and Sezen (2013) [83] analyzed the effects of efficiency and structural quality of Turkish hospitals on patient satisfaction. They applied DEA using data from 524 hospitals from which a sample of 348 observations was extracted, and multiple regression analysis was applied to evaluate the relationship between patient satisfaction, structural quality, hospital efficiency, and institutional factors. The study detected that small-size hospitals are relatively more efficient, having higher patient satisfaction. In contrast, large hospitals provide comparatively higher quality care, tending to increase their infrastructure to meet the care process more. Structural quality proved to significantly impact patient satisfaction, with efficiency negatively moderating the relationship between structural quality and satisfaction.
The study of Cheng et al. (2015) [61] examined the technical efficiency and productivity of Henan county hospitals during China’s Healthcare Reform Plan started in 2009, using two methodologies (Stochastic Frontier Analysis–SFA, and DEA) seeking to determine whether and how efficiency is affected by a series of environmental and institutional factors. The study detected a considerable space for technology efficiency improvement, with 98.2% of the sample, with 114 hospitals considered inefficient in 2010 and 2011 and 91.2% in 2012.
Kawaguchi, Tone and Tsutsui (2014) [72] developed the first study applying the dynamic-network (DN) DEA model in healthcare, performing an evaluation of the policy effect of Japan’s municipal hospitals’ reform, focusing on efficiency improvements both within the hospital and within two separate internal hospitals organizations. They selected a hospital with more than 300 beds among 1000 hospitals. The results obtained implied three policy implications: (i) the dynamic change in period-divisional efficiency scores between 2007 and 2009 was relatively small in administrative and medical divisions, not finding positive policy effects on average on Japanese municipal hospitals; (ii) looking for individual hospitals, the study could not show a strong correlation between the efficiency scores of administration and medical divisions; (iii) focusing on the efficiency improvements of two divisions in individual hospitals, the ratio of hospitals where both divisions improved efficiency was 16.96% while the ration of hospitals where efficiencies were maintained or reduced was 58.92%, and the rate of hospitals where change direction differed between both divisions was 24.12%. The authors conclude they did not find any significant efficiency improvement even with the implemented municipal hospital reform policy.
Kounetas and Papathana-ssopoulos (2013) [107] developed a study intending to measure Greek hospitals’ performance using SFA and DEA, using a dataset consisting of 114 hospitals from 130 in a statistical record from the Greek Ministry of Health and Social Solidarity Welfare for 2008. The authors defined the hospitals’ performances as not encouraging, demonstrating that their study’s technical efficiency scores are lower than in previous ones. They also found that bed occupancy ratio was inversely related to technical and scale inefficiency and that the type of hospital improved technical efficiency while scale inefficiency is unaffected.
Lee, Yang and Choi (2009) [71] assessed the relationship between hospital ownership and technical efficiency in a managed care environment. The data used in the study are related to 435 hospitals in Florida (United States) from 2001 to 2004. DEA was used to calculate hospital technical efficiency scores, determining that non-profit hospitals were generally more efficient than for-profit ones in the four-years timeline explored. No difference was found between non-profit and for-profit hospitals with less than 100 beds and between 250 and 399 beds. However, a statistically significant difference was detected between non-profit and for-profit hospitals with 100 and 249 beds and those with more than 400 beds.
The study by Mitropoulos, Talias and Mitropoulos [109] is dedicated to accounting for the impact of statistical noise in DEA. They proposed a combination of a chance-constrained DEA (CCDEA) with a Bayesian approach, making an empirical application in 117 Greek public hospitals, divided into 17 primary hospitals, 71 secondary, and 29 tertiary. The DEA input variables used were: the number of doctors, number of other personnel, number of beds, and total operating cost. The outputs defined selected were: the annual number of inpatient admissions and aggregated scheduled and emergency outpatient visits. The authors’ findings confirmed the efficacy of the Bayesian-CCDEA model, showing that it can also be applied in contexts where there is uncertainty to provide comparisons between technical and technology gaps among different groups.
Valdmanis, Rosko and Mutter [23] applied congestion analysis to assess trade-offs between quality and efficiency in 1377 urban hospitals in 34 states in the United States. This analysis is a variation of DEA, and for this study, the authors considered as inputs: the number of bassinets, the number of licensed and staffed beds minus the number of beds in nonacute units; licensed and staffed “other” beds, the full-time equivalent number of registered nurses, number of licensed practical nurses, number of medical residents and number of other personnel. As the outputs, the authors defined: the number of Medicare case mix index adjusted admissions, total surgeries, total outpatients’ visits, total births, and total other patient days. Among their findings, they detected some characteristics associated with inefficiency and quality congestion in the hospital studied: 3% of the total inefficiency can be attributed to quality congestion; most hospitals in the sample were operating at diseconomies of scale, suggesting that slack, mainly on beds, can be an inefficiency related factor; in teaching hospitals, the main source of inefficiency was diseconomy of scale; high-technology equipment was associated with higher quality.
Cheng et al. (2016) [60] studied the efficiency and productivity changes in 48 township hospitals in the three-tier rural healthcare system of China, from 2008 to 2014. They applied the bootstrapping DEA to estimate technical efficiency, pure technical efficiency, and scale efficiency and then they applied the bootstrapping Malmquist productivity index to calculate productivity changes within the studied period. Their findings showed that the average technical and pure technical efficiency of the hospitals in the sample was relatively low, indicating a great potential for improvement. In contrast, the average scale efficiency was relatively high; most inefficient hospitals were in decreasing returns to scale, and there is a considerable possibility of improvement for the output if this case is better managed.
The study by Caballer-Tarazona et al. [79] was focused on the efficiency of 22 hospitals in the Valencian Community (Spain). In this study, the authors designed and applied a healthcare performance evaluation system based on DEA to discover and improve potential inefficiencies. They used the number of doctors and beds as input variables and the number of admissions weighted by the case mix, first and successive consultations, and surgical innervations as output variables. They highlighted some results regarding the different analyses to approach the efficiency measuring: the DEA model was considered more useful when studying each service separately instead of studying the overall efficiency of a given hospital; the DEA model can be difficult to be used by hospitals’ managers, and it implied in the construction of user-friendly indicators to support efficiency measuring (namely the indicators “Weighted admissions/doctors” and “Interventions/doctors”), as an alternative to DEA.
Jat and Sebastian [84] developed a study to evaluate the technical efficiency of 40 public hospitals’ maternal healthcare services in Madhya Pradesh (India). They applied DEA, collecting data from the hospital from January to December 2010, using the health management information system and other records from the state’s health management agency. The authors defined their study as the first attempt to achieve the defined objective using DEA, describing that the average pure technical efficiency of 0.90 can produce the same number of outputs by saving 10% of the inputs, implying that the input savings can be applied to provide more healthcare services for more people through the community health centers in rural poor areas. Another result highlighted by the authors was that 50% of district hospitals are operating at a less-than-optimal level, and eleven of these hospitals obtained scores below 0.8, implying that the inefficient hospitals could significantly improve their efficiency with better resource management.
Lee, Chun and Lee [70] explained the relationship between the case-mix specialization index and the efficiency of inpatient hospital care services using data from 106 acute care hospitals in Seoul (South Korea). For this purpose, the authors applied DEA with the collected data using the case-mix specialization index (in the study, they calculated it as the Information Theory index) to measure the extent of hospital specialization. The results obtained indicated that only 10.3% of the 106 hospitals were relatively efficient in the market, providing practical implications for hospital managers to identify areas for improvement based on the examined variables in the inefficient hospital.
4. Cluster Analysis
This section is dedicated to a general classification and discussion of the bibliographic network containing the 203 references on hospital efficiency retrieved after the third refinement (Q3). Figure 5 illustrates the distance-based bibliometric network using the Vosviewer tool [62,66]. This network was constructed on the bibliographic coupling of works. Links are created when two publications cite the same third publication [119]. The visualization parameters are attraction = 8, repulsion = 0, resolution = 1 and the minimum cluster size = 58. Based on the bibliographic coupling network, we construct three co-occurrence landscapes and three radar charts for discussing a research agenda and highlight the most prominent perspectives on healthcare efficiency.
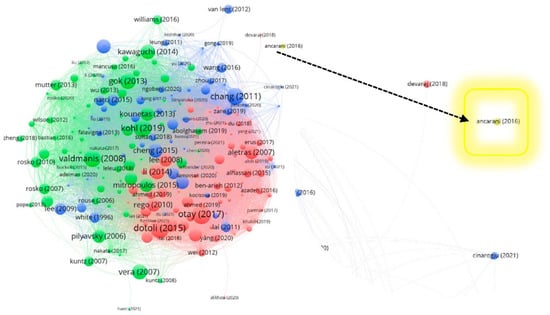
Figure 5.
Distance-based network visualization for 203 Web of Science papers.
The relations among publications are represented by the number of links and the distance of nodes. For instance, the work of Cheng et al. (2015) [61] on evaluating the technical efficiency of Chinese county hospitals (blue node in the center of this visualization) is more related to the work of Sultan et al. (2018) [69] on measuring the efficiency of Palestinian public hospitals (smaller blue node just above the work of Cheng et al. 2015) than it is to the work of Van Lent et al. (2012) [120] on exploring improvements in patient logistics in Dutch hospitals (blue node on the extreme upper-right side of the visualization). The colors red, green and blue (and one small yellow cluster composed of only one publication, Ancarani et al. (2016) [52]) indicate the groups to which a publication about hospital efficiency belongs. They are used to classify the network in the following subsection.
4.1. General Classification
Table 4 reports the general literature classification into the four clusters. The red cluster has 20 core publications out of 73 publications [28,42,46,50,55,61,64,73,75,76,77,78,82,86,87,89,91,94,95,96]. It is related to mostly econometric approaches to aid the efficiency analysis, such as Tobit Regressions, Bootstrap and Principal Component Analysis, and Multi-criteria and decision support approaches, such as AHP, Fuzzy Cognitive Map, Stochastic Multicriteria Acceptability Analysis and Multiple Stage approaches. This cluster is dedicated to the efficiency analysis of healthcare units involving environmental and socioeconomic contexts.

Table 4.
Cluster Definitions and Keywords.
The green cluster with one publication less than the red one is the second biggest group of publications. It has 20 core publications out of 72 publications [1,2,26,45,49,51,52,54,56,57,58,59,62,65,68,71,72,74,83,85]. This cluster includes financial or managerial perspectives in the performance management of hospitals. Developments on the recurrent trade-off between healthcare quality and technical efficiency, patient satisfaction, benchmarking, uncertainty, and health payment systems are reported in many publications present in this group. This cluster also includes information, communication and decision-support technologies, such as picture archiving and topics about healthcare information technology performance, electronic medical record and discussions about endogeneity and appropriate incentive structures.
The blue cluster has 23 core publications out of 58 publications [16,29,31,34,41,43,44,47,48,53,60,63,66,67,69,70,79,80,84,88,90,92,93]. This cluster is about interesting frontier applications in hospital sectors and healthcare categories that are not usual in the field of hospital efficiency analysis. Some of the related applications are in sectors and healthcare services related to cardiovascular diseases, acute care, pharmacies, rural medical systems, laboratories, surgery, cancer screening, and pet cancer. The last (yellow) cluster refers to only one publication (Ancarani et al. [52]) about different religious perspectives and how they might impact the efficiency of hospitals.
4.2. Co-Occurrence Networks
Each cluster is analyzed and separated for the purpose of this investigation. The bibliographic information for each documentation was treated using Mendeley Desktop version 1.19.3. The co-occurrence networks in Figure 6, Figure 7 and Figure 8 are the products of such bibliographic treatment exported into a .ris file. Keywords in any systematic review are essential sources for knowledge abstraction because they summarize in one or a few words the content of a document and main concepts of great significance in the field of scientific investigation. Consider i = 1, 2, 3, …, n keywords to be mapped in each publication cluster. For any j ≠ i keywords, the number of co-occurrences of the two keywords j and i is the number of publications in which both keywords occur together, denoted by = , and the total number of co-occurrences for the keyword i is [62,228].
Full counting was applied as the citation counting method, which is the most common approach where each co-occurrence link has the same weight [62,228]. The total number of keywords for the red cluster is 232 (from 2 to 156 total link strength). This number for the green and blue clusters is 221 (from 2 to 143 total link strength) and 229 (from 2 to 175 total link strength). Table 5 reports the most recurrent keywords (with the minimum number of three occurrences for a keyword) for each cluster (see the keywords co-occurrence map visualizations in Figure 6, Figure 7 and Figure 8).

Table 5.
Recurrent Keywords reported in the Co-occurrence Networks.
4.3. Outlining a Research Agenda
One of the most significant challenges to developing innovative ideas and models to cope with problems of a quantitative nature is that we can determine all the potential determinants affecting the object of study. Most of the time, we can only measure the impact of some known potential determinants of the investigation, i.e., testing whether the true values of variables are close to following a predictive path designed by the analyst. This is also a challenge in identifying relevant research topics to build a research agenda that comprehends the social needs for scientific advances. An interesting avenue to pursue this purpose is reported in Daraio et al. [231], which use a similar bibliometric methodology to assess the relevance of different applications in the field of efficiency analysis.
The co-occurrence of the concepts, perspectives, approaches, methods, categories, activities, and areas can be used to define a degree of generality that identifies gaps and overlaps in the research field. The Degree of Generality (DG) is defined as the inverse of the relevance score [231]. This exercise can stimulate knowledge discovery by identifying “context clues” left on titles, keywords and abstracts for interesting topics that can be explored in future research agendas on the field of investigation. Table 6 reports the main topics extracted from each cluster network classified per area with the range of generality for directing a research agenda in the field of healthcare efficiency. According to Daraio et al. [231], degrees of generality between 0 and 1 are reserved for limited topics (terms) and fields of application, neither sufficiently covered by scientific publications nor co-occurring with other terms or fields.

Table 6.
Selected Topics and Degree of Generality for a Research Agenda.
All the topics reported in Table 6 have a DG equal or below 1, with the exceptions on multiple stage approach (DG = 1.035), undesirable output (DG = 1.438), uncertainty (DG = 1.534), public hospital (DG = 2.027) and complexity (2.178) in the Red Cluster, and for the Green Cluster the topics effectiveness (DG = 1.460) and readmission (DG = 1.810). The most prominent topics to be prioritized for promoting a research agenda according to the bibliometric network are benchmarking (0.624), integrated quality (0.333), and fee schedule (0.250) with regard to Financial and Managerial Perspectives; allocation efficiency (0.250), directional distance functions (0.635) to principal component analysis (0.458) about the methods and support approaches.
About hospital sectors, activities and categories, applications related to church hospitals (0.941), cancer (0.500), surgical procedure (0.333), primary care (0.296) and pharmaceutical supplier (0.125) present the most notable topics; health care reform (0.609), economic development (0.500), inter-regional difference, equality, inequality, Gini coefficient (0.250), hazardous waste (0.500) and eco-efficiency (0.333) are the prominent concepts that can be explored with regard social, economic and environmental prospects. Concerning the class Information Technology, Systems and Communication, picture archiving and communication systems (0.500), and social computing platform (0.302) are the topics that are worth attention in future healthcare performance applications. Figure 9, Figure 10 and Figure 11 illustrate through radar charts the selected topics according to the relevance score for each topic on each cluster. The charts were created with the support of https://www.onlinecharttool.com/, accessed on 22 January 2022.
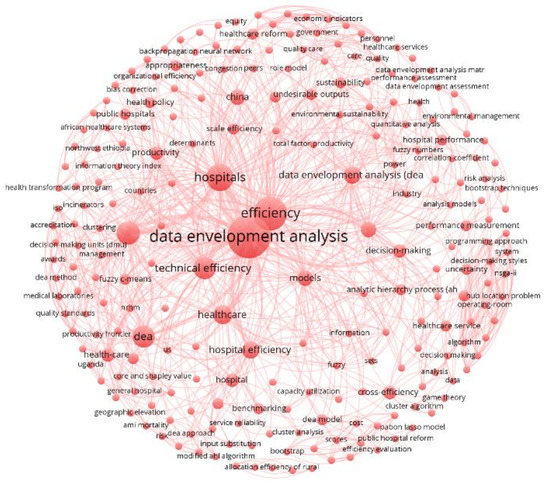
Figure 6.
Keywords Co-occurrence for the Red Cluster.
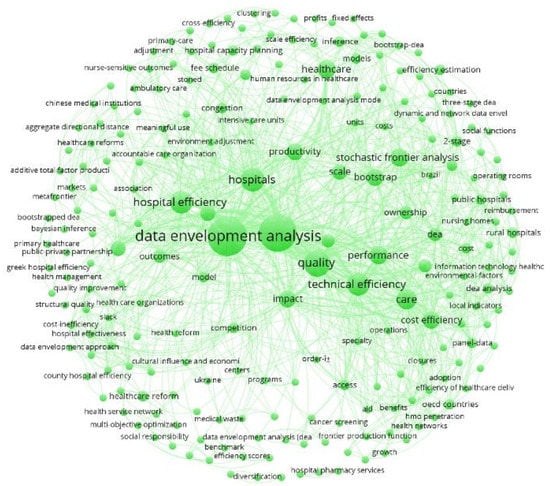
Figure 7.
Keywords Co-occurrence for the Green Cluster.
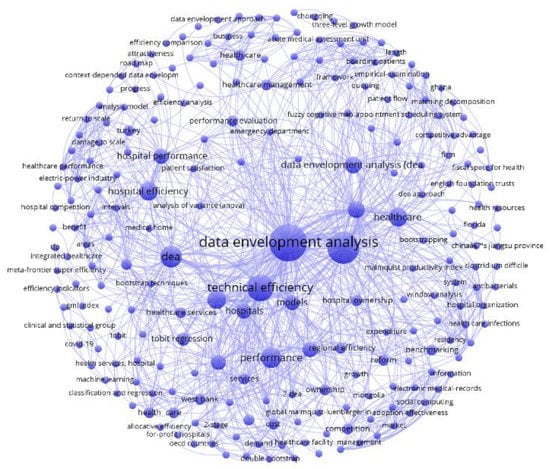
Figure 8.
Keywords Co-occurrence for the Blue Cluster.
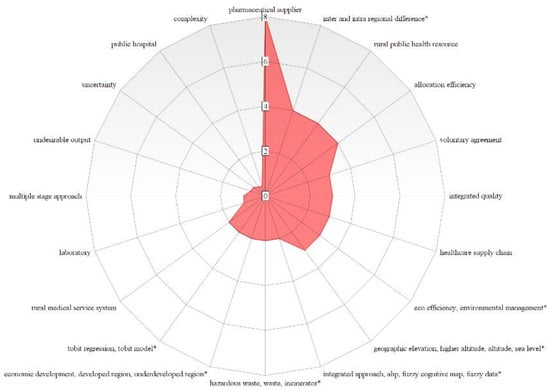
Figure 9.
Hot Topics for a Research Agenda in the Red Cluster.
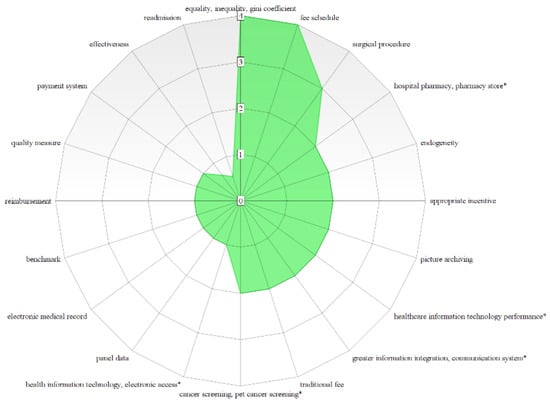
Figure 10.
Hot Topics for a Research Agenda in the Green Cluster.
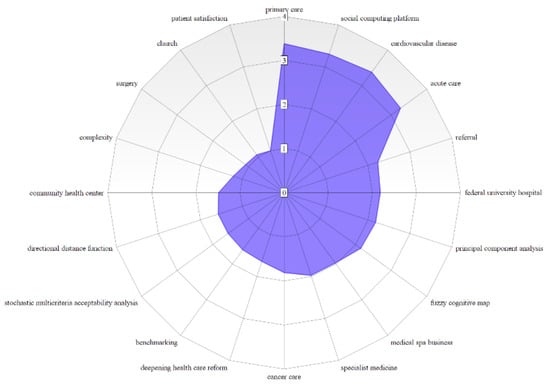
Figure 11.
Hot Topics for a Research Agenda in the Blue Cluster.
5. Conclusions
This work provided a comprehensive bibliometric investigation of the state-of-the-art frontier applications in hospitals using core publications, cluster analysis and co-occurrence networks. In the introduction, we proposed to address four research questions with this systematic bibliometric investigation. For the first question (RQ1): “Who are the most prominent contributions to the core literature of the DEA for the efficiency evaluation of hospitals?” we report in the Systematic Review Design and in the Core Publications and Research Impact sessions the most recurrent contributors, the most relevant publications in the core of healthcare efficiency ranked by an attractiveness metric (citations over time), and two different bibliometric classifications, one for the core and the one for the broad set of publications. The clusters for the 66 core publications highlighted the research impact in the field with a comprehensive discussion on the 12 top-cited core publications and the most relevant contributions.
The research questions (RQ2): “What are the main quantity and quality variables used in the literature on hospital efficiency evaluation through DEA?” and (RQ3): “What are the main models and support approaches used in the literature on hospital efficiency evaluation through DEA? Which of these are most suitable for including different inputs and outputs combinations?” were addressed in the third and fourth sessions reporting the most common inputs, outputs and models, addressed by a timeline-based and distance-based network visualizations with a responsive discussion on the investigations and healthcare perspectives present in the most relevant core contributions. The traditional CCR and BCC are, without any doubt, the most recurrent used non-parametric approaches. In addition, Bootstrap DEA, Malmquist (MPI), Two-Stage DEA and some Network models have been given particular attention in the context of healthcare efficiency. Most of those models use staff, beds and different expenditure types as common resources to produce some interesting, even controversial outputs, such as emergency visits, ordinary and ICU admissions, consultations, intermediate products, and some undesirable outputs, such as in-hospital mortality, the length of hospitalization stays and readmissions.
Lastly, to address the research question (RQ4): “What are the main gaps and overlaps in the literature on hospital efficiency evaluation through DEA? How can we use this perspective to construct and address future research agendas in the field?” we construct the clusters for the 203 Web of Science papers in the Cluster Analysis session. The distance-based network visualizations were investigated based on the recurrent keywords and topics reported in the co-occurrence networks for outlining a research agenda. Selected hot topics for this research agenda were investigated based on degrees of generality that identify gaps and overlaps in the research field. The topics and discussions related to efficiency concepts, econometric support approaches, financial, environmental, social and economic prospects, hospital sectors, segments and technologies, among others, can offer an interesting managerial perspective for scholars, practitioners and analysts of healthcare efficiency. We hope this research can aid such prospects in the healthcare management industry.
6. Update
On 12 June 2022, at 11:43 am (UTC-03:00), we applied the final query string (Q4) for updating the systematic search with possible recent publications that were not covered in this investigation. This search results in the following additional references, which we kindly invite readers to consult [87,232,233,234,235,236,237,238,239,240,241,242,243,244,245,246].
Author Contributions
Conceptualization, T.C.C.N. and L.P.O.; methodology, T.C.C.N.; software, T.C.C.N.; validation, T.C.C.N., L.P.O., V.D.H.d.C., T.P. and C.L.; formal analysis, T.C.C.N.; investigation, T.C.C.N., L.P.O., V.D.H.d.C. and T.P.; resources, C.L.; data curation, T.C.C.N. and L.P.O.; writing—original draft preparation, T.C.C.N. and L.P.O.; writ-ing—review and editing, T.C.C.N., L.P.O., V.D.H.d.C., T.P. and C.L.; visualization, T.C.C.N., V.D.H.d.C. and T.P.; supervision, C.L.; project administration, T.C.C.N.; funding acquisition, T.C.C.N. and C.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
We acknowledge the support from the Brazilian National Council for Scientific and Technological Development (CNPq) and Coordination for the Improvement of Higher Education (CAPES).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ghandour, Z.; Siciliani, L.; Straume, O.R. Investment and quality competition in healthcare markets. J. Health Econ. 2022, 82, 102588. [Google Scholar] [CrossRef] [PubMed]
- Massaro, M. Digital transformation in the healthcare sector through blockchain technology. Insights from academic research and business developments. Technovation 2021, 102386. [Google Scholar] [CrossRef]
- Dwivedi, Y.K.; Hughes, D.L.; Coombs, C.; Constantiou, I.; Duan, Y.; Edwards, J.S.; Gupta, B.; Lal, B.; Misra, S.; Prashant, P.; et al. Impact of COVID-19 pandemic on information management research and practice: Transforming education, work and life. Int. J. Inf. Manag. 2020, 55, 102211. [Google Scholar] [CrossRef]
- Leite, H.; Lindsay, C.; Kumar, M. COVID-19 outbreak: Implications on healthcare operations. TQM J. 2021, 33, 247–256. [Google Scholar] [CrossRef]
- Kamel, M.A.; Mousa, M.E.-S. Measuring operational efficiency of isolation hospitals during COVID-19 pandemic using data envelopment analysis: A case of Egypt. Benchmarking 2020, 28, 2178–2201. [Google Scholar] [CrossRef]
- Kohl, S.; Schoenfelder, J.; Fügener, A.; Brunner, J.O. The use of Data Envelopment Analysis (DEA) in healthcare with a focus on hospitals. Health Care Manag. Sci. 2019, 22, 245–286. [Google Scholar] [CrossRef]
- Cordero, J.M.; García-García, A.; Lau-Cortés, E.; Polo, C. Assessing Panamanian hospitals’ performance with alternative frontier methods. Int. Trans. Oper. Res. 2021. [Google Scholar] [CrossRef]
- Scippacercola, S.; Sepe, E. Critical comparison of the main methods for the technical efficiency. Electron. J. Appl. Stat. Anal. 2016, 9, 760–780. [Google Scholar] [CrossRef]
- Piubello Orsini, L.; Leardini, C.; Vernizzi, S.; Campedelli, B. Inefficiency of public hospitals: A multistage data envelopment analysis in an Italian region. BMC Health Serv. Res. 2021, 21, 1281. [Google Scholar] [CrossRef]
- Charnes, A.; Cooper, W.W.; Rhodes, E. Measuring the efficiency of decision-making units. Eur. J. Oper. Res. 1979, 3, 339. [Google Scholar] [CrossRef]
- O’Neill, L.; Rauner, M.; Heidenberger, K.; Kraus, M. A cross-national comparison and taxonomy of DEA-based hospital efficiency studies. Socioecon. Plann. Sci. 2008, 42, 158–189. [Google Scholar] [CrossRef]
- Zhang, X.; Tone, K.; Lu, Y. Impact of the Local Public Hospital Reform on the Efficiency of Medium-Sized Hospitals in Japan: An Improved Slacks-Based Measure Data Envelopment Analysis Approach. Health Serv. Res. 2018, 53, 896–918. [Google Scholar] [CrossRef] [PubMed]
- Nayar, P.; Ozcan, Y.A. Data envelopment analysis comparison of hospital efficiency and quality. J. Med. Syst. 2008, 32, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Ferrier, G.D.; Trivitt, J.S. Incorporating quality into the measurement of hospital efficiency: A double DEA approach. J. Product. Anal. 2013, 40, 337–355. [Google Scholar] [CrossRef]
- Wu, D.; Wu, D.D. Risk-Based Robust Evaluation of Hospital Efficiency. IEEE Syst. J. 2019, 13, 1906–1914. [Google Scholar] [CrossRef]
- Broadus, R.N. Toward a definition of “bibliometrics”. Scientometrics 1987, 12, 373–379. [Google Scholar] [CrossRef]
- Donthu, N.; Kumar, S.; Mukherjee, D.; Pandey, N.; Lim, W.M. How to conduct a bibliometric analysis: An overview and guidelines. J. Bus. Res. 2021, 133, 285–296. [Google Scholar] [CrossRef]
- Web of Science. Available online: https://www.webofscience.com/wos/woscc/basic-search (accessed on 13 January 2022).
- Web of Science. Available online: https://www.webofscience.com/wos/woscc/summary/19e2b276-091a-4b90-940a-2981442406bb-1e90b506/relevance/1 (accessed on 13 January 2022).
- Web of Science. Available online: https://www.webofscience.com/wos/woscc/summary/a9698216-4a73-46ee-a9e6-50535059194c-1e90ea1d/relevance/1 (accessed on 13 January 2022).
- Web of Science. Available online: https://www.webofscience.com/wos/woscc/summary/6ac5c3a3-3958-4c20-8eb0-9a6b2a5721fa-1e913490/relevance/1 (accessed on 13 January 2022).
- Web of Science. Available online: https://www.webofscience.com/wos/woscc/summary/71d1c2dc-5f7f-4a68-a328-720996eb04be-1e915b02/relevance/1 (accessed on 13 January 2022).
- Valdmanis, V.G.; Rosko, M.D.; Mutter, R.L. Hospital quality, efficiency, and input slack differentials. Health Serv. Res. 2008, 43, 1830–1848. [Google Scholar] [CrossRef]
- Pilyavsky, A.I.; Aaronson, W.E.; Bernet, P.M.; Rosko, M.D.; Valdmanis, V.G.; Golubchikov, M.V. East—West: Does it make a difference to hospital efficiencies in Ukraine? Health Econ. 2006, 15, 1173–1186. [Google Scholar] [CrossRef]
- Mutter, R.L.; Rosko, M.D.; Wong, H.S. Measuring Hospital Inefficiency: The Effects of Controlling for Qualityand Patient Burden of Illness. Health Serv. Res. 2008, 43, 1992–2013. [Google Scholar] [CrossRef]
- Mutter, R.L.; Greene, W.H.; Spector, W.; Rosko, M.D.; Mukamel, D.B. Investigating the impact of endogeneity on inefficiency estimates in the application of stochastic frontier analysis to nursing homes. J. Product. Anal. 2013, 39, 101–110. [Google Scholar] [CrossRef]
- Rosko, M.D.; Mutter, R.L. Inefficiency Differences between Critical Access Hospitals and Prospectively Paid Rural Hospitals. J. Health Polit. Policy Law 2010, 35, 95–126. [Google Scholar] [CrossRef] [PubMed]
- Rosko, M.D. Impact of HMO penetration and other environmental factors on hospitalX-inefficiency. Med. CARE Res. Rev. 2001, 58, 430–454. [Google Scholar] [CrossRef]
- Rosko, M.D.; Proenca, J.; Zinn, J.S.; Bazzoli, G.J. Hospital inefficiency: What is the impact of membership in different types of systems? Inq. J. Health CARE Organ. Provis. Financ. 2007, 44, 335–349. [Google Scholar] [CrossRef] [PubMed]
- Al-Amin, M.; Makarem, S.C.; Rosko, M. Efficiency and hospital effectiveness in improving Hospital Consumer Assessment of Healthcare Providers and Systems ratings. Health Care Manag. Rev. 2016, 41, 296–305. [Google Scholar] [CrossRef] [PubMed]
- Leleu, H.; Al-Amin, M.; Rosko, M.; Valdmanis, V.G. A robust analysis of hospital efficiency and factors affecting variability. Health Serv. Manag. Res. 2018, 31, 33–42. [Google Scholar] [CrossRef]
- Rosko, M.; Al-Amin, M.; Tavakoli, M. Efficiency and profitability in US not-for-profit hospitals. Int. J. Health Econ. Manag. 2020, 20, 359–379. [Google Scholar] [CrossRef]
- Rosko, M.; Wong, H.S.; Mutter, R. Characteristics of High- and Low-Efficiency Hospitals. Med. Care Res. Rev. 2018, 75, 454–478. [Google Scholar] [CrossRef]
- Langabeer, J.R.; Ozcan, Y.A. The economics of cancer care: Longitudinal changes in provider efficiency. Health Care Manag. Sci. 2009, 12, 192–200. [Google Scholar] [CrossRef]
- Ozcan, Y.A.; Begun, J.W.; McKinney, M.M. Benchmarking organ procurement organizations: A national study. Health Serv. Res. 1999, 34, 855–874. [Google Scholar]
- White, K.R.; Ozcan, Y.A. Church ownership and hospital efficiency. Hosp. Health Serv. Adm. 1996, 41, 297–310. [Google Scholar] [PubMed]
- Pakyz, A.L.; Ozcan, Y.A. Use of Data Envelopment Analysis to Quantify Opportunities for Antibacterial Targets for Reduction of Health Care–Associated Clostridium difficile Infection. Am. J. Med. Qual. 2014, 29, 437–444. [Google Scholar] [CrossRef] [PubMed]
- DePuccio, M.J.; Ozcan, Y.A. Exploring efficiency differences between medical home and non-medical home hospitals. Int. J. Healthc. Manag. 2017, 10, 147–153. [Google Scholar] [CrossRef]
- Özgen Narcı, H.; Ozcan, Y.A.; Şahin, İ.; Tarcan, M.; Narcı, M. An examination of competition and efficiency for hospital industry in Turkey. Health Care Manag. Sci. 2015, 18, 407–418. [Google Scholar] [CrossRef]
- Mancuso, P.; Valdmanis, V.G. Care Appropriateness and Health Productivity Evolution: A Non-Parametric Analysis of the Italian Regional Health Systems. Appl. Health Econ. Health Policy 2016, 14, 595–607. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Valdmanis, V.; Yu, T. Productivity growth in Chinese medical institutions during 2009–2018. Sustainability 2020, 12, 3080. [Google Scholar] [CrossRef]
- De Nicola, A.; Gitto, S.; Mancuso, P.; Valdmanis, V. Healthcare reform in Italy: An analysis of efficiency based on nonparametric methods. Int. J. Health Plann. Manag. 2014, 29, E48–E63. [Google Scholar] [CrossRef]
- Gholami, R.; Añón Higón, D.; Emrouznejad, A. Hospital performance: Efficiency or quality? Can we have both with IT? Expert Syst. Appl. 2015, 42, 5390–5400. [Google Scholar] [CrossRef]
- Vafaee Najar, A.; Pooya, A.; Alizadeh Zoeram, A.; Emrouznejad, A. Assessing the Relative Performance of Nurses Using Data Envelopment Analysis Matrix (DEAM). J. Med. Syst. 2018, 42, 125. [Google Scholar] [CrossRef]
- Omrani, H.; Shafaat, K.; Emrouznejad, A. An integrated fuzzy clustering cooperative game data envelopment analysis model with application in hospital efficiency. Expert Syst. Appl. 2018, 114, 615–628. [Google Scholar] [CrossRef]
- Safdar, K.A.; Emrouznejad, A.; Dey, P.K. Assessing the Queuing Process Using Data Envelopment Analysis: An Application in Health Centres. J. Med. Syst. 2016, 40, 32. [Google Scholar] [CrossRef] [PubMed]
- Kirigia, J.M.; Sambo, L.G.; Emrouznejad, A. Technical efficiency of public hospitals in Kenya. J. Med. Syst. 2002, 26, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Stefko, R.; Gavurova, B.; Kocisova, K. Healthcare efficiency assessment using DEA analysis in the Slovak Republic. Health Econ. Rev. 2018, 8, 6. [Google Scholar] [CrossRef] [PubMed]
- Kočišová, K.; Cygańska, M.; Kludacz-Alessandri, M. The application of data envelopment analysis for evaluation of efficiency of healthcare delivery for cvd patients. Econ. Manag. 2020, 23, 96–113. [Google Scholar] [CrossRef]
- Kocisova, K.; Hass-Symotiuk, M.; Kludacz-Alessandri, M. Use of the DEA method to verify the performance model for hospitals. Econ. Manag. 2018, 21, 125–140. [Google Scholar] [CrossRef]
- Kocisova, K.; Gavurova, B.; Behun, M. The importance of implementing environmental variables in the process of assessment of healthcare efficiency through DEA. Ekon. Cas. 2019, 2019, 367–387. [Google Scholar]
- Ancarani, A.; Ayach, A.; Di Mauro, C.; Gitto, S.; Mancuso, P. Does Religious Diversity in Health Team Composition Affect Efficiency? Evidence from Dubai. Br. J. Manag. 2016, 27, 740–759. [Google Scholar] [CrossRef]
- Ancarani, A.; Di Mauro, C.; Gitto, S.; Mancuso, P.; Ayach, A. Technology acquisition and efficiency in Dubai hospitals. Technol. Forecast. Soc. Chang. 2016, 113, 475–485. [Google Scholar] [CrossRef]
- Watanabe, Y.; Noguchi, H.; Nakata, Y. How efficient are surgical treatments in Japan? The case of a high-volume Japanese hospital. Health Care Manag. Sci. 2020, 23, 401–413. [Google Scholar] [CrossRef]
- Nakata, Y.; Watanabe, Y.; Otake, H. Equality of Surgical Fee Schedule in Japan: A Retrospective Observational Study. Health Serv. Insights 2021, 14, 11786329211048130. [Google Scholar] [CrossRef]
- Nakata, Y.; Watanabe, Y.; Narimatsu, H.; Yoshimura, T.; Otake, H.; Sawa, T. Predictors of surgeons’ efficiency in the operating rooms. Health Serv. Manag. Res. 2017, 30, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Nakata, Y.; Yoshimura, T.; Watanabe, Y.; Otake, H.; Oiso, G.; Sawa, T. Efficiency of inpatient orthopedic surgery in Japan: A medical claims database analysis. Int. J. Health Care Qual. Assur. 2017, 30, 506–515. [Google Scholar] [CrossRef] [PubMed]
- Yin, G.; Chen, C.; Zhuo, L.; He, Q.; Tao, H. Efficiency comparison of public hospitals under different administrative affiliations in china: A pilot city case. Healthcare 2021, 9, 437. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Lu, W.; Tao, H. Efficiency of health resource utilisation in primary-level maternal and child health hospitals in Shanxi Province, China: A bootstrapping data envelopment analysis and truncated regression approach. BMC Health Serv. Res. 2020, 20, 179. [Google Scholar] [CrossRef]
- Cheng, Z.; Cai, M.; Tao, H.; He, Z.; Lin, X.; Lin, H.; Zuo, Y. Efficiency and productivity measurement of rural township hospitals in China: A bootstrapping data envelopment analysis. BMJ Open 2016, 6, e011911. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Z.; Tao, H.; Cai, M.; Lin, H.; Lin, X.; Shu, Q.; Zhang, R.N. Technical efficiency and productivity of Chinese county hospitals: An exploratory study in Henan province, China. BMJ Open 2015, 5, e007267. [Google Scholar] [CrossRef] [PubMed]
- Van Eck, N.J.; Waltman, L. Visualizing Bibliometric Networks. In Measuring Scholarly Impact: Methods and Practice; Ding, Y., Rousseau, R., Wolfram, D., Eds.; Springer International Publishing: Cham, Switzerland, 2014; pp. 285–320. ISBN 978-3-319-10377-8. [Google Scholar]
- Seidman, S.B. Network structure and minimum degree. Soc. Netw. 1983, 5, 269–287. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Group, P.-P.; Altman, D.G.; et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Daraio, C.; Nepomuceno, T.C.C.; Costa, A.P.C.S. Theoretical and Empirical Advances in the Assessment of Productive Efficiency since the introduction of DEA: A Bibliometric Analysis. Int. J. Oper. Res. 2020. [Google Scholar] [CrossRef]
- Van Eck, N.J.; Waltman, L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics 2010, 84, 523–538. [Google Scholar] [CrossRef]
- Chang, S.J.; Hsiao, H.C.; Huang, L.H.; Chang, H. Taiwan quality indicator project and hospital productivity growth. Omega 2011, 39, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Lacalle, J.; Martin, E. Rural vs urban hospital performance in a “competitive” public health service. Soc. Sci. Med. 2010, 71, 1131–1140. [Google Scholar] [CrossRef] [PubMed]
- Sultan, W.I.M.; Crispim, J. Measuring the efficiency of Palestinian public hospitals during 2010–2015: An application of a two-stage DEA method. BMC Health Serv. Res. 2018, 18, 381. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.S.; Chun, K.H.; Lee, J.S. Reforming the hospital service structure to improve efficiency: Urban hospital specialization. Health Policy 2008, 87, 41–49. [Google Scholar] [CrossRef]
- Lee, K.H.; Yang, S.B.; Choi, M. The association between Hospital ownership and technical efficiency in a managed care environment. J. Med. Syst. 2009, 33, 307–315. [Google Scholar] [CrossRef]
- Kawaguchi, H.; Tone, K.; Tsutsui, M. Estimation of the efficiency of Japanese hospitals using a dynamic and network data envelopment analysis model. Health Care Manag. Sci. 2014, 17, 101–112. [Google Scholar] [CrossRef]
- Giménez, V.; Prieto, W.; Prior, D.; Tortosa-Ausina, E. Evaluation of efficiency in Colombian hospitals: An analysis for the post-reform period. Socioecon. Plann. Sci. 2019, 65, 20–35. [Google Scholar] [CrossRef]
- Liu, T.; Li, J.; Chen, J.; Yang, S. Regional differences and influencing factors of allocation efficiency of rural public health resources in china. Healthcare 2020, 8, 270. [Google Scholar] [CrossRef]
- Alonso, J.M.; Clifton, J.; Díaz-Fuentes, D. The impact of New Public Management on efficiency: An analysis of Madrid’s hospitals. Health Policy 2015, 119, 333–340. [Google Scholar] [CrossRef]
- Amare, T.; Yitayal, M.; Amare, G. Technical efficiency of maternal health services provision in public hospitals of northwest ethiopia: A two-stage data envelopment analysis. Risk Manag. Healthc. Policy 2020, 13, 3135–3146. [Google Scholar] [CrossRef]
- Araújo, C.; Barros, C.P.; Wanke, P. Efficiency determinants and capacity issues in Brazilian for-profit hospitals. Health Care Manag. Sci. 2014, 17, 126–138. [Google Scholar] [CrossRef] [PubMed]
- Caballer-Tarazona, M.; Clemente-Collado, A.; Vivas-Consuelo, D. A cost and performance comparison of Public Private Partnership and public hospitals in Spain. Health Econ. Rev. 2016, 6, 17. [Google Scholar] [CrossRef] [PubMed]
- Caballer-Tarazona, M.; Moya-Clemente, I.; Vivas-Consuelo, D.; Barrachina-Martínez, I. A model to measure the efficiency of hospital performance. Math. Comput. Model. 2010, 52, 1095–1102. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, J.; Zhu, J.; Sherman, H.D.; Chou, S.Y. How the Great Recession affects performance: A case of Pennsylvania hospitals using DEA. Ann. Oper. Res. 2019, 278, 77–99. [Google Scholar] [CrossRef]
- Du, T. Performance measurement of healthcare service and association discussion between quality and efficiency: Evidence from 31 provinces of mainland China. Sustainability 2018, 10, 74. [Google Scholar] [CrossRef]
- Ferreira, D.C.; Marques, R.C. Do quality and access to hospital services impact on their technical efficiency? Omega 2019, 86, 218–236. [Google Scholar] [CrossRef]
- Gok, M.S.; Sezen, B. Analyzing the ambiguous relationship between efficiency, quality and patient satisfaction in healthcare services: The case of public hospitals in Turkey. Health Policy 2013, 111, 290–300. [Google Scholar] [CrossRef]
- Jat, T.R.; Sebastian, M.S. Technical efficiency of public district hospitals in Madhya Pradesh, India: A data envelopment analysis. Glob. Health Action 2013, 6, 21742. [Google Scholar] [CrossRef]
- Jiang, S.; Min, R.; Fang, P.Q. The impact of healthcare reform on the efficiency of public county hospitals in China. BMC Health Serv. Res. 2017, 17, 838. [Google Scholar] [CrossRef]
- Kim, Y.; Lee, K.H.; Choi, S.W. Multifaced evidence of hospital performance in Pennsylvania. Healthcare 2021, 9, 670. [Google Scholar] [CrossRef]
- Lefèvre, M.; Bouckaert, N.; Camberlin, C.; Van de Voorde, C. Economies of scale and optimal size of maternity services in Belgium: A Data Envelopment Analysis. Int. J. Health Plann. Manag. 2022, 37, 1421–1438. [Google Scholar] [CrossRef]
- Liu, J.; He, B.; Xu, X.; Zhou, L.; Li, J.; Wang, G.; Chen, Y. Determinants of efficiency growth of county-level public hospitals-evidence from Chongqing, China. BMC Health Serv. Res. 2019, 19, 858. [Google Scholar] [CrossRef] [PubMed]
- Mitropoulos, P. Production and quality performance of healthcare services in EU countries during the economic crisis. Oper. Res. 2021, 21, 857–873. [Google Scholar] [CrossRef]
- Navarro-Espigares, J.L.; Torres, E.H. Efficiency and quality in health services: A crucial link. Serv. Ind. J. 2011, 31, 385–403. [Google Scholar] [CrossRef]
- Vrabková, I.; Vaňková, I. Efficiency of human resources in public hospitals: An example from the Czech Republic. Int. J. Environ. Res. Public Health 2021, 18, 4711. [Google Scholar] [CrossRef]
- Wang, X.; Luo, H.; Qin, X.; Feng, J.; Gao, H.; Feng, Q. Evaluation of performance and impacts of maternal and child health hospital services using Data Envelopment Analysis in Guangxi Zhuang Autonomous Region, China: A comparison study among poverty and non-poverty county level hospitals. Int. J. Equity Health 2016, 15, 131. [Google Scholar] [CrossRef]
- Zare, Z. Service performance in public healthcare system: Data envelopment analysis. AD-Minister 2017, 237–265. [Google Scholar] [CrossRef]
- Zheng, W.; Sun, H.; Zhang, P.; Zhou, G.; Jin, Q.; Lu, X. A four-stage DEA-based efficiency evaluation of public hospitals in China after the implementation of new medical reforms. PLoS ONE 2018, 13, e0203780. [Google Scholar] [CrossRef]
- Akkan, C.; Karadayi, M.A.; Ekinci, Y.; Ülengin, F.; Uray, N.; Karaosmanoğlu, E. Efficiency analysis of emergency departments in metropolitan areas. Socioecon. Plann. Sci. 2020, 69, 100679. [Google Scholar] [CrossRef]
- Aletras, V.; Kontodimopoulos, N.; Zagouldoudis, A.; Niakas, D. The short-term effect on technical and scale efficiency of establishing regional health systems and general management in Greek NHS hospitals. Health Policy 2007, 83, 236–245. [Google Scholar] [CrossRef]
- Barnum, D.T.; Johnson, M.; Gleason, J.M. Importance of Statistical Evidence in Estimating Valid DEA Scores. J. Med. Syst. 2016, 40, 47. [Google Scholar] [CrossRef] [PubMed]
- Dotoli, M.; Epicoco, N.; Falagario, M.; Sciancalepore, F. A cross-efficiency fuzzy Data Envelopment Analysis technique for performance evaluation of Decision Making Units under uncertainty. Comput. Ind. Eng. 2015, 79, 103–114. [Google Scholar] [CrossRef]
- Ekiz Bozdemir, M.K.; Avci, S.; Aladag, Z. Assessment of the Turkish Health Transformation Program with Data Envelopment Analysis. IEEE Trans. Eng. Manag. 2021, 1–9. [Google Scholar] [CrossRef]
- Flokou, A.; Kontodimopoulos, N.; Niakas, D. Employing post-DEA cross-evaluation and cluster analysis in a sample of Greek NHS hospitals. J. Med. Syst. 2011, 35, 1001–1014. [Google Scholar] [CrossRef]
- Girginer, N.; Köse, T.; Uçkun, N. Efficiency Analysis of Surgical Services by Combined Use of Data Envelopment Analysis and Gray Relational Analysis. J. Med. Syst. 2015, 39, 56. [Google Scholar] [CrossRef] [PubMed]
- Halkos, G.E.; Tzeremes, N.G. A conditional nonparametric analysis for measuring the efficiency of regional public healthcare delivery: An application to Greek prefectures. Health Policy 2011, 103, 73–82. [Google Scholar] [CrossRef]
- Hasni, M.; Layeb, S.B.; Aissaoui, N.O.; Mannai, A. Hybrid model for a cross-department efficiency evaluation in healthcare systems. Manag. Decis. Econ. 2021, 43, 1311–1329. [Google Scholar] [CrossRef]
- Jahangoshai Rezaee, M.; Karimdadi, A.; Izadbakhsh, H. Road map for progress and attractiveness of Iranian hospitals by integrating self-organizing map and context-dependent DEA. Health Care Manag. Sci. 2019, 22, 410–436. [Google Scholar] [CrossRef]
- Jahangoshai Rezaee, M.; Moini, A.; Haji-Ali Asgari, F. Unified performance evaluation of health centers with integrated model of data envelopment analysis and bargaining game. J. Med. Syst. 2012, 36, 3805–3815. [Google Scholar] [CrossRef]
- Katharaki, M. Approaching the management of hospital units with an operation research technique: The case of 32 Greek obstetric and gynaecology public units. Health Policy 2008, 85, 19–31. [Google Scholar] [CrossRef]
- Kounetas, K.; Papathanassopoulos, F. How efficient are Greek hospitals? A case study using a double bootstrap DEA approach. Eur. J. Health Econ. 2013, 14, 979–994. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.; Deng, Y.J.; Lu, W.M.; Kweh, Q.L. Impulse response function analysis of the impacts of hospital accreditations on hospital efficiency. Health Care Manag. Sci. 2019, 22, 394–409. [Google Scholar] [CrossRef] [PubMed]
- Mitropoulos, P.; Talias, M.A.; Mitropoulos, I. Combining stochastic DEA with Bayesian analysis to obtain statistical properties of the efficiency scores: An application to Greek public hospitals. Eur. J. Oper. Res. 2015, 243, 302–311. [Google Scholar] [CrossRef]
- Ramírez-Valdivia, M.T.; Maturana, S.; Salvo-Garrido, S. A multiple stage approach for performance improvement of primary healthcare practice. J. Med. Syst. 2011, 35, 1015–1028. [Google Scholar] [CrossRef] [PubMed]
- Rouyendegh, B.D.; Oztekin, A.; Ekong, J.; Dag, A. Measuring the efficiency of hospitals: A fully-ranking DEA–FAHP approach. Ann. Oper. Res. 2019, 278, 361–378. [Google Scholar] [CrossRef]
- Wei, F.; Zhang, X.; Song, J.; Yang, F. Efficiency evaluation of healthcare services in China based on stochastic multicriteria acceptability analysis and directional distance function. Int. Trans. Oper. Res. 2021. [Google Scholar] [CrossRef]
- Yaya, S.; Xi, C.; Xiaoyang, Z.; Meixia, Z. Evaluating the efficiency of China’s healthcare service: A weighted DEA-game theory in a competitive environment. J. Clean. Prod. 2020, 270, 122431. [Google Scholar] [CrossRef]
- Zare, H.; Tavana, M.; Mardani, A.; Masoudian, S.; Kamali Saraji, M. A hybrid data envelopment analysis and game theory model for performance measurement in healthcare. Health Care Manag. Sci. 2019, 22, 475–488. [Google Scholar] [CrossRef]
- Zheng, D.; Gong, J.; Zhang, C. Efficiency of medical service systems in the rural areas of Mainland China: A comparative study from 2013 to 2017. Public Health 2019, 171, 139–147. [Google Scholar] [CrossRef]
- Zhou, L.; Xu, X.; Antwi, H.A.; Wang, L. Towards an equitable healthcare in China: Evaluating the productive efficiency of community health centers in Jiangsu Province. Int. J. Equity Health 2017, 16, 89. [Google Scholar] [CrossRef]
- Nepomuceno, T.C.C.; Silva, W.M.N.; Nepomuceno, K.T.C.; Barros, I.K.F. A DEA-Based Complexity of Needs Approach for Hospital Beds Evacuationduring the COVID-19 Outbreak. J. Healthc. Eng. 2020, 2020, 8857553. [Google Scholar] [CrossRef] [PubMed]
- Nepomuceno, T.C.C.; Santiago, K.T.M.; Daraio, C.; Costa, A.P.C.S. Exogenous crimes and the assessment of public safety efficiency and effectiveness. Ann. Oper. Res. 2020. [Google Scholar] [CrossRef]
- Kessler, M.M. Bibliographic coupling between scientific papers. Am. Doc. 1963, 14, 10–25. [Google Scholar] [CrossRef]
- van Lent, W.A.M.; Sanders, E.M.; van Harten, W.H. Exploring improvements in patient logistics in Dutch hospitals with asurvey. BMC Health Serv. Res. 2012, 12, 232. [Google Scholar] [CrossRef] [PubMed]
- Abiodun, A.J.; Adeyemi, K.S. Performance role models among public health facilities: An application of data envelopment analysis. Int. J. Healthc. Manag. 2020, 13, 193–200. [Google Scholar] [CrossRef]
- Ahmed, S.; Hasan, M.Z.; MacLennan, M.; Dorin, F.; Ahmed, M.W.; Hasan, M.M.; Hasan, S.M.; Islam, M.T.; Khan, J.A.M. Measuring the efficiency of health systems in Asia: A data envelopment analysis. BMJ Open 2019, 9, e022155. [Google Scholar] [CrossRef]
- Ahmed, S.; Hasan, M.Z.; Laokri, S.; Jannat Zerinand Ahmed, M.W.; Dorin, F.; Vargas, V.; Khan, J.A.M. Technical efficiency of public district hospitals in Bangladesh: A dataenvelopment analysis. Cost Eff. Resour. Alloc. 2019, 17, 15. [Google Scholar] [CrossRef]
- Aksezer, C.S. Reliability evaluation of healthcare services by assessing the technical efficiency. Serv. Ind. J. 2011, 31, 2309–2319. [Google Scholar] [CrossRef]
- Alhassan, R.K.; Nketiah-Amponsah, E.; Akazili, J.; Spieker, N.; Arhinful, D.K.; de Wit, T.F.R. Efficiency of private and public primary health facilities accredited by the National Health Insurance Authority in Ghana. Cost Eff. Resour. Alloc. 2015, 13, 23. [Google Scholar] [CrossRef]
- Alikhasi, M.; Vasili, M. Development of a discrete locating model for the healthcare facilitiesconsidering efficiency and readiness. Rev. Gest. Tecnol. Manag. Technol. 2020, 20, 30–53. [Google Scholar] [CrossRef]
- Aloh, H.E.; Onwujekwe, O.E.; Ichoku, H.E.; Osigwe, A.C. Scaling up Maternal and Child Healthcare Delivery among MissionHospitals in Southeast Nigeria: An Empirical Application of Data Envelopment Analysis for Setting Benchmarks and Targets. Afr. J. Reprod. Health 2019, 23, 57–67. [Google Scholar] [CrossRef]
- Andrews, A. The Efficiency of New Zealand District Health Boards in Administrating Public Funds: An Application of Bootstrap DEA and Beta Regression. Int. J. Public Adm. 2021, 44, 1297–1308. [Google Scholar] [CrossRef]
- Ayiko, R.; Mujasi, P.N.; Abaliwano, J.; Turyareeba, D.; Enyaku, R.; Anguyo, R.; Odoch, W.; Bakibinga, P.; Aliti, T. Levels, trends and determinants of technical efficiency of general hospitals in Uganda: Data envelopment analysis and Tobit regression analysis. BMC Health Serv. Res. 2020, 20, 916. [Google Scholar] [CrossRef] [PubMed]
- Azadeh, A.; Haghighi, S.M.; Gaeini, Z.; Shabanpour, N. Optimization of healthcare supply chain in context of macro-ergonomicsfactors by a unique mathematical programming approach. Appl. Ergon. 2016, 55, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Bahrami, M.A.; Rafiei, S.; Abedi, M.; Askari, R. Data envelopment analysis for estimating efficiency of intensive care units: A case study in Iran. Int. J. Health Care Qual. Assur. 2018, 31, 276–282. [Google Scholar] [CrossRef]
- Ben-Arieh, D.; Gullipalli, D.K. Data Envelopment Analysis of clinics with sparse data: Fuzzy clustering approach. Comput. Ind. Eng. 2012, 63, 13–21. [Google Scholar] [CrossRef][Green Version]
- Binyaruka, P.; Anselmi, L. Understanding efficiency and the effect of pay-for-performance across health facilities in Tanzania. BMJ Glob. Health 2020, 5, e002326. [Google Scholar] [CrossRef]
- Cakmak Barsbay, M. Energy efficiency analysis in public hospitals: An application of radialand non-radial data envelopment analysis models. Pamukkale Univ. J. Eng. Sci. Muhendis. Bilim. Derg. 2021, 27, 35–42. [Google Scholar] [CrossRef]
- Chai, P.; Wan, Q.; Kinfu, Y. Efficiency and productivity of health systems in prevention and control of non-communicable diseases in China, 2008–2015. Eur. J. Health Econ. 2021, 22, 267–279. [Google Scholar] [CrossRef]
- Chitnis, A.; Mishra, D.K. Performance Efficiency of Indian Private Hospitals Using Data Envelopment Analysis and Super-efficiency DEA. J. Health Manag. 2019, 21, 279–293. [Google Scholar] [CrossRef]
- Devaraj, S.; Patel, P.C. Negative Association of Hospital Efficiency under Increasing Geographic Elevation on Acute Myocardial Infarction In-Patient Mortality. J. Healthc. Qual. 2018, 40, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Erus, B.; Hatipoglu, O. Physician payment schemes and physician productivity: Analysis of Turkish healthcare reforms. Health Policy 2017, 121, 553–557. [Google Scholar] [CrossRef] [PubMed]
- Fumbwe, F.; Lihawa, R.; Andrew, F.; Kinyanjui, G.; Mkuna, E. Examination on level of scale efficiency in public hospitals in Tanzania. Cost Eff. Resour. Alloc. 2021, 19, 49. [Google Scholar] [CrossRef] [PubMed]
- Giménez, V.; Prior, D.; Keith, J.R. Strategic alliances’ effects over hospital efficiency and capacity utilization in México. Acad. Rev. Latinoam. Adm. 2020, 33, 128–146. [Google Scholar] [CrossRef]
- Hamid, M.; Tavakkoli-Moghaddam, R.; Golpaygani, F.; Vahedi-Nouri, B. A multi-objective model for a nurse scheduling problem by emphasizing human factors. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2020, 234, 179–199. [Google Scholar] [CrossRef]
- Ibrahim, M.D.; Daneshvar, S. Efficiency Analysis of Healthcare System in Lebanon Using Modified Data Envelopment Analysis. J. Healthc. Eng. 2018, 2018, 2060138. [Google Scholar] [CrossRef]
- Kakemam, E.; Dargahi, H. The health sector evolution plan and the technical efficiency of public hospitals in Iran. Iran. J. Public Health 2019, 48, 1681–1689. [Google Scholar] [CrossRef]
- Khaldi, R.; El Afia, A.; Chiheb, R. Performance prediction of pharmaceutical suppliers: Comparative studybetween DEA-ANFIS-PSO and DEA-ANFIS-GA. Int. J. Comput. Appl. Technol. 2019, 60, 317–325. [Google Scholar] [CrossRef]
- Kim, J.R.; Jeon, E.C.; Cho, S.; Kim, H. The promotion of environmental management in the South Korean health sector-case study. Sustainability 2018, 10, 2081. [Google Scholar] [CrossRef]
- Kwon, H.B.; Marvel, J.H.; Roh, J.J. Three-stage performance modeling using DEA–BPNN for better practice benchmarking. Expert Syst. Appl. 2017, 71, 429–441. [Google Scholar] [CrossRef]
- Lai, K.K.; Cheung, M.T.; Fu, Y.L. Resource Allocation in Public Healthcare: A Team-DEA Model. J. Syst. Sci. Complex. 2018, 31, 463–472. [Google Scholar] [CrossRef]
- Lamovšek, N.; Klun, M. Efficiency of Medical Laboratories after Quality Standard Introduction: Trend Analysis of EU Countries and Case Study from Slovenia. Cent. Eur. Public Adm. Rev. 2020, 18, 143–163. [Google Scholar] [CrossRef]
- Lan, T.; Chen, T.; Hu, Y.; Yang, Y.; Pan, J. Governmental Investments in Hospital Infrastructure Among Regions and Its Efficiency in China: An Assessment of Building Construction. Front. Public Health 2021, 9, 1553. [Google Scholar] [CrossRef] [PubMed]
- Lari, M.S.; Sefiddashti, S.E. Measuring the Efficiency of Health Systems: A Case of Mental Health inMiddle East and North Africa Countries. Iran. J. Public Health 2021, 50, 1017–1027. [Google Scholar]
- Lesniowska-Gontarz, M. Evaluation of Technical Efficiency in Financial Dimension of Privatemedical Entities in Podkarpackie Voivodhip—Dea Approach. Financ. Internet Q. 2021, 17, 24–31. [Google Scholar] [CrossRef]
- Li, H.; Dong, S.; Liu, T. Relative efficiency and productivity: A preliminary exploration of public hospitals in Beijing, China. BMC Health Serv. Res. 2014, 14, 158. [Google Scholar] [CrossRef]
- Li, Y.; Lin, T.-Y.; Chiu, Y.-H. Dynamic linkages among economic development, environmental pollution andhuman health in Chinese. Cost Eff. Resour. Alloc. 2020, 18, 1–19. [Google Scholar] [CrossRef]
- Mirmozaffari, M.; Shadkam, E.; Khalili, S.M.; Yazdani, M. Developing a Novel Integrated Generalised Data Envelopment Analysis(DEA) to Evaluate Hospitals Providing Stroke Care Services. Bioengineering 2021, 8, 207. [Google Scholar] [CrossRef]
- Noveiri, M.J.S.; Kordrostami, S. Sustainability assessment using a fuzzy DEA aggregation approach: A healthcare application. SOFT Comput. 2021, 25, 10829–10849. [Google Scholar] [CrossRef]
- Nuti, S.; Daraio, C.; Speroni, C.; Vainieri, M. Relationships between technical efficiency and the quality and costs of health care in Italy. Int. J. Qual. Health Care 2011, 23, 324–330. [Google Scholar] [CrossRef][Green Version]
- Otay, I.; Oztaysi, B.; Onar, S.C.; Kahraman, C. Multi-expert performance evaluation of healthcare institutions using an integrated intuitionistic fuzzy AHP&DEA methodology. Knowl.-Based Syst. 2017, 133, 90–106. [Google Scholar] [CrossRef]
- Parmar, D.; Rai, M. Performance Evaluation of Combined Biomedical Waste Treatment Plants with Specific Focus on Incinerators Using Data Envelope Analysis in Uttar Pradesh, India. J. Hazard. Toxic Radioact. Waste 2017, 21, 05016002. [Google Scholar] [CrossRef]
- Pereira, M.A.; Ferreira, D.C.; Figueira Jose Ruiand Marques, R.C. Measuring the efficiency of the Portuguese public hospitals: A valuemodelled network data envelopment analysis with simulation. Expert Syst. Appl. 2021, 181, 115169. [Google Scholar] [CrossRef]
- Rego, G.; Nunes, R.; Costa, J. The challenge of corporatisation: The experience of Portuguese publichospitals. Eur. J. Health Econ. 2010, 11, 367–381. [Google Scholar] [CrossRef] [PubMed]
- Rezaee, M.J.; Yousefi, S.; Hayati, J. A decision system using fuzzy cognitive map and multi-group data envelopment analysis to estimate hospitals’ outputs level. Neural Comput. Appl. 2018, 29, 761–777. [Google Scholar] [CrossRef]
- Roth, A.; Tucker, A.L.; Venkataraman, S.; Chilingerian, J. Being on the Productivity Frontier: Identifying “Triple Aim Performance” Hospitals. Prod. Oper. Manag. 2019, 28, 2165–2183. [Google Scholar] [CrossRef]
- Sapienza, F.; Matranga, D. Evaluating the reform of the healthcare system in sicily: Variations of efficiency and appropriateness between 2008 and 2010. Epidemiol. Biostat. Public Health 2018, 15, e12593-1–e12593-10. [Google Scholar] [CrossRef]
- Sinimole, K.R. Performance Evaluation of Healthcare Systems: A Study on NRHM Programme in Kerala. J. Health Manag. 2017, 19, 121–131. [Google Scholar] [CrossRef]
- Tavana, M.; Nazari-Shirkouhi, S.; Farzaneh Kholghabad, H. An integrated quality and resilience engineering framework in healthcare with Z-number data envelopment analysis. Health Care Manag. Sci. 2021, 24, 768–785. [Google Scholar] [CrossRef]
- Top, M.; Konca, M.; Sapaz, B. Technical efficiency of healthcare systems in African countries: An application based on data envelopment analysis. Health Policy Technol. 2020, 9, 62–68. [Google Scholar] [CrossRef]
- Wei, C.-K.; Chen, L.-C.; Li, R.-K.; Tsai, C.-H.; Huang, H.-L. A study of optimal weights of Data Envelopment Analysis—Development ofa context-dependent DEA-R model. Expert Syst. Appl. 2012, 39, 4599–4608. [Google Scholar] [CrossRef]
- Yang, S.-W.; Chu, K.-C.; Kreng, V.B. The Impact of Global Budgeting on the Efficiency of Healthcare under aSingle-Payer System in Taiwan. Int. J. Environ. Res. Public Health 2021, 18, 10983. [Google Scholar] [CrossRef]
- Yang, W.; Cai, L.L.; Edalatpanah, S.A.; Smarandache, F. Triangular Single Valued Neutrosophic Data Envelopment Analysis: Application to Hospital Performance Measurement. Symmetry 2020, 12, 588. [Google Scholar] [CrossRef]
- Zhu, J.; Song, X. Changes in efficiency of tertiary public general hospitals during the reform of public hospitals in Beijing, China. Int. J. Health Plann. Manag. 2022, 37, 143–155. [Google Scholar] [CrossRef] [PubMed]
- Abolghasem, S.; Toloo, M.; Amézquita, S. Cross-efficiency evaluation in the presence of flexible measures with an application to healthcare systems. Health Care Manag. Sci. 2019, 22, 512–533. [Google Scholar] [CrossRef] [PubMed]
- Adelman, D. An efficient frontier approach to scoring and ranking hospital performance. Oper. Res. 2020, 68, 762–792. [Google Scholar] [CrossRef]
- Ali, M.; Wang, W.; Chaudhry, N.; Geng, Y.; Ashraf, U. Assessing knowledge, performance, and efficiency for hospital waste management—a comparison of government and private hospitals in Pakistan. Environ. Monit. Assess. 2017, 189, 181. [Google Scholar] [CrossRef]
- Bao, C.; Bardhan, I.R. Performance of Accountable Care Organizations: Health Information Technology and Quality–Efficiency Trade-Offs. Inf. Syst. Res. 2021, 33, 399–764. [Google Scholar] [CrossRef]
- Bastian, N.D.; Kang, H.; Swenson, E.R.; Fulton, L.V.; Griffin, P.M. Evaluating the Impact of Hospital Efficiency on Wellness in the MilitaryHealth System. Mil. Med. 2016, 181, 827–834. [Google Scholar] [CrossRef][Green Version]
- Buckell, J.; Smith, A.; Longo, R.; Holland, D. Efficiency, heterogeneity and cost function analysis: Empirical evidencefrom pathology services in the National Health Service in England. Appl. Econ. 2015, 47, 3311–3331. [Google Scholar] [CrossRef]
- Butala, N.M.; Hidrue, M.K.; Swersey, A.J.; Singh, J.P.; Weilburg, J.B.; Ferris, T.G.; Armstrong, K.A.; Wasfy, J.H. Measuring individual physician clinical productivity in an era of consolidated group practices. Health J. Deliv. Sci. Innov. 2019, 7. [Google Scholar] [CrossRef]
- Chen, Z.S.; Chen, X.L.; Gan, X.Q.; Bai, K.X.; Balezentis, T.; Cui, L.X. Technical Efficiency of Regional Public Hospitals in China Based on the Three-Stage DEA. Int. J. Environ. Res. Public Health 2020, 17, 9383. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.H.; Fortsch, S.M.; Park, I.; Jung, I. Efficiency of U.S. hospitals between 2001 and 2011. Manag. Decis. Econ. 2017, 38, 1071–1081. [Google Scholar] [CrossRef]
- Ferreira, D.; Marques, R.C. Identifying congestion levels, sources and determinants on intensive care units: The Portuguese case. Health Care Manag. Sci. 2018, 21, 348–375. [Google Scholar] [CrossRef] [PubMed]
- Foo, C.Y.; Lim, K.K.; Sivasampu, S.; Dahian, K.B.; Goh, P.P. Improving the effectiveness of service delivery in the public healthcare sector: The case of ophthalmology services in Malaysia. BMC Health Serv. Res. 2015, 15, 349. [Google Scholar] [CrossRef]
- Haeri, A.; Hosseini-Motlagh, S.M.; Samani, M.R.G.; Rezaei, M. An integrated socially responsible-efficient approach toward health service network design. Ann. Oper. Res. 2021, 1–54. [Google Scholar] [CrossRef]
- Han, A.; Lee, K.-H. The Impact of Public Reporting Schemes and Market Competition onHospital Efficiency. Healthcare 2021, 9, 1031. [Google Scholar] [CrossRef]
- Jiang, N.; Andrews, A. Efficiency of New Zealand’s District Health Boards at Providing Hospital Services: A stochastic frontier analysis. J. Product. Anal. 2020, 53, 53–68. [Google Scholar] [CrossRef]
- Kawaguchi, H.; Hashimoto, H.; Matsuda, S. Efficacy of a numerical value of a fixed-effect estimator in stochastic frontier analysis as an indicator of hospital production structure. BMC Health Serv. Res. 2012, 12, 334. [Google Scholar] [CrossRef]
- Kuntz, L.; Scholtes, S.; Vera, A. Incorporating efficiency in hospital-capacity planning in Germany. Eur. J. Health Econ. 2007, 8, 213–223. [Google Scholar] [CrossRef]
- Kuntz, L.; Scholtes, S.; Vera, A. DRG cost weight volatility and hospital performance. OR Spectr. 2008, 30, 331–354. [Google Scholar] [CrossRef]
- Li, D.; Chao, J.Q.; Kong, J.; Cao, G.; Lv, M.R.; Zhang, M. The efficiency analysis and spatial implications of health information technology: A regional exploratory study in China. Health Inform. J. 2020, 26, 1700–1713. [Google Scholar] [CrossRef] [PubMed]
- Liu, X. The efficiency of healthcare facilities providing PET cancer screening in Japan. Jpn. J. Radiol. 2012, 30, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Franco Miguel, J.L.; Fullana Belda, C.; Cordero Ferrera, J.M.; Polo, C.; Nuño-Solinís, R. Efficiency in chronic illness care coordination: Public-private collaboration models vs. traditional management. BMC Health Serv. Res. 2020, 20, 1044. [Google Scholar] [CrossRef] [PubMed]
- Nedelea, I.C.; Fannin, J.M. Testing for cost efficiency differences between two groups of rural hospitals. Int. J. Healthc. Manag. 2017, 10, 57–65. [Google Scholar] [CrossRef]
- Pai, D.; Hosseini, H. Analyzing Operational and Financial Performance of Us Hospitals Using Two-Stage Production Process; Lawrence, K.D., Klimberg, R.K., Eds.; IAP-Information Age Publishing: Charlotte, NC, USA, 2018; Volume 3, ISBN 978-1-64113-054-7. [Google Scholar]
- Pope, B.; Johnson, A. Returns to scope: A metric for production synergies demonstrated for hospital production. J. Product. Anal. 2013, 40, 239–250. [Google Scholar] [CrossRef]
- Pourreza, A.; Alipour, V.; Arabloo, J.; Bayati, M.; Ahadinezhad, B. Health production and determinants of health systems performance in WHO Eastern Mediterranean Region. East. Mediterr. Health J. 2017, 23, 368–374. [Google Scholar] [CrossRef]
- Pross, C.; Strumann, C.; Geissler, A.; Herwartz, H.; Klein, N. Quality and resource efficiency in hospital service provision: Ageoadditive stochastic frontier analysis of stroke quality of care in Germany. PLoS ONE 2018, 13, e0203017. [Google Scholar] [CrossRef]
- Rouse, P.; Swales, R. Pricing public health care services using DEA: Methodology versus politics. Ann. Oper. Res. 2006, 145, 265–280. [Google Scholar] [CrossRef]
- See, K.F.; Md Hamzah, N.; Yu, M.M. Metafrontier efficiency analysis for hospital pharmacy services using dynamic network DEA framework. Socioecon. Plann. Sci. 2021, 78, 101044. [Google Scholar] [CrossRef]
- See, K.F.; Yen, S.H. Does happiness matter to health system efficiency? A performance analysis. Health Econ. Rev. 2018, 8, 33. [Google Scholar] [CrossRef]
- Vera, A.; Kuntz, L. Process-based organization design and hospital efficiency. Health Care Manag. Rev. 2007, 32, 55–65. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.; Asi, Y.; Raffenaud, A.; Bagwell, M.; Zeini, I. The effect of information technology on hospital performance. Health Care Manag. Sci. 2016, 19, 338–346. [Google Scholar] [CrossRef] [PubMed]
- Wilson, A.B.; Kerr, B.J.; Bastian, N.D.; Fulton, L.V. Financial performance monitoring of the technical efficiency of critical access hospitals: A data envelopment analysis and logistic regression modeling approach. J. Healthc. Manag. 2012, 57, 200–213. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-H.; Chang, C.-C.; Chen, P.-C.; Kuo, K.-N. Efficiency and productivity change in Taiwan’s hospitals: A non-radialquality-adjusted measurement. Cent. Eur. J. Oper. Res. 2013, 21, 431–453. [Google Scholar] [CrossRef]
- Babalola, T.K.; Moodley, I. Technical efficiency and productivity of public district hospitals in KwaZulu-Natal province, South Africa. J. Public Health Res. 2020, 9, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Cabinova, V.; Fedorcikova, R.; Jurova, N. Innovative methods of evaluating business efficiency: A comparative study. Mark. Manag. Innov. 2021, 5, 133–145. [Google Scholar] [CrossRef]
- Chang, L.; Lan, Y.-W. Has the National Health Insurance Scheme improved hospital efficiency in Taiwan? Identifying factors that affects its efficiency. Afr. J. Bus. Manag. 2010, 4, 3752–3760. [Google Scholar]
- Cinaroglu, S. Efficiency in health services based on professionals consensus quality indicators. Int. J. Healthc. Manag. 2021, 14, 993–1001. [Google Scholar] [CrossRef]
- Danilov, A.V. Scenarios for restructuring the regional inpatient healthcare system based on efficiency indicators and specialization indices. Int. J. Healthc. Manag. 2021, 1–8. [Google Scholar] [CrossRef]
- Du, N.; Wu, P.; Yuan, M.; Li, Z. Performance evaluation of combining with medical and old-age care in pension institutions of china: A two-stage data envelopment analysis. Risk Manag. Healthc. Policy 2021, 14, 4211–4222. [Google Scholar] [CrossRef] [PubMed]
- Falavigna, G.; Ippoliti, R.; Manello, A. Hospital organization and performance: A directional distance function approach. Health Care Manag. Sci. 2013, 16, 139–151. [Google Scholar] [CrossRef] [PubMed]
- Gong, G.; Chen, Y.; Gao, H.; Su, D.; Chang, J. Has the efficiency of China’s healthcare system improved after healthcare reform? A network data envelopment analysis and tobit regression approach. Int. J. Environ. Res. Public Health 2019, 16, 4847. [Google Scholar] [CrossRef] [PubMed]
- Helton, J.R.; Langabeer, J.R. Longitudinal changes in the operating efficiency of public safety-net hospitals. J. Healthc. Manag. 2012, 57, 214–226. [Google Scholar] [CrossRef]
- Kang, H.J.; Bastian, N.D.; Riordan, J.P. Evaluating the Relationship between Productivity and Quality in Emergency Departments. J. Healthc. Eng. 2017, 2017, 9626918. [Google Scholar] [CrossRef]
- Keshtkar, L.; Rashwan, W.; Abo-Hamad, W.; Arisha, A. A hybrid system dynamics, discrete event simulation and data envelopment analysis to investigate boarding patients in acute hospitals. Oper. Res. Health Care 2020, 26, 100266. [Google Scholar] [CrossRef]
- Kholghabad, H.F.; Alisoltani, N.; Nazari-Shirkouhi, S.; Azadeh, M.; Moosakhani, S. A Unique Mathematical Framework for Optimizing Patient Satisfaction in Emergency Departments. Iran. J. Manag. Stud. 2019, 12, 81–105. [Google Scholar] [CrossRef]
- Lai, M.-C.; Huang, H.-C.; Wang, W.-K. Designing a knowledge-based system for benchmarking: A DEA approach. Knowl.-Based Syst. 2011, 24, 662–671. [Google Scholar] [CrossRef]
- Leung, R.C.; Pasupathy, K.S. The economics of social computing: Some preliminary findings on healthcare organizations. J. Comput. Sci. 2011, 2, 253–261. [Google Scholar] [CrossRef]
- Manavgat, G.; Demirci, A. Decentralization Matter of Healthcare and Effect on Regional HealthcareEfficiency: Evidence from Turkey. Sosyoekonomi 2020, 28, 261–282. [Google Scholar] [CrossRef]
- Mousa, W.; Aldehayyat, J.S. Regional efficiency of healthcare services in Saudi Arabia. Middle East Dev. J. 2018, 10, 152–174. [Google Scholar] [CrossRef]
- Ngobeni, V.; Breitenbach, M.C.; Aye, G.C. Technical efficiency of provincial public healthcare in South Africa. Cost Eff. Resour. Alloc. 2020, 18, 3. [Google Scholar] [CrossRef] [PubMed]
- Novignon, J.; Nonvignon, J. Improving primary health care facility performance in Ghana: Efficiency analysis and fiscal space implications. BMC Health Serv. Res. 2017, 17, 399. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, L.; Dexter, F. Tactical increases in operating room block time based on financial data and market growth estimates from data envelopment analysis. Anesth. Analg. 2007, 104, 355–368. [Google Scholar] [CrossRef][Green Version]
- Peixoto, M.G.M.; Musetti, M.A.; de Mendonca, M.C.A. Performance management in hospital organizations from the perspective of Principal Component Analysis and Data Envelopment Analysis: The case of Federal University Hospitals in Brazil. Comput. Ind. Eng. 2020, 150, 106873. [Google Scholar] [CrossRef]
- Peng, Z.; Zhu, L.; Wan, G.; Coyte, P.C. Can integrated care improve the efficiency of hospitals? Research based on 200 Hospitals in China. Cost Eff. Resour. Alloc. 2021, 19, 61. [Google Scholar] [CrossRef]
- Schneider, A.M.; Oppel, E.M.; Schreyogg, J. Investigating the link between medical urgency and hospital efficiency—Insights from the German hospital market. Health Care Manag. Sci. 2020, 23, 649–660. [Google Scholar] [CrossRef]
- Sultan, W.I.M.; Crispim, J. Are public hospitals reforming efficiently in West Bank? Confl. Health 2018, 12, 44. [Google Scholar] [CrossRef]
- Su, S.; Lai, M.C.; Huang, H.C. Healthcare industry value creation and productivity measurement in an emerging economy. Serv. Ind. J. 2009, 29, 963–975. [Google Scholar] [CrossRef]
- Thai, K.Q.; Noguchi, M. Evaluating efficiency of English acute foundation trusts under system reform: A two-stage DEA approach. Health Serv. Outcomes Res. Methodol. 2019, 19, 215–240. [Google Scholar] [CrossRef]
- van Eck, N.J.; Waltman, L.; Dekker, R.; van den Berg, J. A comparison of two techniques for bibliometric mapping: Multidimensional scaling and VOS. J. Am. Soc. Inf. Sci. Technol. 2010, 61, 2405–2416. [Google Scholar] [CrossRef]
- Xu, Y.; Park, Y.S.; Park, J.D. Measuring the Response Performance of U.S. States against COVID-19 Using an Integrated DEA, CART, and Logistic Regression Approach. Healthcare 2021, 9, 268. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Liu, Z.; Zhang, T.; Hatab, A.A.; Lan, J. Measuring productivity of healthcare services under environmental constraints: Evidence from China. BMC Health Serv. Res. 2020, 20, 673. [Google Scholar] [CrossRef]
- Daraio, C.; Kerstens, K.; Nepomuceno, T.; Sickles, R.C. Empirical surveys of frontier applications: A meta-review. Int. Trans. Oper. Res. 2020, 27, 709–738. [Google Scholar] [CrossRef]
- Guo, B.J.; Zhang, J.H.; Fu, X.M. Evaluation of Unified Healthcare Efficiency in China: A Meta-Frontier Non-radial Directional Distance Function Analysis During 2009–2019. Front. Public Health 2022, 10, 876449. [Google Scholar] [CrossRef]
- Bashir, S.; Nasir, M.; Grasic, K.; Moulin, M.; Ali, S. Association between efficiency and quality of care of public healthcare facilities: Evidence from Pakistan. Int. J. Health Plann. Manag. 2022. [Google Scholar] [CrossRef]
- Cinaroglu, S. Exploring the nexus of equality and efficiency in healthcare. Int. J. Product. Perform. Manag. 2022. [Google Scholar] [CrossRef]
- Al-Hanawi, M.K.; Makuta, I.F. Changes in productivity in healthcare services in the Kingdom of Saudi Arabia. Cost Eff. Resour. Alloc. 2022, 20, 3. [Google Scholar] [CrossRef]
- Shafie, A.A.; Mohammed, N.S.; See, K.F.; Ibrahim, H.M.; Wong, J.H.Y.; Chhabra, I.K. Efficiency and management factors: Finding the balance in Thalassaemia care centres. Health Econ. Rev. 2022, 12, 9. [Google Scholar] [CrossRef]
- Nayer, M.Y.; Fazaeli, A.A.; Hamidi, Y. Hospital efficiency measurement in the west of Iran: Data envelopment analysis and econometric approach. Cost Eff. Resour. Alloc. 2022, 20, 5. [Google Scholar] [CrossRef]
- Mirmozaffari, M.; Yazdani, R.; Shadkam, E.; Khalili, S.M.; Tavassoli, L.S.; Boskabadi, A. A Novel Hybrid Parametric and Non-Parametric Optimisation Model for Average Technical Efficiency Assessment in Public Hospitals during and Post-COVID-19 Pandemic. Bioengineering 2022, 9, 7. [Google Scholar] [CrossRef] [PubMed]
- Chiu, C.M.; Chen, M.S.; Lin, C.S.; Lin, W.Y.; Lang, H.C. Evaluating the comparative efficiency of medical centers in Taiwan: A dynamic data envelopment analysis application. BMC Health Serv. Res. 2022, 22, 435. [Google Scholar] [CrossRef] [PubMed]
- Mohamadi, E.; Kiani, M.M.; Olyaeemanesh, A.; Takian, A.; Majdzadeh, R.; Lotfi, F.H.; Sharafi, H.; Sajadi, H.S.; Goodarzi, Z.; Hekmat, S.N. Two-Step Estimation of the Impact of Contextual Variables on Technical Efficiency of Hospitals: The Case Study of Public Hospitals in Iran. Front. Public Health 2022, 9, 785489. [Google Scholar] [CrossRef]
- Lin, C.S.; Chiu, C.M.; Huang, Y.C.; Lang, H.C.; Chen, M.S. Evaluating the Operational Efficiency and Quality of Tertiary Hospitals in Taiwan: The Application of the EBITDA Indicator to the DEA Method and TOBIT Regression. Healthcare 2022, 10, 58. [Google Scholar] [CrossRef] [PubMed]
- Bai, Q.; Man, X.W.; Hong, B.L.; Li, B.; Shi, X.F.; Bian, Y. Do China rural traditional Chinese medicine hospitals provide efficient healthcare to the people? Empirical study from 2013 to 2018 using data envelopment analysis. PLoS ONE 2022, 17, e0267490. [Google Scholar] [CrossRef] [PubMed]
- Hajiagha, S.H.R.; Mahdiraji, H.A.; Hashemi, S.S.; Garza-Reyes, J.A.; Joshi, R. Public Hospitals Performance Measurement through a Three-Staged Data Envelopment Analysis Approach: Evidence from an Emerging Economy. Cybern. Syst. 2022, 1–26. [Google Scholar] [CrossRef]
- Onder, O.; Cook, W.; Kristal, M. Does quality help the financial viability of hospitals? A data envelopment analysis approach. Socioecon. Plann. Sci. 2022, 79, 101105. [Google Scholar] [CrossRef]
- Klumpp, M.; Loske, D.; Bicciato, S. COVID-19 health policy evaluation: Integrating health and economic perspectives with a data envelopment analysis approach. Eur. J. Health Econ. 2022. [Google Scholar] [CrossRef]
- Peykani, P.; Memar-Masjed, E.; Arabjazi, N.; Mirmozaffari, M. Dynamic Performance Assessment of Hospitals by Applying Credibility-Based Fuzzy Window Data Envelopment Analysis. Healthcare 2022, 10, 876. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).