Calcification of the Atlanto-Occipital Ligament (Ponticulus Posticus) in Orthodontic Patients: A Retrospective Study
Abstract
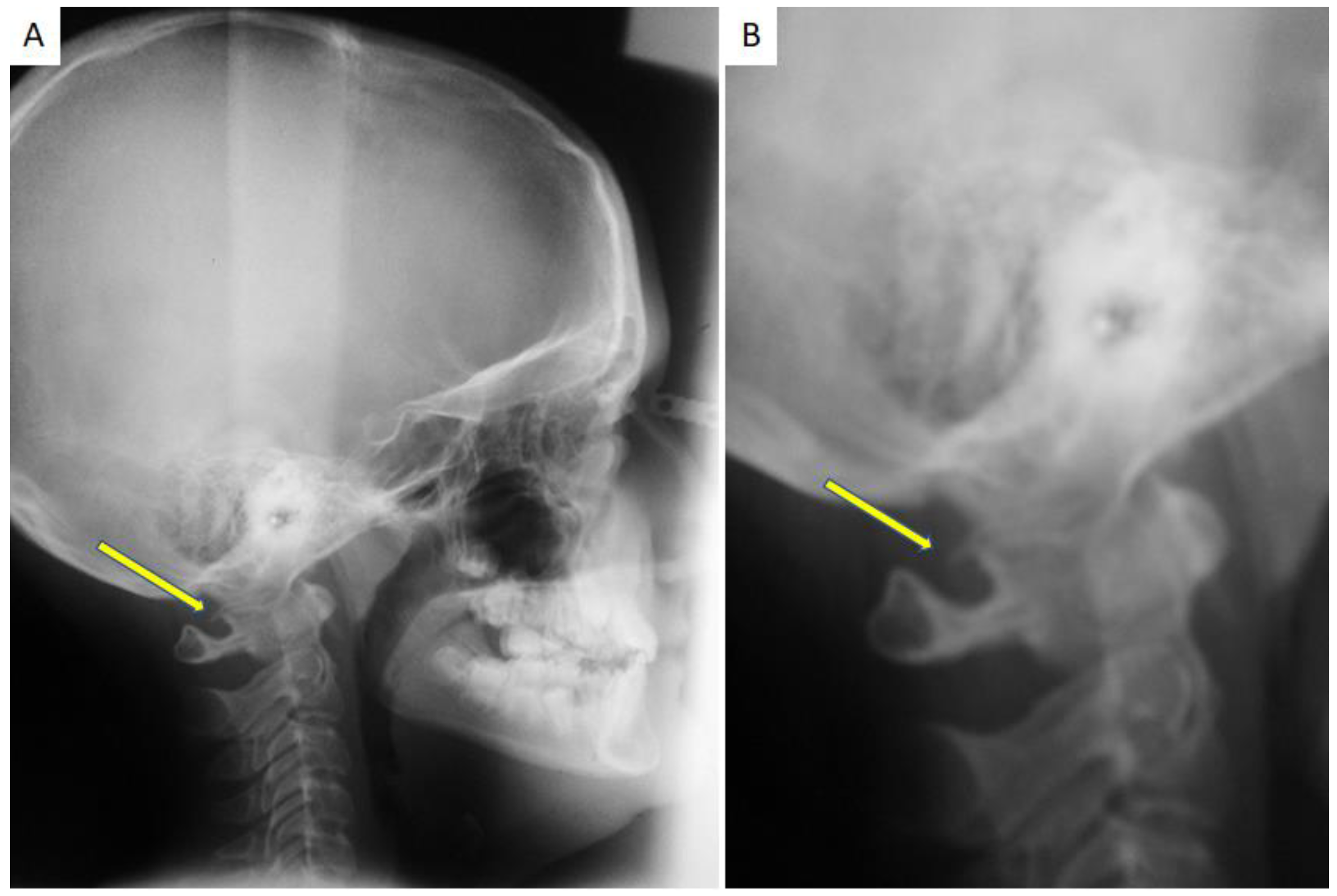
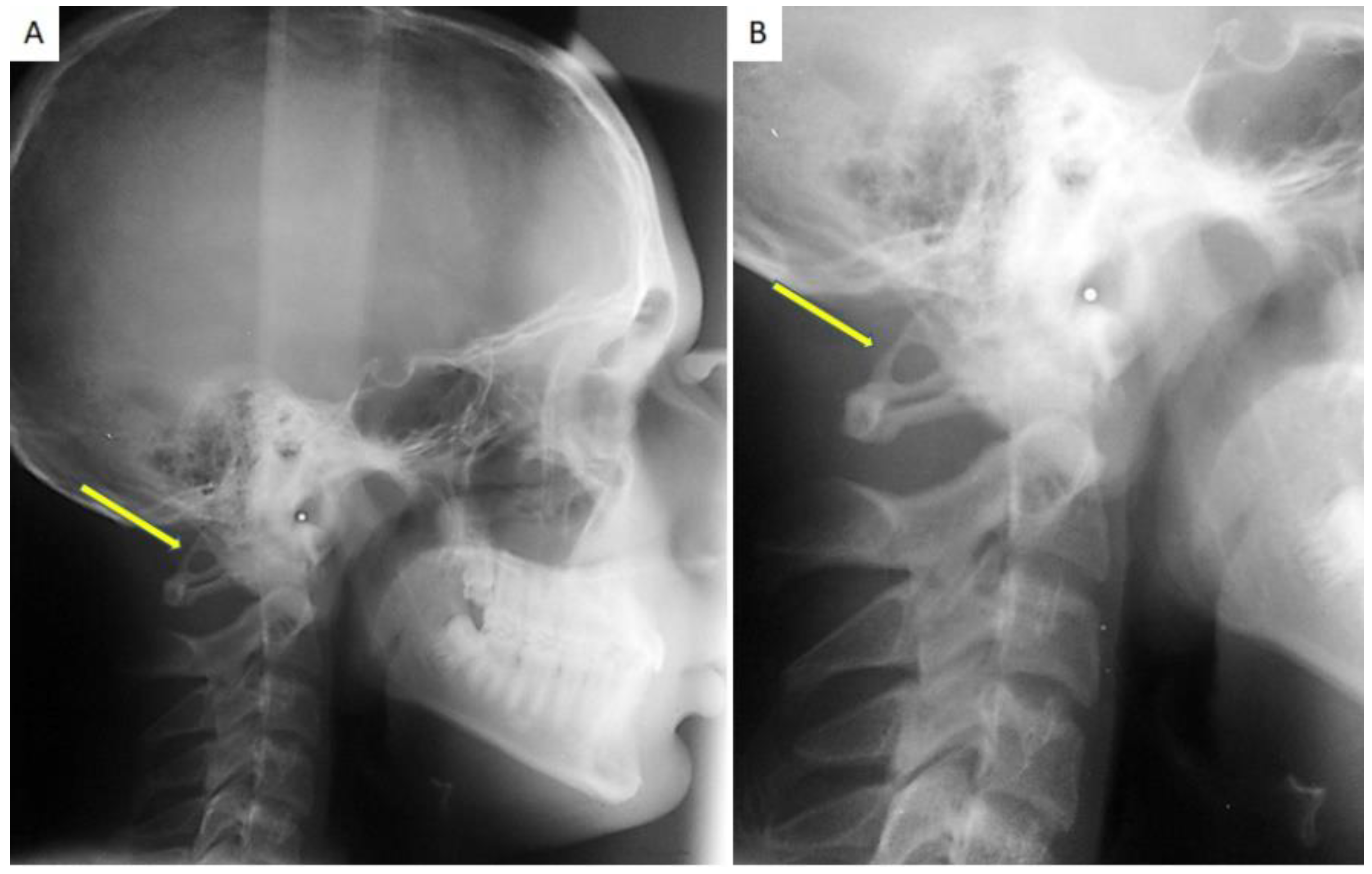
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rajani, S. Is Variant Anatomy of Atlas Clinically Important? A Review. Basic Sci. Med. 2014, 7, 1–7. [Google Scholar]
- Hasan, M.; Shukla, S.; Shakil Siddiqui, M.; Singh, D. Posterolateral Tunnels and Ponticuli in Human Atlas Vertebrae. J. Anat. 2001, 199, 339–343. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.; Duran, M.; Syldort, S.; Rizvi, A.; D’Antoni, A.V.; Johal, J.; Iwanaga, J.; Oskouian, R.J.; Tubbs, R.S. Arcuate Foramen: Anatomy, Embryology, Nomenclature, Pathology, and Surgical Considerations. World Neurosurg. 2018, 118, 197–202. [Google Scholar] [CrossRef]
- Di Venere, D.; Laforgia, A.; Lorusso, P.; Capodiferro, S.; Corsalini, M. Ectopic Eruption of the First Permanent Molar in the Maxilla: Cephalometric Features of 13 Pediatric Patients. Appl. Sci. 2021, 11, 7869. [Google Scholar] [CrossRef]
- Sharma, V.; Chaudhary, D.; Mitra, R. Prevalence of Ponticulus Posticus in Indian Orthodontic Patients. Dentomaxillofac. Radiol. 2010, 39, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Rapone, B.; Palmisano, C.; Ferrara, E.; Di Venere, D.; Albanese, G.; Corsalini, M. The Accuracy of Three Intraoral Scanners in the Oral Environment with and without Saliva: A Comparative Study. Appl. Sci. 2020, 10, 7762. [Google Scholar] [CrossRef]
- Selby, S.; Garn, S.M.; Kanareff, V. The Incidence and Familial Nature of a Bony Bridge on the First Cervical Vertebra. Am. J. Phys. Anthropol. 1955, 13, 129–141. [Google Scholar] [CrossRef]
- Dinesh, K.; Amol, A.; Nilanjan, R.; Purushottam, R.M.; Vaishaly, B. A Study of Foramen of Arcuale in Atlas Vertebra: Incidence and Clinical Correlations. Int. J. Contemp. Res. Rev. 2015, 7, 9–11. [Google Scholar]
- Lo Giudice, A.; Caccianiga, G.; Crimi, S.; Cavallini, C.; Leonardi, R. Frequency and Type of Ponticulus Posticus in a Longitudinal Sample of Non orthodontically Treated Patients: Relationship with Gender, Age, Skeletal Maturity, and Skeletal Malocclusion. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 126, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Gibelli, D.; Cappella, A.; Cerutti, E.; Spagnoli, L.; Dolci, C.; Sforza, C. Prevalence of Ponticulus Posticus in a Northern Italian Orthodontic Population: A Lateral Cephalometric Study. Surg. Radiol. Anat. 2016, 38, 309–312. [Google Scholar] [CrossRef]
- Koutsouraki, E.; Avdelidi, E.; Michmizos, D.; Kapsali, S.-E.; Costa, V.; Baloyannis, S. Kimmerle’s Anomaly as a Possible Causative Factor of Chronic Tension-Type Headaches and Neurosensory Hearing Loss: Case Report and Literature Review. Int. J. Neurosci. 2010, 120, 236–239. [Google Scholar] [CrossRef]
- Adisen, M.Z.; Misirlioglu, M. Prevalence of Ponticulus Posticus among Patients with Different Dental Malocclusions by Digital Lateral Cephalogram: A Comparative Study. Surg. Radiol. Anat. 2017, 39, 293–297. [Google Scholar] [CrossRef] [PubMed]
- Haji Ghadimi, M.; Amini, F.; Hamedi, S.; Rakhshan, V. Associations among Sella Turcica Bridging, Atlas Arcuate Foramen (Ponticulus Posticus) Development, Atlas Posterior Arch Deficiency, and the Occurrence of Palatally Displaced Canine Impaction. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Tassoker, M.; Kok, H.; Ozcan, S. Investigation of the Relationship between “Sella Turcica Bridge” and “Ponticulus Posticus”: A Lateral Cephalometric Study. Int. J. Morphol. 2017, 35, 337–344. [Google Scholar] [CrossRef]
- Sekerci, A.E.; Soylu, E.; Arikan, M.P.; Aglarci, O.S. Is There a Relationship between the Presence of Ponticulus Posticus and Elongated Styloid Process? Clin. Imaging 2015, 39, 220–224. [Google Scholar] [CrossRef]
- Shahidi, S.; Hasani, M.; Khozaei, M. Evaluating the Relation between the Elongated Styloid Process and the Ponticulus Posticus Using Cone Beam Computed Tomography. Folia Morphol. 2021, 81, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Putrino, A.; Leonardi, R.M.; Barbato, E.; Galluccio, G. The Association between Ponticulus Posticus and Dental Agenesis: A Retrospective Study. Open Dent. J. 2018, 12, 510–519. [Google Scholar] [CrossRef] [PubMed]
- Di Venere, D. Early Mandibular Canine-Lateral Incisor Transposition: Case Report. Oral Implantol. 2017, 10, 181. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, R.; Barbato, E.; Vichi, M.; Caltabiano, M. Skeletal Anomalies and Normal Variants in Patients with Palatally Displaced Canines. Angle Orthod. 2009, 79, 727–732. [Google Scholar] [CrossRef]
- Perez, I.; Chavez, A. Frequency of Ponticulus Posticus, Sella Turcica Bridge and Clinoid Enlargement in Cleft Lip and Palate Peruvian Patients: A Comparative Study with Non-Cleft Patients. Int. J. Morphol. 2015, 33, 895–901. [Google Scholar] [CrossRef][Green Version]
- Leonardi, R.; Santarelli, A.; Barbato, E.; Ciavarella, D.; Bolouri, S.; Härle, F.; Palazzo, G.; Muzio, L.L. Atlanto-Occipital Ligament Calcification: A Novel Sign in Nevoid Basal Cell Carcinoma Syndrome. Anticancer Res. 2010, 30, 4265–4267. [Google Scholar]
- Friedrich, R.E. Ponticulus Posticus Is a Frequent Radiographic Finding on Lateral Cephalograms in Nevoid Basal Cell Carcinoma Syndrome (Gorlin–Goltz Syndrome). Anticancer Res. 2014, 34, 7395–7399. [Google Scholar]
- Baccetti, T.; Franchi, L.; McNamara, J.A. An Improved Version of the Cervical Vertebral Maturation (CVM) Method for the Assessment of Mandibular Growth. Angle Orthod. 2002, 72, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Bayrakdar, İ.Ş.; Miloğlu, Ö.; Yeşiltepe, S.; Yılmaz, A.B. Ponticulus Posticus in a Cohort of Orthodontic Children and Adolescent Patients with Different Sagittal Skeletal Anomalies: A Comparative Cone Beam Computed Tomography Investigation. Folia Morphol. 2018, 77, 7. [Google Scholar] [CrossRef] [PubMed]
- Arntsen, T.; Sonnesen, L. Cervical Vertebral Column Morphology Related to Craniofacial Morphology and Head Posture in Preorthodontic Children with Class II Malocclusion and Horizontal Maxillary Overjet. Am. J. Orthod. Dentofac. Orthop. 2011, 140, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Corsalini, M.; Capodiferro, S.; dell’Olio, F.; Albanese, G.; Quaranta, N.; Solarino, B.; Catapano, S.; Di Venere, D. Cranio-Mandibular Disorders after Whiplash Injury: A Mono-Institutional Clinical Study on 31 Patients. Int. J. Environ. Res. Public. Health 2022, 19, 901. [Google Scholar] [CrossRef] [PubMed]
- Tambawala, S.S.; Karjodkar, F.R.; Sansare, K.; Motghare, D.; Mishra, I.; Gaikwad, S.; Dora, A.C. Prevalence of Ponticulus Posticus on Lateral Cephalometric Radiographs, Its Association with Cervicogenic Headache and a Review of Literature. World Neurosurg. 2017, 103, 566–575. [Google Scholar] [CrossRef] [PubMed]
| Male | Female | Total | |
|---|---|---|---|
| Patients | 67 (45%) | 83 (55%) | 150 |
| Age | 12.8 | 11.6 | 10.3 (±2.7) |
| PP | 4 (2.7%) | 8 (5.3%) | 12 (8%) |
| Dental Agenesis | 1 (0.7%) | 2 (1.3%) | 3 (2%) |
| Impacted canine | 7 (4.7%) | 9 (6%) | 16 (10.7%) |
| Type of PP | ||||
|---|---|---|---|---|
| Absence of PP | Partial PP | Complete PP | Total | |
| Male | 63 | 1 | 3 | 67 |
| Female | 75 | 4 | 4 | 83 |
| Total | 138 | 5 | 7 | 150 |
| χ2: 1.2944; p-value: 0.5235 | ||||
| Type of PP | ||||
|---|---|---|---|---|
| Absence of PP | Partial | Complete | Total | |
| From 4 to 11 years | 78 | 3 | 4 | 85 |
| From 12 to 18 years | 60 | 2 | 3 | 65 |
| 138 | 5 | 7 | 150 | |
| χ2: 0.0245; p-value: 0.987849 | ||||
| With PP | Without PP | Total | |
|---|---|---|---|
| Patients with dental agenesis | 1 | 2 | 3 |
| Patients without dental agenesis | 11 | 136 | 147 |
| Total | 12 | 138 | 150 |
| χ2 with Yates correction: 0.3124; p-value: 0.5762 | |||
| With PP | Without PP | Total | |
|---|---|---|---|
| Patients with palatally impacted canines | 3 | 13 | 16 |
| Patients without palatally impacted canines | 9 | 125 | 134 |
| Total | 12 | 138 | 150 |
| χ2 with Yates’s correction: 1.4148; p-value: 0.2342 | |||
| Type of PP | ||||
|---|---|---|---|---|
| Absence | Partial | Complete | Total | |
| Class I | 41 | 3 | 3 | 47 |
| Class II | 53 | 1 | 3 | 57 |
| Class III | 44 | 1 | 1 | 46 |
| Total | 138 | 5 | 7 | 150 |
| χ2: 3.0645; p-value: 0.547086 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Venere, D.; Laforgia, A.; Azzollini, D.; Barile, G.; De Giacomo, A.; Inchingolo, A.D.; Rapone, B.; Capodiferro, S.; Kazakova, R.; Corsalini, M. Calcification of the Atlanto-Occipital Ligament (Ponticulus Posticus) in Orthodontic Patients: A Retrospective Study. Healthcare 2022, 10, 1234. https://doi.org/10.3390/healthcare10071234
Di Venere D, Laforgia A, Azzollini D, Barile G, De Giacomo A, Inchingolo AD, Rapone B, Capodiferro S, Kazakova R, Corsalini M. Calcification of the Atlanto-Occipital Ligament (Ponticulus Posticus) in Orthodontic Patients: A Retrospective Study. Healthcare. 2022; 10(7):1234. https://doi.org/10.3390/healthcare10071234
Chicago/Turabian StyleDi Venere, Daniela, Alessandra Laforgia, Daniela Azzollini, Giuseppe Barile, Andrea De Giacomo, Alessio Danilo Inchingolo, Biagio Rapone, Saverio Capodiferro, Rada Kazakova, and Massimo Corsalini. 2022. "Calcification of the Atlanto-Occipital Ligament (Ponticulus Posticus) in Orthodontic Patients: A Retrospective Study" Healthcare 10, no. 7: 1234. https://doi.org/10.3390/healthcare10071234
APA StyleDi Venere, D., Laforgia, A., Azzollini, D., Barile, G., De Giacomo, A., Inchingolo, A. D., Rapone, B., Capodiferro, S., Kazakova, R., & Corsalini, M. (2022). Calcification of the Atlanto-Occipital Ligament (Ponticulus Posticus) in Orthodontic Patients: A Retrospective Study. Healthcare, 10(7), 1234. https://doi.org/10.3390/healthcare10071234











