Challenges Facing Undergraduate Medical Education in Ambulatory Care Clinics at Tertiary Care Hospitals
Abstract
1. Introduction
2. Methodology
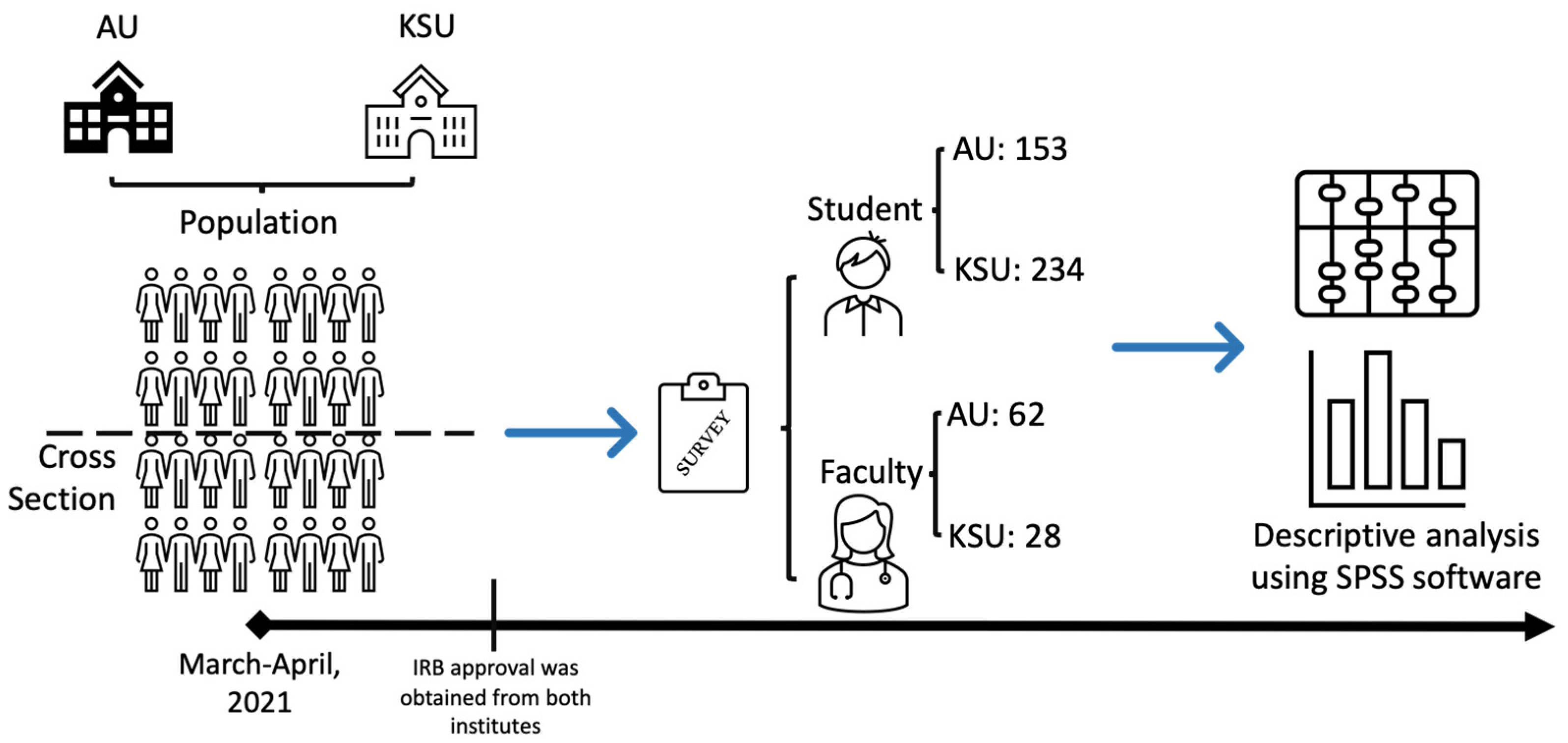
2.1. Study Design and Population
2.2. Sample Size
2.3. Data Collection/Instrument
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
3.1. Students Survey Analysis
3.1.1. Demographic Factors
3.1.2. Student’s General Perception
3.1.3. Virtual Clinics and Preferred Clinics
3.1.4. Environmental Barriers
3.1.5. Faculty-Related Barriers
3.1.6. Patient-Related Factors
3.1.7. Student-Related Factors
3.2. Faculty Survey Analysis
3.2.1. Demographic Factors
3.2.2. Faculty’s General Perception
3.2.3. Environmental Factors
3.2.4. Faculty Related Factors
3.2.5. Patient Related Factors
3.2.6. Student Related Factors
4. Discussion
4.1. Environmental Factors
4.2. Faculty Related Factors
4.3. Patient Related Factors
4.4. Student Related Factors
4.5. Study Implications
4.6. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Myung, S.J.; Kang, S.H.; Kim, Y.S.; Lee, E.B.; Shin, J.S.; Shin, H.Y.; Park, W.B. The use of standardized patients to teach medical students clinical skills in ambulatory care settings. Med. Teach. 2010, 32, e467–e470. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Petterson, S.M.; Liaw, W.R.; Phillips, R.L., Jr.; Rabin, D.L.; Meyers, D.S.; Bazemore, A. Projecting US Primary Care Physician Workforce Needs: 2010–2025. Ann. Fam. Med. 2012, 10, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Franco, R.L.O.; Machado, J.L.M.; Grinbaum, R.S.; Porfírio, G.J.M. Barriers to outpatient education for medical students: A narrative review. Int. J. Med. Educ. 2019, 10, 180–190. [Google Scholar] [CrossRef] [PubMed]
- Woolliscroft, J.; Schwenk, T.L. Teaching and learning in the ambulatory setting. Acad. Med. 1989, 64, 644–648. [Google Scholar] [CrossRef]
- Densen, P. Challenges and opportunities facing medical education. Trans. Am. Clin. Climatol. Assoc. 2011, 122, 48–58. [Google Scholar]
- Holmboe, E.S.; Bowen, J.L.; Green, M.; Gregg, J.; DiFrancesco, L.; Reynolds, E.; Alguire, P.; Battinelli, D.; Lucey, C.; Duffy, D. Reforming internal medicine residency training. J. Gen. Intern. Med. 2005, 20, 1165–1172. [Google Scholar] [CrossRef][Green Version]
- Nadkarni, M.; Reddy, S.; Bates, C.K.; Fosburgh, B.; Babbott, S.; Holmboe, E. Ambulatory-Based Education in Internal Medicine: Current Organization and Implications for Transformation. Results of A National Survey of Resident Continuity Clinic Directors. J. Gen. Intern. Med. 2010, 26, 16–20. [Google Scholar] [CrossRef]
- Thomas, K.G.; West, C.P.; Popkave, C.; Bellini, L.M.; Weinberger, S.E.; Kolars, J.C.; Kogan, J.R. Alternative Approaches to Ambulatory Training: Internal Medicine Residents’ and Program Directors’ Perspectives. J. Gen. Intern. Med. 2009, 24, 904–910. [Google Scholar] [CrossRef]
- Fields, S.A.; Usatine, R.; Steiner, E. Teaching Medical Students in the Ambulatory Setting: Strategies for success. JAMA 2000, 283, 2362–2364. [Google Scholar] [CrossRef]
- Ferenchick, G.S.; Chamberlain, J.; Alguire, P. Community-based teaching: Defining the added value for students and preceptors. Am. J. Med. 2002, 112, 512–517. [Google Scholar] [CrossRef]
- Steven, K.; Wenger, E.; Boshuizen, H.; Scherpbier, A.; Dornan, T. How Clerkship Students Learn from Real Patients in Practice Settings. Acad. Med. 2014, 89, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Lake, F.R.; Vickery, A.W. Teaching on the run tips 14: Teaching in ambulatory care. Med. J. Aust. 2006, 185, 166–167. [Google Scholar] [CrossRef] [PubMed]
- Salerno, S.M.; O’Malley, P.G.; Pangaro, L.N.; Wheeler, G.A.; Moores, L.K.; Jackson, J. Faculty development seminars based on the one-minute preceptor improve feedback in the ambulatory setting. J. Gen. Intern. Med. 2002, 17, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Krackov, S.K.; Packman, C.H.; Regan-Smith, M.G.; Birskovich, L.; Seward, S.J.; Baker, S.D. Perspectives on ambulatory programs: Barriers and implementation strategies. Teach. Learn. Med. 1993, 5, 243–250. [Google Scholar] [CrossRef]
- Dent, J.A.; Hesketh, E.A. Developing the teaching instinct. 9: How to teach in an ambulatory care (outpatient) teaching centre. Med. Teach. 2003, 25, 488–491. [Google Scholar] [CrossRef]
- Lesky, L.G.; Borkan, S.C. Strategies to improve teaching in the ambulatory medicine setting. Arch. Intern. Med. 1990, 150, 2133–2137. [Google Scholar] [CrossRef]
- Adams, M.; Eisenberg, J.M. What is the cost of ambulatory education? J. Gen. Intern. Med. 1997, 12, S104–S110. [Google Scholar] [CrossRef][Green Version]
- Rose, S. Medical Student Education in the Time of COVID-19. JAMA 2020, 323, 2131–2132. [Google Scholar] [CrossRef]
- Batais, M.A.; Temsah, M.-H.; AlGhofili, H.; AlRuwayshid, N.; Alsohime, F.; Almigbal, T.H.; Al-Rabiaah, A.; Al-Eyadhy, A.A.; Mujammami, M.H.; Halwani, R.; et al. The coronavirus disease of 2019 pandemic-associated stress among medical students in middle east respiratory syndrome-CoV endemic area: An observational study. Medicine 2021, 100, e23690. [Google Scholar] [CrossRef]
- Saddik, B.; Hussein, A.; Sharif-Askari, F.S.; Kheder, W.; Temsah, M.-H.; Koutaich, R.A.; Haddad, E.S.; Al-Roub, N.M.; Marhoon, F.A.; Hamid, Q.; et al. Increased Levels of Anxiety Among Medical and Non-Medical University Students during the COVID-19 Pandemic in the United Arab Emirates. Risk Manag. Heal. Policy 2020, 13, 2395–2406. [Google Scholar] [CrossRef]
- Harries, A.J.; Lee, C.; Jones, L.; Rodriguez, R.M.; Davis, J.A.; Boysen-Osborn, M.; Kashima, K.J.; Krane, N.K.; Rae, G.; Kman, N.; et al. Effects of the COVID-19 pandemic on medical students: A multicenter quantitative study. BMC Med. Educ. 2021, 21, 14. [Google Scholar] [CrossRef] [PubMed]
- Bardgett, R.J.; A Dent, J. Teaching and learning in outpatients and beyond: How ambulatory care teaching can contribute to student learning in child health. Arch. Dis. Child. Educ. Pr. Ed. 2011, 96, 148–152. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Denton, G.D.; Lo, M.C.; Brandenburg, S.; Hingle, S.; Meade, L.; Chheda, S.; Fazio, S.B.; Blanchard, M.; Hoellein, A. Solutions to Common Problems in Training Learners in General Internal Medicine Ambulatory Settings. Am. J. Med. 2015, 128, 1152–1157. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, K.; Shiozawa, M.; Aiso, S.; Taniguchi, S.; Yamashita, S. Distribution of gamma-glutamyl transpeptidase in human pancreas: Immunohistochemical study with a monoclonal antibody. J. Histochem. Cytochem. 1990, 38, 339–350. [Google Scholar] [CrossRef] [PubMed]
- Croft, A.; Carruthers, D.; Justice, E. Undergraduate teaching in the outpatient clinic: Can we do better? Med. Teach. 2012, 34, 674. [Google Scholar] [CrossRef]
- Young, B.L.; Graham, R.P.; Shipengrover, J.; James, P.A. Components of learning in ambulatory settings: A qualitative analysis. Acad. Med. 1998, 73 (Suppl. 10), S60–S63. [Google Scholar] [CrossRef]
- McGee, S.R.; Irby, D.M. Teaching in the outpatient clinic. J. Gen. Intern. Med. 1997, 12 (Suppl. 2), S34–S40. [Google Scholar] [CrossRef]
- Feltovich, J.; A Mast, T.; Soler, N.G. Teaching medical students in ambulatory settings in departments of internal medicine. Acad. Med. 1989, 64, 36–41. [Google Scholar] [CrossRef]
- Phillips, R.R.; Gerlis, L.M.; Wilson, N.; Walker, D.R. Aortic valve damage caused by operative balloon dilatation of critical aortic valve stenosis. Heart 1987, 57, 168–170. [Google Scholar] [CrossRef]
- Ramani, S.; Leinster, S. AMEE Guide no. 34: Teaching in the clinical environment. Med. Teach. 2008, 30, 347–364. [Google Scholar] [CrossRef]
- Skeff, K.M.; Bowen, J.L.; Irby, D. Protecting time for teaching in the ambulatory care setting. Acad. Med. 1997, 72, 694–697. [Google Scholar] [CrossRef] [PubMed]
- Marwan, Y.; Al-Saddique, M.; Hassan, A.; Karim, J.; Al-Saleh, M. Are medical students accepted by patients in teaching Hospitals? Med. Educ. Online 2012, 17, 17172. [Google Scholar] [CrossRef] [PubMed]
- Coleman, K.; Murray, E. Patients’ views and feelings on the community-based teaching of undergraduate medical students: A qualitative study. Fam. Pr. 2002, 19, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Salisbury, K.; A Farmer, E.; Vnuk, A. Patients’ views on the training of medical students in Australian general practice settings. Aust. Fam. Physician 2004, 33, 281–283. [Google Scholar] [PubMed]
- Passaperuma, K.; Higgins, J.; Power, S.; Taylor, T. Do patients’ comfort levels and attitudes regarding medical student involvement vary across specialties? Med. Teach. 2008, 30, 48–54. [Google Scholar] [CrossRef]
- Simon, S.R.; Peters, A.S.; Christiansen, C.L.; Fletcher, R.H. Effect of medical student teaching on patient satisfaction in a managed care setting. J. Gen. Intern. Med. 2000, 15, 457–461. [Google Scholar] [CrossRef][Green Version]
- Speicher, M.R.; Sterrenberg, T.R. Students do not reduce patient satisfaction in a family medicine clinic as measured by a nationally used patient satisfaction instrument. Fam. Med. 2015, 47, 227–230. [Google Scholar]
- Fortuna, R.J.; Garfunkel, L.; Mendoza, M.D.; Ditty, M.; West, J.; Nead, K.; Robbins, B.W. Factors Associated with Resident Continuity in Ambulatory Training Practices. J. Grad. Med. Educ. 2016, 8, 532–540. [Google Scholar] [CrossRef]
- Dubé, K.; Gupta, R.; Kong, M.; Knox, M.; Bodenheimer, T. Continuity of Care in Residency Teaching Practices: Lessons from “Bright Spots”. Perm. J. 2018, 22, 18–28. [Google Scholar] [CrossRef]
- Irby, D.M. Teaching and learning in ambulatory care settings: A thematic review of the literature. Acad. Med. 1995, 70, 898–931. [Google Scholar] [CrossRef]
- Leiva, R.I.; Bitran, C.M.; Saldías, P.F. Evaluation of a teaching ambulatory module of respiratory diseases in the undergraduate medical curriculum. Rev. Med. Chile 2012, 140, 616–624. [Google Scholar] [CrossRef] [PubMed]
- Dent, J.A. AMEE Guide No 26: Clinical teaching in ambulatory care settings: Making the most of learning opportunities with outpatients. Med. Teach. 2005, 27, 302–315. [Google Scholar] [CrossRef] [PubMed]
- Azher, H.; Lay, J.; Stupart, D.A.; Guest, G.D.; Watters, D. Medical student participation in a surgical outpatient clinic: A randomized controlled trial. ANZ J. Surg. 2013, 83, 466–471. [Google Scholar] [CrossRef] [PubMed]

| Frequency | Percentage | |
|---|---|---|
| Sex | ||
| Female | 177 | 45.7 |
| Male | 210 | 54.3 |
| Study year | ||
| 4th | 190 | 49.1 |
| 5th | 197 | 50.9 |
| University | ||
| Alfaisal University | 153 | 39.5 |
| King Saud University | 234 | 60.5 |
| With whom do you prefer attending clinics? | ||
| Consultant | 171 | 44.2 |
| Fellow | 60 | 15.5 |
| Junior Resident | 58 | 15 |
| Senior Resident | 98 | 25.3 |
| What are the challenges to have proper and efficient outpatient education? | ||
| Faculty related | 150 | 39 |
| Institution related | 134 | 34.8 |
| Patient related | 57 | 14.8 |
| Student related | 32 | 8.3 |
| COVID-19 related | 24 | 6.2 |
| Other factors | 10 | 2.6 |
| Frequency | Percentage (%) | |
|---|---|---|
| Do you support involving medical students in virtual clinics? | ||
| To No extent | 78 | 20.2 |
| To little extent | 59 | 15.2 |
| To Moderate extent | 98 | 25.3 |
| To Great extent | 59 | 15.2 |
| To Very great extent | 93 | 24 |
| What are the best clinics you have attended during your medical school? | ||
| Internal medicine and IM subspecialties | 145 | 40.4 |
| Oby-Gyn | 75 | 20.9 |
| Pediatrics | 72 | 20.1 |
| General surgery | 68 | 18.9 |
| Ophthalmology | 53 | 14.8 |
| Orthopedics | 50 | 13.9 |
| Family medicine | 41 | 11.4 |
| ENT | 32 | 8.9 |
| Psychiatry | 25 | 7 |
| Neuroscience | 9 | 2.5 |
| Other clinics | 6 | 1.7 |
| Vascular and thoracic surgery | 1 | 0.3 |
| Frequency (%) | |
|---|---|
| Environment-related factors | |
| - Restrictions due to COVID-19 | 203 (52.5) |
| - Lack of structured teaching objectives | 94 (24.3) |
| - Inadequate distribution of student in ambulatory clinics | 74 (19.1) |
| - Inappropriate or small clinics rooms | 16 (4.1) |
| Faculty-related factors | |
| - Inadequate supervision and teaching by faculty | 188 (48.6) |
| - Lack of time for teaching by doctor due to intense patient agenda | 131 (33.9) |
| - Inappropriate or absence of feedback | 47 (12.1) |
| - Fear of losing private patients | 21 (5.4) |
| Patient-related factors | |
| - Patients’ refusal to be seen by medical students | 192 (49.6) |
| - No follow-up/continuity of care for cases attended | 98 (25.3) |
| - Lack of suitable patients for teaching | 97 (25.1) |
| Student-related factors | |
| - The increasing number of students attending ambulatory clinics | 151 (39) |
| - Not enough time to attend the clinics | 118 (30.5) |
| - Lack of student’s commitment and interest in learning | 72 (18.6) |
| - No additional information gained compared to inpatient setting | 46 (11.9) |
| AU n = 153 | KSU, n = 234 | Test Statistic | p-Value | |
|---|---|---|---|---|
| Sex | ||||
| Female | 95 (62.1) | 82 (35) | χ2 (1) = 27.3 | <0.001 |
| Male | 58 (37.9) | 152 (65) | ||
| Study year | ||||
| 4th | 83 (54.2) | 107 (45.7) | χ2 (1) = 2.67 | 0.101 |
| 5th | 70 (45.8) | 127 (54.3) | ||
| As a medical student, with whom do you prefer attending clinics? | ||||
| Consultant | 60 (39.2) | 111 (47.4) | χ2 (3) = 7.50 | 0.057 |
| Fellow | 33 (21.6) | 27 (11.5) | ||
| Junior resident | 22 (14.4) | 36 (15.4) | ||
| Senior resident | 38 (24.8) | 60 (25.6) | ||
| During your training in 4th/5th year, what are the barriers and challenges for medical students to have proper and efficient outpatient education? | ||||
| Faculty related | 70 (45.8) | 80 (34.2) | χ2 (1) = 5.22 | 0.022 |
| Patient related | 26 (17) | 31 (13.2) | χ2 (1) = 1.04 | 0.309 |
| Student related | 13 (8.5) | 19 (8.1) | χ2 (1) = 0.017 | 0.895 |
| Institution related | 35 (22.9) | 99 (42.3) | χ2 (1) = 15.43 | <0.001 |
| COVID-19 related | 4 (2.6) | 20 (8.5) | χ2 (1) = 5.60 | 0.018 |
| Other factors | 4 (2.6) | 6 (2.6) | χ2 (1) = 0.002 | 0.976 |
| Do you support involving medical students in virtual clinics? -Mean (SD) | 3.28 (1.49) | 2.94 (1.40) | t(309.7) = 2.23 | 0.026 |
| What do you think are the best clinics you have attended during your medical school? | ||||
| Internal Medicine and IM subspecialties | 76 (49.7) | 69 (29.5) | χ2 (1) = 16.1 | <0.001 |
| Oby-Gyn | 40 (26.1) | 35 (15) | χ2 (1) = 7.41 | 0.006 |
| Orthopedics | 3 (2) | 47 (20.1) | χ2 (1) = 27.01 | 0.001 |
| Psychiatry | 1 (0.7) | 24 (10.3) | χ2 (1) = 14.1 | <0.001 |
| Pediatrics | 58 (37.9) | 14 (6) | χ2 (1) = 62.3 | <0.001 |
| ENVIRONMENTAL-RELATED FACTORS | ||||
| Inadequate distribution of student in ambulatory clinics | 23 (15) | 51 (21.8) | χ2 (3) = 25.8 | <0.001 |
| Inappropriate or small clinics rooms | 6 (3.9) | 10 (4.3) | ||
| Lack of structured teaching objectives | 58 (37.9) | 36 (15.4) | ||
| Restrictions due to COVID-19 | 66 (37.9) | 137 (58.5) | ||
| FACULTY-RELATED FACTORS | ||||
| Fear of losing private patients | 13 (8.5) | 8 (3.4) | χ2 (3) = 4.91 | 0.179 |
| Inadequate supervision and teaching by faculty | 73 (47.7) | 115 (49.1) | ||
| Inappropriate or absence of feedback | 19 (12.4) | 28 (12) | ||
| Lack of time for teaching by doctor due to intense patient agenda | 48 (31.4) | 83 (35.5) | ||
| PATIENT-RELATED FACTORS | ||||
| Lack of suitable patients for teaching | 35 (22.9) | 62 (26.5) | χ2 (2) = 3.10 | 0.216 |
| No follow-up/continuity of care for cases attended | 46 (30.1) | 52 (22.2) | ||
| Patients’ refusal to be seen by medical students | 72 (47.1) | 120 (51.3) | ||
| STUDENT-RELATED FACTORS | ||||
| Increasing number of students attending ambulatory clinics | 41 (26.8) | 110 (47) | χ2 (3) = 21.81 | <0.001 |
| Lack of student’s commitment and interest in learning | 36 (23.5) | 36 (15.4) | ||
| No additional information gained compared to inpatient setting | 28 (18.3) | 18 (7.7) | ||
| Not enough time to attend the clinics | 48 (31.4) | 70 (29.9) | ||
| Frequency (90) | Percentage (%) | |
|---|---|---|
| Sex | ||
| Female | 15 | 16.7 |
| Male | 75 | 83.3 |
| Age group | ||
| 30–39 years | 15 | 16.7 |
| 40–49 years | 32 | 35.6 |
| 50–59 years | 32 | 35.6 |
| 60 years and above | 11 | 12.2 |
| University | ||
| Alfaisal University | 62 | 68.9 |
| King Saud University | 28 | 31.1 |
| Academic title | ||
| Assistant professor | 30 | 33.3 |
| Associate professor | 32 | 35.6 |
| Lecturer | 4 | 4.4 |
| Professor | 24 | 26.7 |
| Specialty | ||
| Internal medicine | 39 | 43.3 |
| Pediatrics | 21 | 23.3 |
| Neurosciences | 6 | 6.7 |
| Emergency medicine | 5 | 5.6 |
| Surgical subspecialties | 4 | 4.4 |
| ENT | 3 | 3.3 |
| Oby-Gyn | 3 | 3.3 |
| Family medicine | 2 | 2.2 |
| Ophthalmology | 2 | 2.2 |
| Psychiatry | 2 | 2.2 |
| Oncology | 1 | 1.1 |
| Orthopedics | 1 | 1.1 |
| Radiology | 1 | 1.1 |
| Frequency | Percentage (%) |
|---|---|
| How comfortable are you if a medical students attend ACC with you? | |
| Uncomfortable | 35.6 |
| Somehow comfortable | 25.6 |
| Moderately | 11.1 |
| Comfortable | 16.7 |
| Very comfortable | 11.1 |
| Outpatient experience is important for medical students and it should be integrated in the curriculum. | 93.3 |
| What are the main challenges & barrier to have proper and efficient medical student education in ACC settings? | |
| Environment/institutional-related | 55.6 |
| Patient-related | 24.4 |
| Faculty-related | 20 |
| Student-related | 16.7 |
| Time-related | 6.7 |
| How much do you support involving medical student in virtual clinics? | |
| To No extent | 20 |
| To little extent | 6.7 |
| Some extent | 18.9 |
| Great extent | 17.8 |
| Very great extent | 36.7 |
| Frequency (%) | |
|---|---|
| Environment-related factors | |
| Restrictions due to COVID-19 | (26.7) |
| Inadequate structuring and distribution of student in ACC | (21.1) |
| Inappropriate or small clinics rooms | (21.1) |
| Lack of institutional support | (18.9) |
| Inadequate financial incentives for academic staff | (12.2) |
| Faculty-related factors | |
| Insufficient time for teaching due to intense patient agenda | (70) |
| Not integrated as part of my current KPI | (20) |
| Not feeling comfortable to have students in my clinic | (7.8) |
| Lack of training for faculty to teach medical students in ACC | (2.2) |
| Patient-related factors | |
| Patients’ refusal to be seen by medical students | (41.1) |
| Fear of patient dissatisfaction | (24.4) |
| No follow-up/continuity of care for cases attended | (21.1) |
| Lack of suitable patients for teaching | (13.3) |
| Student-related factors | |
| Increasing numbers of students | (48.9) |
| Lack of student’s commitment and interest in learning | (51.1) |
| University | ||||
|---|---|---|---|---|
| AU (n = 62) | KSU (n = 28) | Test Statistic | p-Value | |
| Sex | ||||
| Female | 12 (19.4) | 3 (10.7) | χ2 (1) = 0.51 | 0.476 |
| Male | 50 (80.6) | 25 (89.3) | ||
| Age group | ||||
| 30–39 years | 10 (161) | 5 (17.9) | χ2 (3) = 4.60 | 0.204 |
| 40–49 years | 18 (29) | 14 (50) | ||
| 50–59 years | 25 (40.3) | 7 (25) | ||
| 60 years and above | 9 (14.5) | 2 (7.1) | ||
| Academic title | ||||
| Assistant professor | 26 (41.9) | 4 (14.3) | χ2 (3) = 13.12 | 0.004 |
| Associate Professor | 16 (25.8) | 16 (57.1) | ||
| Lecturer | 4 (6.5) | 0 | ||
| Professor | 16 (25.8) | 8 (28.6) | ||
| How comfortable you are if a medical students attend ACC with you? mean (SD) | 2.40 (1.49) | 2.46 (1.2) | t(64.23) = 0.21 | 0.837 |
| Do you think outpatient experience is important for medical students and it should be integrated in the curriculum? | ||||
| No | 2 (3.2) | 4 (14.3) | χ2 (1) = 2.22 | 0.136 |
| Yes | 60 (96.8) | 24 (85.7) | ||
| From your experience, what are the main challenges/barrier to have proper and efficient medical student education in ACC settings? | ||||
| Environment/institutional-related | 32 (51.6) | 18 (64.3) | χ2 (1) = 1.26 | 0.263 |
| Faculty-related | 10 (16.1) | 8 (28.6) | χ2 (1) = 1.87 | 0.172 |
| Patient-related | 14 (22.6) | 8 (28.6) | χ2 (1) = 0.376 | 0.541 |
| Student-related | 10 (16.1) | 5 (17.9) | χ2 (1) = 0.041 | 0.839 |
| Time-related | 4 (6.5) | 2 (7.1) | χ2 (1) < 0.001 | 1.000 |
| How much do you support involving medical student in virtual clinics? mean (SD) | 3.66 (1.48) | 2.96 (1.55) | t(88) = 2.04 | 0.045 |
| ENVIRONMENTAL-RELATED FACTORS | ||||
| Inadequate financial incentives for academic staff | 10 (16.1) | 1 (3.6) | χ2 (4) = 5.65 | 0.227 |
| Inadequate structuring and distribution of student in OPD | 15 (24.2) | 4 (14.3) | ||
| Inappropriate or small clinics rooms | 11 (17.7) | 8 (28.8) | ||
| Lack of institutional support | 11 (17.7) | 6 (21.4) | ||
| Restrictions due to COVID-19 | 15 (24.2) | 9 (32.1) | ||
| FACULTY-RELATED FACTORS | ||||
| Insufficient time for teaching due to intense patient agenda | 43 (69.4) | 20 (71.4) | χ2 (3) = 9.15 | |
| Lack of training/retraining for faculty to teach medical students in ACC | 1 (1.6) | 1 (3.6) | ||
| Not feeling comfortable to have students in my clinic | 2 (3.2) | 5 (17.6) | ||
| Not integrated as part of my current KPI | 16 (25.8) | 2 (7.1) | ||
| PATIENT-RELATED FACTORS | ||||
| Fear of patient dissatisfaction | 16 (25.8) | 6 (21.4) | χ2 (3) = 1.34 | 0.72 |
| Lack of suitable patients for teaching | 9 (14.5) | 3 (10.7) | ||
| No follow-up/continuity of care for cases attended | 14 (22.6) | 5 (17.9) | ||
| Patients’ refusal to be seen by medical students | 23 (37.1) | 14 (50) | ||
| STUDENT-RELATED FACTORS | ||||
| Increasing numbers of students | 31 (50) | 13 (46.4) | χ2 (1) = 0.10 | 0.754 |
| Lack of student’s commitment and interest in learning | 31 (50) | 15 (53.6) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almushait, Y.B.; Alabdaljabar, M.S.; Alkhani, K.; Abdalla, H.M.; Alhayaza, R.; Temsah, M.-H.; Alsohaibani, F. Challenges Facing Undergraduate Medical Education in Ambulatory Care Clinics at Tertiary Care Hospitals. Healthcare 2022, 10, 496. https://doi.org/10.3390/healthcare10030496
Almushait YB, Alabdaljabar MS, Alkhani K, Abdalla HM, Alhayaza R, Temsah M-H, Alsohaibani F. Challenges Facing Undergraduate Medical Education in Ambulatory Care Clinics at Tertiary Care Hospitals. Healthcare. 2022; 10(3):496. https://doi.org/10.3390/healthcare10030496
Chicago/Turabian StyleAlmushait, Youssef B., Mohamad S. Alabdaljabar, Khalid Alkhani, Hesham M. Abdalla, Raid Alhayaza, Mohamad-Hani Temsah, and Fahad Alsohaibani. 2022. "Challenges Facing Undergraduate Medical Education in Ambulatory Care Clinics at Tertiary Care Hospitals" Healthcare 10, no. 3: 496. https://doi.org/10.3390/healthcare10030496
APA StyleAlmushait, Y. B., Alabdaljabar, M. S., Alkhani, K., Abdalla, H. M., Alhayaza, R., Temsah, M.-H., & Alsohaibani, F. (2022). Challenges Facing Undergraduate Medical Education in Ambulatory Care Clinics at Tertiary Care Hospitals. Healthcare, 10(3), 496. https://doi.org/10.3390/healthcare10030496







