Impact of the Cognitive–Behavioral Approach and Psychoeducational Intervention in Breast Cancer Management: A Prospective Randomized Clinical Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Sample Size
2.4. Procedures
CBT Psychoeducational Intervention
2.5. Counseling Sessions
2.6. Statistical Analysis
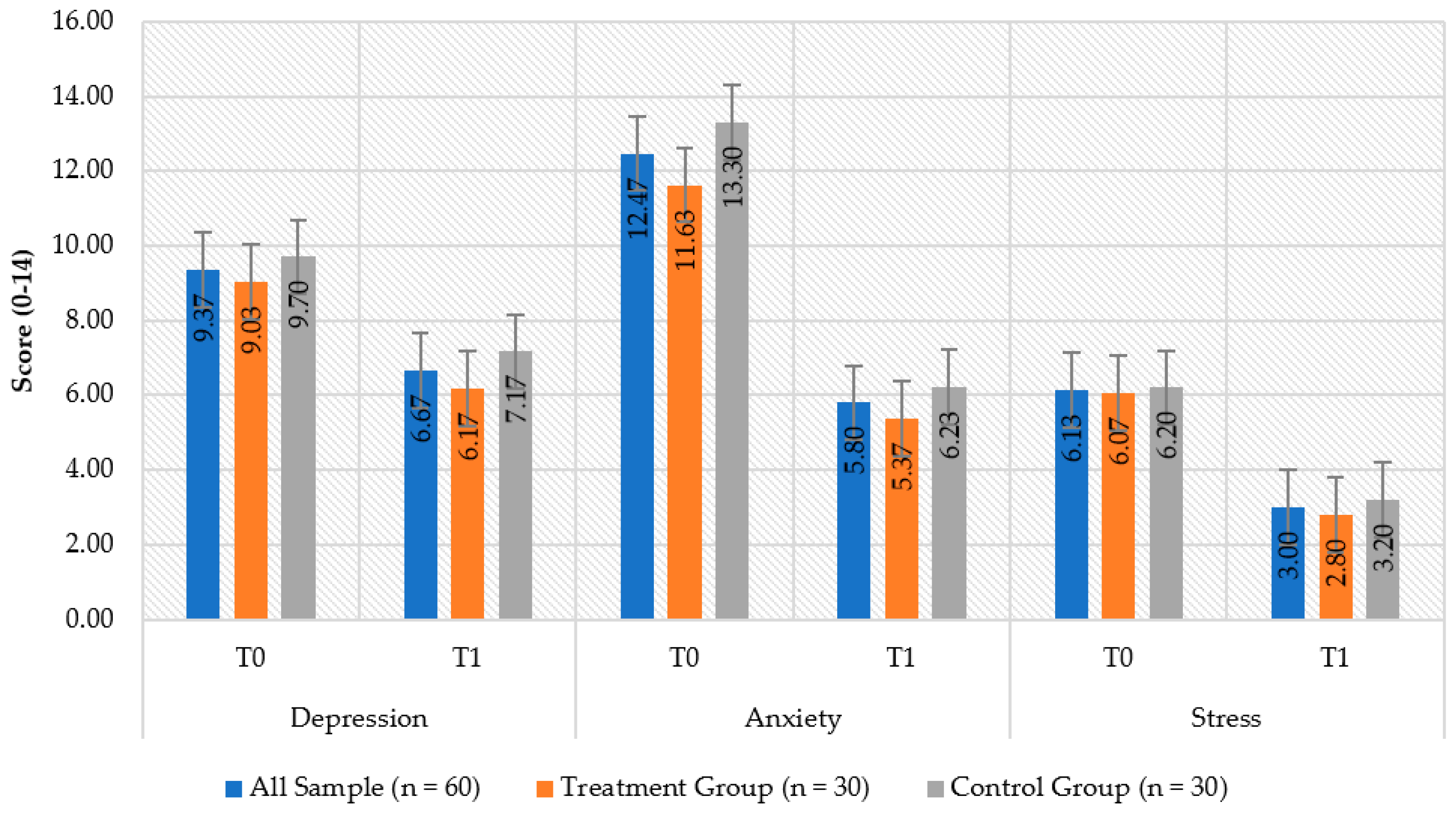
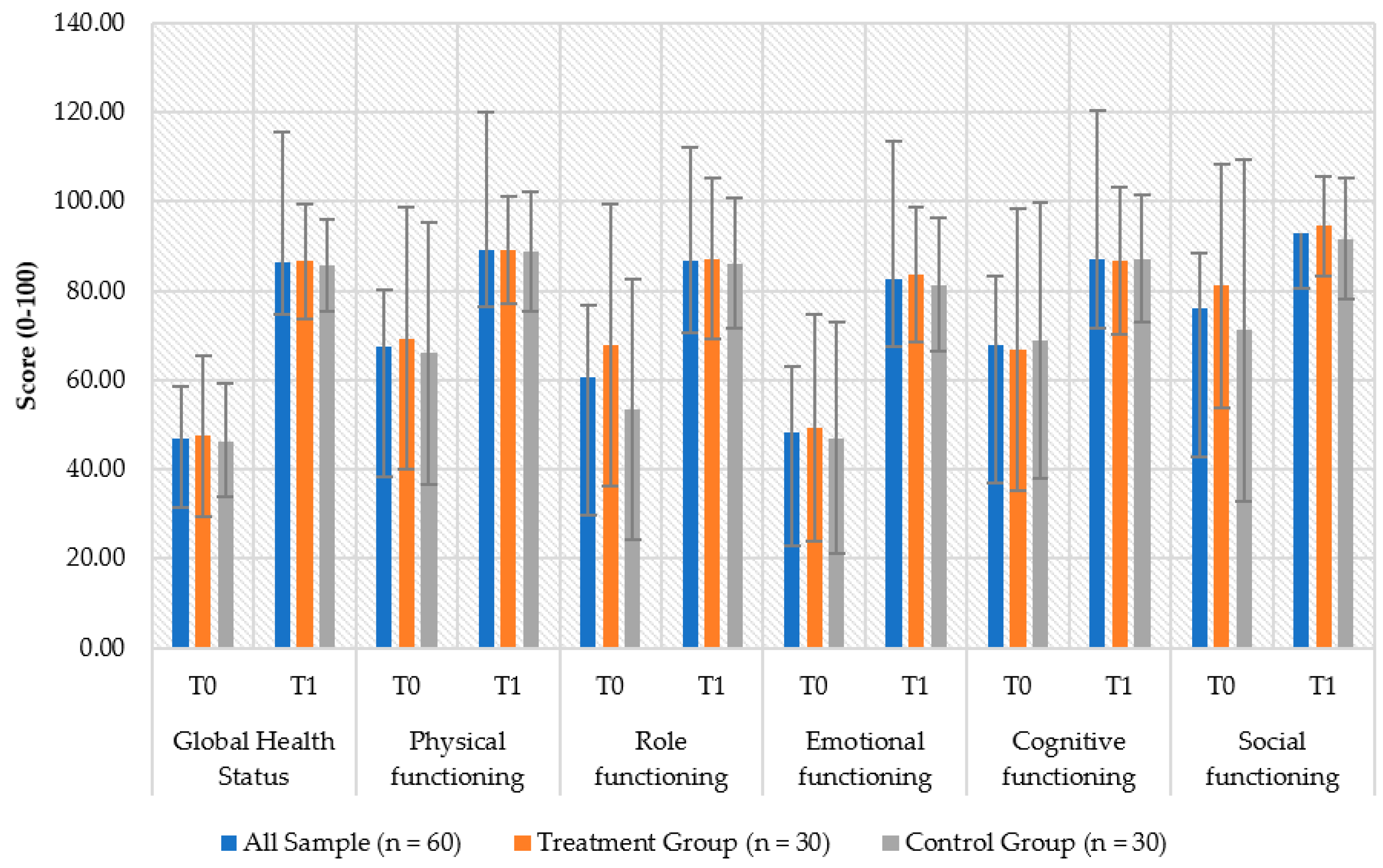
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Breastcancer.org. U.S. Breast Cancer Statistics. Available online: https://www.breastcancer.org/symptoms/understand_bc/statistics (accessed on 25 January 2022).
- Union, E. Breast Cancer Burden in EU-27. Available online: https://ecis.jrc.ec.europa.eu/pdf/Breast_cancer_factsheet-Oct_2020.pdf (accessed on 30 January 2022).
- OECD. Health at a Glance 2019—OECD Indicators. Available online: http://www.oecd.org/health/health-at-a-glance.htm (accessed on 30 January 2022).
- Wojtyla, C.; Bertuccio, P.; Wojtyla, A.; La Vecchia, C. European trends in breast cancer mortality, 1980-2017 and predictions to 2025. Eur. J. Cancer 2021, 152, 4–17. [Google Scholar] [CrossRef] [PubMed]
- Acquati, C.; Kayser, K. Predictors of psychological distress among cancer patients receiving care at a safety-net institution: The role of younger age and psychosocial problems. Support Care Cancer 2017, 25, 2305–2312. [Google Scholar] [CrossRef] [PubMed]
- Grassi, L.; Johansen, C.; Annunziata, M.A.; Capovilla, E.; Costantini, A.; Gritti, P.; Torta, R.; Bellani, M.; Italian Society of Psycho-Oncology Distress Thermometer Study Group. Screening for distress in cancer patients: A multicenter, nationwide study in Italy. Cancer 2013, 119, 1714–1721. [Google Scholar] [CrossRef]
- Zabora, J.; BrintzenhofeSzoc, K.; Curbow, B.; Hooker, C.; Piantadosi, S. The prevalence of psychological distress by cancer site. Psychooncology 2001, 10, 19–28. [Google Scholar] [CrossRef]
- Fashoyin-Aje, L.A.; Martinez, K.A.; Dy, S.M. New patient-centered care standards from the commission on cancer: Opportunities and challenges. J. Support Oncol. 2012, 10, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Sanjida, S.; McPhail, S.M.; Shaw, J.; Couper, J.; Kissane, D.; Price, M.A.; Janda, M. Are psychological interventions effective on anxiety in cancer patients? A systematic review and meta-analyses. Psychooncology 2018, 27, 2063–2076. [Google Scholar] [CrossRef] [PubMed]
- Oates, G.R.; Juarez, L.D.; Hansen, B.; Kiefe, C.I.; Shikany, J.M. Social Risk Factors for Medication Nonadherence: Findings from the CARDIA Study. Am. J. Health Behav. 2020, 44, 232–243. [Google Scholar] [CrossRef] [PubMed]
- Rodin, G.; Lloyd, N.; Katz, M.; Green, E.; Mackay, J.A.; Wong, R.K.; Supportive Care Guidelines Group of Cancer Care Ontario Program in Evidence-Based Care. The treatment of depression in cancer patients: A systematic review. Support Care Cancer 2007, 15, 123–136. [Google Scholar] [CrossRef]
- Faller, H.; Koch, U.; Brahler, E.; Harter, M.; Keller, M.; Schulz, H.; Wegscheider, K.; Weis, J.; Boehncke, A.; Hund, B.; et al. Satisfaction with information and unmet information needs in men and women with cancer. J. Cancer Surviv. 2016, 10, 62–70. [Google Scholar] [CrossRef]
- Cruickshank, S.; Kennedy, C.; Lockhart, K.; Dosser, I.; Dallas, L. Specialist breast care nurses for supportive care of women with breast cancer. Cochrane Database Syst. Rev. 2008, 1, CD005634. [Google Scholar] [CrossRef] [Green Version]
- Riba, M.B.; Donovan, K.A.; Andersen, B.; Braun, I.; Breitbart, W.S.; Brewer, B.W.; Buchmann, L.O.; Clark, M.M.; Collins, M.; Corbett, C.; et al. Distress Management, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2019, 17, 1229–1249. [Google Scholar] [CrossRef] [PubMed]
- Associazione Italiana di Oncologia Medica. Assistenza Psico-Sociale dei Malati Oncologici. Available online: https://www.aiom.it/wp-content/uploads/2019/10/2019_LG_AIOM_Psicosociali.pdf (accessed on 30 January 2022).
- Associazione Italiana di Oncologia Medica. Assistenza Psico-Sociale dei Malati Oncologici. Available online: http://media.aiom.it/userfiles/files/doc/LG/2016_LG_AIOM_Psicosociali.pdf (accessed on 30 January 2022).
- Cipolletta, S.; Simonato, C.; Faccio, E. The Effectiveness of Psychoeducational Support Groups for Women With Breast Cancer and Their Caregivers: A Mixed Methods Study. Front. Psychol. 2019, 10, 288. [Google Scholar] [CrossRef] [PubMed]
- Guarino, A.; Polini, C.; Forte, G.; Favieri, F.; Boncompagni, I.; Casagrande, M. The Effectiveness of Psychological Treatments in Women with Breast Cancer: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lally, R.M.; Kupzyk, K.A.; Bellavia, G.; Hydeman, J.; Gallo, S.; Helgeson, V.S.; Erwin, D.; Mills, A.C.; Brown, J.K. CaringGuidance after breast cancer diagnosis eHealth psychoeducational intervention to reduce early post-diagnosis distress. Support Care Cancer 2020, 28, 2163–2174. [Google Scholar] [CrossRef] [Green Version]
- Musiat, P.; Tarrier, N. Collateral outcomes in e-mental health: A systematic review of the evidence for added benefits of computerized cognitive behavior therapy interventions for mental health. Psychol. Med. 2014, 44, 3137–3150. [Google Scholar] [CrossRef]
- Sun, H.; Huang, H.; Ji, S.; Chen, X.; Xu, Y.; Zhu, F.; Wu, J. The Efficacy of Cognitive Behavioral Therapy to Treat Depression and Anxiety and Improve Quality of Life Among Early-Stage Breast Cancer Patients. Integr. Cancer Ther. 2019, 18, 1534735419829573. [Google Scholar] [CrossRef] [Green Version]
- Xiao, F.; Song, X.; Chen, Q.; Dai, Y.; Xu, R.; Qiu, C.; Guo, Q. Effectiveness of Psychological Interventions on Depression in Patients After Breast Cancer Surgery: A Meta-analysis of Randomized Controlled Trials. Clin. Breast Cancer 2017, 17, 171–179. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Meader, N.; Symonds, P. Diagnostic validity of the Hospital Anxiety and Depression Scale (HADS) in cancer and palliative settings: A meta-analysis. J. Affect. Disord. 2010, 126, 335–348. [Google Scholar] [CrossRef]
- Holland, J.C.; Alici, Y. Management of distress in cancer patients. J. Support Oncol. 2010, 8, 4–12. [Google Scholar]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; de Haes, J.C.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef]
- Kim, Y.H.; Choi, K.S.; Han, K.; Kim, H.W. A psychological intervention programme for patients with breast cancer under chemotherapy and at a high risk of depression: A randomised clinical trial. J. Clin. Nurs. 2018, 27, 572–581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tee, J.; Kazantzis, N. Collaborative empiricism in cognitive therapy: A definition and theory for the relationship construct. Clin. Psychol. Sci. Pract. 2011, 18, 47–61. [Google Scholar] [CrossRef]
- Dobson, D.; Dobson, K.S. Evidence-Based Practice of Cognitive-Behavoral Therapy, 2nd ed.; Gilford Press: New York, NY, USA, 2017. [Google Scholar]
- Mazzi, M.A.; Perlini, C.; Deledda, G.; Ghilardi, A.; Buizza, C.; Bottacini, A.; Goss, C.; Del Piccolo, L. Employment status and information needs of patients with breast cancer: A multicentre cross-sectional study of first oncology consultations. BMJ Open 2020, 10, e038543. [Google Scholar] [CrossRef] [PubMed]
- Beatty, L.; Koczwara, B.; Wade, T. Cancer coping online: A pilot trial of a self-guided CBT internet intervention for cancer-related distress. EJ Appl. Psychol. 2011, 7, 17–25. [Google Scholar] [CrossRef]
- Foley, E.; Baillie, A.; Huxter, M.; Price, M.; Sinclair, E. Mindfulness-based cognitive therapy for individuals whose lives have been affected by cancer: A randomized controlled trial. J. Consult Clin. Psychol. 2010, 78, 72–79. [Google Scholar] [CrossRef]
- Zimmermann, T.; Heinrichs, N.; Baucom, D.H. “Does one size fit all?” moderators in psychosocial interventions for breast cancer patients: A meta-analysis. Ann. Behav. Med. 2007, 34, 225–239. [Google Scholar] [CrossRef]
- Jacobsen, P.B.; Meade, C.D.; Stein, K.D.; Chirikos, T.N.; Small, B.J.; Ruckdeschel, J.C. Efficacy and costs of two forms of stress management training for cancer patients undergoing chemotherapy. J. Clin. Oncol. 2002, 20, 2851–2862. [Google Scholar] [CrossRef]
- Krischer, M.M.; Xu, P.; Meade, C.D.; Jacobsen, P.B. Self-administered stress management training in patients undergoing radiotherapy. J. Clin. Oncol. 2007, 25, 4657–4662. [Google Scholar] [CrossRef]
- Angell, K.L.; Kreshka, M.A.; McCoy, R.; Donnelly, P.; Turner-Cobb, J.M.; Graddy, K.; Kraemer, H.C.; Koopman, C. Psychosocial intervention for rural women with breast cancer: The Sierra-Stanford Partnership. J. Gen. Intern. Med. 2003, 18, 499–507. [Google Scholar] [CrossRef] [Green Version]
- Coutino-Escamilla, L.; Pina-Pozas, M.; Tobias Garces, A.; Gamboa-Loira, B.; Lopez-Carrillo, L. Non-pharmacological therapies for depressive symptoms in breast cancer patients: Systematic review and meta-analysis of randomized clinical trials. Breast 2019, 44, 135–143. [Google Scholar] [CrossRef]
- Li, Z.; Geng, W.; Yin, J.; Zhang, J. Effect of one comprehensive education course to lower anxiety and depression among Chinese breast cancer patients during the postoperative radiotherapy period—One randomized clinical trial. Radiat Oncol. 2018, 13, 111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jassim, G.A.; Whitford, D.L.; Hickey, A.; Carter, B. Psychological interventions for women with non-metastatic breast cancer. Cochrane Database Syst. Rev. 2015, 5, CD008729. [Google Scholar] [CrossRef] [PubMed]

| Whole Sample (n = 60) | Treatment Group (n = 30) | Control Group (n = 30) | p-Value | |
|---|---|---|---|---|
| Age | ||||
| 36–50 years | 11 (18.33%) | 7 (23.33%) | 4 (13.33) | 0.190 |
| 51–65 years | 26 (43.33%) | 15 (50.00%) | 11 (36.67) | |
| >65 years | 23 (38.33%) | 8 (26.67%) | 15 (50.00) | |
| Time from the first diagnosis | ||||
| 1–3 years | 49 (81.7%) | 23 (76.7%) | 26 (86.7%) | 0.506 |
| >3 years | 11 (18.3%) | 7 (23.3%) | 4 (13.3%) | |
| Qualification | ||||
| High School | 57 (95.0%) | 28 (93.3%) | 29 (96.7%) | 1.000 |
| Degree or Higher | 3 (5.0%) | 2 (6.7%) | 1 (3.3%) | |
| Marital Status | ||||
| Single | 5 (8.33%) | 3 (10.00%) | 2 (6.67%) | 0.229 |
| Married | 46 (76.67%) | 25 (83.33%) | 21 (70.00%) | |
| Divorced | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | |
| Widower | 9 (15.00%) | 2 (6.67%) | 7 (23.33%) | |
| BMI | ||||
| Underweight (≤18.49) | 1 (1.67%) | 1 (3.33%) | 0 (0.00%) | 0.482 |
| Normal weight (18.5–24.99) | 19 (31.67%) | 11 (36.67%) | 8 (26.67%) | |
| Overweight (25.0–29.99) | 29 (48.33%) | 12 (40.00%) | 17 (56.67%) | |
| Obese (≥30) | 11 (18.33%) | 6 (20.00%) | 5 (16.67%) | |
| Diabetes | 5 (8.33%) | 2 (6.67%) | 3 (10.00%) | 1.000 |
| Use of antidepressants or benzodiazepines | 3 (5.00%) | 2 (6.67%) | 1 (3.33%) | 1.000 |
| Psychiatric disease | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | NA |
| Staging | ||||
| 0 | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0.923 |
| I | 10 (16.67%) | 4 (13.33%) | 6 (20.00%) | |
| II | 24 (40.00%) | 13 (43.33%) | 11 (36.67%) | |
| III | 12 (20.00%) | 6 (20.00%) | 6 (20.00%) | |
| IV | 14 (23.33%) | 7 (23.33%) | 7 (23.33%) | |
| Histologic grade | ||||
| Grade 1 | 4 (6.67%) | 1 (3.33%) | 3 (10.00%) | 0.475 |
| Grade 2 | 24 (40.00%) | 11 (36.67%) | 13 (43.33%) | |
| Grade 3 | 32 (53.33%) | 18 (60.00%) | 14 (46.67%) | |
| Surgical treatment | 37 (61.67%) | 19 (63.33%) | 18 (60.00%) | 1.000 |
| Reconstruction | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | NA |
| Chemotherapy | ||||
| None | 5 (8.33%) | 2 (6.67%) | 3 (10.00%) | 1.000 |
| Adjuvant | 11 (18.33%) | 6 (20.00%) | 5 (16.67%) | |
| Neoadjuvant | 44 (73.33%) | 22 (73.33%) | 22 (73.33%) | |
| Hormonal treatment | ||||
| None | 36 (60.00%) | 16 (53.33%) | 20 (66.67%) | 0.614 |
| Pre-menopause | 5 (8.33%) | 3 (10.00%) | 2 (6.67%) | |
| Post-menopause | 19 (31.67%) | 11 (36.67%) | 8 (26.67%) | |
| Radiotherapy | 19 (31.67%) | 9 (30.00%) | 10 (33.33%) | 1.000 |
| Biological treatment | 19 (31.67%) | 10 (33.33%) | 9 (30.00%) | 1.000 |
| Molecular targeted treatment | 18 (30.00%) | 9 (30.00%) | 9 (30.00%) | 1.000 |
| Lymphedema | 10 (16.67%) | 5 (16.67%) | 5 (16.67%) | 1.000 |
| Whole Sample (n = 60) | Treatment Group (n = 30) | Control Group (n = 30) | p-Value | |||||
|---|---|---|---|---|---|---|---|---|
| Fatigue | T0 | 40.93 | ±23.90 | 35.56 | ±24.13 | 46.30 | ±22.81 | 0.117 |
| T1 | 13.52 | ±11.77 | 12.59 | ±12.29 | 14.44 | ±11.36 | 0.467 | |
| p-value | 0.000 | 0.000 | 0.000 | |||||
| Nausea and Vomiting | T0 | 21.39 | ±32.34 | 16.67 | ±30.01 | 26.11 | ±34.38 | 0.214 |
| T1 | 5.28 | ±10.40 | 4.44 | ±10.66 | 6.11 | ±10.25 | 0.355 | |
| p-value | 0.000 | 0.006 | 0.000 | |||||
| Pain | T0 | 41.11 | ±32.83 | 36.11 | ±35.85 | 46.11 | ±29.26 | 0.137 |
| T1 | 15.83 | ±12.81 | 14.44 | ±14.66 | 17.22 | ±11.97 | 0.355 | |
| p-value | 0.000 | 0.000 | 0.000 | |||||
| Dyspnea | T0 | 25.56 | ±34.92 | 22.22 | ±35.38 | 28.89 | ±34.72 | 0.325 |
| T1 | 7.78 | ±15.49 | 7.78 | ±16.80 | 7.78 | ±14.34 | 1.000 | |
| p-value | 0.000 | 0.004 | 0.000 | |||||
| Insomnia | T0 | 51.67 | ±31.55 | 46.67 | ±34.57 | 56.67 | ±27.89 | 0.274 |
| T1 | 18.33 | ±16.72 | 15.56 | ±16.91 | 21.11 | ±16.34 | 0.299 | |
| p-value | 0.000 | 0.000 | 0.000 | |||||
| Appetite Loss | T0 | 23.89 | ±33.67 | 14.44 | ±28.61 | 33.33 | ±36.09 | 0.024 |
| T1 | 6.67 | ±13.45 | 5.56 | ±12.63 | 7.78 | ±14.34 | 0.748 | |
| p-value | 0.000 | 0.055 | 0.000 | |||||
| Constipation | T0 | 13.89 | ±27.65 | 12.22 | ±26.96 | 15.56 | ±28.68 | 0.638 |
| T1 | 4.44 | ±11.43 | 4.44 | ±1.52 | 4.44 | ±11.52 | 1.000 | |
| p-value | 0.001 | 0.125 | 0.016 | |||||
| Diarrhea | T0 | 7.78 | ±18.78 | 5.56 | ±17.69 | 10.00 | ±19.87 | 0.292 |
| T1 | 2.78 | ±9.29 | 1.11 | ±6.09 | 4.44 | ±11.52 | 0.353 | |
| p-value | 0.008 | 0.250 | 0.063 | |||||
| Financial Difficulties | T0 | 4.44 | ±15.61 | 3.33 | ±13.42 | 5.56 | ±17.69 | 0.806 |
| T1 | 0.56 | ±4.30 | 1.11 | ±6.09 | 0.00 | ±0.00 | 1.000 | |
| p-value | 0.063 | 0.500 | 0.250 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ardizzone, A.; Bavetta, D.; Garo, M.L.; Santangelo, D.; Bongiorno, A.; Bono, M. Impact of the Cognitive–Behavioral Approach and Psychoeducational Intervention in Breast Cancer Management: A Prospective Randomized Clinical Trial. Healthcare 2022, 10, 629. https://doi.org/10.3390/healthcare10040629
Ardizzone A, Bavetta D, Garo ML, Santangelo D, Bongiorno A, Bono M. Impact of the Cognitive–Behavioral Approach and Psychoeducational Intervention in Breast Cancer Management: A Prospective Randomized Clinical Trial. Healthcare. 2022; 10(4):629. https://doi.org/10.3390/healthcare10040629
Chicago/Turabian StyleArdizzone, Antonella, Domenico Bavetta, Maria Luisa Garo, Domenico Santangelo, Antonio Bongiorno, and Maria Bono. 2022. "Impact of the Cognitive–Behavioral Approach and Psychoeducational Intervention in Breast Cancer Management: A Prospective Randomized Clinical Trial" Healthcare 10, no. 4: 629. https://doi.org/10.3390/healthcare10040629
APA StyleArdizzone, A., Bavetta, D., Garo, M. L., Santangelo, D., Bongiorno, A., & Bono, M. (2022). Impact of the Cognitive–Behavioral Approach and Psychoeducational Intervention in Breast Cancer Management: A Prospective Randomized Clinical Trial. Healthcare, 10(4), 629. https://doi.org/10.3390/healthcare10040629






