Palliative Care for Patients with End-Stage, Non-Oncologic Diseases—A Retrospective Study in Three Public Palliative Care Departments in Northern Italy
Abstract
:1. Introduction
2. Materials and Methods
3. Results
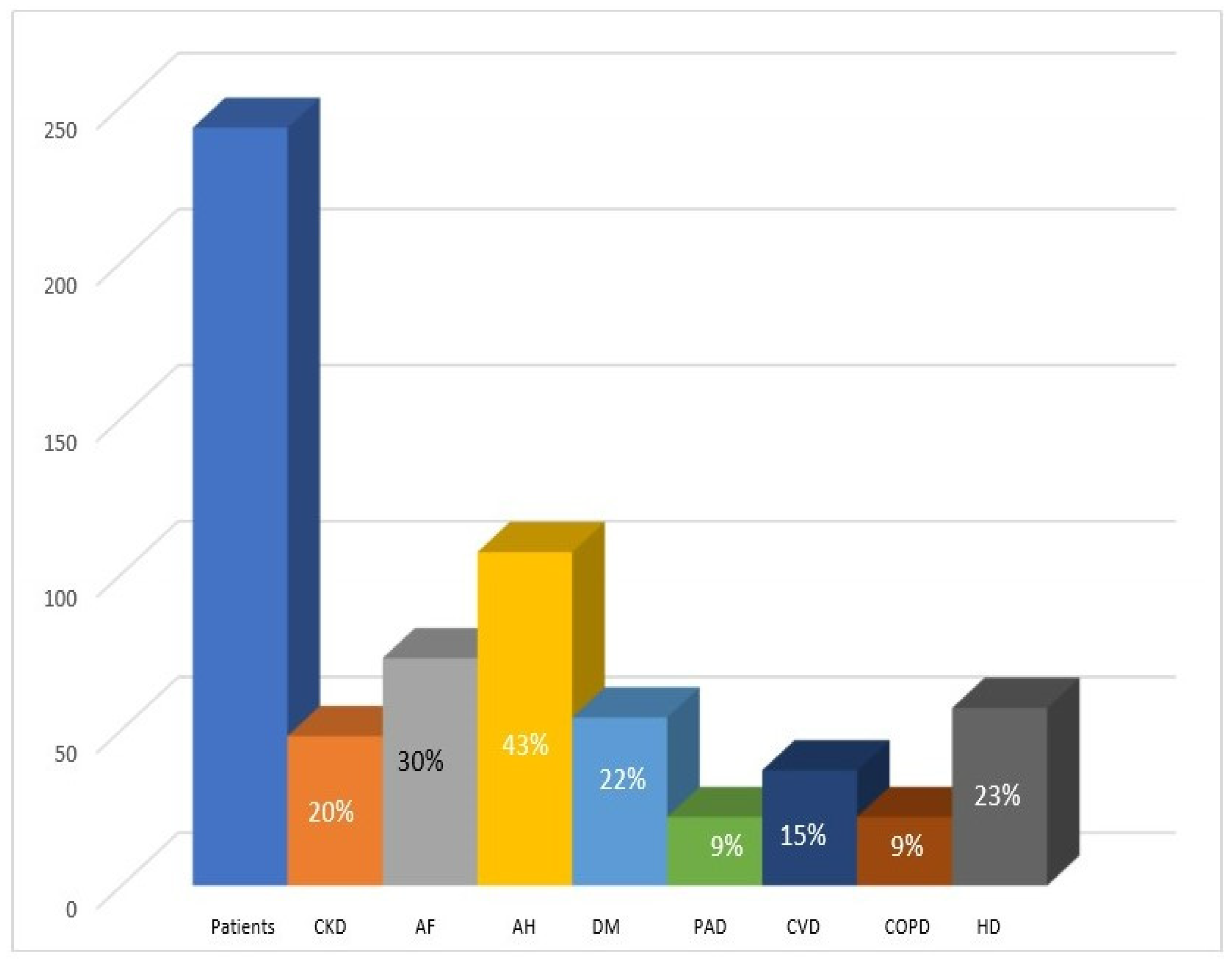
3.1. Baseline Patient Profiles
3.2. Palliative Care Characteristics and Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Available online: http://www.who.int/cancer/palliative/definition/en (accessed on 28 November 2020).
- World Health Organization. Global Atlas of Palliative Care at the End of Life. 2014. Available online: www.who.int (accessed on 12 March 2022).
- Sleeman, K.E.; de Brito, M.; Etkind, S.; Nkhoma, K.; Guo, P.; Higginson, I.J.; Gomes, B.; Harding, R. The escalating global burden of serious health-related suffering: Projections to 2060 by world regions, age groups, and health conditions. Lancet Glob. Health 2019, 7, e883–e892. [Google Scholar] [CrossRef] [Green Version]
- Radbruch, L.; Payne, S. White Paper on standards and norms for hospice and palliative care in Europe: Part 1. Eur. J. Palliat. Care 2009, 16, 278–289. [Google Scholar]
- Kelley, A.S.; Morrison, R.S. Palliative Care for the seriously ill. N. Engl. J. Med. 2015, 373, 747–755. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McIlvennan, C.K.; Allen, L.A. Palliative care in patients with heart failure. BMJ 2016, 353, i1010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ho, F.; Lau, F.; Downing, M.G.; Lesperance, M. A reliability and validity study of the Palliative Performance Scale. BMC Palliat. Care 2008, 7, 10. [Google Scholar] [CrossRef] [Green Version]
- Lau, C.; Meaney, C.; Morgan, M.; Cook, R.; Zimmermann, C.; Wentlandt, K. Disparities in access to palliative care facilities for patients with and without cancer: A retrospective review. Palliat. Med. 2021, 35, 1191–1201. [Google Scholar] [CrossRef]
- Quinn, K.L.; Stukel, T.; Stall, N.M.; Huang, A.; Isenberg, S.; Tanuseputro, P.; Goldman, R.; Cram, P.; Kavalieratos, D.; Detsky, A.S.; et al. Association between palliative care and healthcare outcomes among adults with terminal non-cancer illness: Population based matched cohort study. BMJ 2020, 370, m2257. [Google Scholar] [CrossRef]
- Gold Standard Framework. Proactive Identification Guidance, 6th ed.; GSF: Shrewsbury, UK, 2017; Available online: www.goldstandardsframework.org.uk/PIG (accessed on 20 July 2020).
- Highet, G.; Crawford, D.; Murray, S.A.; Boyd, K. Development and evaluation of the supportive and palliative care indicators tool (SPICT): A mixed-methods study. BMJ Support. Palliat. Care 2014, 4, 285–290. [Google Scholar] [CrossRef]
- Gómez-Batiste, X.; Martínez-Muñoz, M.; Blay, C.; Amblas, J.; Vila, L.; Costa, X.; Espaulella, J.; Villanueva, A.; Oller, R.; Martori, J.C.; et al. Utility of the NECPAL CCOMS-ICO© tool and the surprise question as screening tools for early palliative care and to predict mortality in patients with advanced chronic conditions: A cohort study. Palliat. Med. 2017, 31, 754–763. [Google Scholar] [CrossRef]
- Deliberazione Giunta Regionale-Lombardia, n. XI/1046 del 17 dicembre 2018. Available online: www.regione.lombardia.it (accessed on 12 March 2022).
- Karnofsky, D.A.; Burchenal, J.H. The clinical evaluation of chemotherapeutic agents in cancer. In Evaluation of chemotherapeutic agents; MacLeod, C.M., Ed.; Columbia University Press: New York, NY, USA, 1949; pp. 191–205. [Google Scholar]
- Gòmez-Baptiste, X.; Martinez-Munoz, M.; Blay, C.; Amblàs, J.; Vila, L.; Costa, X.; Espaulella, J.; Espinosa, J.; Constante, C.; Mitchell, G.K. Prevalence and characteristics of patients with advanced chronic conditions in need of palliative care in the general population: A cross-sectional study. Palliat. Med. 2014, 28, 302–311. [Google Scholar] [CrossRef]
- Morita, T.; Tsunoda, J.; Inoue, S.; Chihara, S. The Palliative Prognostic Index: A scoring system for survival prediction of terminally ill cancer patients. Support Care Cancer 1999, 7, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Scaccabarozzi, G.L.; Lovaglio, P.G.; Limonta, F.; Peruselli, C.; Bellentani, M.; Crippa, M. Monitoring the Italian Home Palliative Care Services. Healthcare 2019, 7, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scaccabarozzi, G.; Amodio, E.; Riva, L.; Corli, O.; Maltoni, M.; Di Silvestre, G.; Turriziani, A.; Morino, P.; Pellegrini, G.; Crippa, M. Clinical Care Conditions and Needs of Palliative Care Patients from Five Italian Regions: Preliminary Data of the DEMETRA Project. Healthcare 2020, 8, 221. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.nhpco.org/hospice-care-overview/hospice-facts-figures/2021EDITION (accessed on 12 March 2022).
- Gadoud, A.; Kane, E.; Oliver, S.E.; Johnson, M.J.; Macleod, U.; Allgar, V. Palliative care for non-cancer conditions in primary care: A time trend analysis in the UK (2009–2014). BMJ Support. Palliat. Care 2020. [Google Scholar] [CrossRef] [PubMed]
- Day, T. Managing the nutritional needs of palliative care patients. Br. J. Nurs. 2017, 26, 21. [Google Scholar] [CrossRef]
- Johnson, M.J.; Bland, J.M.; Gahbauer, E.A.; Ekström, M.; Sinnarajah, A.; Gill, T.M.; Currow, D.C. Breathlessness in Elderly Adults During the Last Year of Life Sufficient to Restrict Activity: Prevalence, Pattern, and Associated Factors. J. Am. Geriatr. Soc. 2016, 64, 73–80. [Google Scholar] [CrossRef]
- Singer, A.; Meeker, D.; Teno, J.; Lynn, J.; Lunney, J.R.; Lorenz, K.A. Symptom trends in the last year of life from 1998 to 2010: A cohort study. Ann. Intern. Med. 2015, 162, 175–183. [Google Scholar] [CrossRef] [Green Version]
- Warraich, H.; Wolf, S.P.; Mentz, R.; Rogers, J.G.; Samsa, G.; Kamal, A.H. Characteristics and trends among patients with cardiovascular disease referred to palliative care. JAMA Netw. Open 2019, 2, e192375. [Google Scholar] [CrossRef]
- Riley, J.P.; Beattie, J.M. Palliative care in heart failure: Facts and numbers. ESC Heart Fail. 2017, 4, 81–87. [Google Scholar] [CrossRef]
- Gadoud, A.; Kane, E.; Macleod, U.; Ansell, P.; Oliver, S.; Johnson, M. Palliative care among heart failure patients in primary care: A comparison to cancer patients using English family practice data. PLoS ONE 2014, 9, e113188. [Google Scholar] [CrossRef]
- Bostwick, D.; Wolf, S.; Samsa, G.; Bull, J.; Taylor, D.H., Jr.; Johnson, K.S.; Kamal, A.H. Comparing the Palliative Care Needs of Those with Cancer to Those with Common Non-Cancer Serious Illness. J. Pain Symptom. Manag. 2017, 53, 1079–1084. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kavalieratos, D.; Mitchell, E.M.; Carey, T.S.; Dev, S.; Biddle, A.K.; Reeve, B.B.; Abernethy, A.P.; Weinberger, M. Not the grim reaper service: An assessment of provider knowledge, attitudes, and perceptions regarding palliative care referral barriers in heart Failure. J. Am. Heart Assoc. 2014, 3, e000544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamal, A.H.; Wolf, S.P.; Troy, J.; Leff, V.; Dahlin, C.; Rotella, J.D.; Handzo, G.; Rodgers, P.E.; Myers, E.R. Policy Changes Key To Promoting Sustainability And Growth Of The Specialty Palliative Care Workforce. Health Aff. 2019, 38, 910–918. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romanò, M. Barriers to Early Utilization of Palliative Care in Heart Failure: A Narrative Review. Healthcare 2020, 8, 36. [Google Scholar] [CrossRef] [Green Version]
- Cherny, N.I. Stigma associated with “palliative care”: Getting around it or getting over it. Cancer 2009, 115, 1808–1812. [Google Scholar] [CrossRef]
- Siouta, N.; Clement, P.; Aertgeerts, B.; Van Beek, K.; Menten, J. Professionals’ perceptions and current practices of integrated palliative care in chronic heart failure and chronic obstructive pulmonary disease: A qualitative study in Belgium. BMC Palliat. Care 2018, 17, 103. [Google Scholar] [CrossRef]
| Total Cohort | Primary Diagnosis | |||||||
|---|---|---|---|---|---|---|---|---|
| Dementia | HD | Lung Disease | Stroke | Neurological Disease | CKD | LD | ||
| Patients (n/%) | 243 (100%) | 78 (32%) | 55 (23%) | 30 (12%) | 29 (12%) | 22 (9%) | 17 (7%) | 12 (5%) |
| Males (n/%) | 112 (46.1%) | 24 (31%) | 21 (38%) | 17 (57%) | 16 (55%) | 16 (73%) | 11 (65%) | 7 (58%) |
| Age (mean − years) | 83.5 | 85.7 | 85.7 | 81.8 | 84.6 | 76.6 | 83.4 | 74.5 |
| Females (n/%) | 131 (53.9%) | 54 (69%) | 34 (62%) | 13 (43%) | 13 (45%) | 6 (27%) | 6 (35%) | 5 (42%) |
| Age (mean − years) | 85.4 | 87.4 | 86.7 | 82.8 | 84 | 78.1 | 86.3 | 75.2 |
| Origin of PCN referral | ||||||||
| Acute-care hospital | 156 (64%) | 43 (55%) | 35 (64%) | 24 (80%) | 23 (79%) | 10 (45%) | 14 (82%) | 7 (58%) |
| Home | 84 (35%) | 33 (42%) | 20 (36%) | 6 (20%) | 5 (18%) | 12 (55%) | 3 (18%) | 5 (42%) |
| Nursing home | 3 (1%) | 2 (3%) | 1 (3%) | |||||
| Baseline clinical findings | ||||||||
| General indicators of disease severity a | ||||||||
| History of ≥2 urgent hospitalizations b | 128 (53%) | 34 (44%) | 31 (56%) | 22 (73%) | 13 (45%) | 9 (39%) | 8 (47%) | 11 (92%) |
| ≥2 comorbidities | 224 (92%) | 70 (89.7%) | 54 (98%) | 30 (100%) | 28 (97%) | 17 (78%) | 16 (94%) | 9 (75%) |
| Malnutrition c | 199 (82%) | 70 (90%) | 41 (74%) | 21 (70%) | 24 (83%) | 16 (74%) | 15 (88%) | 12 (100%) |
| All 3 of the above | 101 (42%) | 30 (39%) | 22 (40 | 15 (50%) | 12 (41%) | 7 (30%) | 7 (41%) | 8 (67%) |
| KPSS 20–10% 30–40% | 155 (64%) 88 (36%) | 60 (77%) 18 (23%) | 26 (48%) 29 (52%) | 12 (40%) 18 (60%) | 22 (75%) 7 (25%) | 15 (68%%) 7 (32%) | 12 (71%) 5 (29%) | 8 (64%) 4 (36%) |
| Most common symptoms | ||||||||
| Pain | 133 (55%) | 39 (50%) | 41 (73%) | 13 (44%) | 19 (66%) | 10 (43%) | 9 (54%) | 2 (17%) |
| Dyspnea | 128 (53%) | 30 (39%) | 39 (69%) | 29 (95%) | 13 (42%) | 9 (41%) | 8 (47%) | 0 |
| Fatigue | 153 (63%) | 38 (49%) | 48 (86%) | 21 (68%) | 12 (41%) | 18 (78%) | 12 (70%) | 4 (33%) |
| ≥2 of the above | 148 (61%) | 32 (42%) | 49 (89%) | 23 (77%) | 16 (55%) | 12 (56%) | 10 (59%) | 6 (50%) |
| None of the above | 12 (5%) | 6 (8%) | (0%) | (0%) | 4 (14%) | 2 (9%) | (0%) | (0%) |
| Total Cohort | Primary Diagnoses | |||||||
|---|---|---|---|---|---|---|---|---|
| Dementia | HD | Lung Disease | Stroke | Neurological Disease | CKD | LD | ||
| Patients (n/%) | 243 (100%) | 78 (32%) | 55 (23%) | 30 (12%) | 29 (12%) | 22 (9%) | 17 (7%) | 12 (5%) |
| Palliative care setting Hospice (n/%) Home (n/%) Both (n/%) | 141 (58%) 85 (35%) 17 (7%) | 44 (56%) 34 (44%) | 28 (51%) 27 (49%) | 19 (63%) 11 (37%) | 23(79%) 6 (21%) | 10 (48%) 12 (52%) | 14 (82%) 3 (18%) | 7 (58%) 5 (42%) |
| In-network mortality | 228 (93.8%) | 72 (92%) | 49 (89%) | 29 (97%) | 29 (100%) | 20 (91%) | 17 (100%) | 12 (100%) |
| Time of death b <3 weeks 3–6 weeks >6 weeks | 172 (75%) 21 (9%) 35 (16%) | 53 (74%) 6 (8%) 13 (18%) | 34 (69%) 5 (10%) 10 (21%) | 21 (73%) 3 (10%) 5 (17%) | 24(83%) 2 (7%) 3 (10%) | 12 (60%) 4 (20%) 4 (20%) | 17 (100%) | 11 (92%) 1 (8%) |
| Setting of death Hospice Home Acute care | 133 (58.4%) 94 (41.2%) 1 (0.4%) | 30 (42%) 42 (58%) 0 | 26 (53%) 22 (45%) 1 (2%) | 19 (66%) 10 (34) 0 | 24 (83%) 5 (17 0 | 13 (68%) 7 (32%) 0 | 14 (82%) 3 (18%) 0 | 7 (58%) 5 (42%) 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romanò, M.; Oldani, S.; Reina, V.; Sofia, M.; Castiglioni, C. Palliative Care for Patients with End-Stage, Non-Oncologic Diseases—A Retrospective Study in Three Public Palliative Care Departments in Northern Italy. Healthcare 2022, 10, 1031. https://doi.org/10.3390/healthcare10061031
Romanò M, Oldani S, Reina V, Sofia M, Castiglioni C. Palliative Care for Patients with End-Stage, Non-Oncologic Diseases—A Retrospective Study in Three Public Palliative Care Departments in Northern Italy. Healthcare. 2022; 10(6):1031. https://doi.org/10.3390/healthcare10061031
Chicago/Turabian StyleRomanò, Massimo, Sabina Oldani, Valter Reina, Michele Sofia, and Claudia Castiglioni. 2022. "Palliative Care for Patients with End-Stage, Non-Oncologic Diseases—A Retrospective Study in Three Public Palliative Care Departments in Northern Italy" Healthcare 10, no. 6: 1031. https://doi.org/10.3390/healthcare10061031
APA StyleRomanò, M., Oldani, S., Reina, V., Sofia, M., & Castiglioni, C. (2022). Palliative Care for Patients with End-Stage, Non-Oncologic Diseases—A Retrospective Study in Three Public Palliative Care Departments in Northern Italy. Healthcare, 10(6), 1031. https://doi.org/10.3390/healthcare10061031





