1. Introduction
Idiopathic scoliosis, for which the causes are unknown, comprises 85% of all reported cases of scoliosis. It mostly occurs during puberty, from the age of 10 through to the adolescent period, until bone growth stops [
1]. At the end of the deformation process, the resultant spinal deformity causes severe functional disorders (e.g., cardiopulmonary conditions and kyphosis) [
2,
3,
4]. Spinal deformity mainly leads to progressive thoracolumbar curvature. When the curve reaches 40°, balance issues arise in the trunk and the upper extremities are used to maintain an upright posture. At 80°, the ribs and pelvis touch each other, leading to severe pain. At a curve of >80°, pulmonary function begins to deteriorate [
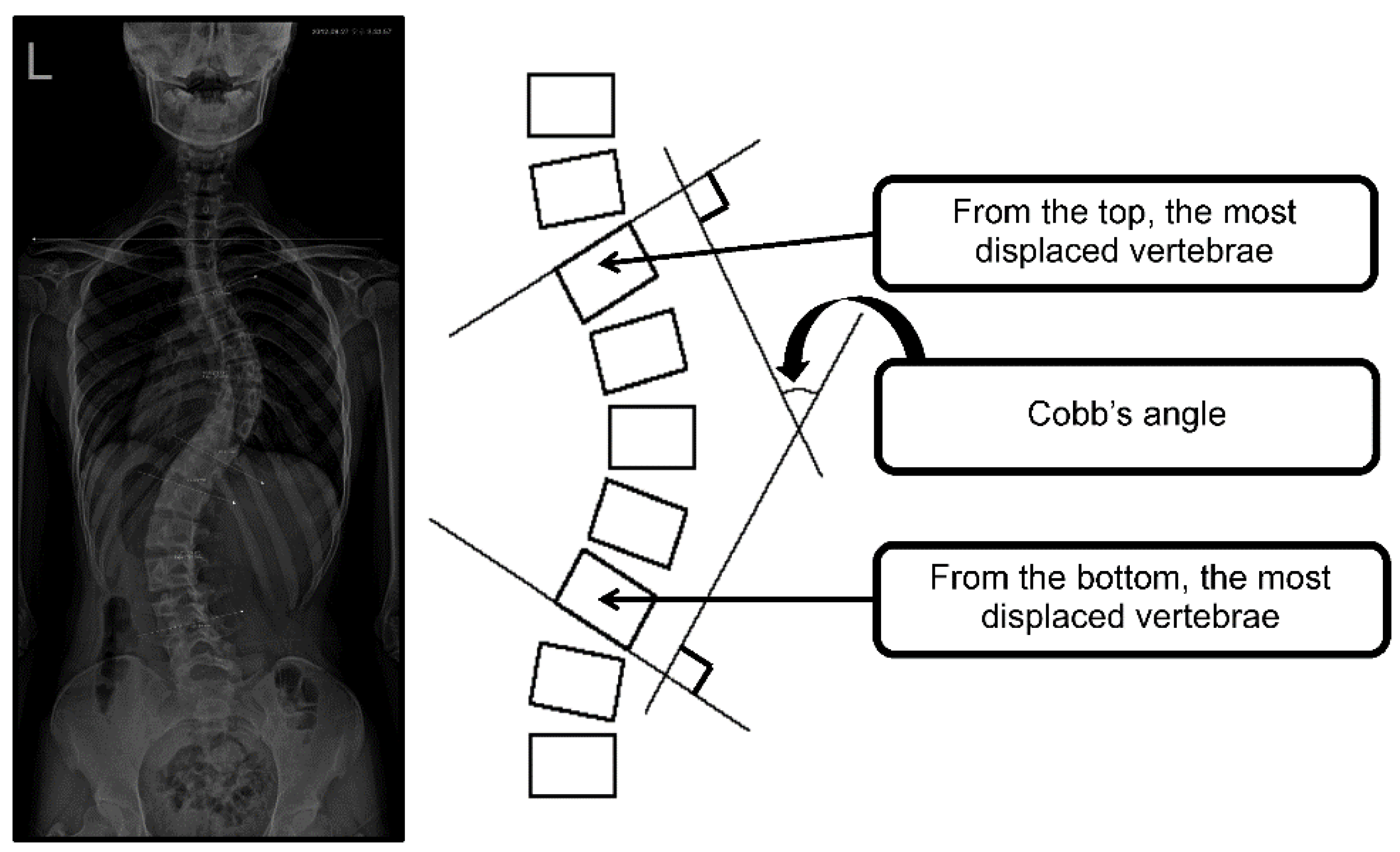
5]. Acting to standardize reports of non-operative research, recommendations by the Scoliosis Research Society (SRS) identify the Cobb’s angle as the primary outcome [
6]. When the Cobb’s angle is >50° and physiologic deterioration is apparent (decreased lung capacity due to narrowing of the diameter of the rib cage, a decrease in proteoglycan and glycoprotein, and an increase of collagen concentration in the nucleus pulposus), surgery is considered [
4]. In other cases, treatment involves conservative methods, such as spinal bracing, manipulation, physical therapy, and prescribed exercise [
7,
8]. Early diagnosis and treatment are therefore essential for idiopathic scoliosis [
9], with early treatment involving spinal bracing, surgery, and directed exercise.
The aim of exercise therapy is to correct muscular imbalance. However, excessive and inappropriate exercise without a precise radiographic diagnosis and physical assessment may interrupt treatment and worsen the condition [
10]. Schroth rehabilitation exercises (SRE) provide stable outcomes and high patient satisfaction [
11,
12]. SRE is a three-dimensional (3-D) exercise method that corrects scoliosis with improvement in body shape and respiratory capacity through the application of rotational breathing [
13]. Similar to a compressed ball that regains its original shape through the injection of air, the SRE respiration technique applies 3-D exercise with optimum feedback to correct scoliosis curvature and deviation [
14].
SRE differs markedly from the standard correction exercises that have previously been used to treat scoliosis [
15,
16]. The advantage of SRE is that patients can more accurately perceive their image in terms of postural imbalance due to scoliosis and improve their abnormal posture in response by intentionally changing their breathing [
13]. Several studies on SRE have reported that severe spinal curvature, pain, muscular endurance, self-image, and surface topography characteristics were improved after exercise intervention [
11,
17,
18]. Moreover, an increase in the calcaneal valgus angle negatively affects the pelvic alignment [
19] and the stability of the standing posture [
20]. Park et al. [
21] reported a positive correlation between idiopathic scoliosis and calcaneal valgus angle. Additionally, eversion of the calcaneus significantly increases hip flexion, hip internal rotation, anterior pelvic tilt, thoracic lateral tilt, and axial rotation in the standing position [
22]. This indicates that the association between the shape and position of the feet and postural alignment occurs through a functional connection between the foot and distal joints and that the closed kinetic chain mediates the movement of the lower extremities [
23]. In a study of 16 children with foot deformities, Rasool et al. [
24] reported an association of foot deformity with spinal abnormalities. Therefore, SRE appears to improve postural balance and reduce the curvature of scoliosis through strengthening the intercostal muscles and promoting normalization of the diaphragmatic and respiratory muscles [
7].
As idiopathic scoliosis occurs spontaneously and progresses slowly, early detection and treatment are essential to reduce the requirement for surgery, alleviate psychological distress, and improve the correction rate. Early treatment using exercise is optimal for some patients [
25]. In a previous study concerning idiopathic scoliosis, SRE performed in clinics under the guidance of exercise specialists significantly reduced the rate of change in Cobb’s angle and rotation angles. Compared to conventional exercises, SRE was more effective in increasing chest expansion, lung capacity, and muscle strength [
11,
26,
27]. In addition, 8 weeks of SRE led to positive improvements in the spine angle, chest expansion, and static balance [
28]. While some studies have verified the effects of SRE on Cobb’s angle [
26], there have been few reports on changes in the calcaneal valgus angle and lower extremity alignment according to the degree of spinal deformity. Furthermore, we set additional goals to reduce pain and improve appearance through increasing stability in terms of controlling foot movement and biomechanically reducing postural asymmetry.
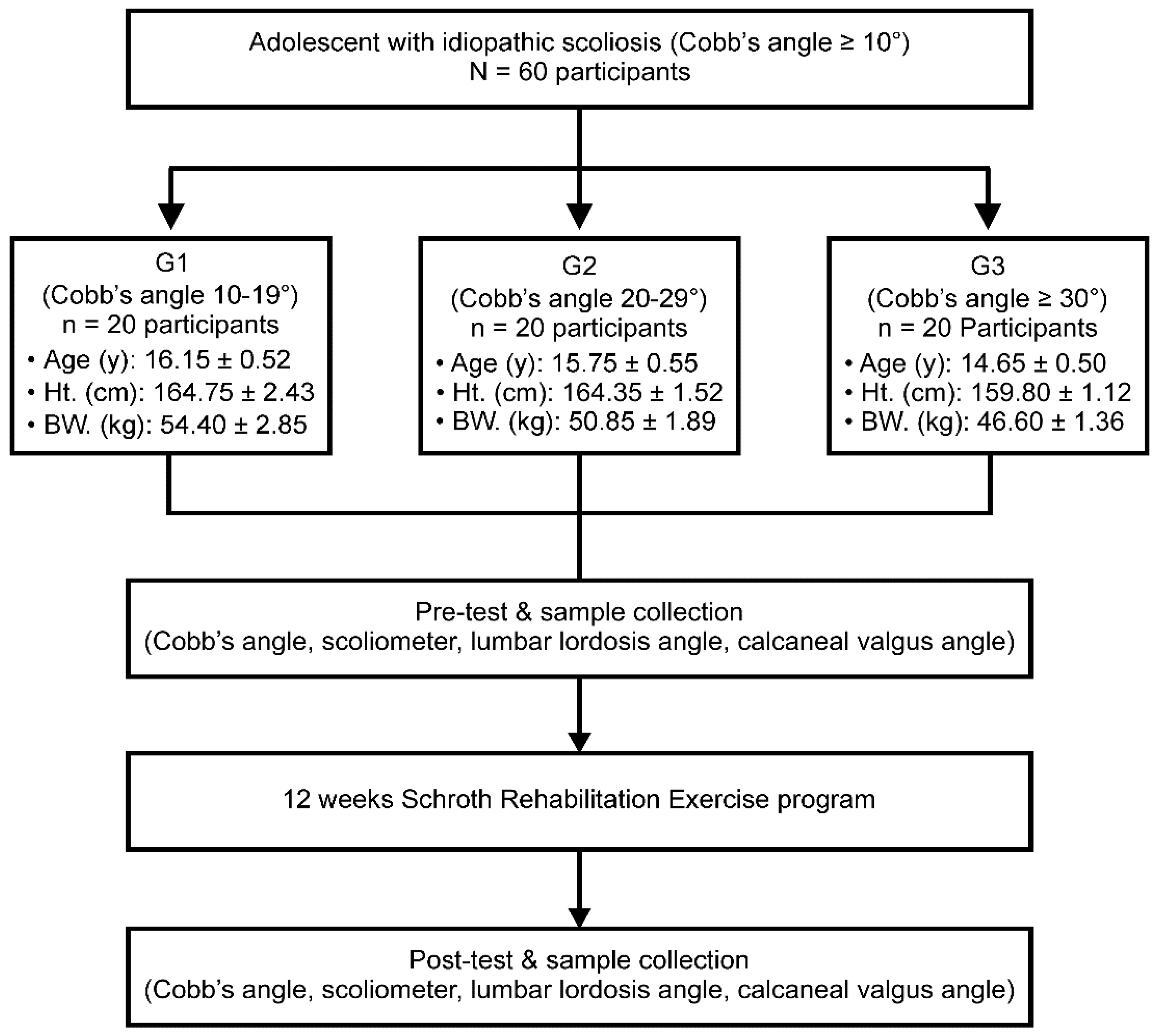
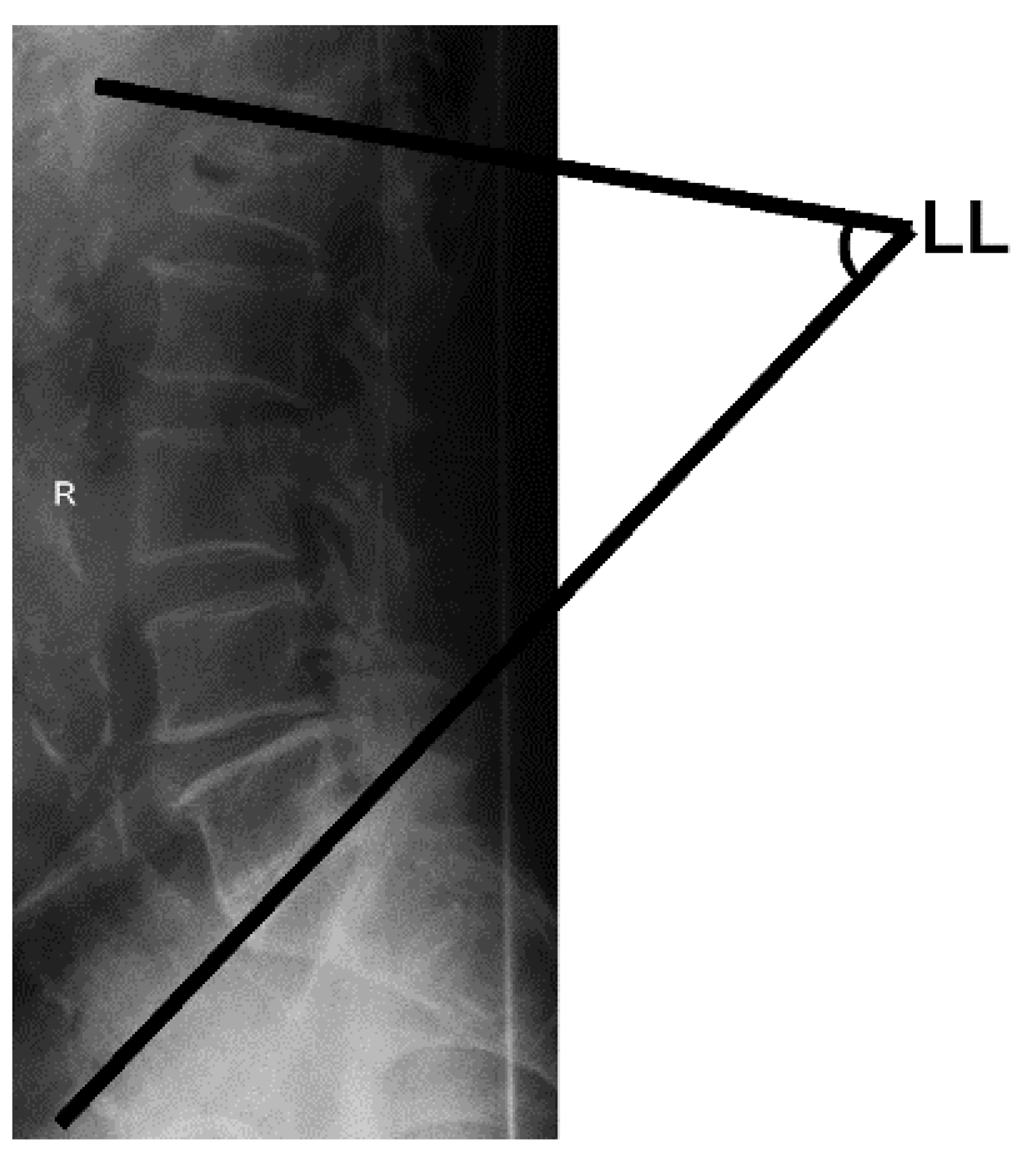
This study classified teenagers who had been diagnosed with scoliosis into three groups according to the Cobb’s angle. This study aimed to verify the effects of the application of SRE, characterized as a 3-D intervention, in the body posture by measuring and analyzing changes in Cobb’s angle, scoliometer readings, total lumbar lordosis, and calcaneal valgus angles. In addition, this study considered whether SRE improved these parameters regardless of the severity of scoliosis. Changes in scoliosis severity were reviewed in each group to assess the effectiveness of the rehabilitation program and to establish a foundation for the clinical application of SRE.
4. Discussion
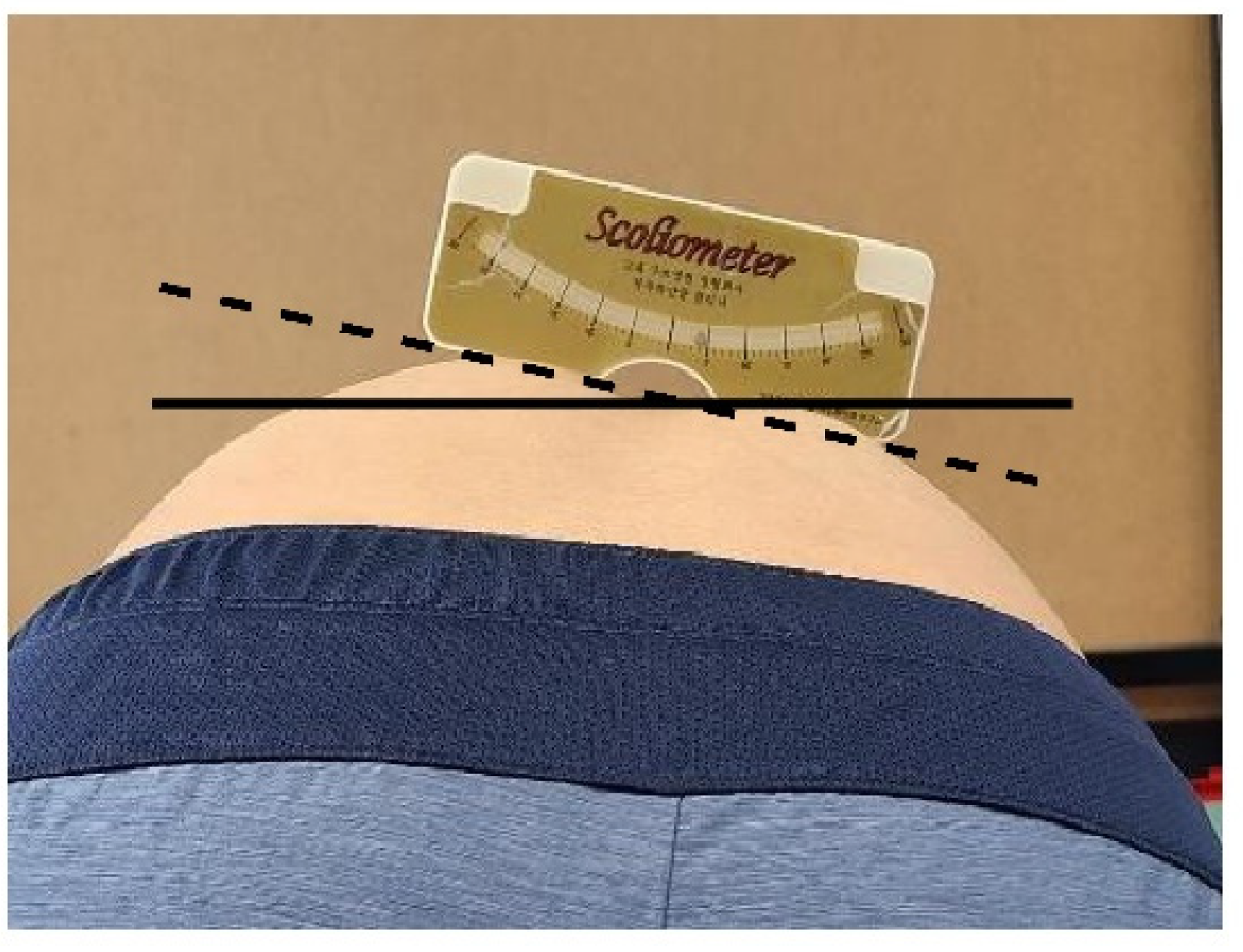
This study evaluated the factors related to the closed kinetic chain to investigate the positive effects of exercise in patients with adolescent idiopathic scoliosis. These factors included the Cobb’s angle, which is a key indicator of scoliosis after SRE intervention, and scoliometer readings, lumbar lordosis, and calcaneal valgus angle, which are related to body stability. The Cobb’s angle is classified according to the degree of scoliosis: curves <25° are considered mild scoliosis, values between 25° and 45° are moderate, and curves ≥45° are severe [
35]. Particularly, a spine curvature of >30° at the end of the growth phase significantly increases the risk of complications in adulthood, including pain, chest and shoulder girdle deformities, reduced quality of life (QOL), various physical disabilities, and major respiratory problems [
35,
36]. Previous studies have reported that SRE had a significant effect on the treatment of scoliosis [
37]. As a result of applying short-term rehabilitation composed of SRE for 7 days to 34 patients with adolescent idiopathic scoliosis with an average Cobb’s angle of 28.7 degrees, the angle of trunk rotation significantly decreased from 11.5 to 8.4 degrees, and the thoracic curves significantly decreased from 8.9 degrees to 6.5 degrees [
28]. In this study, there were significant changes in the Cobb’s angle, which is the most important indicator of scoliosis diagnosis, in all three groups compared to that before the SRE intervention. In particular, the most significant change was in the moderate scoliosis or higher group with a Cobb’s angle between 30° and 39°. Additionally, the scoliometer readings and lumbar lordosis, which are indirect indicators of the Cobb’s angle, significantly improved after the 12-week SRE program.
SRE is proposed as a special program used to treat idiopathic scoliosis in young adolescents [
17]. Fusco et al. [
37] reported that a meta-analysis of SRE showed significant improvement in back muscle strength and respiratory function in patients with scoliosis, as well as slowed curve progression and a reduced Cobb’s angle. Moreover, in addition to improving various elements of scoliosis, function, and QOL, Schreiber et al. [
12] reported that SRE is very useful for adolescents with a curve between 10° and 45°, and is very effective for psychological stability as it greatly increases self-esteem. The variables ultimately evaluated in this study were to confirm the possibility of restoring correct posture; the change of Cobb’s angle through SRE was assessed through scoliometer readings and lumbar lordosis, and posture was confirmed by the calcaneal valgus angle.
Rib humps and posterior thoracic deformities were partially reduced with a rotational breathing treatment. As the mechanisms involved in lumbar and thoracic movement on lateral bending differ, this difference may be a significant indicator when analyzing changes in the severity of scoliosis. Additionally, Schreiber et al. [
38] reported that posture balance and signs and symptoms of scoliosis were improved after 6 months of SRE in adolescent patients with idiopathic scoliosis of 10° to 45°, regardless of orthosis usage. The patients’ conditions improved despite the Cobb’s angle not improving beyond the generally accepted threshold of 5°. In our study, positive changes in scoliometer readings, lumbar lordosis, and calcaneal valgus angle were observed in all groups after SRE regardless of the severity of scoliosis. Therefore SRE led to a basic improvement of the Cobb’s angle, improvement of normal postural alignment, static/dynamic postural control, and correction of spinal stability. Our findings align with the ultimate goal of SRE reported by Schreiber et al. [
12], which is to improve QOL through sensory movement, posture recovery, and breathing exercises.
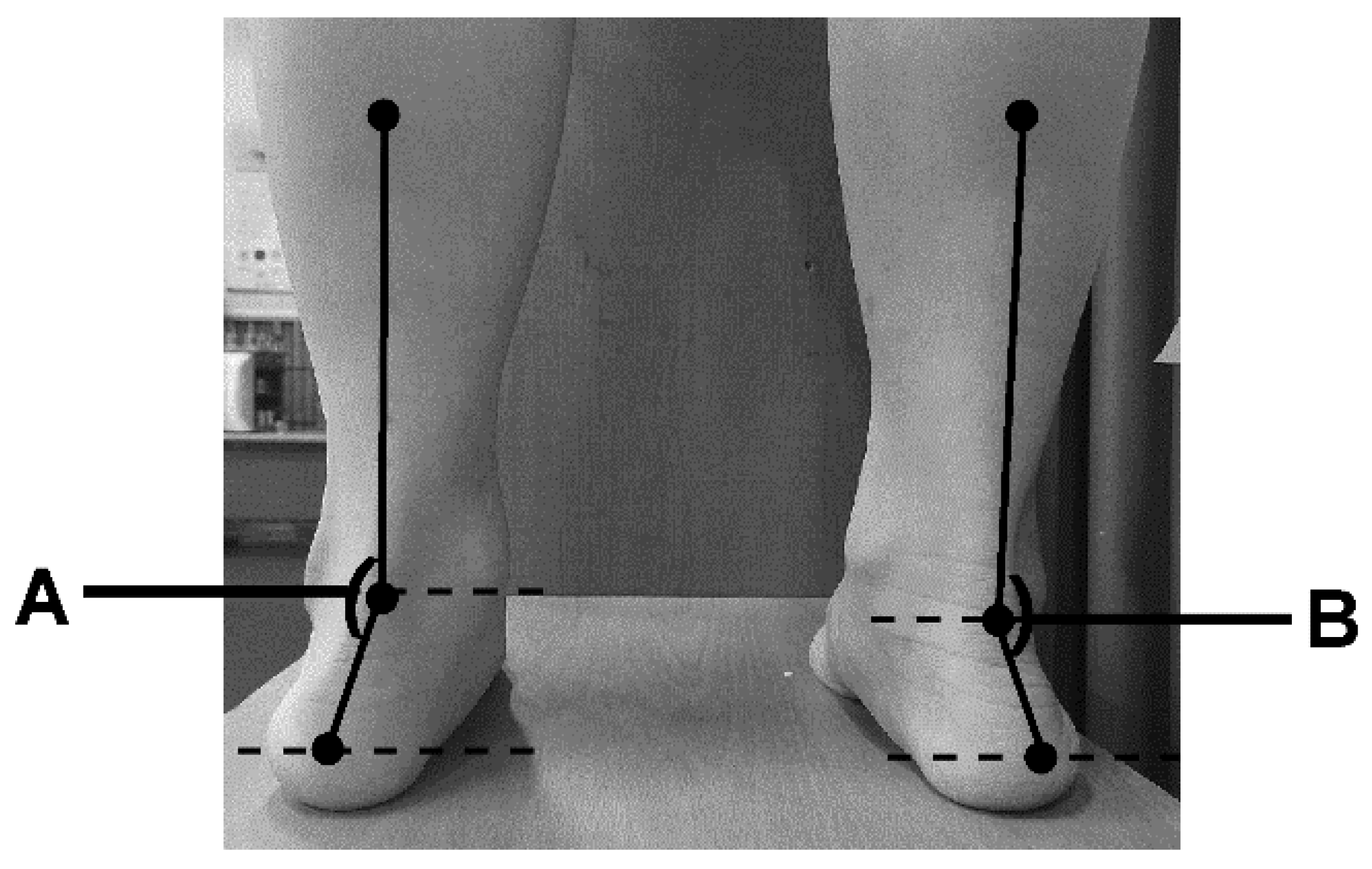
In this study, Schroth 3-D motion was shown to delay an additional increase in curvature and to increase the structural stability of the body, as reported in a previous study [
39]. Meanwhile, a significant correlation was reported between idiopathic scoliosis (with a Cobb’s angle 15–60°) and the tibio-calcaneal angle in a previous study on the correlation between scoliosis and physical alignment in 70 adolescents [
40]. Postural asymmetry is also associated with a risk of progression to idiopathic scoliosis. The curvature of scoliosis can generally be viewed as a difference in the left and right anatomical calcaneal valgus angle and leg length [
41], which is consistent with the difference in the calcaneus valgus angle found in participants in the SRE program in this study. Rehabilitative exercise has been considered to have a positive effect on body balance recovery by reducing the deviation in spinal curvature angles and in lower extremity malalignment. Generally, patients with scoliosis have significantly less balancing ability when standing than those without scoliosis [
42]. In terms of the pathogenesis of scoliosis, the spine is flexed to one side as the 3-D deformation of the spine occurs due to an imbalance in the foot, such as when the body load is generally concentrated on one foot. Therefore, it has been reported that a change in the angle of the foot that then supports the weight of both feet is a factor that can affect the prognosis of the disease. [
43]. Balance is the ability to maintain a center of gravity on the base of support in a given environment and is an essential factor for spinal movement and stability [
44]. Szulc et al. [
45] reported that in patients with only right-sided thoracic scoliosis, more weight was loaded on their right side than on their left. The evaluation of the foot’s calcaneal angle is a method for assessing postural stability and is a validated tool to measure the structure of the foot based on static equilibrium [
46]. The normal range of the calcaneal angle is 2°–8° of calcaneal varus/inversion [
47]. However, Gauchard et al. [
48] concluded that the weight load in patients with scoliosis could vary according to the level, extent, and type of curvature. Unlike previous studies, this study showed significant changes in the calcaneal valgus angle after exercise using a two-dimensional analysis system. In this study, after applying the same program to all groups, the calcaneal valgus angle returned to normal in all three groups.
Balance control is achieved through complex exercise control with inertial response and nervous system processing, and a change in sensory information immediately affects balance control [
49]. In one study, 0.5% postural body sway was observed in individuals without scoliosis, as opposed to 14.5% in patients with scoliosis [
50]. In a 4-month study involving trunk rotation exercise in 12 adolescent males and females with idiopathic scoliosis, Mooney et al. [
51] reported that asymmetric muscle strength completely recovered, whereas balance and Cobb’s angles significantly worsened. An exercise program should be individualized according to the type and extent of scoliotic curvature. Neumann reported that thoracic and lumbar axis rotating mechanisms differ from a kinematics perspective [
34]. Tension around the lumbar vertebrae transmits structural instability to the upper thoracic spine, and this abnormal spinal tension generates cross-stress effects around the thoracic spine, leading to secondary rotational displacement scoliosis. However, thoracic torsion generally occurs in the opposite direction to generate cross balance with lumbar torsion [
52], which supports the premise that the type and magnitude of scoliosis curvature require different exercise programs [
53]. Although SRE is based on the five principles of axis elongation, reverse bending, reverse rotation, facilitation, and stabilization, the characteristics and merits of each exercise differ. In this study, the SRE program did not apply traditional traction therapy, as SRE routines consolidate the breathing method and address inactive muscles, and a 3-D exercise for spinal deformity and scoliosis was applied using a rib as a lever. The program in this study also applied aerobic capacity improvement through a fixed bicycle exercise, lumbopelvic stabilization through a muscle cylinder exercise, and stabilization of each segment of the spine through isometric exercise. Lastly, SRE had a positive effect on vertebral rotation and scoliosis curvature and may have improved the asymmetric thoracic-lumbar rotation angle and vertebral deviation due to simultaneous reverse bending and rotation during exercise.
Passive treatment such as the use of a scoliosis brace has limitations in achieving high muscle strength improvement and normal balance [
54]. Thus, in adolescent patients with idiopathic scoliosis, active rehabilitation exercises such as SRE can improve scoliometer readings, lumbar lordosis, and the calcaneal valgus angle, thereby enhancing spinal muscle function and balance ability. Furthermore, it is thought that positive effects can be obtained in daily life and sports activities. One limitation of this study was that we could not accurately measure the change in mobility due to rib asymmetry and scoliosis, and failed to evaluate the difference in the ventilation capacity of the lungs due to reduced mobility. In addition, to verify the effect more clearly, the SRE group was compared with the control group treated only with conservative treatment. However, an SRE group including various variables that can evaluate the angle of trunk rotation, Cobb’s angle, Risser sign, the angle of spine rotation on X-ray, and QOL is required. Future studies need to identify these physiological factors and consider the variables evaluated in this study.