Compliance Surveillance of the Tobacco Control Legislation in a Spanish Region and Characterization of Passive Exposure to Tobacco Smoke and E-Cig in Children in Outdoor Spaces
Abstract
1. Introduction
2. Materials and Methods
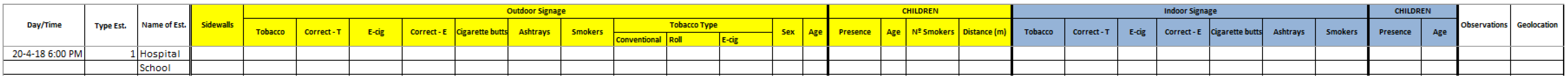
2.1. Study Design and Data Collection
2.2. Study Variables
2.3. Statistical Analyses
3. Results
4. Discussion
4.1. Main Finding of This Study
4.2. What Is Already Known on This Topic
4.3. What This Study Adds
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix B

References
- U.S. Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General; Centre for Disease Control and Prevention: Atlanta, GA, USA, 2006. Available online: https://pubmed.ncbi.nlm.nih.gov/20669524/ (accessed on 10 April 2022).
- Díez-Izquierdo, A.; Balaguer, A.; Lidón-Moyano, C.; Martín-Sánchez, J.C.; Galán, I.; Fernández, E.; Martínez-Sánchez, J.M. Correlation between Tobacco Control Policies and Preterm Births and Low Birth Weight in Europe. Environ. Res. 2018, 160, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Faber, T.; Been, J.V.; Reiss, I.K.; MacKenbach, J.P.; Sheikh, A. Smoke-Free Legislation and Child Health. NPJ Prim. Care Respir. Med. 2016, 26, 16067. [Google Scholar] [CrossRef] [PubMed]
- Ciaccio, C.E.; Gurley-Calvez, T.; Shireman, T.I. Indoor Tobacco Legislation Is Associated with Fewer Emergency Department Visits for Asthma Exacerbation in Children. Ann. Allergy Asthma Immunol. 2016, 117, 641–645. [Google Scholar] [CrossRef] [PubMed]
- Moser, D.K.; Burkhart, P.V.; Mannino, D.; Hahn, E.J.; Zhang, M.; Lee, S.; Rayens, M.K. Reduction in Asthma-Related Emergency Department Visits after Implementation of a Smoke-Free Law. J. Allergy Clin. Immunol. 2008, 122, 537–541. [Google Scholar]
- Been, J.V.; Nurmatov, U.B.; Cox, B.; Nawrot, T.S.; Van Schayck, C.P.; Sheikh, A. Effect of Smoke-Free Legislation on Perinatal and Child Health: A Systematic Review and Meta-Analysis. Lancet 2014, 383, 1549–1560. [Google Scholar] [CrossRef]
- Mackay, D.F.; Nelson, S.M.; Haw, S.J.; Pell, J.P. Impact of Scotland’s Smoke-Free Legislation on Pregnancy Complications: Retrospective Cohort Study. PLoS Med. 2012, 9, e1001175. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.L.; Wong, W.H.S.; Lau, Y.L. Smoke-Free Legislation Reduces Hospital Admissions for Childhood Lower Respiratory Tract Infection. Tob. Control 2016, 25, e90–e94. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Report on the Global Tobacco Epidemic, 2017; World Health Organization: Geneva, Switzerland, 2017; Licence: CCentre C BY-NC-SA 3.0 IGO. [Google Scholar]
- World Health Organization. WHO Report on the Global Tobacco Epidemic, Six Policies to Reverse the Tobacco Epidemic; World Health Organization: Geneva, Switzerland, 2008; pp. 23–41. Available online: http://www.who.int/tobacco/mpower/mpower_report_six_policies_2008.pdf (accessed on 1 April 2021).
- World Health Organisation. WHO Framework Convention on Tobacco Control; WHO Press: Geneva, Switzerland, 2005; Volume 1, pp. 270–271. [Google Scholar] [CrossRef]
- Gobierno de España. Ley 42/2010, de 30 de Diciembre, por la que se Modifica la Ley 28/2005, de 26 de Diciembre, de Medidas Sanitarias Frente al Tabaquismo y Reguladora de la Venta, el Suministro, el Consumo y la Publicidad de Los Productos del Tabaco; Boletín Oficial Del Estado (BOE), Gobierno de España: Madrid, España, 2010; BOE-A-2012-5403.
- Gobierno de España. Ley 28/2005, de 26 de Diciembre, de Medidas Sanitarias Frente Al Tabaquismo y Reguladora de La Venta, El Suministro, El Consumo y La Publicidad de Los Productos Del Tabaco; Boletín Oficial Del Estado (BOE), Gobierno de España: Madrid, España, 2005; Volume 309.
- Alavanja, M.; Baron, J.A.; Brownson, R.C.; Buffler, P.A.; DeMarini, D.M.; Djordjevic, M.V.; Doll, R.; Fontham ET, H.; Gao, Y.T.; Gray, N.; et al. Tobacco smoke and involuntary smoking. In IARC Monographs on the Evaluation of Carcinogenic Risks to Humans; IARC: Lyon, France, 2004; Volume 83, pp. 1–1413. ISBN 9283212835. Available online: http://monographs.iarc.fr/ENG/Monographs/vol83/index.php (accessed on 10 April 2022).
- Grupo de Trabajo sobre Tabaquismo de la Sociedad Española de Epidemiología. Evaluación de Las Políticas de Control Del Tabaquismo En España (Leyes 28/2005 y 42/2010) Revisión de La Evidencia. 2017. Available online: http://seepidemiologia.es/documents/dummy/MONOGRAFIA.pdf (accessed on 10 April 2022).
- Gobierno de España. Real Decreto 579/2017, de 9 de Junio, Por El Que Se Regulan Determinados Aspectos Relativos a La Fabricación, Presentación y Comercialización de Los Productos Del Tabaco y Los Productos Relacionados; Boletín Oficial Del Estado (BOE): Madrid, España, 2017.
- Sureda, X.; Martínez-Sánchez, J.M.; López, M.J.; Fu, M.; Agüero, F.; Saltó, E.; Nebot, M.; Fernández, E. Secondhand Smoke Levels in Public Building Main Entrances: Outdoor and Indoor PM2.5 Assessment. Tob. Control 2012, 21, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Matilla-Santander, N.; Fu, M.; Ballbè, M.; Bunch, K.; Lidón-Moyano, C.; Martín-Sánchez, J.C.; Fernández, E.; Martínez-Sánchez, J.M. Use of Electronic Cigarettes in Public and Private Settings in Barcelona (Spain). Environ. Res. 2017, 158, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Gobierno de España. Ley 3/2014, de 27 de Marzo, Por La Que Se Modifica El Texto Refundido de La Ley General Para La Defensa de Los Consumidores y Usuarios y Otras Leyes Complementarias, Aprobado Por El Real Decreto Legislativo 1/2007, de 16 de Noviembre; Boletin Oficial del Estado (BOE): Madrid, España, 2014.
- US Surgeon General. Surgeon General’s Advisory on E-Cigarette Use Among Youth the E-Cigarette Epidemic Among Youth E-Cigarettes Come in Many Shapes and Sizes You Can Take Action. 2018; pp. 2–5. Available online: https://e-cigarettes.surgeongeneral.gov/documents/surgeon-generals-advisory-on-e-cigarette-use-among-youth-2018.pdf (accessed on 10 April 2022).
- Martínez-Sánchez, J.M.; Curto, A.; Fernández, E. Agreement between two observers in the measurement of smoking and use of safety belt and cell phones in vehicles. Gac. Sanit. 2012, 26, 91–93. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ajuntament de Sant Cugat. Guia Urbana de Sant Cugat. 2019. Available online: https://geo.santcugat.cat/santcugat/visor-guia.jsp (accessed on 10 April 2022).
- Xarxa Catalana d’Hospitals sense Fum. Recintes Sanitaris Sense Fum. 2010. Available online: https://www.xchsf.cat/docs/159-AccionsXarxa_1.1.pdf (accessed on 10 April 2022).
- Ministerio de Sanidad, Consumo y Bienestar Social. Señalización. 2019. Available online: https://www.mscbs.gob.es/ciudadanos/proteccionSalud/tabaco/senalizacion.htm (accessed on 10 April 2022).
- Gencat. Retolació per Descarregar. Canal Salut. 2018. Available online: http://canalsalut.gencat.cat/ca/salut-a-z/t/tabac/tabac/retolacio-per-descarregar/ (accessed on 10 April 2022).
- Vardavas, C.; Agaku, I.; Patelarou, E.; Anagnostopoulos, N.; Nakou, C.; Dramba, V.; Giourgouli, G.; Argyropoulou, P.; Antoniadis, A.; Gourgoulianis, K.; et al. Ashtrays and Signage as Determinants of a Smoke-Free Legislation’s Success. PLoS ONE 2013, 8, e72945. [Google Scholar] [CrossRef] [PubMed]
- Lidón-Moyano, C.; Martínez-Sánchez, J.M.; Fu, M.; Ballbè, M.; Martín-Sánchez, J.C.; Martínez, C.; Fernández, E. Secondhand Smoke Risk Perception and Smoke-Free Rules in Homes: A Cross-Sectional Study in Barcelona (Spain). BMJ Open 2017, 7, e014207. [Google Scholar] [CrossRef] [PubMed]
- Kruger, J.; Patel, R.; Kegler, M.; Babb, S.D.; King, B.A. Perceptions of Harm from Secondhand Smoke Exposure among U.S. Adults, 2009–2010. Tob. Induc. Dis. 2016, 14, 3. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho Ribeiro, F.A.; de Moraes, M.K.; de Morais Caixeta, J.C.; da Silva, J.N.; Sanches Lima, A.; Santana Parreira, S.L.; Silva Fernandes, V.L. Perception of Parents about Second Hand Smoke on the Health of Their Children: An Ethnographic Study. Rev. Paul. Pediatr. 2015, 33, 394–399. [Google Scholar] [PubMed]
- Campaign for Tobacco-Free Kids. Tobacco Control Laws. 2019. Available online: https://www.tobaccocontrollaws.org/ (accessed on 10 April 2022).
- Betevé. Campanya d’inspecció a Les Terrasses per Comprovar Si Es Compleix La Llei Antitabac. 2019. Available online: https://beteve.cat/basics/generalitat-inspeccions-terrasses-tabac/ (accessed on 10 April 2022).
- Euromonitor International. Smokeless Tobacco and Vapour Products. 2019. Available online: https://www.euromonitor.com/smokeless-tobacco-and-vapour-products (accessed on 1 April 2022).
- Mello, S.; Bigman, C.A.; Sanders-Jackson, A.; Tan, A. Perceived Harm of Secondhand Electronic Cigarette Vapors and Policy Support to Restrict Public Vaping: Results from a National Survey of US Adults. Nicotine Tob. Res. 2016, 18, 686–693. [Google Scholar] [CrossRef] [PubMed]
- Matt, G.E.; Quintana, P.J.E.; Zakarian, J.M.; Fortmann, A.L.; Chatfield, D.A.; Hoh, E.; Uribe, A.M.; Hovell, M.F. When Smokers Move out and Non-Smokers Move in: Residential Thirdhand Smoke Pollution and Exposure. Tob. Control 2011, 20, e1. [Google Scholar] [CrossRef] [PubMed]
- Díez-izquierdo, A.; Cassanello-Peñarroya, P.; Lidón-Moyano, C.; Matilla-Santander, N.; Balaguer, A.; Martínez-Sánchez, J.M. Update on Thirdhand Smoke: A Comprehensive Systematic Review. Environ. Res. 2018, 167, 341–371. [Google Scholar] [CrossRef] [PubMed]
- Sureda, X.; Fernández, E.; Martínez-Sánchez, J.M.; Fu, M.; López, M.J.; Martínez, C.; Saltó, E. Secondhand Smoke in Outdoor Settings: Smokers’ Consumption, Non-Smokers’ Perceptions, and Attitudes towards Smoke-Free Legislation in Spain. BMJ Open 2015, 5, e007554. [Google Scholar] [CrossRef] [PubMed]
- Díez-Izquierdo, A.; Lidón-Moyano, C.; Martín-Sánchez, J.C.; Matilla-Santander, N.; Cassanello-Peñarroya, P.; Balaguer; Martínez-Sánchez, J.M. Smoke-Free Homes and Attitudes towards Banning Smoking in Vehicles Carrying Children in Spain (2016). Environ. Res. 2017, 158, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Mackay, D.; Haw, S.; Ayres, J.G.; Fischbacher, C.; Pell, J.P. Smoke-Free Legislation and Hospitalizations for Childhood Asthma. N. Engl. J. Med. 2010, 363, 1139–1145. [Google Scholar] [CrossRef] [PubMed]
| Conventional Tobacco | Electronic Cigarettes | ||||||
|---|---|---|---|---|---|---|---|
| n | Signage | n | Correctness * | Signage | n | Correctness | |
| Total | 179 | 30.7% | 55 | 50.9% | 1.7% | 3 | 66.7% |
| Primary education | 25 | 20.0% | 5 | 40.0% | 0.0% | 0 | 0.0% |
| Secondary education | 17 | 17.7% | 3 | 33.3% | 0.0% | 0 | 0.0% |
| Hospitality venues | 111 | 28.8% | 32 | 46.9% | 0.9% | 1 | 0.0% |
| Healthcare facilities | 10 | 80.0% | 8 | 37.5% | 20.0% | 2 | 100.0% |
| Public administration | 12 | 0.0% | 0 | - | 0.0% | 0 | - |
| Transport | 9 | 55.6% | 5 | 100.0% | 0.0% | 0 | - |
| Hospitality Venues’ Terraces | Entrances of Educational Centres | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | All Terraces | p-Value | Terraces with Children (n = 39) | p-Value | Terraces without Children (n = 70) | p-Value | n | Total | p-Value | ||
| Total | 109 | 66.97% | - | 66.67% | - | 67.14% | - | 24 | 16.67% | - | |
| Age of the child | - | 1.000 1 | - | 1.000 2 | |||||||
| <1 year old | 15 | - | 66.67% | - | 4 | 0.00% | |||||
| 1–5 years old | 24 | - | 66.67% | - | 20 | 20.00% | |||||
| Conventional tobacco door signage | 0.433 1 | 1.000 1 | 0.354 2 | 1.000 2 | |||||||
| Yes | 31 | 74.19% | 68.75% | 80.00% | 5 | 20.00% | |||||
| No | 78 | 64.10% | 65.22% | 63.64% | 19 | 15.79% | |||||
| Correct signage * | 0.685 2 | 1.000 2 | 0.525 2 | 1.000 2 | |||||||
| Yes | 15 | 80.00% | 66.67% | 88.89% | 2 | 0.00% | |||||
| No | 16 | 68.75% | 70.00% | 66.67% | 3 | 33.33% | |||||
| Cigarette butts | 1.000 2 | 1.000 2 | 1.000 2 | 1.000 2 | |||||||
| Yes | 107 | 67.29% | 66.67% | 67.65% | 23 | 17.39% | |||||
| No | 2 | 50.00% | - | 50.00% | 1 | 0.00% | |||||
| Ashtrays | <0.001 1 | 0.008 2 | 0.002 1 | 1.000 2 | |||||||
| Yes | 76 | 80.26% | 81.48% | 79.59% | 0 | - | |||||
| No | 33 | 36.36% | 33.33% | 38.10% | 24 | 16.67% | |||||
| Type of terrace | 0.370 1 | 1.000 2 | 0.313 2 | - | |||||||
| With sidewalls | 22 | 77.27% | 70.00% | 83.33% | - | ||||||
| Without sidewalls | 87 | 64.37% | 65.52% | 63.79% | - | ||||||
| Time of day | 0.531 1 | 0.589 2 | 0.733 1 | 1.000 2 | |||||||
| Morning | 22 | 59.09% | 50.00% | 61.11% | 20 | 20.00% | |||||
| Afternoon | 87 | 68.97% | 68.57% | 69.23% | 4 | 0.00% | |||||
| Day of the week | 0.339 1 | 0.157 1 | 0.982 1 | - | |||||||
| Weekdays | 51 | 72.55% | 76.00% | 69.23% | - | ||||||
| Weekends | 58 | 62.07% | 50.00% | 65.91% | - | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jovell, L.; Díez-Izquierdo, A.; Martín-Sánchez, J.C.; Cartanyà-Hueso, À.; González-Marrón, A.; Lidón-Moyano, C.; Martínez-Sánchez, J.M. Compliance Surveillance of the Tobacco Control Legislation in a Spanish Region and Characterization of Passive Exposure to Tobacco Smoke and E-Cig in Children in Outdoor Spaces. Healthcare 2022, 10, 717. https://doi.org/10.3390/healthcare10040717
Jovell L, Díez-Izquierdo A, Martín-Sánchez JC, Cartanyà-Hueso À, González-Marrón A, Lidón-Moyano C, Martínez-Sánchez JM. Compliance Surveillance of the Tobacco Control Legislation in a Spanish Region and Characterization of Passive Exposure to Tobacco Smoke and E-Cig in Children in Outdoor Spaces. Healthcare. 2022; 10(4):717. https://doi.org/10.3390/healthcare10040717
Chicago/Turabian StyleJovell, Laura, Ana Díez-Izquierdo, Juan Carlos Martín-Sánchez, Àurea Cartanyà-Hueso, Adrián González-Marrón, Cristina Lidón-Moyano, and Jose M. Martínez-Sánchez. 2022. "Compliance Surveillance of the Tobacco Control Legislation in a Spanish Region and Characterization of Passive Exposure to Tobacco Smoke and E-Cig in Children in Outdoor Spaces" Healthcare 10, no. 4: 717. https://doi.org/10.3390/healthcare10040717
APA StyleJovell, L., Díez-Izquierdo, A., Martín-Sánchez, J. C., Cartanyà-Hueso, À., González-Marrón, A., Lidón-Moyano, C., & Martínez-Sánchez, J. M. (2022). Compliance Surveillance of the Tobacco Control Legislation in a Spanish Region and Characterization of Passive Exposure to Tobacco Smoke and E-Cig in Children in Outdoor Spaces. Healthcare, 10(4), 717. https://doi.org/10.3390/healthcare10040717








