1. Introduction
Pain is a multidimensional and personal experience, and its assessment is key to optimal pain management [
1]. It can cause pathophysiological changes, which can affect the patient’s level of consciousness, sleep, circulatory system, endocrine system, metabolism and/or gastrointestinal system, as well as psychological disorders [
2,
3,
4,
5]. Furthermore, as a major consequence, acute pain may evolve to chronic pain and can lead to various negative psychological outcomes [
6].
The patient’s self-report should be obtained whenever possible, as it is the gold standard measure of pain. However, critically ill patients may be incapable of self-report due to mechanical ventilation and sedation [
7,
8]. Therefore, assessing pain in this population is a challenge for the intensive care unit (ICU) care team. In non-communicative patients, such as those who are mechanically ventilated (MV) and sedated, behavioural assessment tools (such as the Behavioural Pain Scal—BPS, and the Critical-Care Pain Observation Tool—CPOT) are alternative measures that can be used by the ICU care team to guide pain control interventions [
1,
2,
7,
8].
Considering their continuous presence at the bedside and their close proximity to the patient and his/her family, nurses play a key role in the assessment and management of pain [
4]. Nurses can perform adequate pain assessment using validated tools, and regular pain monitoring is indispensable for optimal pain management. Indeed, the implementation of pain assessment tools has improved care outcomes, for example, by shortening the mechanical ventilation duration and ICU length of stay, reducing nosocomial infection rates and decreasing the number of long-term complications [
6].
Studies have shown that the Behavioural Pain Scale (BPS) [
9] and the Critical-Care Pain Observation Tool (CPOT) [
10] are the most suitable alternative measures for pain assessment in critically ill patients unable to self-report.
However, in some studies, BPS scores increased during both painful and a nonpainful procedures, whereas CPOT scores only increased during a painful procedure [
11,
12]. Therefore, the CPOT was identified as the tool of choice for the assessment of pain in patients in the ICU with altered levels of consciousness [
5,
11,
13]. The original BPS can only be used for mechanically ventilated patients, while for pain assessment in non-intubated patients, the BPS-non-intubated (NI) is the alternative option, and it is not yet available in Portuguese [
14].
So far, the BPS has been the only validated pain scale in the Portuguese population and was selected by the Portuguese Society of Intensive Care [
14]. Nevertheless, the Society of Critical Care Medicine suggests both the BPS/BPS-NI and the CPOT scales in their practice guidelines [
4]. Therefore, their translation and validation are fundamental [
15,
16] to provide valid pain assessment tools in critically ill Portuguese patients.
This study aimed to translate the CPOT into Portuguese and validate the translated version. Our specific objectives were to determine the CPOT discriminative validity, criterion validity and convergent validity as well as the inter-examiner reliability of the Portuguese version.
2. Materials and Methods
2.1. Design
A prospective observational cohort study was conducted, reported according to the STROBE statement for observational studies [
17].
2.2. Setting and Sample
We used a consecutive sample of 110 medical and surgical patients who were admitted to a 11-bed intensive care unit (ICU), at a University Hospital located in Lisbon (Portugal). For this study, we defined the inclusion criteria described below: (a) were admitted to the ICU; (b) had a minimum length of stay in the ICU of 24 h; (c) were 18 years old or older; (d) were mechanically ventilated; and (e) were able to understand Portuguese before intubation. Patients with neurological deficits (such as reduced range of movement, decreased strength and functionality, altered sensitivity) were excluded.
2.3. Data Collection Tools and Methods
In the initial stage of the study, following a written authorisation by the author of the CPOT (CG) and after obtaining permission to use the English version of the CPOT, the tool was translated into Portuguese. International guidelines relevant to the cross-cultural adaptation process were followed to ensure linguistic equivalence, conceptual equivalence and psychometric equivalence [
18,
19].
The process included the following steps: preparation, forward-translation, reconciliation, back-translation, back-translation review, expert panel and pilot testing.
The translation from English to Portuguese was carried out by two professional translators. After the translations were analysed and the consensus version was obtained, two professional English translators performed the back-translation. Following the results for the back-translation, all versions were harmonised to detect and address any discrepancies that might arise between different language versions, ensuring conceptual equivalence.
Content and face validity were submitted to a Delphi panel consisting of eight nurses (with a master’s degree and experience working in the ICU) and two PhD experts in scale validation. Each of the Delphi panel members gave their opinion on the adequacy of the translation and the relevance of the item. The level of agreement for each item was 100%. The Portuguese translation was pilot tested by three ICU nurses on 15 patients to check the interpretation and ease of comprehension. No changes were necessary.
Following the completion of the transcultural adaptation process, we appraised the CPOT’s psychometric characteristics. The patients were assessed with the CPOT and the BPS (the BPS was used for convergent validity) at rest pre-procedure, during a nociceptive procedure (NP) and 20 min after the procedure (t2), for a total of three assessments of each patient. The NP included one of the following standard care procedures commonly used in previous validation studies: turning/positioning and endotracheal or tracheal suctioning [
20,
21,
22,
23,
24]. Pain assessments were performed simultaneously and independently by two trained ICU nurses during the daytime.
The raters (ICU nurses) received a 90-min standardised training session (theoretical and practical) from the primary investigator, during which they were taught how to use the CPOT and practiced its administration, inspired by the one developed by the authors of the CPOT [
11,
24]. Following training, they completed bedside assessments with the CPOT in the presence of the study investigator to ensure that the tool was used appropriately.
The CPOT and the BPS were used for all participants. In several studies, authors reported a correlation coefficient between the scores of two scales (e.g., BPS and CPOT) and described this strategy as convergent or criterion validation [
20].
Whenever the BPS score exceeded 5, pain was considered to be present. The inter-rater reliability of nurses’ CPOT scores was described at each time point. Comparison of CPOT scores at rest pre- and post-procedure with the NP allowed the examination of discriminative validity. Criterion validity was established using the BPS threshold for the absence (BPS ≤ 5) versus the presence (BPS > 5) of pain to examine their association with CPOT scores. The association between the two scales (BPS and CPOT) was commonly performed as a validation strategy in previous studies [
20]. Finally, associations between vital signs (i.e., heart rate [HR], mean arterial pressure [MAP] and respiratory rate [RR]) extracted from the bedside monitors, as well as CPOT scores, were described at each time point for the examination of convergent validity.
2.4. Instruments
Critical-Care Pain Observation Tool: The CPOT was initially developed in French Canadian by Gélinas and colleagues in 2006 based on a thorough content validation process and was translated into English using a forward–backward method [
20]. The CPOT is divided into four sections, each pertaining to different behavioural categories: facial expression, body movements, muscle tension and compliance with the ventilator (only for mechanically ventilated patients) or vocalisation (only for non-intubated patients). Each section is scored from 0 to 2, and the possible total score ranges from 0 to 8 [
10]. The CPOT is available in at least 19 languages and has been tested in almost 4000 ICU patients [
20]. The initial validation testing was achieved using a convenience sample of 105 patients. All participants were evaluated when mechanically ventilated (64 unconscious and 51 conscious), as well as post-extubation. The validation findings supported inter-rater reliability, discriminative validity between nociceptive and non-nociceptive procedures, criterion validity with positive associations between CPOT scores and self-reported pain scores [
10]. It was found to be feasible and clinically relevant by ICU nurses [
20].
The raters completed a 90-min standardised training session, inspired by the one developed by the author of the CPOT, during which they were taught how to use the CPOT and practiced scoring using the tool in the presence of the primary investigator [
11,
24]. Following training, they completed bedside assessments using the CPOT in the presence of the study investigator to ensure that the tool was used appropriately.
Behavioural Pain Scale: The BPS was initially developed in French from France by Payen and colleagues in 2001 and includes four behavioural indicators: facial expression, upper limb movements and compliance with mechanical ventilation. Each item is scored from 1 to 4, and the possible total score ranges from 3 to 12 [
9]. Its initial validation testing in a sample of 30 mechanically ventilated ICU patients (269 observations) showed good inter-rater reliability and discriminative validity between nociceptive and non-nociceptive procedures. The Brazilian version of the BPS showed good agreement between raters (intraclass correlation coefficient (ICC) = 0.80 and 0.97) and good criterion validity with self-reported pain scores. Discriminative validity led to variable findings across studies, including significant increases during both nociceptive and non-nociceptive procedures [
25].
Socio-demographic and clinical information: Sociodemographic (sex and age) and clinical data (medical or surgical diagnosis, Glasgow Coma Scale (GCS), presence of continuous and/or intermittent sedation and analgesia), as well as vital signs (MAP, HR and RR) available through continuous monitoring in the ICU, were also collected.
The GCS is used to assess the patient’s level of consciousness, which includes three sections: eye opening (scored from 1 to 4), verbal response (scored from 1 to 5) and motor response (scored from 1 to 6). The probable score ranges from 3 (unconscious, the worst response) to 15 (fully conscious and oriented, the best response). Patients were classified as unconscious with GCS ≤ 8 and conscious with GCS > 9.
2.5. Data Analysis
Data were analysed using SPSS version 21 for Windows (IBM Corp., Armonk, NY, USA). Descriptive data analysis was performed using frequencies, percentages, mean ± standard deviation (SD) and ranges. Data normality was analysed through the Shapiro–Wilk test. Several non-parametric tests were used to assess validity, and the alpha was set at 0.05. The Wilcoxon Signed-Rank test (Z) was performed to evaluate the differences in CPOT scores at all time points (discriminative validity). The Mann–Whitney test was performed to compare CPOT scores using the BPS threshold for the absence versus the presence of pain as the reference standard, and receiver operating characteristic (ROC) curve analyses were also performed (criterion validity). ROC analyses is a common strategy to establish the performance of a tool to detect a condition (e.g., pain) as well as the sensitivity and specificity associated with the best threshold [
20]. Spearman correlations between CPOT scores and vital signs (MAP, HR, RR) were obtained (convergent validity). Finally, inter-rater reliability between ICU nurses’ CPOT scores was estimated using weighted kappa coefficients (95% CI) at each time point. Values from 0.40 to 0.60 were considered moderate, and values above 0.60 were considered excellent [
26].
2.6. Ethical and Institutional Approvals
The study was conducted in accordance with the Declaration of Helsinki [
27], and the protocol was approved by the Ethics Committee (no: 423/16). Trained ICU nurses explained the study to eligible patients or their relatives, and informed written consent was obtained. When the patient was not able to provide his/her informed written consent, a close relative/legal representative was asked to complete the written consent form on the patient’s behalf. Personal data were processed in accordance with the EU General Data Protection Regulation (GDPR2016/679).
3. Results
Sample Description: The sample included 110 participants. A total of 38.2% of them were women, and their ages ranged from 20 to 95 (67.24 ± 14.61) years. Almost half of the participants were admitted to the ICU for a surgical diagnosis (56, 51%), 53 did not receive analgesia (48%) and 93 did not receive any sedation (85%). Patients were classified as ‘unconscious’ (63, 57%) or ‘conscious’ (47, 43%).
Validity: Discriminative validity was supported by higher median CPOT scores during NP, when compared to CPOT scores at rest pre-procedure (baseline). Within-group analysis revealed higher CPOT scores during NP compared with those obtained at rest (
p < 0.001) (
Table 1).
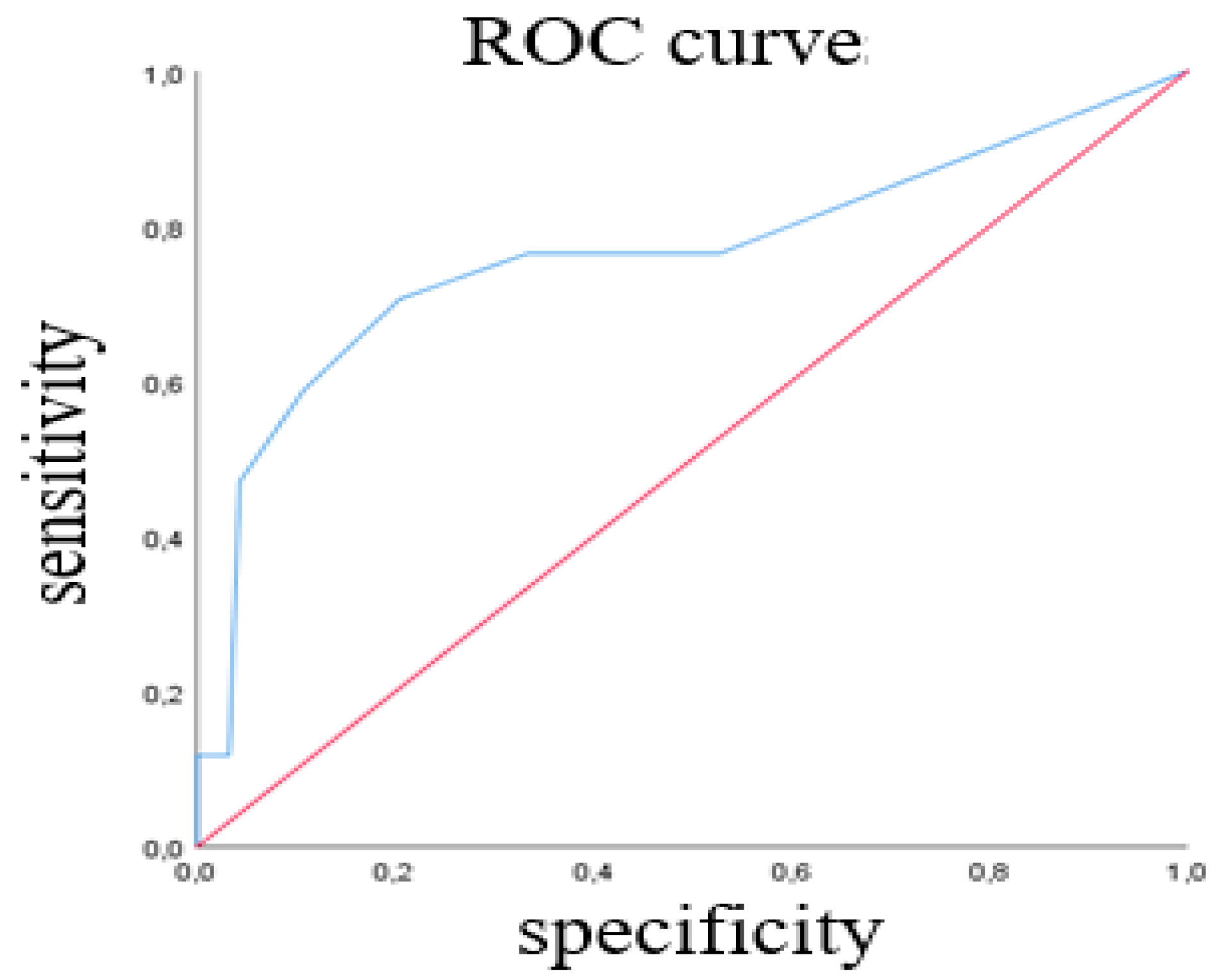
The ROC of Rater 1 CPOT scores during the nociceptive procedure for the total sample is presented in
Figure 1.
The ROC of Rater 1′s scores during NP showed good performance of the CPOT to classify patients with pain based on BPS > 5 (AUC = 0.764; SE = 0.077; 95% CI 0.613–0.915; p < 0.001) with a sensitivity of 71% and a specificity of 80%. A similar performance of the CPOT was found based on ROC analysis of Rater 2’s scores. In this sample, the optimal CPOT threshold was ≥3.
According to the convergent validity, associations between CPOT scores and vital signs were evaluated; therefore, we present below the mean and standard deviation values of the vital signs: mean arterial pressure (MAP), heart rate (HR) and respiratory rate (RR), at each time point. At rest pre-procedure: MAP = 84.50 (16.47), RR = 21.50 (6.14) and HR = 85.10 (19.45); during a nociceptive procedure: MAP = 94.14 (16.40), RR = 23.97 (6.48) and HR = 91.10 (20.53); 20 min after the procedure: MAP = 83.28 (17.34), RR = 20.68 (6.02) and HR = 85.97 (19.16).
Positive mild associations were found between CPOT scores, HR (both raters) and RR (Rater 2) (
Table 2). Very low to no associations were obtained between CPOT and MAP.
Regarding criterion validity, CPOT scores during NP were significantly associated with the presence of pain (BPS > 5) for Rater 1 and Rater 2 (
Table 3). In fact, CPOT scores were higher in patients with BPS > 5 (presence of pain) when compared to those with BPS scores ≤ 5 (absence of pain).
Inter-rater reliability: Weighted kappa coefficients between ICU nurses’ CPOT scores ranged from 0.39 to 1.00, indicating moderate to excellent inter-rater reliability.
4. Discussion
This study aimed to translate and validate the Portuguese version of the CPOT in 110 medical and surgical mechanically ventilated ICU patients, either conscious or unconscious. The level of consciousness and sedation may influence pain behaviours, which are less frequent or blurred in patients who are unconscious or heavily sedated [
20].
In this validation process, we examined the discriminative validity, criterion validity, convergent validity and inter-rater reliability of the CPOT. Through these validation strategies, we were able to determine the tool’s psychometric characteristics in this Portuguese sample.
Similar to previous studies [
3,
4,
10,
11,
13,
21,
28,
29], scores on the Portuguese version of the CPOT increased during common standard care procedures compared to rest in both conscious and unconscious groups, demonstrating discriminative validity. Criterion validity was also demonstrated, with significant associations of CPOT with the BPS threshold as the reference standard. During NP, higher CPOT scores were obtained in patients with BPS > 5 compared to those with BPS ≤ 5. ROC findings showed a moderate performance (AUC 0.6–0.8) [
28] of the CPOT to detect pain during NP with a threshold of 3, as found in previous studies [
20,
29,
30]. In our study, correlations between vital signs and CPOT scores were low to very low; therefore, they did not support convergent validity and lacked clinical relevance to pain assessment. Vital signs were not found to be good indicators for pain assessment in the ICU [
11,
26,
28,
31] when considered individually [
2,
20,
32], because they are also influenced by other factors (such as sedation, anxiety, difficulty breathing or sepsis) [
13].
Inter-rater reliability was satisfactory. Most kappa coefficients were moderate to excellent [
26]. These results demonstrated that both ICU nurses obtained consistent CPOT scores at each time point following standardised training. Similar findings were reported in previous studies [
33].
In this study, we found that the correlation between vital signs and the score obtained with the CPOT assessment were low, because when individually assessed vital signs were not relevant, they could have been influenced by other factors such as anxiety, sedation or breathing difficulties.
The Danish study [
30] confirms that pain cannot be evaluated only through physiological indicators, even when the patient is awake, without sedation due to the changes that they may be experiencing due to the patient’s clinical situation (sepsis anxiety).
Our study, as well as the Swedish [
16] and the Danish [
30], was carried out by two independent evaluators and proved that CPOT should be applied to critically ill patients who are unable to verbalise, showing good inter-rater reliability.
As in previous studies on this study, 53 patients did not receive analgesia and 93 patients did not receive sedation, which allowed for the observation of higher CPOT scores during painful procedures in comparison to non-painful procedures. However, it was not possible to verify a correlation between pain and PFM increase, which justifies the aforementioned statements.
In our study, we used another BPS behavioural assessment scale as a comparison in our pain assessment, which showed a good correlation between the two. In the Danish study [
30], the CAM-ICU scale was applied concomitantly, in which 28 patients had a positive CAM ICU, which may affect the reliability of pain self-assessment, which is considered the gold standard.
Despite this, we can say that the results obtained in the different studies were convergent, with regard to the increase in the CPOT score during painful procedures.
4.1. Limitations
Some limitations must be mentioned. Due to difficulties in reconciling the presence of three raters in all instants of assessment, we chose to use only two. This strategy had already been employed in other validation studies [
16,
30]. However, some authors suggest that, to evaluate the CPOT’s inter-rater reliability, more than two raters should be involved in the process [
11,
20].
4.2. Implications and Recommendations for Practice
The Portuguese version of the CPOT was shown to be valid in this sample of Portuguese mechanically ventilated ICU patients, who were conscious or unconscious. Portuguese ICU nurses should not rely on vital signs for pain assessment and are encouraged to use a valid behavioural scale such as the CPOT when they suspect that their patient may be in pain.
5. Conclusions
The Portuguese version of the CPOT seems to be a valid and reliable tool for pain assessment in mechanically ventilated ICU patients, whether they are conscious or unconscious. Thus, the CPOT is an alternative option to the BPS which, until now, has been the sole validated scale for pain assessment in Portuguese ICU patients. The CPOT can be applied to ICU patients who are incapable of communicating verbally or using signs, whether they are mechanically ventilated or not.
The inter-rater reliability of the CPOT was excellent at rest and fair to moderate during the nociceptive procedure. The CPOT could discriminate between conditions with higher scores during the nociceptive procedure when compared to CPOT scores at rest. The optimal CPOT cut-off score was >2 with a sensitivity of 71% and a specificity of 80% using self-reported pain as the gold standard criterion. Significant but low correlations were found between CPOT scores, the heart rate and the respiratory rate during the nociceptive procedure.
Nurses have a fundamental role to play in monitoring and managing pain. For this purpose, they must use appropriate pain assessment tools adapted to the patient’s ability to communicate their pain, such as self-report or behavioural scales. In Portugal and in addition to the BPS, the CPOT appears to be another valid alternative scale to use because it is applicable to patients unable to self-report, whether they are mechanically ventilated or not.
Author Contributions
Conceptualization: R.M., F.A. and M.F.; methodology: R.M., F.A., M.F. and M.A.D.; software, validation and formal analysis: R.M. and M.A.D.; investigation and resources: R.M., F.A., M.F. and J.F.; data curation: R.M. and M.A.D.; writing—original draft preparation: R.M., F.A., M.F. and J.F.; writing—review and editing: M.A.D. and C.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Study was conducted under all assumptions from the Helsinki Declaration and was approved by the institution and received a positive opinion from the Ethics Committee (CE-No. 423/16).
Informed Consent Statement
Since the study was conducted with ventilated, sedated and unconscious patients, informed consent was obtained through their legal representative. The objectives of the study were presented, and it was guaranteed that the data obtained were confidential, anonymous and only for the exclusive use of this work.
Data Availability Statement
All data are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bottega, F.H.; Fontana, R.T. Pain as the fifth vital sign: Use of the assessment scale by nurses in general hospital. Texto Context.-Enferm. 2010, 19, 283–290. [Google Scholar] [CrossRef]
- Nascimento, J.C.C.; Silva, L.C.S. Assessment of pain in patients under care in intensive care units: A literature review. Rev. Mov. 2014, 7, 711–720. Available online: https://www.revista.ueg.br/index.php/movimenta/article/view/6274 (accessed on 18 December 2021).
- Arbour, C.; Gélinas, C.; Michaud, C. Impact of the Implementation of the Critical-Care Pain Observation Tool (CPOT) On Pain Management and Clinical Outcomes in Mechanically Ventilated Trauma Intensive Care Unit Patients: A Pilot Study. J. Trauma Nurs. 2011, 18, 52–60. [Google Scholar] [CrossRef]
- Devlin, J.W.; Skrobik, Y.; Gélinas, C.; Needham, D.M.; Slooter, A.J.C.; Pandharipande, P.; Watson, P.L.; Weinhouse, G.L.; Nunnally, M.E.; Rochwerg, B.; et al. Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit. Care Med. 2018, 46, e825–e873. [Google Scholar] [CrossRef]
- Liu, Y.; Li, L.; Herr, K. Evaluation of Two Observational Pain Assessment Tools in Chinese Critically Ill Patients. Pain Med. 2015, 16, 1622–1628. [Google Scholar] [CrossRef]
- Al Darwish, Z.Q.; Hamdi, R.; Fallatah, S. Evaluation of Pain Assessment Tools in Patients Receiving Mechanical Ventilation. AACN Adv. Crit. Care 2016, 27, 162–172. [Google Scholar] [CrossRef]
- Bourbonnais, F.F.; Malone-Tucker, S.; Dalton-Kischel, D. Intensive care nurses assessment of pain in patients who are mecanically ventilated: How a pilot study helped to influence practice. Crit. Care Nurse 2016, 27, 24–29. Available online: https://pubmed.ncbi.nlm.nih.gov/29461721/ (accessed on 20 January 2022).
- Dunwoody, C.J.; Krenzischek, D.A.; Pasero, C.; Rathmell, J.P.; Polomano, R.C. Assessment, physiological monitoring, and consequences of inadequately treated acute pain. J. Perianesth. Nurs. 2008, 23, S15–S27. [Google Scholar] [CrossRef]
- Payen, J.F.; Bru, O.; Bosson, J.L.; Lagrasta, A.; Novel, E.; Deschaux, I.; Lavagne, P.; Jacquot, C. Assessing Pain in Critically Ill Sedated Patients by Using a Behavioral Pain Scale. Crit. Care Med. 2001, 29, 2258–2263. [Google Scholar] [CrossRef]
- Gélinas, C.; Fillion, L.; Puntillo, K.A.; Viens, C.; Fortier, M. Validation of the Critical-Care Pain Observation Tool in Adult Patients. Am. J. Crit. Care 2006, 15, 420–427. [Google Scholar] [CrossRef]
- Rijkenberg, S.; Stilma, W.; Endeman, H.; Bosman, R.; Oudemans-van Straaten, H. Pain measurement in mechanically ventilated critically ill patients: Behavioral Pain Scale versus Critical-Care Pain Observation Tool. J. Crit. Care 2015, 30, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Rijkenberg, S.; Stilma, W.; Bosman, R.J.; van der Meer, N.J.; van der Voort, P.H. Pain Measurement in Mechanically Ventilated Patients After Cardiac Surgery: Comparison of the Behavioral Pain Scale (BPS) and the Critical-Care Pain Observation Tool (CPOT). J. Cardiothorac. Vasc. Anesth. 2017, 31, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
- Georgiou, E.; Hadjibalassi, M.; Lambrinou, E.; Andreou, P.; Papathanassoglou, E.D. The Impact of Pain Assessment on Critically Ill Patients’ Outcomes: A Systematic Review. BioMed Res. Int. 2015, 2015, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Batalha, L.M.C.; Figueiredo, A.M.; Marques, M.; Bizarro, V. Cultural adaptation and psychometric properties of the Portuguese version of the Behavioral Pain Scale—Intubated Patient (BPS-IP/PT). Rev. Enf. Ref. 2013, 3, 7–16. [Google Scholar] [CrossRef]
- Echegaray-Benites, C.; Kapoustina, O.; Gélinas, C. Validation of the use of the Critical-Care Pain Observation Tool (CPOT) with brain surgery patients in the neurosurgical intensive care unit. Intensiv. Crit. Care Nurs. 2014, 30, 257–265. [Google Scholar] [CrossRef]
- Damström, D.N.; Saboonchi, F.; Sackey, P.V.; Björling, G. A preliminary validation of the Swedish version of the critical-care pain observation tool in adults. Acta Anaesthesiol. Scand. 2011, 55, 379–386. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M. Guidelines for the Process of Cross-Cultural Adaptation of Self-Report Measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Reichenheim, M.; Moraes, C. Operationalizing the cross-cultural adaptation of epidemiological measurement instruments. Rev. Saúde Pública 2007, 41, 665–673. [Google Scholar] [CrossRef]
- Gélinas, C.; Joffe, D.A.M.; Szumita, P.M.; Payen, J.-F.; Bérubé, M.; T., S.S.; Boitor, M.; Chanques, G.; Puntillo, K.A. A Psychometric Analysis Update of Behavioral Pain Assessment Tools for Noncommunicative, Critically Ill Adults. AACN Adv. Crit. Care 2019, 30, 365–387. [Google Scholar] [CrossRef]
- Topolovec-Vranic, J.; Gélinas, C.; Li, Y.; Pollmann-Mudryj, M.A.; Innis, J.; McFarlan, A.; Canzian, S. Validation and Evaluation of Two Observational Pain Assessment Tools in a Trauma and Neurosurgical Intensive Care Unit. Pain Res. Manag. 2013, 18, 107–114. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kotfis, K.; Zegan-Baranska, M.; Szydlowski, L.; Żukowski, M.; Ely, E.W. Methods of pain assessment in adult intensive care unit patients—Polish version of the CPOT (Critical Care Pain Observation Tool) and BPS (Behavioral Pain Scale). Anaesthesiol. Intensive Ther. 2017, 49, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Puntillo, K.; White, C.; Morris, A.; Perdue, S.; Stanik-Hutt, J.; Thompson, C.; Wild, L. Patients’ perceptions and responses to procedural pain: Results from Thunder Project II. Am. J. Crit. Care 2001, 10, 238–251. Available online: https://pubmed.ncbi.nlm.nih.gov/11432212/ (accessed on 5 December 2021). [CrossRef] [PubMed]
- Gélinas, C.; Arbour, C.; Michaud, C.; Vaillant, F.; Desjardins, S. Implementation of the critical-care pain observation tool on pain assessment/management nursing practices in an intensive care unit with nonverbal critically ill adults: A before and after study. Int. J. Nurs. Stud. 2011, 48, 1495–1504. [Google Scholar] [CrossRef]
- Pinheiro, A.; Marques, R. Behavioral Pain Scale and Critical Care Pain Observation Tool for pain evaluation in orotracheally tubed critical patients. A systematic review of the literature. Rev. Bras. Ter. Intensiva 2019, 31, 571–581. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. Available online: https://www.jstor.org/stable/2529310?seq=1 (accessed on 18 December 2021). [CrossRef]
- WMA. Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 18 December 2021).
- Hanley, J.A.; McNeil, B.J. The meaning and the use of the area under a receiver operating characteristic (ROC) curve. Radiology 1982, 143, 29–36. [Google Scholar] [CrossRef]
- Vadelka, A.; Busnelli, A.; Bonetti, L. Comparison Between Two Behavioural Scales for the Evaluation of Pain in Critical Patients, as Related to the State of Sedation: An Observational Study. Scenario 2017, 34, 4–14. [Google Scholar] [CrossRef]
- Frandsen, J.; O’Reilly, P.K.; Laerkner, E.; Stroem, T. Validation of the Danish version of the Critical Care Pain Observation Tool. Acta Anaesthesiol. Scand 2016, 60, 1314–1322. [Google Scholar] [CrossRef]
- Klein, C.; Caumo, W.; Gélinas, C.; Patines, V.; Pilger, T.; Lopes, A.; Backes, F.N.; Villas-Boas, D.F.; Vieira, S.R.R. Validation of Two Pain Assessment Tools Using a Standardized Nociceptive Stimulation in Critically Ill Adults. J. Pain Symptom Manag. 2018, 56, 594–601. [Google Scholar] [CrossRef]
- Gélinas, C.; Johnston, C. Pain assessment in the critically ill ventilated adult: Validation of the critical-care pain observation tool and physiologic indicators. Clin. J. Pain 2007, 23, 497–505. [Google Scholar] [CrossRef] [PubMed]
- Gelinas, C.; Tousignant-Laflamme, Y.; Tanguay, A.; Bourgault, P. Exploring the validity of the bispectral index, the Critical-Care Pain Observation Tool and vital signs for the detection of pain in sedated and mechanically ventilated critically ill adults: A pilot study. Intensive Crit. Care Nurs. 2011, 27, 46–52. [Google Scholar] [CrossRef] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).