Antibiotic Usage in Surgical Prophylaxis: A Retrospective Study in the Surgical Ward of a Governmental Hospital in Riyadh Region
Abstract
1. Introduction
2. Materials and Methods
3. Results
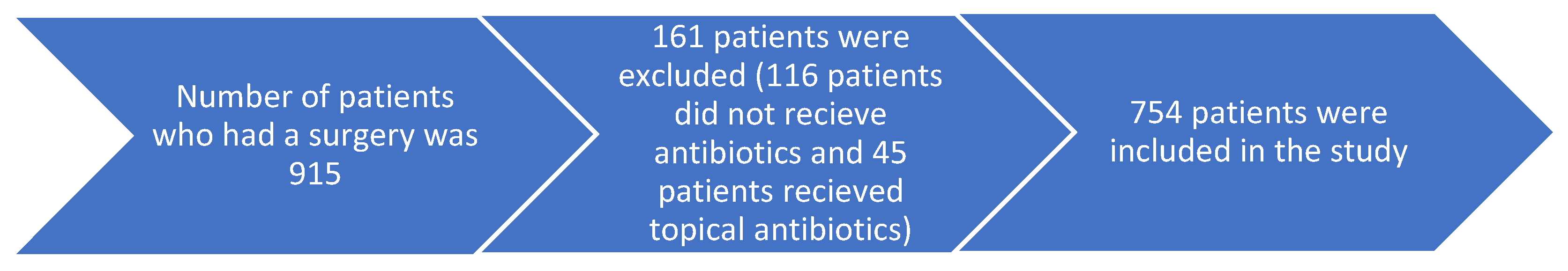
3.1. Number and Percentage of Patients Who Received Antibiotics
3.2. The Most Prescribed Antibiotics in the Surgical Ward
3.3. The Personal Data of the Patients Who Received Antibiotics in the Surgical Ward
4. Discussion
5. Limitation and Strength
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Haque, M.; Sartelli, M.; McKimm, J.; Abu Bakar, M. Health care-associated infections—An overview. Infect. Drug Resist. 2018, 11, 2321–2333. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Types of Healthcare-Associated Infections. Available online: https://www.cdc.gov/hai/infectiontypes.html (accessed on 21 January 2022).
- Klevens, R.M.; Edwards, J.R.; Richards, C.L., Jr.; Horan, T.C.; Gaynes, R.P.; Pollock, D.A.; Cardo, D.M. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007, 122, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Kefale, B.; Tegegne, G.T.; Degu, A.; Molla, M.; Kefale, Y. Surgical site infections and prophylaxis antibiotic use in the surgical ward of public hospital in Western Ethiopia: A hospital-based retrospective cross-sectional study. Infect. Drug Resist. 2020, 13, 3627–3635. [Google Scholar] [CrossRef] [PubMed]
- Allegranzi, B.; Bagheri Nejad, S.; Combescure, C.; Graafmans, W.; Attar, H.; Donaldson, L.; Pittet, D. Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis. Lancet 2011, 377, 228–241. [Google Scholar] [CrossRef]
- World Health Organization. Global Guidelines for the Prevention of Surgical Site Infection. Available online: https://www.who.int/gpsc/global-guidelines-web.pdf (accessed on 21 January 2022).
- Gouvêa, M.; Novaes, C.D.O.; Pereira, D.M.T.; Iglesias, A.C. Adherence to guidelines for surgical antibiotic prophylaxis: A review. Braz. J. Infect. Dis. 2015, 19, 517–524. [Google Scholar] [CrossRef]
- Hall, C.; Allen, J.; Barlow, G. Antibiotic prophylaxis. Surgery 2012, 30, 651–658. [Google Scholar] [CrossRef]
- Alavi, S.M.; Roozbeh, F.; Behmanesh, F.; Alavi, L. Antibiotics use patterns for surgical prophylaxis site infection in different surgical wards of a teaching hospital in Ahvaz, Iran. Jundishapur J. Microbiol. 2014, 7, e12251. [Google Scholar] [CrossRef]
- Bedouch, P.; Labarère, J.; Chirpaz, E.; Allenet, B.; Lepape, A.; Fourny, M.; Pavese, P.; Girardet, P.; Merloz, P.; Saragaglia, D.; et al. Compliance with guidelines on antibiotic prophylaxis in total hip replacement surgery: Results of a retrospective study of 416 patients in a teaching hospital. Infect. Control Hosp. Epidemiol. 2004, 25, 302–307. [Google Scholar] [CrossRef]
- Herawati, F.; Yulia, R.; Hak, E.; Hartono, A.H.; Michiels, T.; Woerdenbag, H.J.; Avanti, C. A retrospective surveillance of the antibiotics prophylactic use of surgical procedures in private hospitals in Indonesia. Hosp. Pharm. 2019, 54, 323–329. [Google Scholar] [CrossRef]
- Enzler, M.J.; Berbari, E.; Osmon, D.R. Antimicrobial prophylaxis in adults. Mayo Clin. Proc. 2011, 86, 686–701. [Google Scholar] [CrossRef]
- Ahmed, N.J.; Jalil, M.A.; Al-Shdefat, R.I.; Tumah, H.N. The practice of preoperative antibiotic prophylaxis and the adherence to guideline in Riyadh hospitals. Bull. Environ. Parmacology Life Sci. 2015, 5, 8–14. [Google Scholar]
- Alghamdi, S.; Berrou, I.; Aslanpour, Z.; Mutlaq, A.; Haseeb, A.; Albanghali, M.; Hammad, M.A.; Shebl, N. Antimicrobial stewardship programmes in Saudi hospitals: Evidence from a national survey. Antibiotics 2021, 10, 193. [Google Scholar] [CrossRef] [PubMed]
- Hammad, M.A.; AL-Akhali, K.M.; Mohammed, A.T. Evaluation of surgical antibiotic prophylaxis in aseer area hospitals in kingdom of Saudi Arabia. J. Phys. Clin. Sci. 2013, 6, 1–7. Available online: https://www.arpapress.com/Volumes/JPCS/Vol6/JPCS_6_01.pdf (accessed on 21 January 2022).
- Tolba, Y.Y.A.; El-Kabbani, A.O.; Al-Kayyali, N.S. An observational study of perioperative antibiotic-prophylaxis use at a major quaternary care and referral hospital in Saudi Arabia. Saudi J. Anaesth. 2018, 12, 82–88. [Google Scholar] [CrossRef]
- World Health Organization. WHO Policy Guidance on Integrated Antimicrobial Stewardship Activities. Available online: https://www.who.int/publications/i/item/9789240025530 (accessed on 21 January 2022).
- Saudi Ministry of Health. Surgical Prophylaxis Guidelines. Available online: https://www.moh.gov.sa/en/CCC/healthp/regulations/Documents/National%20Antimicrobial%20%20Guidelines.pdf (accessed on 21 January 2022).
- Bennett, N.J.; Bull, A.L.; Dunt, D.R.; Russo, P.L.; Spelman, D.W.; Richards, M.J. Surgical antibiotic prophylaxis in smaller hospitals. ANZ J. Surg. 2006, 76, 676–678. [Google Scholar] [CrossRef]
- Cooke, E.M.; Coello, R.; Sedgwick, J.; Ward, V.; Wilson, J.; Charlett, A.; Ward, B.; Pearson, A. A national surveillance scheme of hospital associated infections in England. J. Hosp. Infect. 2000, 46, 1–3. [Google Scholar] [CrossRef]
- Fennessy, B.G.; O’sullivan, M.J.; Fulton, G.J.; Kirwan, W.O.; Redmond, H.P. Prospective study of use of perioperative antimicrobial therapy in general surgery. Surg. Infect. 2006, 7, 355–360. [Google Scholar] [CrossRef]
- Sumiyama, Y.; Kusachi, S.; Yoshida, Y.; Arima, Y.; Tanaka, H.; Nakamura, Y.; Nagao, J.; Saida, Y.; Watanabe, M.; Sato, J. Questionnaire on perioperative antibiotic therapy in 2003: Postoperative prophylaxis. Surg. Today 2006, 36, 107–113. [Google Scholar] [CrossRef]
- Gul, Y.A.; Hong, L.C.; Prasannan, S. Appropriate antibiotic administration in elective surgical procedures. Asian J. Surg. 2005, 28, 104–108. [Google Scholar] [CrossRef]
- Andrajati, R.; Vlček, J.; Kolar, M.; Pípalová, R. Survey of surgical antimicrobial prophylaxis in Czech republic. Pharm. World Sci. 2005, 27, 436–441. [Google Scholar] [CrossRef]
- Castella, A.; Charrier, L.; Di Legami, V.; Pastorino, F.; Farina, E.C.; Argentero, P.A.; Zotti, C.M.; Piemonte Nosocomial Infection Study Group. Surgical site infection surveillance: Analysis of adherence to recommendations for routine infection control practices. Infect. Control Hosp. Epidemiol. 2006, 27, 835–840. [Google Scholar] [CrossRef] [PubMed]
- Gagliotti, C.; Ravaglia, F.; Resi, D.; Moro, M.L. Quality of local guidelines for surgical antimicrobial prophylaxis. J. Hosp. Infect. 2004, 56, 67–70. [Google Scholar] [CrossRef] [PubMed]
- Sohn, A.H.; Parvez, F.M.; Vu, T.; Hai, H.H.; Bich, N.N.; Le Thi, A.T.; Le Thi, T.H.; Thanh, N.H.; Viet, T.V.; Archibald, L.K.; et al. Prevalence of surgical-site infections and patterns of antimicrobial use in a large tertiary care hospital. Infect. Control Hosp. Epidemiol. 2002, 23, 382–387. [Google Scholar] [CrossRef] [PubMed]
- Alemkere, G. Antibiotic usage in surgical prophylaxis: A prospective observational study in the surgical ward of Nekemte referral hospital. PLoS ONE 2018, 13, e0203523. [Google Scholar] [CrossRef] [PubMed]
- Mohamoud, S.A.; Yesuf, T.A.; Sisay, E.A. Utilization assessment of surgical antibiotic prophylaxis at Ayder Referral hospital, Northern Ethiopia. J. Appl. Pharm. 2016, 8, 1–5. [Google Scholar] [CrossRef]
- van Kasteren, M.E.; Kullberg, B.J.; de Boer, A.S.; Mintjes-de Groot, J.; Gyssens, I.C. Adherence to local hospital guidelines for surgical antimicrobial prophylaxis: A multicentre audit in Dutch hospitals. J. Antimicrob. Chemother. 2003, 51, 1389–1396. [Google Scholar] [CrossRef]
- Oh, A.L.; Goh, L.M.; Nik Azim, N.A.; Tee, C.S.; Shehab Phung, C.W. Antibiotic usage in surgical prophylaxis: A prospective surveillance of surgical wards at a tertiary hospital in Malaysia. J. Infect. Dev. Ctries. 2014, 8, 193–201. [Google Scholar] [CrossRef]
- Al-Azzam, S.I.; Alzoubi, K.H.; Mhaidat, N.M.; Haddadin, R.D.; Masadeh, M.M.; Tumah, H.N.; Magableh, A.; Maraqa, N.K. Preoperative antibiotic prophylaxis practice and guideline adherence in Jordan: A multi-centre study in Jordanian hospitals. J. Infect. Dev. Ctries. 2012, 6, 715–720. [Google Scholar] [CrossRef]
- Salkind, A.R.; Rao, K.C. Antiobiotic prophylaxis to prevent surgical site infections. Am. Fam. Physician 2011, 83, 585–590. [Google Scholar] [PubMed]
- Parulekar, L.; Soman, R.; Singhal, T.; Rodrigues, C.; Dastur, F.D.; Mehta, A. How good is compliance with surgical antibiotic prophylaxis guidelines in a tertiary care private hospital in India? A prospective study. Indian J. Surg. 2009, 71, 15–18. [Google Scholar] [CrossRef][Green Version]
- Musmar, S.M.; Baba, H.; Owais, A. Adherence to guidelines of antibiotic prophylactic use in surgery: A prospective cohort study in North West Bank, Palestine. BMC Surg. 2014, 14, 69. [Google Scholar] [CrossRef] [PubMed]
- Tourmousoglou, C.E.; Yiannakopoulou, E.C.; Kalapothaki, V.; Bramis, J.; St Papadopoulos, J. Adherence to guidelines for antibiotic prophylaxis in general surgery: A critical appraisal. J. Antimicrob. Chemother. 2008, 61, 214–218. [Google Scholar] [CrossRef]
- Khan, Z.; Ahmed, N.; Zafar, S.; Khan, F.U.; Saqlain, M.; Kamran, S.; Rahman, H. Audit of antibiotic prophylaxis and adherence of surgeons to standard guidelines in common abdominal surgical procedures. East. Mediterr. Health J. 2020, 26, 1052–1061. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Aziz, A.; El-Menyar, A.; Al-Thani, H.; Zarour, A.; Parchani, A.; Asim, M.; El-Enany, R.; Al-Tamimi, H.; Latifi, R. Adherence of surgeons to antimicrobial prophylaxis guidelines in a tertiary general hospital in a rapidly developing country. Adv. Pharmacol. Pharm. Sci. 2013, 2013, 842593. [Google Scholar] [CrossRef] [PubMed]
- Gouvêa, M.; Novaes, C.D.O.; Iglesias, A.C. Assessment of antibiotic prophylaxis in surgical patients at the Gaffrée e Guinle university hospital. Rev. Colégio Bras. Cir. 2016, 43, 225–234. [Google Scholar] [CrossRef]
| Antibiotic | Number | Percentage |
|---|---|---|
| Ceftriaxone | 397 | 28.44 |
| Metronidazole | 368 | 26.36 |
| Piperacillin/Tazobactam | 90 | 6.45 |
| Cefazolin | 71 | 5.09 |
| Gentamicin | 69 | 4.94 |
| Amoxicillin/Clavulanic acid | 68 | 4.87 |
| Meropenem | 67 | 4.80 |
| Ciprofloxacin | 59 | 4.23 |
| Imipenem/Cilastatin | 46 | 3.30 |
| Cefuroxime | 35 | 2.50 |
| Linezolid | 27 | 1.93 |
| Vancomycin | 26 | 1.86 |
| Azithromycin | 20 | 1.43 |
| Amoxicillin | 12 | 0.86 |
| Ceftazidime | 10 | 0.72 |
| Clindamycin | 10 | 0.72 |
| Doxycycline | 7 | 0.50 |
| Cefotaxime | 4 | 0.29 |
| Tigecycline | 4 | 0.29 |
| Amikacin | 1 | 0.07 |
| Cefepime | 1 | 0.07 |
| Colistin | 1 | 0.07 |
| Clarithromycin | 1 | 0.07 |
| Moxifloxacin | 1 | 0.07 |
| Ceftazidime/Avibactam | 1 | 0.07 |
| Total number of antibiotics | 1396 | 100 |
| Variable | Category | Number | Percentage |
|---|---|---|---|
| Gender | Male | 461 | 61.14% |
| Female | 293 | 38.86% | |
| Age | <10 | 38 | 5.04% |
| 10–19 | 44 | 5.83% | |
| 20–29 | 153 | 20.29% | |
| 30–39 | 172 | 22.81% | |
| 40–49 | 147 | 19.50% | |
| 50–59 | 101 | 13.40% | |
| >59 | 99 | 13.13% |
| Antibiotic | Capsule or Tablet | Syrup or Suspension | Vial or Ampule |
|---|---|---|---|
| Ceftriaxone | 0 | 0 | 397 |
| Metronidazole | 35 | 1 | 332 |
| Piperacillin/Tazobactam | 0 | 0 | 90 |
| Cefazolin | 0 | 0 | 71 |
| Gentamicin | 0 | 0 | 69 |
| Amoxicillin/Clavulanic acid | 22 | 6 | 40 |
| Meropenem | 0 | 0 | 67 |
| Ciprofloxacin | 24 | 0 | 35 |
| Imipenem/Cilastatin | 0 | 0 | 46 |
| Cefuroxime | 1 | 0 | 34 |
| Linezolid | 0 | 0 | 27 |
| Vancomycin | 0 | 0 | 26 |
| Azithromycin | 17 | 3 | 0 |
| Amoxicillin | 8 | 4 | 0 |
| Ceftazidime | 0 | 0 | 10 |
| Clindamycin | 0 | 0 | 10 |
| Doxycycline | 7 | 0 | 0 |
| Cefotaxime | 0 | 0 | 4 |
| Tigecycline | 0 | 0 | 4 |
| Amikacin | 0 | 0 | 1 |
| Cefepime | 0 | 0 | 1 |
| Colistin | 0 | 0 | 1 |
| Clarithromycin | 1 | 0 | 0 |
| Moxifloxacin | 1 | 0 | 0 |
| Ceftazidime/Avibactam | 0 | 0 | 1 |
| Total | 116 (8.31%) | 14 (1.00%) | 1266 (90.69%) |
| Antibiotic | 1 Day | 2 Days | 3 Days | 4 Days | 5 Days | 6 Days | 7 Days |
|---|---|---|---|---|---|---|---|
| Ceftriaxone | 3 | 14 | 25 | 3 | 57 | 0 | 295 |
| Metronidazole | 0 | 1 | 10 | 4 | 104 | 1 | 248 |
| Piperacillin/Tazobactam | 0 | 0 | 1 | 0 | 8 | 0 | 81 |
| Cefazolin | 6 | 3 | 27 | 0 | 21 | 1 | 13 |
| Gentamicin | 1 | 1 | 22 | 0 | 18 | 0 | 27 |
| Amoxicillin/Clavulanic acid | 3 | 1 | 6 | 1 | 10 | 1 | 46 |
| Meropenem | 0 | 0 | 0 | 0 | 0 | 3 | 64 |
| Ciprofloxacin | 0 | 0 | 3 | 0 | 12 | 0 | 44 |
| Imipenem/Cilastatin | 0 | 0 | 0 | 0 | 2 | 0 | 44 |
| Cefuroxime | 0 | 0 | 1 | 0 | 12 | 0 | 22 |
| Linezolid | 0 | 0 | 1 | 0 | 4 | 0 | 22 |
| Vancomycin | 0 | 0 | 1 | 0 | 1 | 0 | 24 |
| Azithromycin | 0 | 1 | 7 | 0 | 6 | 2 | 4 |
| Amoxicillin | 0 | 0 | 0 | 0 | 5 | 0 | 7 |
| Ceftazidime | 0 | 0 | 0 | 0 | 2 | 0 | 8 |
| Clindamycin | 0 | 0 | 2 | 0 | 4 | 0 | 4 |
| Doxycycline | 0 | 0 | 0 | 0 | 0 | 0 | 7 |
| Cefotaxime | 1 | 0 | 0 | 0 | 2 | 0 | 1 |
| Tigecycline | 1 | 0 | 0 | 0 | 0 | 0 | 3 |
| Amikacin | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Cefepime | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Colistin | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Clarithromycin | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Moxifloxacin | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Ceftazidime/Avibactam | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Total | 15 (1.08%) | 21 (1.51%) | 106 (7.59%) | 8 (0.57%) | 268 (19.20%) | 8 (0.57%) | 970 (69.48%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmed, N.; Balaha, M.; Haseeb, A.; Khan, A. Antibiotic Usage in Surgical Prophylaxis: A Retrospective Study in the Surgical Ward of a Governmental Hospital in Riyadh Region. Healthcare 2022, 10, 387. https://doi.org/10.3390/healthcare10020387
Ahmed N, Balaha M, Haseeb A, Khan A. Antibiotic Usage in Surgical Prophylaxis: A Retrospective Study in the Surgical Ward of a Governmental Hospital in Riyadh Region. Healthcare. 2022; 10(2):387. https://doi.org/10.3390/healthcare10020387
Chicago/Turabian StyleAhmed, Nehad, Mohamed Balaha, Abdul Haseeb, and Amer Khan. 2022. "Antibiotic Usage in Surgical Prophylaxis: A Retrospective Study in the Surgical Ward of a Governmental Hospital in Riyadh Region" Healthcare 10, no. 2: 387. https://doi.org/10.3390/healthcare10020387
APA StyleAhmed, N., Balaha, M., Haseeb, A., & Khan, A. (2022). Antibiotic Usage in Surgical Prophylaxis: A Retrospective Study in the Surgical Ward of a Governmental Hospital in Riyadh Region. Healthcare, 10(2), 387. https://doi.org/10.3390/healthcare10020387









