Psychosocial and Behavioral Effects of the COVID-19 Pandemic on Children and Adolescents with Autism and Their Families: Overview of the Literature and Initial Data from a Multinational Online Survey
Abstract
:1. Introduction
2. Comprehensive Review of the Literature
2.1. Search Strategy
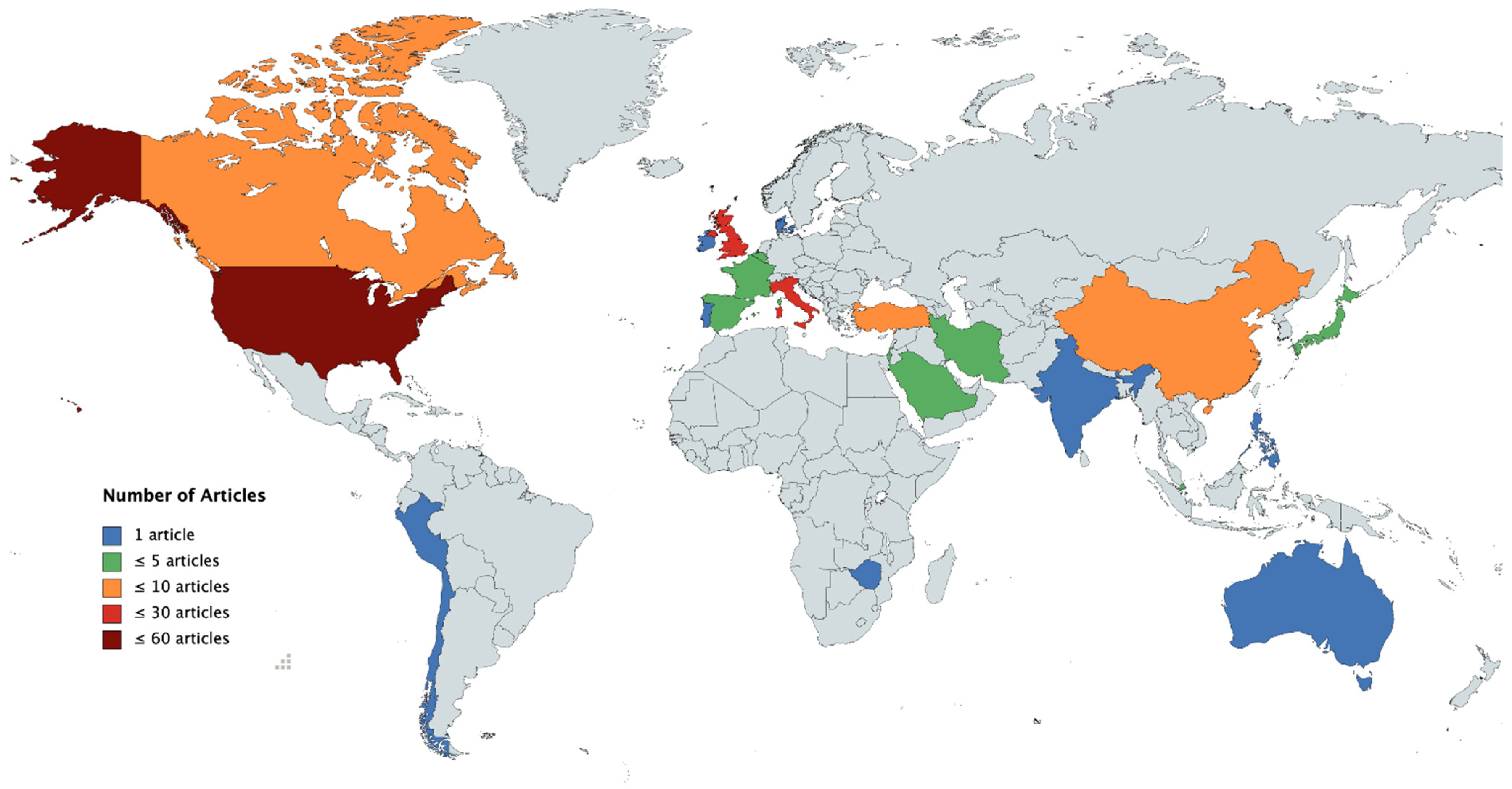
2.2. Regional and Temporal Factors
2.3. Well-Being of Parents, Caregivers, and Individuals with Autism
2.4. Schools, Home Schooling, Home Office, and Work Opportunities
2.5. Leisure Time, Physical Activities, Internet, and Social Media Use
2.6. Modulating Effects of Level of Functioning, Additional Intellectual Disabilities, and Other Developmental Disorders
2.7. Diagnosis and Intervention
2.7.1. Telehealth
2.7.2. Cognitive and Behavioral Methods
2.8. Further Topics of Interest
2.9. Summary of Reviewed Work
3. Online Survey
3.1. Materials
3.2. Participants
3.3. Data Analysis
3.4. Results
3.5. Summary and Discussion of the Online Survey Results
4. General Discussion
Outlook: The Importance of Social Interaction in the Face of the Pandemic
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rudert, S.C.; Gleibs, I.H.; Gollwitzer, M.; Häfner, M.; Hajek, K.V.; Harth, N.S.; Häusser, J.A.; Imhoff, R.; Schneider, D. Us and the virus: Understanding the COVID-19 pandemic through a social psychological lens. Eur. Psychol. 2021, 26, 259–271. [Google Scholar] [CrossRef]
- Van Bavel, J.J.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Willer, R. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef]
- Schneider, D.; Glaser, M.; Senju, A. Autism spectrum disorder. In Encyclopedia of Personality and Individual Differences; Zeigler-Hill, V., Shackelford, T.K., Eds.; Springer International: Cham, Switzerland, 2017; pp. 329–333. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Dsm-5; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- de Leeuw, A.; Happé, F.; Hoekstra, R.A. A conceptual framework for understanding the cultural and contextual factors on autism across the globe. Autism Res. 2020, 13, 1029–1050. [Google Scholar] [CrossRef] [Green Version]
- Narzisi, A. Handle the autism spectrum condition during coronavirus (COVID-19) stay at home period: Ten tips for helping parents and caregivers of young children. Brain Sci. 2020, 10, 207. [Google Scholar] [CrossRef] [Green Version]
- Wong, P.W.; Lam, Y.; Lau, J.S.; Fok, H. The resilience of social service providers and families of children with autism or development delays during the COVID-19 pandemic-a community case study in Hong Kong. Front. Psychiatry 2021, 11, 561657. [Google Scholar] [CrossRef]
- Gevarter, C.; Najar, A.M.; Flake, J.; Tapia-Alvidrez, F.; Lucero, A. Naturalistic communication training for early intervention providers and latinx parents of children with signs of autism. J. Dev. Phys. Disabil. 2021, 34, 147–169. [Google Scholar] [CrossRef]
- Wachtel, L.E. Far from an elective procedure electroconvulsive therapy and autism in the era of COVID-19. J. ECT 2021, 37, 10–12. [Google Scholar] [CrossRef]
- Jefsen, O.H.; Rohde, C.; Nørremark, B.; Østergaard, S.D. Editorial perspective: COVID-19 pandemic-related psychopathology in children and adolescents with mental illness. J. Child Psychol. Psychiatry Allied Discip. 2021, 62, 798–800. [Google Scholar] [CrossRef]
- Else, H. How a torrent of COVID science changed research publishing-in seven charts. Nature 2020, 588, 553. [Google Scholar] [CrossRef]
- Wang, C. The impact of COVID-19 on autism research: Reflections from china. Autism Res. 2020, 13, 1028. [Google Scholar] [CrossRef]
- Espinosa, D.F.; Metko, A.; Raimondi, M.; Impenna, M.; Scognamiglio, E. A model of support for families of children with autism living in the COVID-19 lockdown: Lessons from italy. Behav. Anal. Pract. 2020, 13, 550–558. [Google Scholar] [CrossRef]
- Nonweiler, J.; Rattray, F.; Baulcomb, J.; Happé, F.; Absoud, M. Prevalence and associated factors of emotional and behavioural difficulties during COVID-19 pandemic in children with neurodevelopmental disorders. Children 2020, 7, 128. [Google Scholar] [CrossRef]
- Jeste, S.; Hyde, C.; Distefano, C.; Halladay, A.; Ray, S.; Porath, M.; Wilson, R.B.; Thurm, A. Changes in access to educational and healthcare services for individuals with intellectual and developmental disabilities during COVID-19 restrictions. J. Intellect. Disabil. Res. 2020, 64, 825–833. [Google Scholar] [CrossRef]
- Beaumont, R.; Walker, H.; Weiss, J.; Sofronoff, K. Randomized controlled trial of a video gaming-based social skills program for children on the autism spectrum. J. Autism Dev. Disord. 2021, 51, 3637–3650. [Google Scholar] [CrossRef]
- Alhuzimi, T. Stress and emotional wellbeing of parents due to change in routine for children with autism spectrum disorder (asd) at home during COVID-19 pandemic in saudi arabia. Res. Dev. Disabil. 2021, 108, 103822. [Google Scholar] [CrossRef]
- Samadi, S.A.; Bakhshalizadeh-Moradi, S.; Khandani, F.; Foladgar, M.; Poursaid-Mohammad, M.; McConkey, R. Using hybrid telepractice for supporting parents of children with asd during the COVID-19 lockdown: A feasibility study in iran. Brain Sci. 2020, 10, 892. [Google Scholar] [CrossRef]
- Kawabe, K.; Hosokawa, R.; Nakachi, K.; Yoshino, A.; Horiuchi, F.; Ueno, S. Excessive and problematic internet use during the coronavirus disease 2019 school closure: Comparison between japanese youth with and without autism spectrum disorder. Front. Public Health 2020, 8, 609347. [Google Scholar] [CrossRef]
- Cahapay, M.B. How filipino parents home educate their children with autism during COVID-19 period. Int. J. Dev. Disabil. 2020, 1–4. [Google Scholar] [CrossRef]
- Majoko, T.; Dudu, A. Parents’ strategies for home educating their children with autism spectrum disorder during the COVID-19 period in zimbabwe. Int. J. Dev. Disabil. 2020, 1–5. [Google Scholar] [CrossRef]
- Echavarria-Ramirez, L.; Diaz-Reyes, D.V.; Narzisi, A. Autism spectrum disorder: Guidelines for management during the period of social isolation by coronavirus (COVID-19). Cuad. Neuropsicol.-Panam. J. Neuropsychol. 2020, 14, 35. [Google Scholar] [CrossRef]
- Oomen, D.; Nijhof, A.D.; Wiersema, J.R. The psychological impact of the COVID-19 pandemic on adults with autism: A survey study across three countries. Mol. Autism 2021, 12, 21. [Google Scholar] [CrossRef] [PubMed]
- Amaral, D.G.; de Vries, P.J. COVID-19 and autism research: Perspectives from around the globe. Autism Res. 2020, 13, 844–869. [Google Scholar] [CrossRef]
- Bellomo, T.R.; Prasad, S.; Munzer, T.; Laventhal, N. The impact of the COVID-19 pandemic on children with autism spectrum disorders. J. Pediatr. Rehabil. Med. 2020, 13, 349–354. [Google Scholar] [CrossRef]
- Courtenay, K.; Perera, B. COVID-19 and people with intellectual disability: Impacts of a pandemic. Ir. J. Psychol. Med. 2020, 37, 231–236. [Google Scholar] [CrossRef]
- Newbutt, N.; Schmidt, M.M.; Riva, G.; Schmidt, C. The possibility and importance of immersive technologies during COVID-19 for autistic people. J. Enabling Technol. 2020, 14, 187–199. [Google Scholar] [CrossRef]
- Colizzi, M.; Sironi, E.; Antonini, F.; Ciceri, M.L.; Bovo, C.; Zoccante, L. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: An online parent survey. Brain Sci. 2020, 10, 341. [Google Scholar] [CrossRef]
- Ren, J.; Li, X.K.; Chen, S.D.; Chen, S.Q.; Nie, Y.G. The influence of factors such as parenting stress and social support on the state anxiety in parents of special needs children during the COVID-19 epidemic. Front. Psychol. 2020, 11, 565393. [Google Scholar] [CrossRef]
- Chen, S.Q.; Chen, S.D.; Li, X.K.; Ren, J. Mental health of parents of special needs children in china during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 9519. [Google Scholar] [CrossRef]
- Manning, J.; Billian, J.; Matson, J.; Allen, C.; Soares, N. Perceptions of families of individuals with autism spectrum disorder during the COVID-19 crisis. J. Autism Dev. Disord. 2021, 51, 2920–2928. [Google Scholar] [CrossRef]
- Bentenuto, A.; Mazzoni, N.; Giannotti, M.; Venuti, P.; de Falco, S. Psychological impact of COVID-19 pandemic in italian families of children with neurodevelopmental disorders. Res. Dev. Disabil. 2021, 109, 103840. [Google Scholar] [CrossRef]
- Althiabi, Y. Attitude, anxiety and perceived mental health care needs among parents of children with autism spectrum disorder (asd) in saudi arabia during COVID-19 pandemic. Res. Dev. Disabil. 2021, 111, 103873. [Google Scholar] [CrossRef] [PubMed]
- Corbett, B.A.; Muscatello, R.A.; Klemencic, M.E.; Schwartzman, J.M. The impact of COVID-19 on stress, anxiety, and coping in youth with and without autism and their parents. Autism Res. 2021, 14, 1496–1511. [Google Scholar] [CrossRef] [PubMed]
- Amorim, R.; Catarino, S.; Miragaia, P.; Ferreras, C.; Viana, V.; Guardiano, M. The impact of COVID-19 on children with autism spectrum disorder. Rev. Neurol. 2020, 71, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Levante, A.; Petrocchi, S.; Bianco, F.; Castelli, I.; Colombi, C.; Keller, R.; Narzisi, A.; Masi, G.; Lecciso, F. Psychological impact of COVID-19 outbreak on families of children with autism spectrum disorder and typically developing peers: An online survey. Brain Sciences 2021, 11, 808. [Google Scholar] [CrossRef]
- Redquest, B.K.; Tint, A.; Ries, H.; Lunsky, Y. Exploring the experiences of siblings of adults with intellectual/developmental disabilities during the COVID-19 pandemic. J. Intellect. Disabil. Res. 2021, 65, 1–10. [Google Scholar] [CrossRef]
- Alyoubi, R.A.; Alofi, E.A. Experiences of parenting child with asd during COVID-19 pandemic: A cross-sectional study. Med. Sci. 2020, 24, 3972–3980. [Google Scholar]
- Mumbardo-Adam, C.; Barnet-Lopez, S.; Balboni, G. How have youth with autism spectrum disorder managed quarantine derived from COVID-19 pandemic? An approach to families perspectives. Res. Dev. Disabil. 2021, 110, 103860. [Google Scholar] [CrossRef]
- Meral, B.F. Parental views of families of children with autism spectrum disorder and developmental disorders during the COVID-19 pandemic. J. Autism Dev. Disord. 2022, 52, 1712–1724. [Google Scholar] [CrossRef]
- Neece, C.; McIntyre, L.L.; Fenning, R. Examining the impact of COVID-19 in ethnically diverse families with young children with intellectual and developmental disabilities. J. Intellect. Disabil. Res. 2020, 64, 739–749. [Google Scholar] [CrossRef]
- Asbury, K.; Fox, L.; Deniz, E.; Code, A.; Toseeb, U. How is COVID-19 affecting the mental health of children with special educational needs and disabilities and their families? J. Autism Dev. Disord. 2021, 51, 1772–1780. [Google Scholar] [CrossRef]
- Nunez, A.; le Roy, C.; Coelho-Medeiros, M.E.; Lopez-Espejo, M. Factors affecting the behavior of children with asd during the first outbreak of the COVID-19 pandemic. Neurol. Sci. 2021, 42, 1675–1678. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, K.; Clark, S.; McGrane, A.; Rock, N.; Burke, L.; Boyle, N.; Joksimovic, N.; Marshall, K. A qualitative study of child and adolescent mental health during the COVID-19 pandemic in ireland. Int. J. Environ. Res. Public Health 2021, 18, 1062. [Google Scholar] [CrossRef] [PubMed]
- Parenteau, C.I.; Bent, S.; Hendren, R.L.; Hossain, B.; Chen, Y.T.; Widjaja, F.; Breard, M. A qualitative analysis: The experience of parents of children with autism spectrum disorder during the COVID-19 pandemic. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, S251. [Google Scholar] [CrossRef]
- Mutluer, T.; Doenyas, C.; Genc, H.A. Behavioral implications of the COVID-19 process for autism spectrum disorder, and individuals’ comprehension of and reactions to the pandemic conditions. Front. Psychiatry 2020, 11, 561882. [Google Scholar] [CrossRef]
- Guller, B.; Yaylaci, F.; Eyuboglu, D. Those in the shadow of the pandemic: Impacts of the COVID-19 outbreak on the mental health of children with neurodevelopmental disorders and their parents. Int. J. Dev. Disabil. 2021, 1–13. [Google Scholar] [CrossRef]
- Huang, S.J.; Sun, T.; Zhu, Y.N.; Song, S.S.; Zhang, J.J.; Huang, L.J.; Chen, Q.; Peng, G.Y.; Zhao, D.M.; Yu, H.; et al. Impact of the COVID-19 pandemic on children with asd and their families: An online survey in china. Psychol. Res. Behav. Manag. 2021, 14, 289–297. [Google Scholar] [CrossRef]
- Berard, M.; Rattaz, C.; Peries, M.; Loubersac, J.; Munir, K.; Baghdadli, A. Impact of containment and mitigation measures on children and youth with asd during the COVID-19 pandemic: Report from the elena cohort. J. Psychiatr. Res. 2021, 137, 73–80. [Google Scholar] [CrossRef]
- Kawaoka, N.; Ohashi, K.; Fukuhara, S.; Miyachi, T.; Asai, T.; Imaeda, M.; Saitoh, S. Impact of school closures due to COVID-19 on children with neurodevelopmental disorders in japan. J. Autism Dev. Disord. 2021, 1–7. [Google Scholar] [CrossRef]
- Panda, P.K.; Gupta, J.; Chowdhury, S.R.; Kumar, R.; Meena, A.K.; Madaan, P.; Sharawat, I.K.; Gulati, S. Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: A systematic review and meta-analysis. J. Trop. Pediatr. 2021, 67, fmaa122. [Google Scholar] [CrossRef]
- Dondi, A.; Fetta, A.; Lenzi, J.; Morigi, F.; Candela, E.; Rocca, A.; Cordelli, D.M.; Lanari, M. Sleep disorders reveal distress among children and adolescents during the COVID-19 first wave: Results of a large web-based italian survey. Ital. J. Pediatr. 2021, 47, 130. [Google Scholar] [CrossRef]
- Cantiani, C.; Dondena, C.; Capelli, E.; Riboldi, E.M.; Molteni, M.; Riva, V. Effects of COVID-19 lockdown on the emotional and behavioral profiles of preschool italian children with and without familial risk for neurodevelopmental disorders. Brain Sci. 2021, 11, 477. [Google Scholar] [CrossRef]
- Siracusano, M.; Segatori, E.; Riccioni, A.; Gialloreti, L.E.; Curatolo, P.; Mazzone, L. The impact of COVID-19 on the adaptive functioning, behavioral problems, and repetitive behaviors of italian children with autism spectrum disorder: An observational study. Children 2021, 8, 96. [Google Scholar] [CrossRef]
- Davidson, C.J.; Lodge, K.; Kam, A. The impact of the COVID-19 pandemic on autistic adults—A survey. Adv. Autism 2021, 7, 311–321. [Google Scholar] [CrossRef]
- Adams, R.E.; Zheng, S.T.; Taylor, J.L.; Bishop, S.L. Ten weeks in: COVID-19-related distress in adults with autism spectrum disorder. Autism 2021, 25, 2140–2145. [Google Scholar] [CrossRef]
- Lugo-Marin, J.; Gisbert-Gustemps, L.; Setien-Ramos, I.; Espanol-Martin, G.; Ibanez-Jimenez, P.; Forner-Puntonet, M.; Arteaga-Henriquez, G.; Soriano-Dia, A.; Duque-Yemail, J.D.; Ramos-Quiroga, J.A. COVID-19 pandemic effects in people with autism spectrum disorder and their caregivers: Evaluation of social distancing and lockdown impact on mental health and general status. Res. Autism Spectr. Disord. 2021, 83, 101757. [Google Scholar] [CrossRef]
- White, L.C.; Law, J.K.; Daniels, A.M.; Toroney, J.; Vernoia, B.; Xiao, S.; The SPARK Consortium; Feliciano, P.; Chung, W.K. Brief report: Impact of COVID-19 on individuals with asd and their caregivers: A perspective from the spark cohort. J. Autism Dev. Disord. 2021, 51, 3766–3773. [Google Scholar] [CrossRef]
- White, S.W.; Stoppelbein, L.; Scott, H.; Spain, D. It took a pandemic: Perspectives on impact, stress, and telehealth from caregivers of people with autism. Res. Dev. Disabil. 2021, 113, 103938. [Google Scholar] [CrossRef]
- Crane, L.; Adu, F.; Arocas, F.; Carli, R.; Eccles, S.; Harris, S.; Jardine, J.; Phillips, C.; Piper, S.; Santi, L.; et al. Vulnerable and forgotten: The impact of the COVID-19 pandemic on autism special schools in england. Front. Educ. 2021, 6, 629203. [Google Scholar] [CrossRef]
- Stenhoff, D.M.; Pennington, R.C.; Tapp, M.C. Distance education support for students with autism spectrum disorder and complex needs during COVID-19 and school closures. Rural. Spec. Educ. Q. 2020, 39, 211–219. [Google Scholar] [CrossRef]
- Garcia, J.M.; Lawrence, S.; Brazendale, K.; Leahy, N.; Fukuda, D. Brief report: The impact of the COVID-19 pandemic on health behaviors in adolescents with autism spectrum disorder. Disabil. Health J. 2021, 14, 101021. [Google Scholar] [CrossRef]
- Broder-Fingert, S.; Brazauskas, K.; Lindgren, K.; Iannuzzi, D.; van Cleave, J. Prevalence of overweight and obesity in a large clinical sample of children with autism. Acad. Pediatr. 2014, 14, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.A.; Downing, K.; Rinehart, N.J.; Barnett, L.M.; May, T.; McGillivray, J.A.; Papadopoulos, N.V.; Skouteris, H.; Timperio, A.; Hinkley, T. Physical activity, sedentary behavior and their correlates in children with autism spectrum disorder: A systematic review. PLoS ONE 2017, 12, e0172482. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, B.; Brusilovskiy, E.; Hallock, T.; Salzer, M.; Davidson, A.P.; Slugg, L.; Feeley, C. Impact of COVID-19 on community participation and mobility in young adults with autism spectrum disorders. J. Autism Dev. Disord. 2022, 52, 1553–1567. [Google Scholar] [CrossRef] [PubMed]
- Yarımkaya, E.; Esentürk, O.K. The novel coronavirus (COVID-19) outbreak: Physical inactivity and children with autism spectrum disorders. Life Span Disabil. 2020, 23, 133–152. [Google Scholar]
- Yarımkaya, E.; Esentürk, O.K. Promoting physical activity for children with autism spectrum disorders during coronavirus outbreak: Benefits, strategies, and examples. Int. J. Dev. Disabil. 2020, 1–6. [Google Scholar] [CrossRef]
- Garcia, J.M.; Cathy, B.S.; Garcia, A.V.; Shurack, R.; Brazendale, K.; Leahy, N.; Fukuda, D.; Lawrence, S. Transition of a judo program from in-person to remote delivery during COVID-19 for youth with autism spectrum disorder. Adv. Neurodev. Disord. 2021, 5, 227–232. [Google Scholar] [CrossRef]
- Brondino, N.; Damiani, S.; Politi, P. Effective strategies for managing COVID-19 emergency restrictions for adults with severe asd in a daycare center in italy. Brain Sci. 2020, 10, 436. [Google Scholar] [CrossRef]
- Eshraghi, A.A.; Li, C.; Alessandri, M.; Messinger, D.S.; Eshraghi, R.S.; Mittal, R.; Armstrong, F.D. COVID-19: Overcoming the challenges faced by individuals with autism and their families. Lancet Psychiatry 2020, 7, 481–483. [Google Scholar] [CrossRef]
- Baron-Cohen, S.; Richler, J.; Bisarya, D.; Gurunathan, N.; Wheelwright, S. The systemizing quotient: An investigation of adults with asperger syndrome or high-functioning autism, and normal sex differences. Philos. Trans. R. Soc. London. Ser. B Biol. Sci. 2003, 358, 361–374. [Google Scholar] [CrossRef] [Green Version]
- Pennisi, P.; Tonacci, A.; Tartarisco, G.; Billeci, L.; Ruta, L.; Gangemi, S.; Pioggia, G. Autism and social robotics: A systematic review. Autism Res. 2016, 9, 165–183. [Google Scholar] [CrossRef]
- Kowallik, A.E.; Schweinberger, S.R. Sensor-based technology for social information processing in autism: A review. Sensors 2019, 19, 4787. [Google Scholar] [CrossRef] [Green Version]
- Reicher, D. Debate: Remote learning during COVID-19 for children with high functioning autism spectrum disorder. Child Adolesc. Ment. Health 2020, 25, 263–264. [Google Scholar] [CrossRef]
- O’Connor, R.C.; Wetherall, K.; Cleare, S.; McClelland, H.; Melson, A.J.; Niedzwiedz, C.L.; O’Carroll, R.E.; O’Connor, D.B.; Platt, S.; Scowcroft, E.; et al. The COVID-19 pandemic should be last orders for poor care of people with neurodevelopmental disorders. Br. J. Psychiatry 2021, 218, 326–333. [Google Scholar] [CrossRef]
- Rauf, B.; Sheikh, H.; Majid, H.; Roy, A.; Pathania, R. COVID-19-related prescribing challenge in intellectual disability. Bjpsych Open 2021, 7, e66. [Google Scholar] [CrossRef]
- Kawabe, K.; Hosokawa, R.; Nakachi, K.; Yoshino, A.; Horiuchi, F.; Ueno, S. Making a brochure about coronavirus disease (COVID-19) for children with autism spectrum disorder and their family members. Psychiatry Clin. Neurosci. 2020, 74, 498–499. [Google Scholar] [CrossRef]
- Sivaraman, M.; Virues-Ortega, J.; Roeyers, H. Telehealth mask wearing training for children with autism during the COVID-19 pandemic. J. Appl. Behav. Anal. 2021, 54, 70–86. [Google Scholar] [CrossRef]
- Wallis, K.E.; Mule, C.; Mittal, S.; Cerda, N.; Shaffer, R.; Scott, A.; Langkamp, D.; Augustyn, M.; Perrin, E.; Soares, N.; et al. Use of telehealth in fellowship-affiliated developmental behavioral pediatric practices during the COVID-19 pandemic. J. Dev. Behav. Pediatr. 2021, 42, 314–321. [Google Scholar] [CrossRef]
- Crockett, J.L.; Becraft, J.L.; Phillips, S.T.; Wakeman, M.; Cataldo, M.F. Rapid conversion from clinic to telehealth behavioral services during the COVID-19 pandemic. Behav. Anal. Pract. 2020, 13, 725–735. [Google Scholar] [CrossRef]
- Tohidast, S.A.; Mansuri, B.; Bagheri, R.; Azimi, H. Provision of speech-language pathology services for the treatment of speech and language disorders in children during the COVID-19 pandemic: Problems, concerns, and solutions. Int. J. Pediatric Otorhinolaryngol. 2020, 138, 110262. [Google Scholar] [CrossRef]
- Kalvin, C.B.; Jordan, R.P.; Rowley, S.N.; Weis, A.; Wood, K.S.; Wood, J.J.; Ibrahim, K.; Sukhodolsky, D.G. Conducting cbt for anxiety in children with autism spectrum disorder during COVID-19 pandemic. J. Autism Dev. Disord. 2021, 51, 4239–4247. [Google Scholar] [CrossRef]
- Rothman, K. Expanding: A case study exploring online work and relationship in one-to-one sessions in an adult learning disability service. Body Mov. Danc. Psychother. 2021, 16, 48–56. [Google Scholar] [CrossRef]
- Conti, E.; Chericoni, N.; Costanzo, V.; Lasala, R.; Mancini, A.; Prosperi, M.; Tancredi, R.; Muratori, F.; Calderoni, S.; Apicella, F. Moving toward telehealth surveillance services for toddlers at risk for autism during the COVID-19 pandemic. Front. Psychiatry 2020, 11, 565999. [Google Scholar] [CrossRef]
- Wagner, L.; Corona, L.L.; Weitlauf, A.S.; Marsh, K.L.; Berman, A.F.; Broderick, N.A.; Warren, Z. Use of the tele-asd-peds for autism evaluations in response to COVID-19: Preliminary outcomes and clinician acceptability. J. Autism Dev. Disord. 2020, 51, 3063–3072. [Google Scholar] [CrossRef]
- Wagner, L.; Weitlauf, A.S.; Hine, J.; Corona, L.L.; Berman, A.F.; Nicholson, A.; Allen, W.; Black, M.; Warren, Z. Transitioning to telemedicine during COVID-19: Impact on perceptions and use of telemedicine procedures for the diagnosis of autism in toddlers. J. Autism Dev. Disord. 2021, 1–11. [Google Scholar] [CrossRef]
- Berger, N.I.; Wainer, A.L.; Kuhn, J.; Bearss, K.; Attar, S.; Carter, A.S.; Ibanez, L.V.; Ingersoll, B.R.; Neiderman, H.; Scott, S.; et al. Characterizing available tools for synchronous virtual assessment of toddlers with suspected autism spectrum disorder: A brief report. J. Autism Dev. Disord. 2021, 52, 423–434. [Google Scholar] [CrossRef]
- Narzisi, A. Phase 2 and later of COVID-19 lockdown: Is it possible to perform remote diagnosis and intervention for autism spectrum disorder? An online-mediated approach. J. Clin. Med. 2020, 9, 1850. [Google Scholar] [CrossRef]
- Summers, J.; Baribeau, D.; Mockford, M.; Goldhopf, L.; Ambrozewicz, P.; Szatmari, P.; Vorstman, J. Supporting children with neurodevelopmental disorders during the COVID-19 pandemic. J. Am. Acad. Child Adolesc. Psychiatry 2021, 60, 2–6. [Google Scholar] [CrossRef]
- Loman, M.; Vogt, E.; Miller, L.; Landsman, R.; Duong, P.; Kasten, J.; DeFrancisco, D.; Koop, J.; Heffelfinger, A. How to operate a pediatric neuropsychology practice during the COVID-19 pandemic: Real tips from one practice’s experience. Child Neuropsychol. 2021, 27, 251–279. [Google Scholar] [CrossRef]
- Eapen, V.; Hiscock, H.; Williams, K. Adaptive innovations to provide services to children with developmental disabilities during the COVID-19 pandemic. J. Paediatr. Child Health 2021, 57, 9–11. [Google Scholar] [CrossRef]
- Ameis, S.H.; Lai, M.C.; Mulsant, B.H.; Szatmari, P. Coping, fostering resilience, and driving care innovation for autistic people and their families during the COVID-19 pandemic and beyond. Mol. Autism 2020, 11, 61. [Google Scholar] [CrossRef]
- Franz, L.; Howard, J.; Viljoen, M.; Sikich, L.; Chandrasekhar, T.; Kollins, S.H.; Lee, L.; Ndlovu, M.; Sabatos-DeVito, M.; Seris, N.; et al. Pragmatic adaptations of telehealth-delivered caregiver coaching for children with autism in the context of COVID-19: Perspectives from the united states and south africa. Autism 2021, 26, 270–275. [Google Scholar] [CrossRef]
- Adamou, M.; Jones, S.L.; Fullen, T.; Galab, N.; Abbott, K.; Yasmeen, S. Remote assessment in adults with autism or adhd: A service user satisfaction survey. PLoS ONE 2021, 16, e0249237. [Google Scholar] [CrossRef]
- Nadler, C.; Godwin, D.L.; Dempsey, J.; Nyp, S.S. Autism and access to care during the COVID-19 crisis. J. Dev. Behav. Pediatr. 2021, 42, 73–75. [Google Scholar] [CrossRef]
- Kowanda, M.; Cartner, L.; Kentros, C.; Geltzeiler, A.R.; Singer, K.E.; Weaver, W.C.; Lehman, C.D.; Smith, S.; Smith, R.S.; Walsh, L.K.; et al. Availability of services and caregiver burden: Supporting individuals with neurogenetic conditions during the COVID-19 pandemic. J. Child Neurol. 2021, 36, 760–767. [Google Scholar] [CrossRef]
- Joseph, B.; Kearney, K.B.; Brady, M.P.; Downey, A.; Torres, A. Teaching small talk: Increasing on-topic conversational exchanges in college students with intellectual and developmental disabilities using remote audio coaching. Behav. Modif. 2021, 45, 251–271. [Google Scholar] [CrossRef]
- Cihon, J.H.; Ferguson, J.L.; Lee, M.; Leaf, J.B.; Leaf, R.; McEachin, J. Evaluating the cool versus not cool procedure via telehealth. Behav. Anal. Pract. 2021, 15, 260–268. [Google Scholar] [CrossRef]
- Su, W.C.; Srinivasan, S.; Cleffi, C.; Bhat, A. Short report on research trends during the COVID-19 pandemic and use of telehealth interventions and remote brain research in children with autism spectrum disorder. Autism 2021, 25, 1816–1822. [Google Scholar] [CrossRef]
- McDevitt, S.E. While quarantined: An online parent education and training model for families of children with autism in china. Res. Dev. Disabil. 2021, 109, 103851. [Google Scholar] [CrossRef]
- Gerow, S.; Radhakrishnan, S.; Akers, J.S.; McGinnis, K.; Swensson, R. Telehealth parent coaching to improve daily living skills for children with asd. J. Appl. Behav. Anal. 2021, 54, 566–581. [Google Scholar] [CrossRef]
- Drozdowicz, L.; Gordon, E.; Shapiro, D.; Jacobson, S.; Zalpuri, I.; Stewart, C.; Lewis, A.L.; Robinson, L.; Myint, M.T.; Daniolos, P.; et al. Sexual health in child and adolescent psychiatry: Multi-site implementation through synchronized videoconferencing of an educational resource using standardized patients. Front. Psychiatry 2020, 11, 593101. [Google Scholar] [CrossRef]
- Cox, D.J.; Plavnick, J.B.; Brodhead, M.T. A proposed process for risk mitigation during the COVID-19 pandemic. Behav. Anal. Pract. 2020, 13, 299–305. [Google Scholar] [CrossRef] [Green Version]
- Kornack, J.; Williams, A.L.; Johnson, K.A.; Mendes, E.M. Reopening the doors to center-based aba services: Clinical and safety protocols during COVID-19. Behav. Anal. Pract. 2020, 13, 543–549. [Google Scholar] [CrossRef]
- Rodriguez, K. Maintaining treatment integrity in the face of crisis: A treatment selection model for transitioning direct aba services to telehealth. Behav. Anal. Pract. 2020, 13, 291–298. [Google Scholar] [CrossRef]
- Colombo, R.A.; Wallace, M.; Taylor, R. An essential service decision model for aba providers during crisis. Behav. Anal. Pract. 2020, 13, 306–311. [Google Scholar] [CrossRef]
- Schieltz, K.M.; Wacker, D.P. Functional assessment and function-based treatment delivered via telehealth: A brief summary. J. Appl. Behav. Anal. 2020, 53, 1242–1258. [Google Scholar] [CrossRef]
- Sergi, L.; Mingione, E.; Ricci, M.C.; Cavallaro, A.; Russo, F.; Corrivetti, G.; Operto, F.F.; Frolli, A. Autism, therapy and COVID-19. Pediatr. Rep. 2021, 13, 35–44. [Google Scholar] [CrossRef]
- Yi, Z.H.; Dixon, M.R. Developing and enhancing adherence to a telehealth aba parent training curriculum for caregivers of children with autism. Behav. Anal. Pract. 2021, 14, 58–74. [Google Scholar] [CrossRef]
- Belisle, J.; Burke, R.; Clark, L.; Jepsen, R.; Welch, K.; Dennis, L.; McDonald, N. Developing remote delivery of language and cognitive training for use with children with autism: A technological report. Behav. Anal. Pract. 2021, 14, 434–444. [Google Scholar] [CrossRef]
- Corona, L.L.; Weitlauf, A.S.; Hine, J.; Berman, A.; Miceli, A.; Nicholson, A.; Stone, C.; Broderick, N.; Francis, S.; Juárez, A.P. Parent perceptions of caregiver-mediated telemedicine tools for assessing autism risk in toddlers. J. Autism Dev. Disord. 2020, 51, 476–486. [Google Scholar] [CrossRef]
- Pollard, J.S.; LeBlanc, L.A.; Griffin, C.A.; Baker, J.M. The effects of transition to technician-delivered telehealth aba treatment during the COVID-19 crisis: A preliminary analysis. J. Appl. Behav. Anal. 2021, 54, 87–102. [Google Scholar] [CrossRef]
- Szabo, T.G.; Richling, S.; Embry, D.D.; Biglan, A.; Wilson, K.G. From helpless to hero: Promoting values-based behavior and positive family interaction in the midst of COVID-19. Behav. Anal. Pract. 2020, 13, 568–576. [Google Scholar] [CrossRef] [PubMed]
- Saline, S. Thriving in the new normal: How COVID-19 has affected alternative learners and their families and implementing effective, creative therapeutic interventions. Smith Coll. Stud. Soc. Work 2021, 91, 1–28. [Google Scholar] [CrossRef]
- Tarbox, C.M.; Silverman, E.A.; Chastain, A.N.; Little, A.; Bermudez, T.L.; Tarbox, J. Taking action: 18 simple strategies for supporting children with autism during the COVID-19 pandemic. Behav. Anal. Pract. 2020, 14, 1099–1127. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.N.; Lancioni, G.E.; Medvedev, O.N.; Hwang, Y.S.; Myers, R.E. Real-time telehealth treatment team consultation for self-injury by individuals with autism spectrum disorder. Adv. Neurodev. Disord. 2021, 5, 170–182. [Google Scholar] [CrossRef]
- Baghdadli, A.; Picot, M.C.; Miot, S.; Munir, K. A call to action to implement effective COVID-19 prevention and screening of individuals with severe intellectual developmental and autism spectrum disorders. J. Autism Dev. Disord. 2021, 51, 2566–2568. [Google Scholar] [CrossRef] [PubMed]
- Turkoglu, S.; Ucar, H.N.; Cetin, F.H.; Guler, H.A.; Tezcan, M.E. The relationship between chronotype, sleep, and autism symptom severity in children with asd in COVID-19 home confinement period. Chronobiol. Int. 2020, 37, 1207–1213. [Google Scholar] [CrossRef]
- Cohen, D. Appreciating COVID-19 as a child and adolescent psychiatrist on the move. Enceph.-Rev. Psychiatr. Clin. Biol. Ther. 2020, 46, S99–S106. [Google Scholar] [CrossRef]
- Nollace, L.; Cravero, C.; Abbou, A.; Mazda-Walter, B.; Bleibtreu, A.; Pereirra, N.; Sainte-Marie, M.; Cohen, D.; Giannitelli, M. Autism and COVID-19: A case series in a neurodevelopmental unit. J. Clin. Med. 2020, 9, 2937. [Google Scholar] [CrossRef]
- Schmidt, B.; Schneider, J.; Deffner, T.; Rosendahl, J. Hypnotic suggestions of safety improve well-being in non-invasively ventilated patients in the intensive care unit. Intensive Care Med. 2021, 47, 485–486. [Google Scholar] [CrossRef]
- Oakley, B.; Tillmann, J.; Ruigrok, A.; Baranger, A.; Takow, C.; Charman, T.; Jones, E.; Cusack, J.; Doherty, M.; Violland, P.; et al. COVID-19 health and social care access for autistic people: European policy review. Br. Med. J. Open 2021, 11, e045341. [Google Scholar] [CrossRef]
- Warmate, Z.; Eldaly, M.K.; Elamer, A.A. Offering flexible working opportunities to people with mental disabilities: The missing link between sustainable development goals and financial implications. Bus. Strategy Environ. 2021, 30, 1563–1579. [Google Scholar] [CrossRef]
- Goldfarb, Y.; Gal, E.; Golan, O. Implications of employment changes caused by COVID-19 on mental health and work-related psychological need satisfaction of autistic employees: A mixed-methods longitudinal study. J. Autism Dev. Disord. 2021, 52, 89–102. [Google Scholar] [CrossRef] [PubMed]
- Leiner, D.J. Sosci Survey (Version 3.2.21) [Computer Software]. Available online: https://www.soscisurvey.de (accessed on 1 December 2019).
- Allison, C.; Auyeung, B.; Baron-Cohen, S. Toward brief red flags for autism screening: The short autism spectrum quotient and the short quantitative checklist in 1000 cases and 3000 controls. J. Am. Acad. Child Adolesc. Psychiatry 2012, 51, 202–212.e7. [Google Scholar] [CrossRef] [PubMed]
- Varni, J.W.; Seid, M.; Kurtin, P.S. Pedsql™ 4.0: Reliability and validity of the pediatric quality of life inventory version 4.0 generic core scales in healthy and patient populations. Med. Care 2001, 39, 800–812. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using g*power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Sosnowy, C.; Silverman, C.; Shattuck, P.; Garfield, T. Setbacks and successes: How young adults on the autism spectrum seek friendship. Autism Adulthood 2019, 1, 44–51. [Google Scholar] [CrossRef] [Green Version]
- Gori, M.; Schiatti, L.; Amadeo, M.B. Masking emotions: Face masks impair how we read emotions. Front. Psychol. 2021, 12, 669432. [Google Scholar] [CrossRef]
- Halbur, M.; Kodak, T.; McKee, M.; Carroll, R.; Preas, E.; Reidy, J.; Cordeiro, M.C. Tolerance of face coverings for children with autism spectrum disorder. J. Appl. Behav. Anal. 2021, 54, 600–617. [Google Scholar] [CrossRef]
- Bzdok, D.; Dunbar, R.I.M. The neurobiology of social distance. Trends Cogn. Sci. 2020, 24, 717–733. [Google Scholar] [CrossRef]
- Bailenson, J.N. Nonverbal overload: A theoretical argument for the causes of zoom fatigue. Technol. Mind Behav. 2021, 2. [Google Scholar] [CrossRef]
- Young, A.W.; Frühholz, S.; Schweinberger, S.R. Face and voice perception: Understanding commonalities and differences. Trends Cogn. Sci. 2020, 24, 398–410. [Google Scholar] [CrossRef] [PubMed]
- Hari, R.; Henriksson, L.; Malinen, S.; Parkkonen, L. Centrality of social interaction in human brain function. Neuron 2015, 88, 181–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunbar, R.I.M.; Shultz, S. Evolution in the social brain. Science 2007, 317, 1344–1347. [Google Scholar] [CrossRef] [Green Version]
- Uljarevic, M.; Hamilton, A. Recognition of emotions in autism: A formal meta-analysis. J. Autism Dev. Disord. 2013, 43, 1517–1526. [Google Scholar] [CrossRef] [PubMed]
- Chevallier, C.; Kohls, G.; Troiani, V.; Brodkin, E.S.; Schultz, R.T. The social motivation theory of autism. Trends Cogn. Sci. 2012, 16, 231–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jaswal, V.K.; Akhtar, N. Being versus appearing socially uninterested: Challenging assumptions about social motivation in autism. Behav. Brain Sci. 2019, 42, E82. [Google Scholar] [CrossRef] [Green Version]
- Mitchell, P.; Sheppard, E.; Cassidy, S. Autism and the double empathy problem: Implications for development and mental health. Br. J. Dev. Psychol. 2021, 39, 1–18. [Google Scholar] [CrossRef]
| Comparison | Sub-Group of Children | General Well-Being | Adaptation Abilities | Overall Anxiety Levels | Emotional Reactions | Social Behavior |
|---|---|---|---|---|---|---|
| Within-family reports (n = 43) | Autistic sibling | −0.40 (1.12) | −0.74 (1.18) | +0.44 (0.91) | −0.09 (1.23) | −0.58 (1.22) |
| Neurotypical sibling | −0.44 (0.93) | −0.19 (0.91) | +0.47 (0.77) | +0.05 (1.0) | −0.26 (1.11) | |
| Paired t-tests | t(42) = 0.323, p = 0.743 | t(42) = −2.439, p = 0.019 | t(42) = −0.147, p = 0.884 | t(42) = −0.650, p = 0.519 | t(42) = −1.207, p = 0.234 | |
| All autistic children with confirmed diagnosis | Low-functioning (n = 28) | −0.25 (1.14) | −0.93 (0.98) | +0.43 (1.0) | −0.14 (1.24) | −0.68 (1.28) |
| High-functioning (n = 29) | −0.34 (1.08) | −0.59 (1.30) | +0.59 (0.87) | +0.10 (1.11) | −0.52 (1.15) | |
| Independent t-tests | t(55) = −0.322, p = 0.748 | t(55) = 1.128, p = 0.265 | t(55) = 0.636, p = 0.528 | t(55) = 0.789, p = 0.434 | t(55) = 0.50, p = 0.619 | |
| Total (n = 57) | −0.30 (1.10) | −0.75 (1.15) | +0.51 (0.93) | −0.02 (1.17) | −0.60 (1.21) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kreysa, H.; Schneider, D.; Kowallik, A.E.; Dastgheib, S.S.; Doğdu, C.; Kühn, G.; Ruttloff, J.M.; Schweinberger, S.R. Psychosocial and Behavioral Effects of the COVID-19 Pandemic on Children and Adolescents with Autism and Their Families: Overview of the Literature and Initial Data from a Multinational Online Survey. Healthcare 2022, 10, 714. https://doi.org/10.3390/healthcare10040714
Kreysa H, Schneider D, Kowallik AE, Dastgheib SS, Doğdu C, Kühn G, Ruttloff JM, Schweinberger SR. Psychosocial and Behavioral Effects of the COVID-19 Pandemic on Children and Adolescents with Autism and Their Families: Overview of the Literature and Initial Data from a Multinational Online Survey. Healthcare. 2022; 10(4):714. https://doi.org/10.3390/healthcare10040714
Chicago/Turabian StyleKreysa, Helene, Dana Schneider, Andrea Erika Kowallik, Samaneh Sadat Dastgheib, Cem Doğdu, Gabriele Kühn, Jenny Marianne Ruttloff, and Stefan R. Schweinberger. 2022. "Psychosocial and Behavioral Effects of the COVID-19 Pandemic on Children and Adolescents with Autism and Their Families: Overview of the Literature and Initial Data from a Multinational Online Survey" Healthcare 10, no. 4: 714. https://doi.org/10.3390/healthcare10040714
APA StyleKreysa, H., Schneider, D., Kowallik, A. E., Dastgheib, S. S., Doğdu, C., Kühn, G., Ruttloff, J. M., & Schweinberger, S. R. (2022). Psychosocial and Behavioral Effects of the COVID-19 Pandemic on Children and Adolescents with Autism and Their Families: Overview of the Literature and Initial Data from a Multinational Online Survey. Healthcare, 10(4), 714. https://doi.org/10.3390/healthcare10040714






