Simulation Study of the Impact of COVID-19 Policies on the Efficiency of a Smart Clinic MRI Service
Abstract
1. Introduction
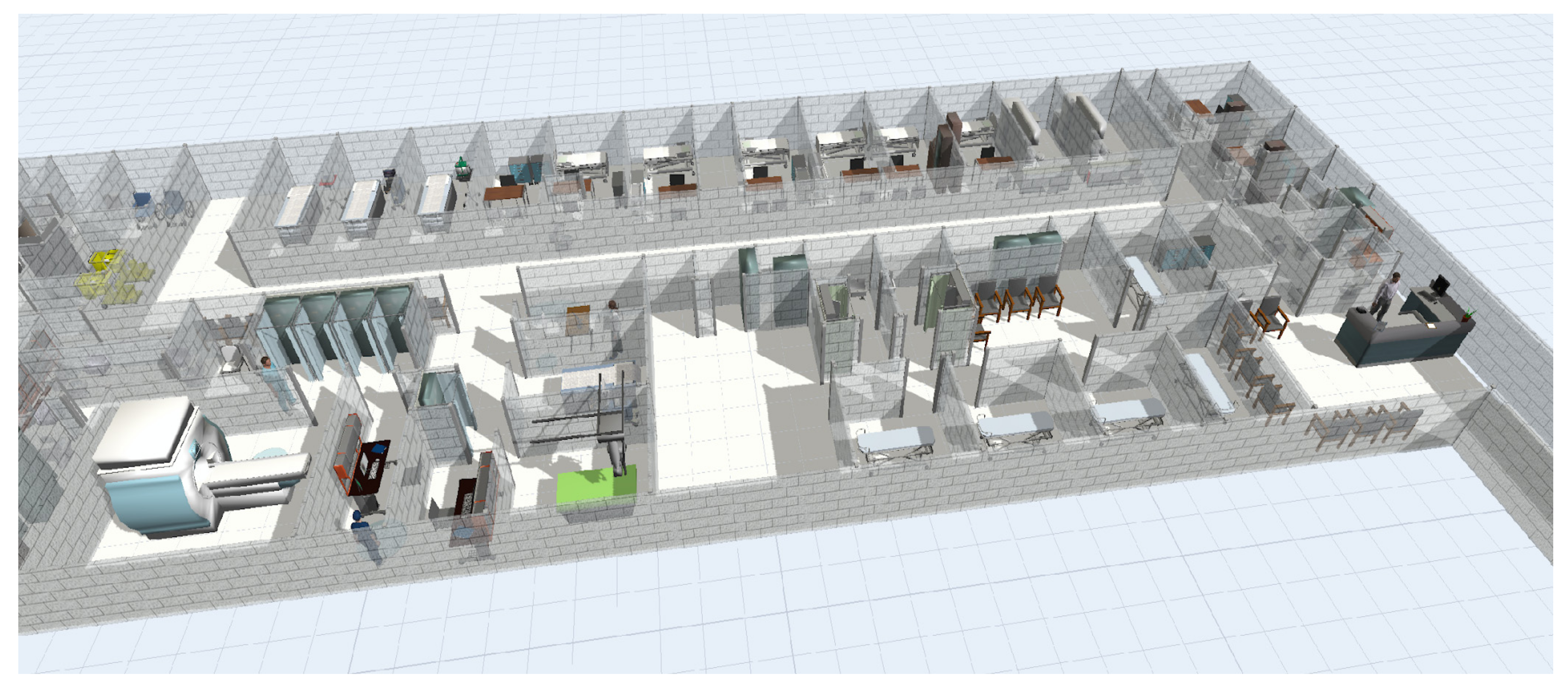
2. Characteristics of a Smart Clinic
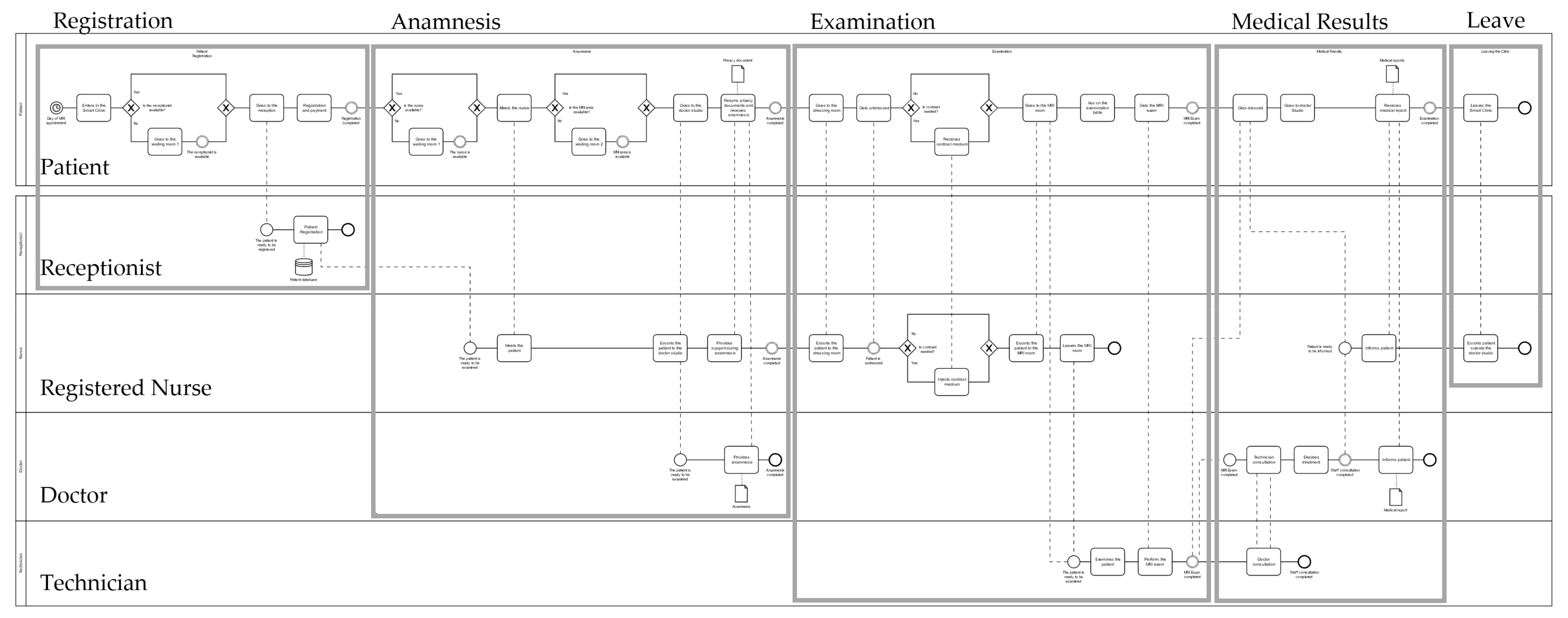
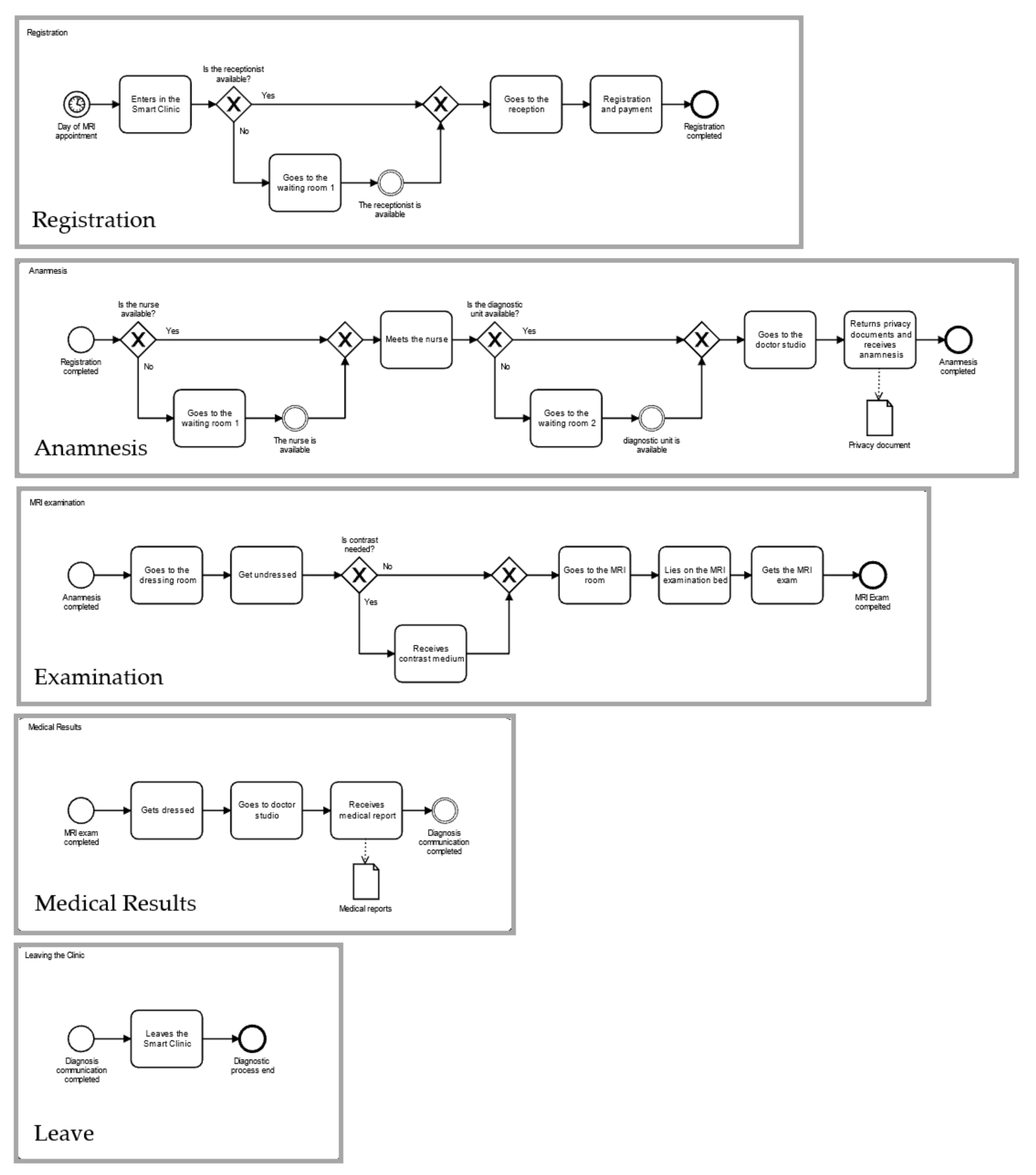
Process Conceptualization
3. Methodology
3.1. Baseline Scenario
3.2. Pandemic Scenario
3.3. Model Data
3.4. Key Performance Indicators
3.5. Improvement of the Pandemic Model
4. Results and Discussion
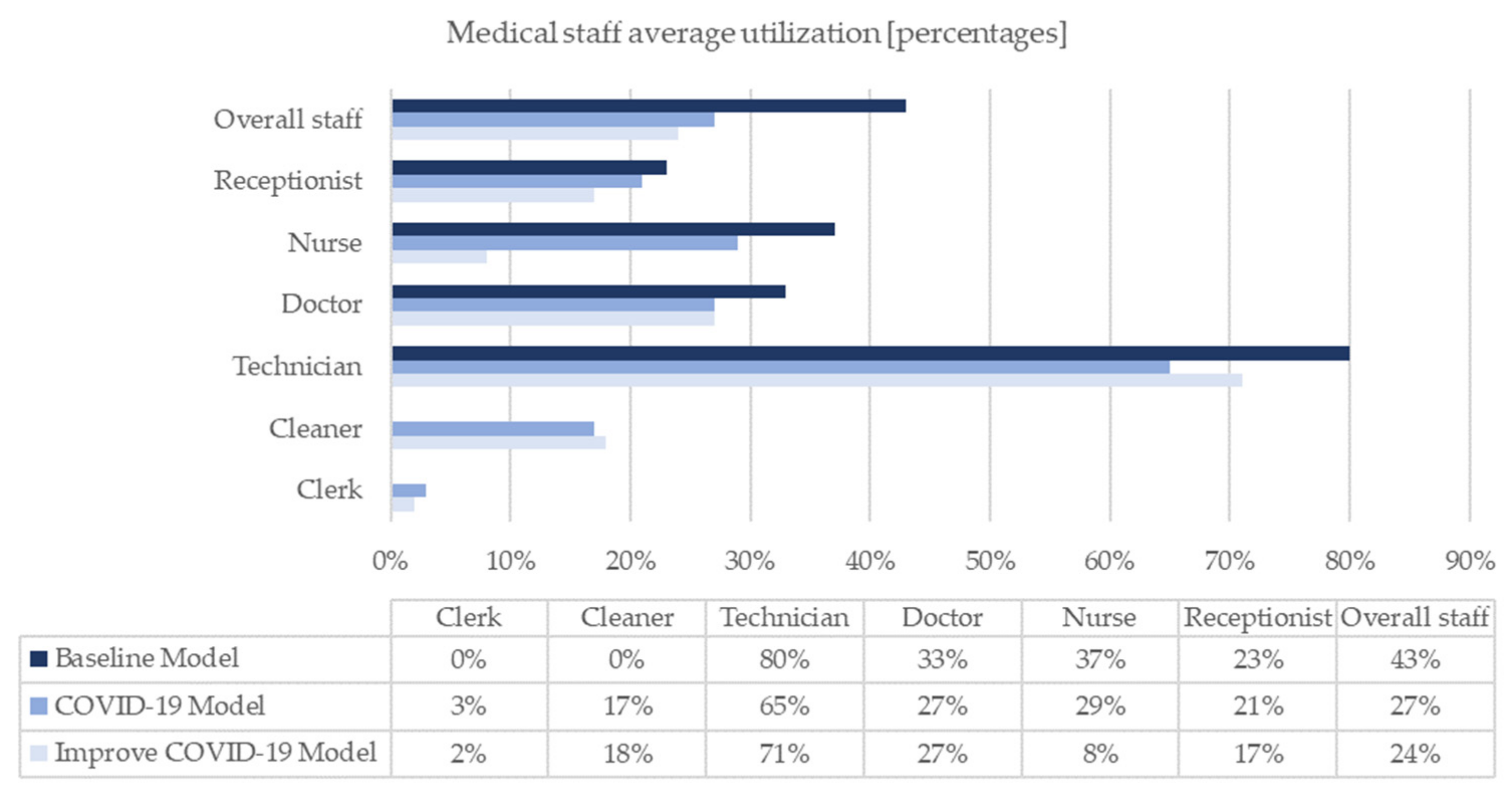
4.1. Results
4.2. Discussion
5. Conclusions and Further Developments
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Moynihan, R.; Sanders, S.; Michaleff, Z.; Scott, A.; Clark, J.; To, E.; Jones, M.; Kitchener, E.; Fox, M.; Johansson, M.; et al. Pandemic impacts on healthcare utilisation: A systematic review. BMJ Open 2020, 11, 1–10. [Google Scholar] [CrossRef]
- Das, A. Impact of the COVID-19 pandemic on the workflow of an ambulatory endoscopy center: An assessment by discrete event simulation. Gastrointest. Endosc. 2020, 92, 914–924. [Google Scholar] [CrossRef] [PubMed]
- Le Lay, J.; Augusto, V.; Xie, X.; Alfonso-Lizarazo, E.; Bongue, B.; Celarier, T.; Gonthier, R.; Masmoudi, M. Impact of COVID-19 Epidemics on Bed Requirements in a Healthcare Center Using Data-Driven Discrete-Event Simulation. In Proceedings of the Proceedings-Winter Simulation Conference (WSC), Orlando, FL, USA, 14–18 December 2020; Institute of Electrical and Electronics Engineers (IEEE) Inc.: Piscataway, NJ, USA, 2020; pp. 771–781. [Google Scholar]
- Garcia-Vicuna, D.; Mallor, F.; Esparza, L. Planning Ward and Intensive Care Unit Beds for COVID-19 Patients Using a Discrete Event Simulation Model. In Proceedings of the Proceedings-Winter Simulation Conference (WSC), Orlando, FL, USA, 14–18 December 2020; Institute of Electrical and Electronics Engineers (IEEE) Inc.: Piscataway, NJ, USA, 2020; pp. 759–770. [Google Scholar]
- Melman, G.J.; Parlikad, A.K.; Cameron, E.A.B. Balancing scarce hospital resources during the COVID-19 pandemic using discrete-event simulation. Health Care Manag. Sci. 2021, 24, 356–374. [Google Scholar] [CrossRef] [PubMed]
- Bovim, T.R.; Gullhav, A.N.; Andersson, H.; Dale, J.; Karlsen, K. Simulating emergency patient flow during the COVID-19 pandemic. J. Simul. 2022, 1–15. [Google Scholar] [CrossRef]
- Garcia-Vicuña, D.; Esparza, L.; Mallor, F. Hospital preparedness during epidemics using simulation: The case of COVID-19. Cent. Eur. J. Oper. Res. 2022, 30, 213–249. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Guan, Y.; Zhong, X.; Fishe, J.N.; Hogan, T. Hospital Beds Planning and Admission Control Policies for COVID-19 Pandemic: A Hybrid Computer Simulation Approach. IEEE Int. Conf. Autom. Sci. Eng. 2021, 17, 956–961. [Google Scholar] [CrossRef]
- Shahverdi, B.; Miller-Hooks, E.; Tariverdi, M.; Ghayoomi, H.; Prentiss, D.; Kirsch, T.D. Models for Assessing Strategies for Improving Hospital Capacity for Handling Patients during a Pandemic. Disaster Med. Public Health Prep. 2022, 10, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sethi, K.; Levine, E.S.; Roh, S.; Marx, J.L.; Ramsey, D.J. Modeling the impact of COVID-19 on Retina Clinic Performance. BMC Ophthalmol. 2021, 21, 206–217. [Google Scholar] [CrossRef] [PubMed]
- Way Tan, K.; Keow Goh, B.; Gunawan, A.; Way, K.; Keow, B.; Way Tan, K.; Keow Goh, B. Redesigning patient flow in paediatric eye clinic for pandemic using simulation. In Proceedings of the 2021 IEEE International Smart Cities Conference (ISC2), Manchester, UK, 7–10 September 2021. [Google Scholar]
- Banks, J. Handbook of Simulation: Principles, Methodology, Advances, Applications, and Practice; Jerry Banks, John Wiley Sons, Inc.: Hoboken, NJ, USA, 1999; Volume 18, pp. 380–381. [Google Scholar] [CrossRef]
- Chung, C.A. (Ed.) Simulation Modeling Handbook: A Practical Approach; Taylor & Francis Inc.: London, UK, 2004. [Google Scholar]
- Ferrin, D.M.; Miller, M.J.; McBroom, D.L. Maximizing hospital finanacial impact and emergency department throughput with simulation. In Proceedings of the Proceedings-Winter Simulation Conference, Washington, DC, USA, 9–12 December 2007; pp. 1566–1573. [Google Scholar]
- Miller, M.J.; Ferrin, D.M.; Szymanski, J.M. Simulating six sigma improvement ideas for a hospital emergency department. Winter Simul. Conf. Proc. 2003, 2, 1926–1929. [Google Scholar] [CrossRef]
- Miller, M.J.; Ferrin, D.M.; Messer, M.G. Fixing the emergency department: A transformational journey with EDSIM. Proc.-Winter Simul. Conf. 2004, 2, 1988–1993. [Google Scholar] [CrossRef][Green Version]
- Pidd, M. Tools for Thinking, Modelling in Management Thinking; John Wiley Sons, Inc.: Hoboken, NJ, USA, 2003; ISBN 978-0-470-72142-1. [Google Scholar]
- Günal, M.M.; Pidd, M. Discrete event simulation for performance modelling in health care: A review of the literature. J. Simul. 2010, 4, 42–51. [Google Scholar] [CrossRef]
- Liu, S.; Li, Y.; Triantis, K.P.; Xue, H.; Wang, Y. The Diffusion of Discrete Event Simulation Approaches in Health Care Management in the Past Four Decades: A Comprehensive Review. MDM Policy Pract. 2020, 5, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X. Application of discrete event simulation in health care: A systematic review. BMC Health Serv. Res. 2018, 18, 687–698. [Google Scholar] [CrossRef]
- Srinivas, S.; Nazareth, R.P.; Ullah, M.S. Modeling and analysis of business process reengineering strategies for improving emergency department efficiency. Simulation 2020, 97, 3–18. [Google Scholar] [CrossRef]
- Chemweno, P.; Thijs, V.; Pintelon, L.; Van Horenbeek, A. Discrete event simulation case study: Diagnostic path for stroke patients in a stroke unit. Simul. Model. Pract. Theory 2014, 48, 45–57. [Google Scholar] [CrossRef]
- Nikakhtar, A.; Hsiang, S.M. Incorporating the dynamics of epidemics in simulation models of healthcare systems. Simul. Model. Pract. Theory 2014, 43, 67–78. [Google Scholar] [CrossRef]
- Torri, A. Utilizzo Della Simulazione ad Eventi Discreti Come Strumento per l’ Analisi ed il Re-Engineering dei Processi Sanitari. PhD Thesis, Università degli Studi di Napoli Federico II, Naples, Italy, 2015. [Google Scholar]
- Preparing for a Mass Patient Move FlexSim. Available online: https://www.flexsim.com/healthcare/case-studies/preparing-mass-patient-move/ (accessed on 26 May 2021).
- FlexSim Healthcare. Available online: https://www.flexsim.com/healthcare/case-studies/getting-most-from-additional-building/ (accessed on 25 January 2022).
- Flexsim. 2019. Available online: https://www.flexsim.com/healthcare/case-studies/better-decisions-emergency-department/ (accessed on 26 January 2022).
- Pongjetanapong, K.; O’Sullivan, M.; Walker, C.; Furian, N. Implementing complex task allocation in a cytology lab via HCCM using Flexsim HC. Simul. Model. Pract. Theory 2018, 86, 139–154. [Google Scholar] [CrossRef]
- Pan, C.; Zhang, D.; Wan Mei Kon, A.; Sue Lea Wai, C.; Boon Ang, W. Patient flow improvement for an ophthalmic specialist outpatient clinic with aid of discrete event simulation and design of experiment. Health Care Manag. Sci. 2015, 18, 137–155. [Google Scholar] [CrossRef] [PubMed]
- Gruppo San Donato, Protocollo per gli Ambulatori Medici per la Gestione Post-Emergenza Covid-19; Gruppo San Donato: Milan, Italy, 2020.
- Gruppo San Donato, Procedura Organizzativa per la Prevenzione della Trasmissione della Malattia da Coronavirus; Gruppo San Donato: Milan, Italy, 2020.
- Humanitas Research Hospital Corporate Profile. Available online: https://www.humanitas.net/?_gl=1*12vgeie*_ga*MTAxMTI5MDU5My4xNjQ4MTkxMTEy*_ga_82CNG99M6T*MTY0ODE5MTExMS4xLjAuMTY0ODE5MTExMy4w (accessed on 25 January 2022).
- Carson, J.S. Model verification and validation. Proc. Winter Simul. Conf. 2002, 1, 52–58. [Google Scholar] [CrossRef]
- Sargent, R.G. Verification and validation of simulation models. Proc. Winter Simul. Conf. 2010, 7, 12–24. [Google Scholar] [CrossRef]




| Participant | Baseline Model Units | COVID-19 Model Units | Time Schedule | States |
|---|---|---|---|---|
| Patient | 123 * | 100 * | 9.00 a.m.–8.00 p.m. | Receiving Direct Care |
| Receiving Indirect Care | ||||
| Receptionist | 1 | 1 | 8.30 a.m.–8.30 p.m. | Registering Patient |
| Booking Appointments | ||||
| Clinic Closing/Opening | ||||
| Registered nurse | 1 | 1 | 9.00 a.m.–8.00 p.m. | Anamnesis |
| CMI | ||||
| Patient Information | ||||
| Physician | 1 | 1 | 9.00 a.m.–8.00 p.m. | Anamnesis |
| Staff Consultation | ||||
| Patient Information | ||||
| Technician | 1 | 1 | 8.30 a.m.–8.30 p.m. | Examination |
| Staff Consultation | ||||
| Clinic Closing/Opening | ||||
| COVID-19 clerk | 0 | 1 | 9.00 a.m.–8.00 p.m. | Sanitization |
| Cleaning staff | 0 | 1 | 9.00 a.m.–8.30 p.m. | Sanitization |
| Process Activity | Distribution (Parameters) (s) | Participant Involved | State of the Participant |
|---|---|---|---|
| Appointment booking | Normal (300,13) | Patient | Receiving Indirect Care |
| Receptionist | Booking Appointments | ||
| Registration and payment | Normal (300,13) | Patient | Receiving Indirect Care |
| Receptionist | Registering Patient | ||
| Anamnesis | Normal (300,13) | Patient | Receiving Direct Care |
| Nurse | Anamnesis | ||
| Doctor | Anamnesis | ||
| Undress CMI * | Normal (180,11) | patient | Receiving Indirect Care |
| Uniform (300,600) | Patient | Receiving Direct Care | |
| Nurse | Contrast Medium Injection | ||
| Patient examination | Normal (120,20) | Patient | Receiving Direct Care |
| Technician | Examination | ||
| MRI exam (single area) * | Uniform (900,1800) | Patient | Receiving Direct Care |
| Technician | Examination | ||
| MRI exam (multiple areas) * | Uniform (2700,3600) | Patient | Receiving Direct Care |
| Technician | Examination | ||
| Dress | Normal (180,11) | Patient | Receiving Indirect Care |
| Check MRI correctness | Normal (120,20) | Technician | Staff Consultation |
| Doctor | Staff Consultation | ||
| Diagnosis | Normal (300,13) | Patient | Receiving Direct Care |
| Doctor | Patient Information | ||
| Nurse | Patient Information |
| Process Activity | Distribution (Parameters) (s) | Participant Involved | State of the Participant |
|---|---|---|---|
| Hand sanitizing | Uniform (5,10) | Patient | Sanitization |
| Temperature scanning | Uniform (8,12) | Patient | Sanitization |
| Clerk | Sanitization | ||
| Wear mask and gloves | Normal (300,13) | Patient | Sanitization |
| CMI site cleaning | Normal (60,2) | Cleaner | Sanitization |
| MRI cleaning | Normal (300,10) | Cleaner | Sanitization |
| Dressing room cleaning | Normal (120,5) | Cleaner | Sanitization |
| KPIs | Definition | |
|---|---|---|
| OPERATIONAL INDICATORS | Facility time (min) | Time spent by patients inside the facility |
| Receiving Direct Care time (min) | Time spent by patients performing tasks that add value to the diagnostic process | |
| Receiving Indirect Care time (min) | Time spent by patients performing indispensable tasks without added value | |
| In transit time (min) | Walking time of patients | |
| Idle time (min) | Time spent by patients in idle or non-value-added tasks | |
| Sanitizing time (min) | Time spent by patients in sanitation activities | |
| PRODUCTIVITY INDICATORS | Throughput (patients) | Number of treated patients/week |
| CMI throughput | Number of CMI patients/week | |
| MRI utilization (min (%)) | Time of MRI use | |
| MRI downtime (min (%)) | Time of MRI downtime | |
| Public closure (min (%)) | Downtime owing to the mismatch between availability and activation of MRI machine | |
| First patient (min (%)) | Downtime owing to the daily first patient | |
| Last patient (min (%)) | Downtime owing to the daily last patient | |
| CMI (min (%)) | Downtime owing to the CMI | |
| Staff consultation (min (%)) | Downtime owing to the technician–doctor consultation | |
| Sanitation (min (%)) | Downtime owing to the MRI sterilisation | |
| Other (min (%)) | Other downtimes not attributable to the previous groups | |
| Staff utilization (%) | Time of staff use in working activities | |
| Receptionist (%) | Time of receptionist use in working activities | |
| Registered Nurse (%) | Time of registered nurse use in working activities | |
| Physician (%) | Time of physician use in working activities | |
| Technician (%) | Time of technician use in working activities | |
| Cleaning Staff (%) | Time of cleaning staff use in working activities | |
| Clerk (%) | Time of clerk in working activities | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sala, F.; Quarto, M.; D’Urso, G. Simulation Study of the Impact of COVID-19 Policies on the Efficiency of a Smart Clinic MRI Service. Healthcare 2022, 10, 619. https://doi.org/10.3390/healthcare10040619
Sala F, Quarto M, D’Urso G. Simulation Study of the Impact of COVID-19 Policies on the Efficiency of a Smart Clinic MRI Service. Healthcare. 2022; 10(4):619. https://doi.org/10.3390/healthcare10040619
Chicago/Turabian StyleSala, Francesca, Mariangela Quarto, and Gianluca D’Urso. 2022. "Simulation Study of the Impact of COVID-19 Policies on the Efficiency of a Smart Clinic MRI Service" Healthcare 10, no. 4: 619. https://doi.org/10.3390/healthcare10040619
APA StyleSala, F., Quarto, M., & D’Urso, G. (2022). Simulation Study of the Impact of COVID-19 Policies on the Efficiency of a Smart Clinic MRI Service. Healthcare, 10(4), 619. https://doi.org/10.3390/healthcare10040619








