Hidden Truth in Cerebral Concussion—Traumatic Axonal Injury: A Narrative Mini-Review
Abstract
:1. Introduction
2. Ambiguity of Diagnostic Criteria for Concussion and Diffuse Axonal Injury
3. Limitation of Conventional Brain MRI in the Detection of TAI in Concussion
4. Evidence of Organic Brain Injury in Concussion
5. History of Traumatic Axonal Injury in Concussion
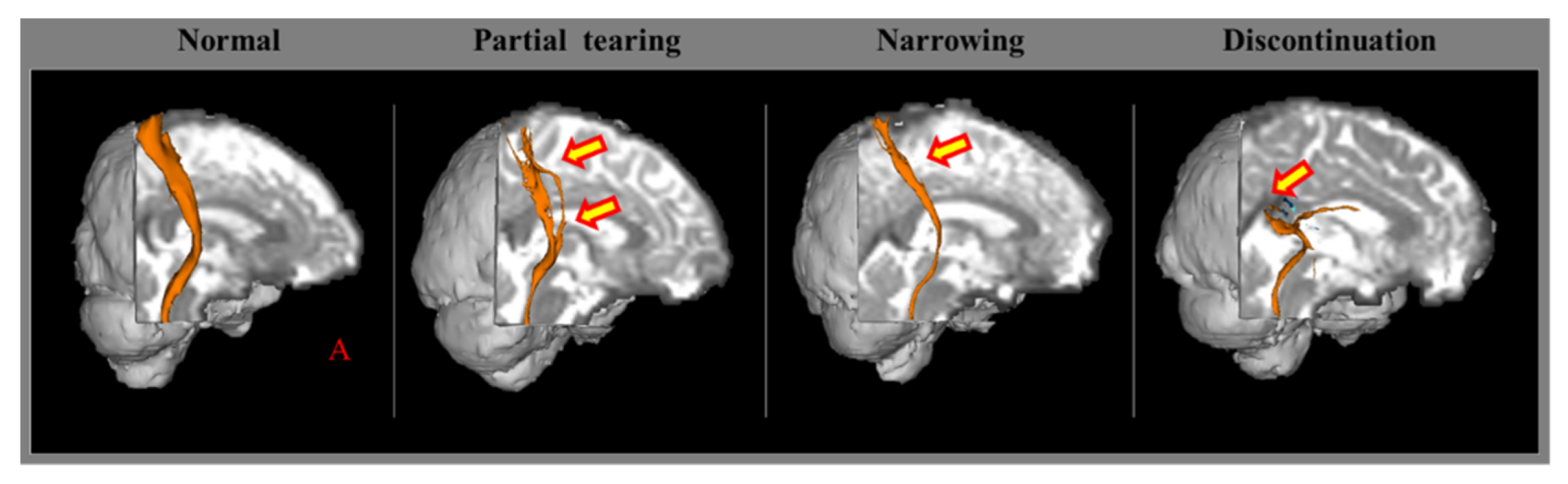
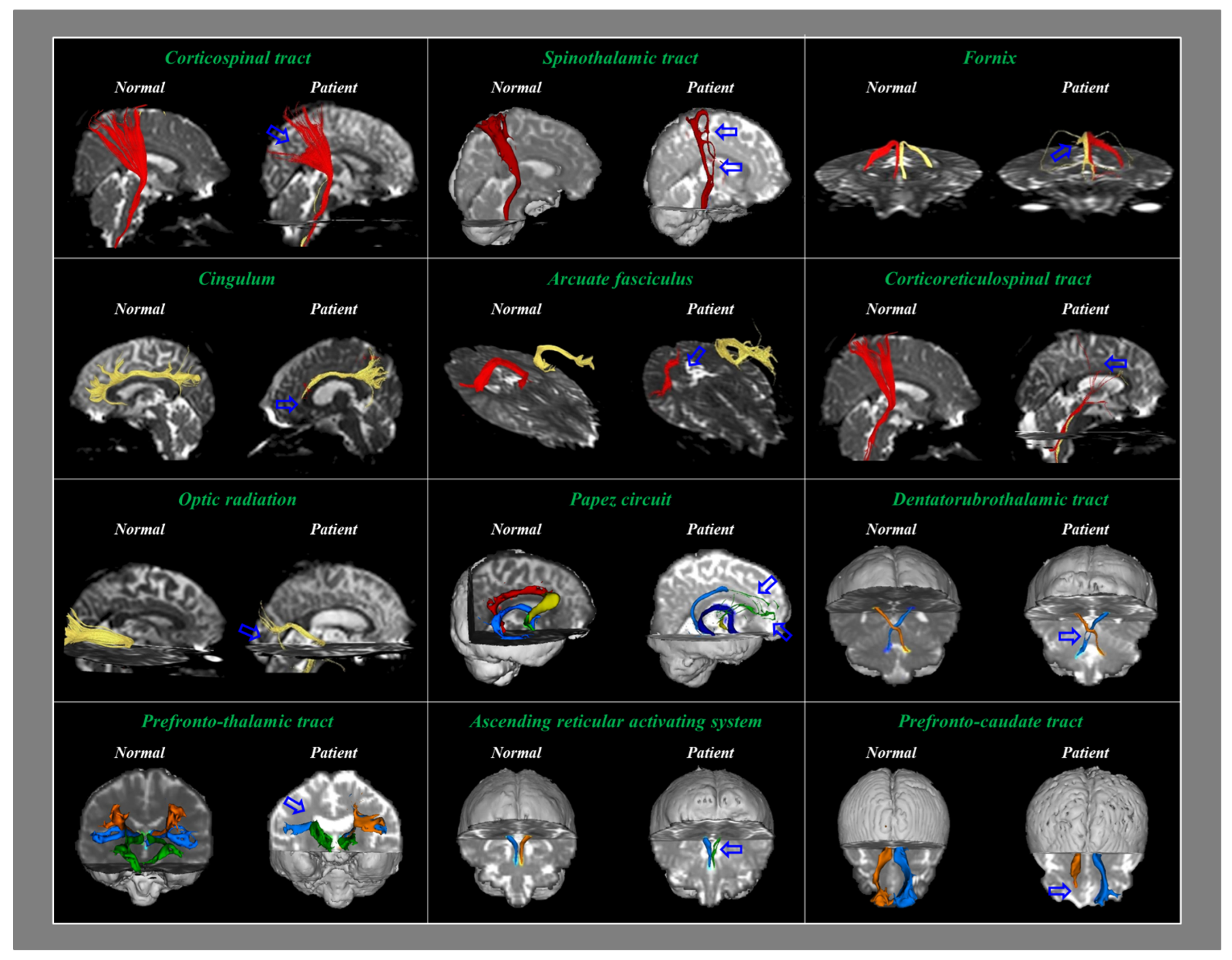
6. Detection of Traumatic Axonal Injury in Concussion Using Diffusion Tensor Imaging
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aubry, M.; Cantu, R.; Dvorak, J.; Graf-Baumann, T.; Johnston, K.; Kelly, J.; Lovell, M.; McCrory, P.; Meeuwisse, W.; Schamasch, P.; et al. Summary and agreement statement of the first international conference on concussion in sport, Vienna 2001. Recommendations for the improvement of safety and health of athletes who may suffer concussive injuries. Br. J. Sports Med. 2002, 36, 6–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anderson, T.; Heitger, M.; Macleod, A.D. Concussion and mild head injury. Pract. Neurol. 2006, 6, 342–357. [Google Scholar] [CrossRef] [Green Version]
- Saatman, K.E.; Duhaime, A.C.; Bullock, R.; Maas, A.I.; Valadka, A.; Manley, G.T. Classification of traumatic brain injury for targeted therapies. J. Neurotrauma. 2008, 25, 719–738. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mild Traumatic Brain Injury Committee. American Congress of Rehabilitation: Head injury interdisciplinary special interest group: Definition of mild traumatic brain injury. J. Head Trauma Rehabil. 1993, 8, 86–87. [Google Scholar] [CrossRef]
- McCrory, P.R.; Berkovic, S.F. Concussion: The history of clinical and pathophysiological concepts and misconceptions. Neurology 2001, 57, 2283–2289. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.H. Diagnostic problems in diffuse axonal injury. Diagnostics 2020, 10, 117. [Google Scholar] [CrossRef] [Green Version]
- Hill, C.S.; Coleman, M.P.; Menon, D.K. Traumatic axonal injury: Mechanisms and translational opportunities. Trends Neurosci. 2016, 39, 311–324. [Google Scholar] [CrossRef] [Green Version]
- Jang, S.H. Traumatic axonal injury in mild traumatic brain injury. In Traumatic Brain Injury, 1st ed.; Gorbunoy, N., Ed.; InTech: London, UK, 2018; pp. 137–154. [Google Scholar]
- Povlishock, J.T.; Becker, D.P.; Cheng, C.L.; Vaughan, G.W. Axonal change in minor head injury. J. Neuropathol. Exp. Neurol. 1983, 42, 225–242. [Google Scholar] [CrossRef]
- Gajawelli, N.; Lao, Y.; Apuzzo, M.L.; Romano, R.; Liu, C.; Tsao, S.; Hwang, D.; Wilkins, B.; Lepore, N.; Law, M. Neuroimaging changes in the brain in contact versus noncontact sport athletes using diffusion tensor imaging. World Neurosurg. 2013, 80, 824–828. [Google Scholar] [CrossRef] [Green Version]
- Tremblay, S.; Henry, L.C.; Bedetti, C.; Larson-Dupuis, C.; Gagnon, J.F.; Evans, A.C.; Theoret, H.; Lassonde, M.; De Beaumont, L. Diffuse white matter tract abnormalities in clinically normal ageing retired athletes with a history of sports-related concussions. Brain 2014, 137, 2997–3011. [Google Scholar] [CrossRef] [Green Version]
- Povlishock, J.T.; Erb, D.E.; Astruc, J. Axonal response to traumatic brain injury: Reactive axonal change, deafferentation, and neuroplasticity. J. Neurotrauma 1992, 9, S189–S200. [Google Scholar] [PubMed]
- Jang, S.H. Diagnostic history of traumatic axonal injury in patients with cerebral concussion and mild traumatic brain Injury. Brain. Neurorehabil. 2016, 9, e1. [Google Scholar] [CrossRef] [Green Version]
- Oppenheimer, D.R. Microscopic lesions in the brain following head injury. J. Neurol. Neurosurg. Psychiatry 1968, 31, 299–306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blumbergs, P.C.; Scott, G.; Manavis, J.; Wainwright, H.; Simpson, D.A.; McLean, A.J. Staining of amyloid precursor protein to study axonal damage in mild head injury. Lancet 1994, 344, 1055–1056. [Google Scholar] [CrossRef]
- Bigler, E.D. Neuropsychological results and neuropathological findings at autopsy in a case of mild traumatic brain injury. J. Int. Neuropsychol. Soc. 2004, 10, 794–806. [Google Scholar] [CrossRef]
- Arfanakis, K.; Haughton, V.M.; Carew, J.D.; Rogers, B.P.; Dempsey, R.J.; Meyerand, M.E. Diffusion tensor MR imaging in diffuse axonal injury. AJNR Am. J. Neuroradiol. 2002, 23, 794–802. [Google Scholar]
- Shenton, M.E.; Hamoda, H.M.; Schneiderman, J.S.; Bouix, S.; Pasternak, O.; Rathi, Y.; Vu, M.-A.; Purohit, M.P.; Helmer, K.; Koerte, I.; et al. A review of magnetic resonance imaging and diffusion tensor imaging findings in mild traumatic brain injury. Brain Imaging Behav. 2012, 6, 137–192. [Google Scholar] [CrossRef]
- DSouza, M.M.; Trivedi, R.; Singh, K.; Grover, H.; Choudhury, A.; Kaur, P.; Kumar, P.; Tripathi, R.P. Traumatic brain injury and the post-concussion syndrome: A diffusion tensor tractography study. Indian J. Radiol. Imaging 2015, 25, 404–414. [Google Scholar] [CrossRef]
- Kim, J.H.; Ahn, S.H.; Cho, Y.W.; Kim, S.H.; Jang, S.H. The relation between injury of the spinothalamocortical tract and central pain in chronic patients with mild traumatic brain injury. J. Head Trauma Rehabil. 2015, 30, E40–E46. [Google Scholar] [CrossRef]
- Jang, S.H.; Kwon, Y.H. Central pain due to traumatic axonal injury of the spinothalamic tract in patients with mild traumatic brain Injury. Brain Neurorehabil. 2018, 11, e7. [Google Scholar] [CrossRef] [Green Version]
- Tayebi, M.; Holdsworth, S.J.; Champagne, A.A.; Cook, D.J.; Nielsen, P.; Lee, T.R.; Wang, A.; Fernandez, J.; Shim, V. The role of diffusion tensor imaging in characterizing injury patterns on athletes with concussion and subconcussive injury: A systematic review. Brain Inj. 2021, 35, 621–644. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Huang, C.; Li, M.; Zhang, H.; Liu, J. White matter abnormalities and cognitive deficit after mild traumatic brain injury: Comparing DTI, DKI, and NODDI. Front. Neurol. 2022, 13, 803066. [Google Scholar] [CrossRef] [PubMed]
- Tamez-Pena, J.; Rosella, P.; Totterman, S.; Schreyer, E.; Gonzalez, P.; Venkataraman, A.; Meyers, S.P. Post-concussive mTBI in student athletes: MRI features and machine learning. Front. Neurol. 2021, 12, 734329. [Google Scholar] [CrossRef] [PubMed]
- Crasta, J.E.; Tucker, R.N.; Robinson, J.; Chen, H.W.; Crocetti, D.; Suskauer, S.J. Altered white matter diffusivity and subtle motor function in a pilot cohort of adolescents with sports-related concussion. Brain Inj. 2022, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.H.; Bae, C.H.; Kim, J.W.; Kwon, H.G. Relationship between dizziness and the core vestibular projection injury in patients with mild traumatic brain injury. Diagnostics 2021, 11, 2070. [Google Scholar] [CrossRef]
- Jang, S.H.; Kim, S.H.; Kwon, H.G. Diagnostic sensitivity of traumatic axonal injury of the spinothalamic tract in patients with mild traumatic brain injury. Medicine 2022, 101, e28536. [Google Scholar] [CrossRef]
- Chang, M.C.; Seo, J.P. Injury of the dentato-rubro-thalamic tract in a patient with intentional tremor after mild traumatic brain injury: A case report. Brain Inj. 2020, 34, 1283–1286. [Google Scholar] [CrossRef]
- Jang, S.H.; Lee, H.D. Diagnostic approach to traumatic axonal injury of the spinothalamic tract in individual patients with mild traumatic brain injury. Diagnostics 2019, 9, 199. [Google Scholar] [CrossRef] [Green Version]
- Jang, S.H.; Lee, H.D. Diagnostic approach to traumatic axonal injury of the optic radiation in mild traumatic brain injury. Am. J. Phys. Med. Rehabil. 2019, 98, e92–e96. [Google Scholar] [CrossRef]
- Jang, S.H.; Seo, Y.S. Diffusion tensor tractography characteristics of axonal injury in concussion/mild traumatic brain injury. Neural. Regen. Res. 2022, 17, 978–982. [Google Scholar] [CrossRef]
- Jang, S.H.; Kim, S.H.; Lee, H.D. Difference in the ascending reticular activating system injury between mild traumatic brain injury and cerebral concussion. Transl. Neurosci. 2019, 10, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.H.; Kim, O.L.; Kim, S.H.; Kim, J.B. The relation between loss of consciousness, severity of traumatic brain injury, and injury of ascending reticular activating system in patients with traumatic brain injury. Am. J. Phys. Med. Rehabil. 2019, 98, 1067–1071. [Google Scholar] [CrossRef] [PubMed]
- Gennarelli, T.A. Cerebral Concussion and Diffuse Brain Injuries. In Head Injury, 3rd ed.; Williams & Wilkins: Baltimore, MD, USA, 1993. [Google Scholar]
- Gennarelli, T.A.; Thibault, L.E.; Adams, J.H.; Graham, D.I.; Thompson, C.J.; Marcincin, R.P. Diffuse axonal injury and traumatic coma in the primate. Ann. Neurol. 1982, 12, 564–574. [Google Scholar] [CrossRef] [PubMed]
- Mittl, R.L.; Grossman, R.I.; Hiehle, J.F.; Hurst, R.W.; Kauder, D.R.; Gennarelli, T.A.; Alburger, G.W. Prevalence of MR evidence of diffuse axonal injury in patients with mild head injury and normal head CT findings. AJNR Am. J. Neuroradiol. 1994, 15, 1583–1589. [Google Scholar] [PubMed]
- Topal, N.B.; Hakyemez, B.; Erdogan, C.; Bulut, M.; Koksal, O.; Akkose, S.; Dogan, S.; Parlak, M.; Ozguc, H.; Korfali, E. MR imaging in the detection of diffuse axonal injury with mild traumatic brain injury. Neurol. Res. 2008, 30, 974–978. [Google Scholar] [CrossRef]
- Humble, S.S.; Wilson, L.D.; Wang, L.; Long, D.A.; Smith, M.A.; Siktberg, J.C.; Mirhoseini, M.F.; Bhatia, A.; Pruthi, S.; Day, M.A.; et al. Prognosis of diffuse axonal injury with traumatic brain injury. J. Trauma Acute Care Surg. 2018, 85, 155–159. [Google Scholar] [CrossRef]
- Adams, J.H.; Graham, D.I.; Murray, L.S.; Scott, G. Diffuse axonal injury due to nonmissile head injury in humans: An analysis of 45 cases. Ann. Neurol. 1982, 12, 557–563. [Google Scholar] [CrossRef]
- Gentry, L.R.; Godersky, J.C.; Thompson, B. MR imaging of head trauma: Review of the distribution and radiopathologic features of traumatic lesions. AJR Am. J. Roentgenol. 1988, 150, 663–672. [Google Scholar] [CrossRef] [Green Version]
- Katzman, G.L. Trauma, Diffuse axonal injury. In Diagnostic Imaging; Osborn, A.G., Salzman, K.L., Barkovich, A.J., Eds.; Amirsys: Salt Lake City, UT, USA, 2010. [Google Scholar]
- Chung, S.W.; Park, Y.S.; Nam, T.K.; Kwon, J.T.; Min, B.K.; Hwang, S.N. Locations and clinical significance of non-hemorrhagic brain lesions in diffuse axonal injuries. J. Korean Neurosurg. Soc. 2012, 52, 377–383. [Google Scholar] [CrossRef]
- WHO. The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research; World Health Organization: Geneva, Switzerland, 1993. [Google Scholar]
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorder, 4th ed; American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar]
- Rutherford, W.H.; Merrett, J.D.; McDonald, J.R. Symptoms at one year following concussion from minor head injuries. Injury 1979, 10, 225–230. [Google Scholar] [CrossRef]
- McMahon, P.; Hricik, A.; Yue, J.K.; Puccio, A.M.; Inoue, T.; Lingsma, H.F.; Beers, S.R.; Gordon, W.A.; Valadka, A.B.; Manley, G.T.; et al. Symptomatology and functional outcome in mild traumatic brain injury: Results from the prospective TRACK-TBI study. J. Neurotrauma 2014, 31, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Khong, E.; Odenwald, N.; Hashim, E.; Cusimano, M.D. Diffusion tensor imaging findings in post-concussion syndrome patients after mild traumatic brain injury: A systematic review. Front. Neurol 2016, 7, 156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rapp, P.E.; Curley, K.C. Is a diagnosis of “mild traumatic brain injury” a category mistake? J. Trauma Acute Care Surg. 2012, 73, S13–S23. [Google Scholar] [CrossRef] [Green Version]
- Sharp, D.J.; Jenkins, P.O. Concussion is confusing us all. Pract. Neurol. 2015, 15, 172–186. [Google Scholar] [CrossRef] [Green Version]
- Sivak, S.; Nosal, V.; Bittsansky, M.; Dluha, J.; Dobrota, D.; Kurca, E. Type and occurrence of serious complications in patients after mild traumatic brain injury. Bratisl. Lek. Listy 2016, 117, 22–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Major, B.P.; Rogers, M.A.; Pearce, A.J. Using transcranial magnetic stimulation to quantify electrophysiological changes following concussive brain injury: A systematic review. Clin. Exp. Pharmacol. Physiol. 2015, 42, 394–405. [Google Scholar] [CrossRef]
- Barkhoudarian, G.; Hovda, D.A.; Giza, C.C. The molecular pathophysiology of concussive brain injury—An update. Phys. Med. Rehabil. Clin. N. Am. 2016, 27, 373–393. [Google Scholar] [CrossRef]
- Bonfante, E.; Riascos, R.; Arevalo, O. Imaging of chronic concussion. Neuroimaging Clin. N. Am. 2018, 28, 127–135. [Google Scholar] [CrossRef]
- Raji, C.A.; Henderson, T.A. PET and single-photon emission computed tomography in brain concussion. Neuroimaging Clin. N. Am. 2018, 28, 67–82. [Google Scholar] [CrossRef]
- Adams, J.H.; Doyle, D.; Ford, I.; Gennarelli, T.A.; Graham, D.I.; McLellan, D.R. Diffuse axonal injury in head injury: Definition, diagnosis and grading. Histopathology 1989, 15, 49–59. [Google Scholar] [CrossRef]
- Johnson, V.E.; Stewart, W.; Smith, D.H. Axonal pathology in traumatic brain injury. Exp. Neurol. 2013, 246, 35–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maxwell, W.L.; Povlishock, J.T.; Graham, D.L. A mechanistic analysis of nondisruptive axonal injury: A review. J. Neurotrauma 1997, 14, 419–440. [Google Scholar] [CrossRef] [PubMed]
- Mac Donald, C.L.; Dikranian, K.; Song, S.K.; Bayly, P.V.; Holtzman, D.M.; Brody, D.L. Detection of traumatic axonal injury with diffusion tensor imaging in a mouse model of traumatic brain injury. Exp. Neurol. 2007, 205, 116–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mac Donald, C.L.; Dikranian, K.; Bayly, P.; Holtzman, D.; Brody, D. Diffusion tensor imaging reliably detects experimental traumatic axonal injury and indicates approximate time of injury. J. Neurosci. 2007, 27, 11869–11876. [Google Scholar] [CrossRef]
- Bennett, R.E.; Mac Donald, C.L.; Brody, D.L. Diffusion tensor imaging detects axonal injury in a mouse model of repetitive closed-skull traumatic brain injury. Neurosci. Lett. 2012, 513, 160–165. [Google Scholar] [CrossRef] [Green Version]
- Li, S.; Sun, Y.; Shan, D.; Feng, B.; Xing, J.; Duan, Y.; Dai, J.; Lei, H.; Zhou, Y. Temporal profiles of axonal injury following impact acceleration traumatic brain injury in rats—A comparative study with diffusion tensor imaging and morphological analysis. Int. J. Legal. Med. 2013, 127, 159–167. [Google Scholar] [CrossRef]
- Tu, T.W.; Lescher, J.D.; Williams, R.A.; Jikaria, N.; Turtzo, L.C.; Frank, J.A. Abnormal injury response in spontaneous mild ventriculomegaly wistar rat brains: A pathological correlation study of diffusion tensor and magnetization transfer imaging in mild traumatic brain injury. J. Neurotrauma 2017, 34, 248–256. [Google Scholar] [CrossRef] [Green Version]
- Jang, S.H. A review of corticospinal tract location at corona radiata and posterior limb of the internal capsule in human brain. Neuro Rehabil. 2009, 24, 279–283. [Google Scholar] [CrossRef]
- Seo, J.P.; Kwon, Y.H.; Jang, S.H. Mini-review of studies reporting the repeatability and reproducibility of diffusion tensor imaging. Investig. Magn. Reason. Imaging 2019, 23, 26–33. [Google Scholar] [CrossRef]
- Rajesh, A.; Cooke, G.E.; Monti, J.M.; Jahn, A.; Daugherty, A.M.; Cohen, N.J.; Kramer, A.F. Differences in Brain Architecture in Remote Mild Traumatic Brain Injury. J. Neurotrauma 2017, 34, 3280–3287. [Google Scholar] [CrossRef]
| Patho-Anatomy | |||
| Diffuse | Focal | ||
| Concussion | Contusion | ||
| Traumatic axonal injury/diffuse axonal injury | Penetrating | ||
| Blast | Hematoma | ||
| Abusive head trauma | Epidural | ||
| Subarachnoid | |||
| Subdural | |||
| Intraventricular | |||
| Intracerebral | |||
| Severity of head trauma | LOC | PTA | GCS |
| Mild: | ≤30 min | ≤24 h | 13~15 |
| Moderate: | >30 min, ≤24 h | >24 h, ≤7 days | 9~12 |
| Severe: | >24 h | >7 days | 3~8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jang, S.H.; Byun, D.H. Hidden Truth in Cerebral Concussion—Traumatic Axonal Injury: A Narrative Mini-Review. Healthcare 2022, 10, 931. https://doi.org/10.3390/healthcare10050931
Jang SH, Byun DH. Hidden Truth in Cerebral Concussion—Traumatic Axonal Injury: A Narrative Mini-Review. Healthcare. 2022; 10(5):931. https://doi.org/10.3390/healthcare10050931
Chicago/Turabian StyleJang, Sung Ho, and Dong Hyun Byun. 2022. "Hidden Truth in Cerebral Concussion—Traumatic Axonal Injury: A Narrative Mini-Review" Healthcare 10, no. 5: 931. https://doi.org/10.3390/healthcare10050931
APA StyleJang, S. H., & Byun, D. H. (2022). Hidden Truth in Cerebral Concussion—Traumatic Axonal Injury: A Narrative Mini-Review. Healthcare, 10(5), 931. https://doi.org/10.3390/healthcare10050931






