Tolerability on Serious Adverse Events of First-Line Bevacizumab and Cetuximab for RAS Wild-Type Metastatic Colorectal Cancer: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources and Search Strategy
2.2. Study Selection and Data Extraction
2.3. Assessment of Bias Risk and Evidence
2.4. Statistical Methods
3. Results
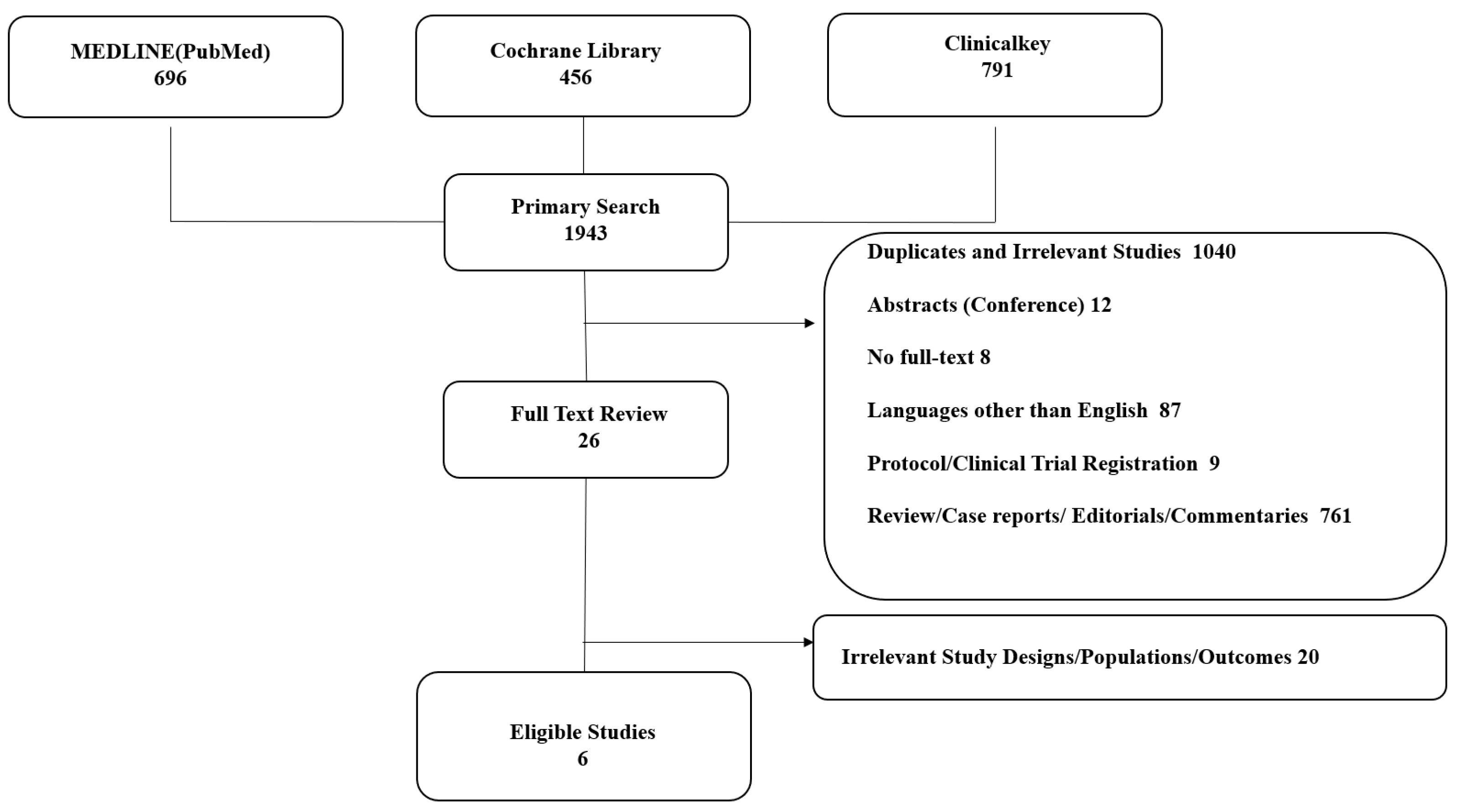
3.1. Study Search and Selection
3.2. Study Characteristics
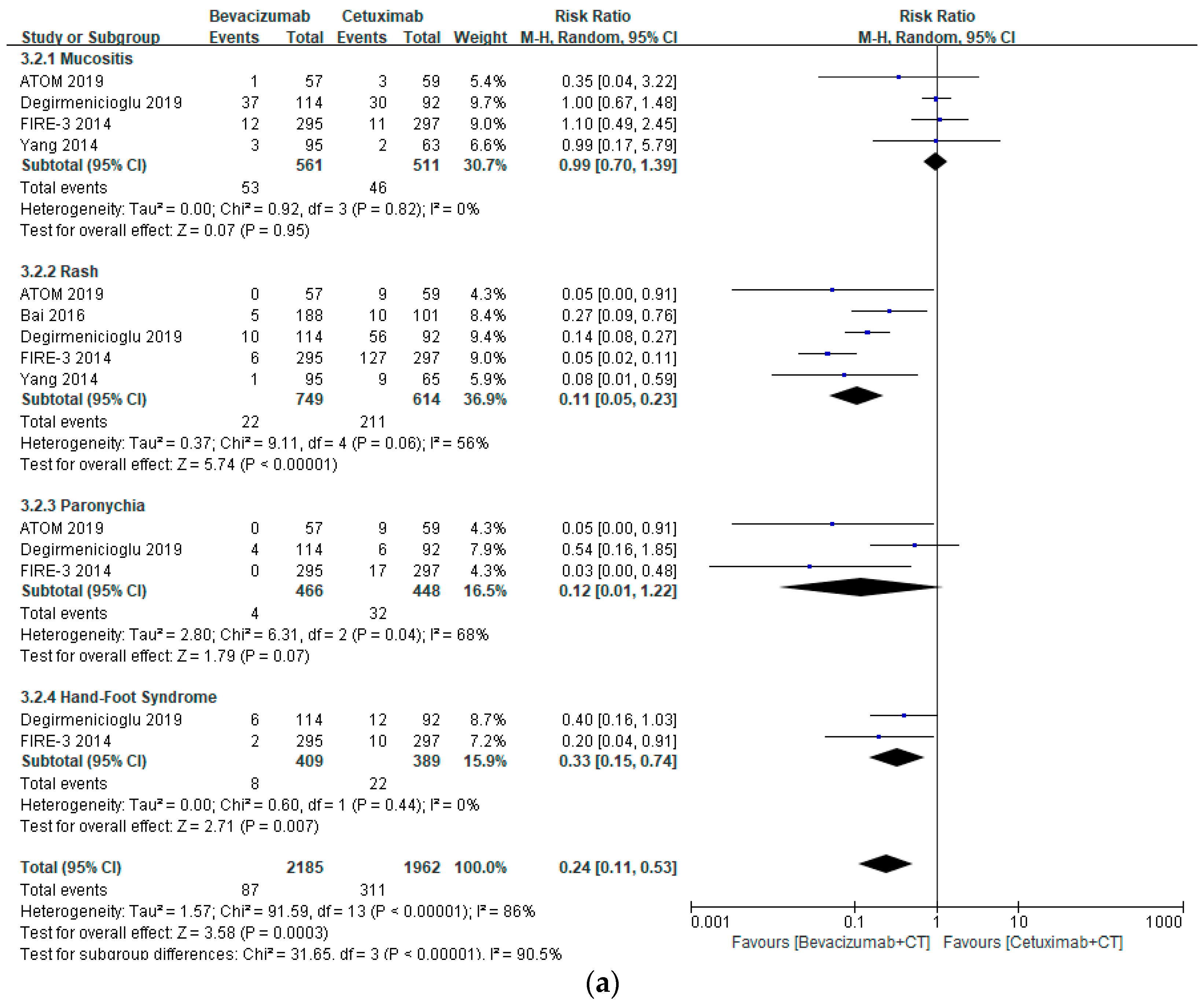
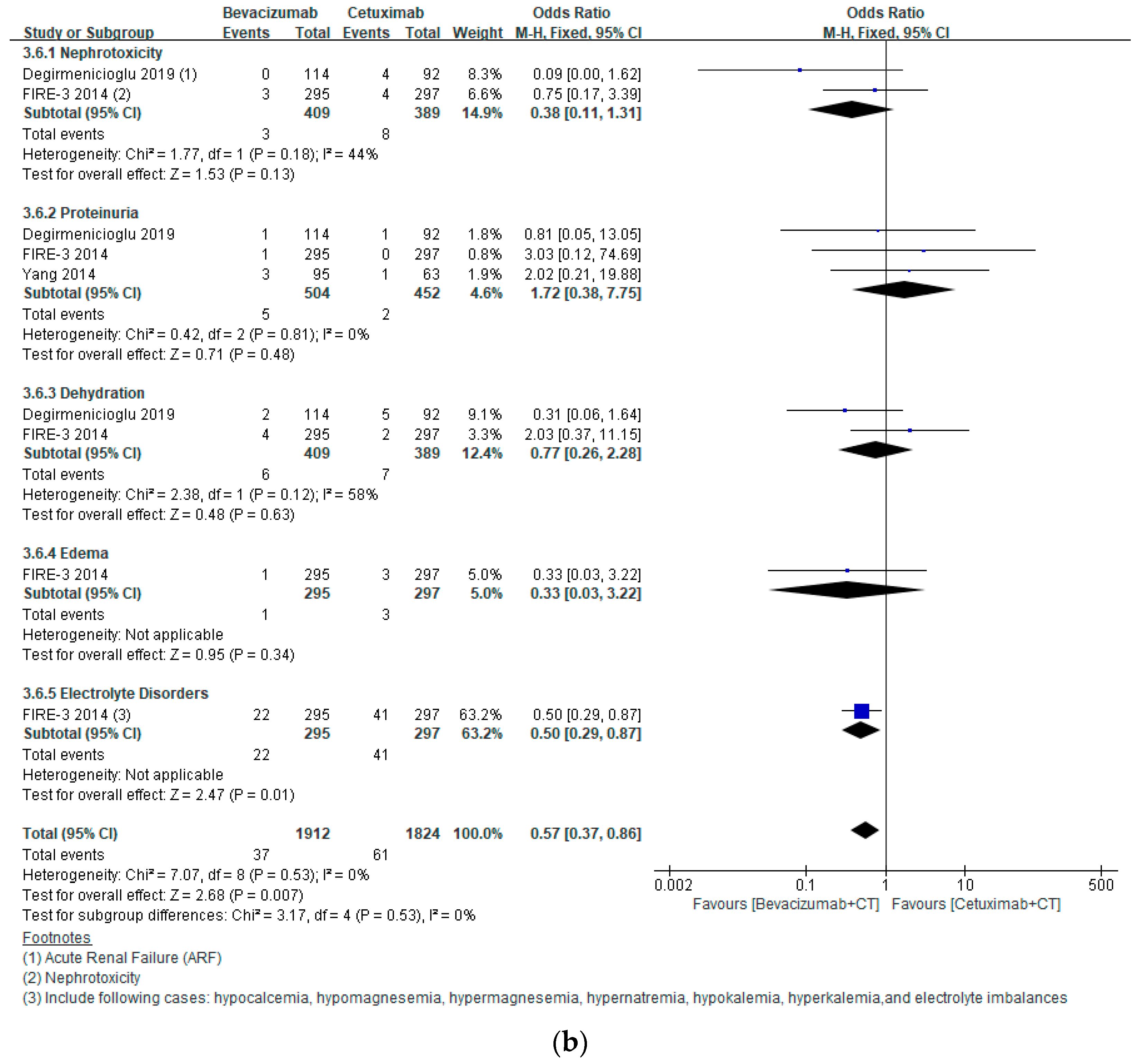
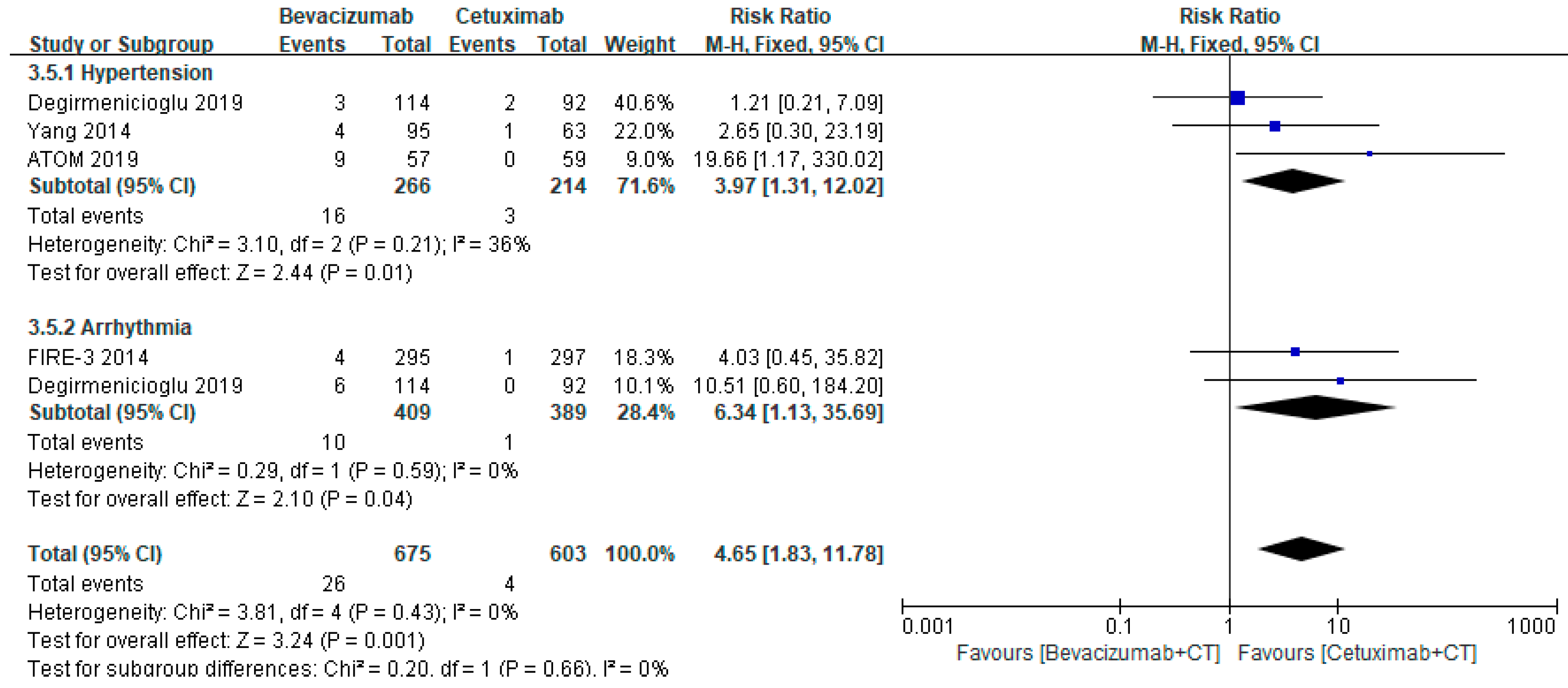
3.3. Safety Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Biller, L.H.; Schrag, D. Diagnosis and treatment of metastatic colorectal cancer: A Review. JAMA 2021, 325, 669–685. [Google Scholar] [CrossRef] [PubMed]
- Jeon, Y.; Park, E.J.; Lim, J.H.; Baik, S.H. Clinical outcomes of complete cytoreduction with concurrent liver resection followed by hyperthermic intraperitoneal chemotherapy for synchronous peritoneal and liver metastatic colorectal cancer. World J. Surg. Oncol. 2019, 17, 214. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network. NCCN Guidelines Version 2. 2021. Colon Cancer. Available online: www.nccn.org (accessed on 30 March 2021).
- Jiang, W.; Yu, Q.; Ning, R.; Zhao, W.; Wei, C. Efficacy of bevacizumab versus epidermal growth factor receptor inhibitors for wild-type RAS metastatic colorectal cancer: A meta-analysis. Onco Targets Ther. 2018, 11, 4271–4281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zheng, B.; Wang, X.; Wei, M.; Wang, Q.; Li, J.; Bi, L.; Deng, X.; Wang, Z. First-line cetuximab versus bevacizumab for RAS and BRAF wild-type metastatic colorectal cancer: A systematic review and meta-analysis. BMC Cancer 2019, 19, 280. [Google Scholar] [CrossRef]
- Du, R.; Wang, X.; Ma, L.; Larcher, L.M.; Tang, H.; Zhou, H.; Chen, C.; Wang, T. Adverse reactions of targeted therapy in cancer patients: A retrospective study of hospital medical data in China. BMC Cancer 2021, 21, 206. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [Green Version]
- U.S. Department of Health and Human Services. Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0. Available online: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/ctcae_v5_quick_reference_5x7.pdf (accessed on 2 March 2021).
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [Green Version]
- Sterne Bennouna, J.A.C.; Higgins, J.P.T.; Elbers, R.G.; Reeves, B.C.; the Development Group for ROBINSI. Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I): Detailed Guidance, Updated 12 October 2016. Available online: http://www.riskofbias.info (accessed on 30 March 2021).
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Oki, E.; Emi, Y.; Yamanaka, T.; Uetake, H.; Muro, K.; Takahashi, T.; Nagasaka, T.; Hatano, E.; Ojima, H.; Manaka, D.; et al. Randomised phase II trial of mFOLFOX6 plus bevacizumab versus mFOLFOX6 plus cetuximab as first-line treatment for colorectal liver metastasis (ATOM trial). Br. J. Cancer 2019, 121, 222. [Google Scholar] [CrossRef] [Green Version]
- Venook, A.P.; Niedzwiecki, D.; Lenz, H.J.; Innocenti, F.; Fruth, B.; Meyerhardt, J.A.; Schrag, D.; Greene, C.; O’Neil, B.H.; Atkins, J.N.; et al. Effect of first-line chemotherapy combined with cetuximab or bevacizumab on overall survival in patients with KRAS wild-type advanced or metastatic colorectal cancer: A randomized clinical trial. JAMA 2017, 317, 2392–2401. [Google Scholar] [CrossRef] [Green Version]
- Heinemann, V.; von Weikersthal, L.F.; Decker, T.; Kiani, A.; Vehling-Kaiser, U.; Al-Batran, S.E.; Heintges, T.; Lerchenmuller, C.; Kahl, C.; Seipelt, G.; et al. FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer (FIRE-3): A randomised, open-label, phase 3 trial. Lancet Oncol. 2014, 15, 1065–1075. [Google Scholar] [CrossRef]
- Bai, L.; Wang, F.; Li, Z.Z.; Ren, C.; Zhang, D.S.; Zhao, Q.; Lu, Y.X.; Wang, D.S.; Ju, H.Q.; Qiu, M.Z.; et al. Chemotherapy plus bevacizumab versus chemotherapy plus cetuximab as first-line treatment for patients with metastatic colorectal cancer: Results of a registry-based cohort analysis. Medicine 2016, 95, e4531. [Google Scholar] [CrossRef] [PubMed]
- Degirmencioglu, S.; Tanriverdi, O.; Menekse, S.; Dogan, M.; Hacıoglu, B.; Oktay, E.; Erdem, D.; Arpaci, E.; Uluc, B.O.; Turhal, S.; et al. A retrospective analysis on first-line bevacizumab, cetuximab, and panitimumab-containing regimens in patients with RAS-wild metastatic colorectal cancer: A Collaborative Study by Turkish Oncology Group (TOG). J. BUON 2019, 24, 136–142. [Google Scholar] [PubMed]
- Yang, Y.H.; Lin, J.K.; Chen, W.S.; Lin, T.C.; Yang, S.H.; Jiang, J.K.; Lan, Y.T.; Lin, C.C.; Yen, C.C.; Tzeng, C.H.; et al. Comparison of cetuximab to bevacizumab as the first-line bio-chemotherapy for patients with metastatic colorectal cancer: Superior progression-free survival is restricted to patients with measurable tumors and objective tumor response--a retrospective study. J. Cancer Res. Clin. Oncol. 2014, 140, 1927–1936. [Google Scholar]
- Fakih, M.; Vincent, M. Adverse events associated with anti-EGFR therapies for the treatment of metastatic colorectal cancer. Curr. Oncol. 2010, 17 (Suppl. 1), S18–S30. [Google Scholar] [CrossRef] [Green Version]
- Totzeck, M.; Mincu, R.I.; Rassaf, T. Cardiovascular adverse events in patients with cancer treated with bevacizumab: A meta-analysis of more than 20 000 patients. J. Am. Heart Assoc. 2017, 10, 6. [Google Scholar] [CrossRef] [Green Version]
- Bennouna, J.; Hiret, S.; Bertaut, A.; Bouche, O.; Deplanque, G.; Borel, C.; Francois, E.; Conroy, T.; Ghiringhelli, F.; des Guetz, G.; et al. Continuation of bevacizumab vs cetuximab plus chemotherapy after first progression in KRAS wild-type metastatic colorectal cancer: The UNICANCER PRODIGE18 randomized clinical trial. JAMA Oncol. 2019, 5, 83–90. [Google Scholar] [CrossRef] [Green Version]
- Balagula, Y.; Wu, S.; Su, X.; Lacouture, M.E. The effect of cytotoxic chemotherapy on the risk of high-grade aceniform rash to cetuximab in cancer patients: A meta-analysis. Ann. Oncol. 2011, 22, 2366–2374. [Google Scholar] [CrossRef]
- Jatoi, A.; Green, E.M.; Rowland, K.M.; Sargent, D.J.; Alberts, S.R. Clinical predictors of severe cetuximab-induced rash: Observations from 933 patients enrolled in north central cancer treatment group study N0147. Oncology 2009, 77, 120–123. [Google Scholar] [CrossRef] [Green Version]
- Fakih, M.G.; Wilding, G.; Lombardo, J. Cetuximab-induced hypomagnesemia in patients with colorectal cancer. Clin. Colorectal. Cancer 2006, 6, 152. [Google Scholar] [CrossRef]
- Wang, Q.; Qi, Y.; Zhang, D.; Gong, C.; Yao, A.; Xiao, Y.; Yang, J.; Zhou, F.; Zhou, Y. Electrolyte disorders assessment in solid tumor patients treated with anti-EGFR monoclonal antibodies: A pooled analysis of 25 randomized clinical trials. Tumour Biol. 2015, 36, 3471–3482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Economopoulou, P.; Kotsakis, A.; Kapiris, I.; Kentepozidis, N. Cancer therapy and cardiovascular risk: Focus on bevacizumab. Cancer Manag. Res. 2015, 7, 133–143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nickel, A.C.; Patel, A.; Saba, N.F.; Leon, A.R.; El-Chami, M.F.; Merchant, F.M. Incidence of cancer treatment-induced arrhythmia associated with novel targeted chemotherapeutic agents. J. Am. Heart Assoc. 2018, 7, e010101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J.; Wang, J.; Ni, T.; He, H.; Zheng, Q. Meta-analysis on the risk of fatal adverse events by bevacizumab, cetuximab, and panitumumab in 31 randomized trials including 25,000 patients with colorectal carcinoma. Medicine 2020, 99, e19908. [Google Scholar] [CrossRef]
- Zheng, Y.; Chen, Y.; Yu, K.; Yang, Y.; Wang, X.; Yang, X.; Qian, J.; Liu, Z.X.; Wu, B. Fatal infections among cancer patients: A population-based study in the United States. Infect. Dis. Ther. 2021, 10, 871–895. [Google Scholar] [CrossRef]
- Alvim, M.M.; Silva, L.A.; Leite, I.C.; Silvério, M.S. Adverse events caused by potential drug-drug interactions in an intensive care unit of a teaching hospital. Rev. Bras. Ter. Intensiva 2015, 27, 353–359. [Google Scholar] [CrossRef]
- Riechelmann, R.; Girardi, D. Drug interactions in cancer patients: A hidden risk? J. Res. Pharm. Pract. 2016, 5, 77–78. [Google Scholar] [CrossRef]
- van Leeuwen, R.W.F.; Jansman, F.G.A.; van den Bemt, P.M.L.A.; de Man, F.; Piran, F.; Vincenten, I.; Jager, A.; Rijneveld, A.W.; Brugma, J.D.; Mathijssen, R.H.J.; et al. Drug–drug interactions in patients treated for cancer: A prospective study on clinical interventions. Ann. Oncol. 2015, 26, 992–997. [Google Scholar] [CrossRef]
- Marques, R.P.; Heudtlass, P.; Pais, H.L.; Quintela, A.; Martins, A.P. Patient-reported outcomes and health-related quality of life for cetuximab versus bevacizumab in metastatic colorectal cancer: A prospective cohort study. J. Cancer Res. Clin. Oncol. 2019, 145, 1719–1728. [Google Scholar] [CrossRef]
- Lahiri, C.; Pawar, S.; Mishra, R. Precision medicine and future of cancer treatment. Precis. Cancer Med. 2019, 2, 33. [Google Scholar] [CrossRef]
- Singla, P.; Musyuni, P.; Aggarwal, G.; Singh, H. Precision Medicine: An emerging paradigm for improved diagnosis and safe therapy in pediatric oncology. Cureus 2021, 13, e16489. [Google Scholar] [CrossRef] [PubMed]
- Madhavan, S.; Beckman, R.A.; McCoy, M.D.; Pishvaian, M.J.; Brody, J.R.; Macklin, P. Envisioning the future of precision oncology trials. Nat. Cancer 2021, 2, 9–11. [Google Scholar] [CrossRef]



| Component | Definition |
|---|---|
| P (patients) | Patients diagnosed with RAS wild-type metastatic CRC who were administered the intervention or the comparator as first-line treatments |
| I (intervention) | Bevacizumab + chemotherapy |
| C (comparator) | Cetuximab + chemotherapy |
| O (outcomes) | SAEs (GRADE 3–4): Hematological SAEs: neutropenia, febrile neutropenia, anemia, thrombocytopenia, hematological toxicity, thrombosis/thromboembolism, infection, and hemorrhage Dermatological SAEs: mucositis, rash, paronychia, and HFS GI AEs: nausea, vomiting, diarrhea, GI perforation, liver toxicity, constipation, ileus, and subileus CV SAEs: hypertension and arrhythmia Neurological SAEs: peripheral neuropathy and fatigue Renal SAEs: proteinuria, dehydration, edema, and electrolyte disorders |
| S (study design) | RCTs and observational studies |
| Study Name | Study Duration | Country | Study Design | Patient Population | Intervention | Comparator | Backbone CT | Outcomes |
|---|---|---|---|---|---|---|---|---|
| RCTs | ||||||||
| ATOM (Oki et al.) 2019 [12] | May 2013–April 2016 | Japan | Multicenter, randomized phase II study | Patients aged between 20 and 80 years with liver-limited metastases from wt (K) RAS CRC | Bevacizumab (5 mg/kg) (n = 57) | Cetuximab (400 mg/m2 first dose followed by 250 mg/m2 on Day 1 through Day 2) (n = 59) | mFOLFOX6 | Hematological, dermatological, GI, neurological, and CV AEs |
| CALGB/SWOG 80405 (Venook et al. 2017) [13] | November 2005–March 2012 | United States and Canada | Multicenter, randomized phase III study | Patients aged ≥18 years with previously untreated advanced or metastatic colorectal cancer whose tumors were KRAS wt | Bevacizumab (5 mg/kg) (n = 559) | Cetuximab (400 mg/m2 followed by 250 mg/m2 weekly) (n = 578) | mFOLFOX6 or FOLFIRI | Hematological, GI, and neurological AEs |
| FIRE-3 (Heinemann et al. 2014) [14] | 23 January 2007–19 September 2012 | Germany, Austria | Randomized, open-label phase 3 trial | Patients aged 18–75 years with stage IV, histologically confirmed, adenocarcinoma of the colon or rectum, ECOG performance status of 0–2, an estimated life expectancy of greater than 3 months and adequate organ function, and no surgery within the 4 weeks before the study | Bevacizumab (5 mg/kg) (n = 295) | Cetuximab (400 mg/m2 on Day 1 and 250 mg/m2 weekly) (n = 297) | FOLFIRI | Hematological, dermatological, GI, neurological, CV, and renal AEs |
| Observational | ||||||||
| Bai et al. 2016 [15] | January 2009–December 2013 | China | Observational cohort study | Patients with histologically proved stage IV CRC who have consecutively received at least 2 courses of bevacizumab-based (KRAS wt or mutated) or cetuximab-based (KRAS wt) triplet biochemotherapy as their first line | Bevacizumab (5 mg/kg biweekly or 7.5 mg/kg triweekly) (n = 188) | Cetuximab (400 mg/m2 first dose, 500 mg/m2 biweekly or 750 mg/m2 triweekly) (n = 101) | mFOLFOX-6, FOLFIRI | Dermatological AEs |
| Degirmenicioglu et al. 2019 [16] | Not specified | Turkey | Retrospective multicenter observational study | Patients diagnosed pathologically as CRC adenocarcinoma with KRAS wt and who received chemotherapy in combination with either bevacizumab, cetuximab or panitumumab | Bevacizumab (n = 114) | Cetuximab (n = 92) | FOLFOX, FOLFIRI | Hematological, dermatological, GI, neurological, CV, and renal AEs |
| Yang et al. 2014 [17] | April 2005–March 2012 | China (Taiwan) | Retrospective cohort | Patients with histologically proven colorectal cancer at clinical stage IVa or IVb according to AJCC VII and who received at least 4 courses of bevacizumab-based or cetuximab-based triplet biochemotherapy as first-line treatments | Bevacizumab (5 mg/kg biweekly) (n = 95) | Cetuximab (500 mg/m2 biweekly) (n = 63) | FOLFIRI, FOLFOX | Hematological, dermatological, GI and CV AEs |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, Y.N.; Choi, Y.J.; Rhie, S.J. Tolerability on Serious Adverse Events of First-Line Bevacizumab and Cetuximab for RAS Wild-Type Metastatic Colorectal Cancer: A Systematic Review and Meta-Analysis. Healthcare 2022, 10, 217. https://doi.org/10.3390/healthcare10020217
Han YN, Choi YJ, Rhie SJ. Tolerability on Serious Adverse Events of First-Line Bevacizumab and Cetuximab for RAS Wild-Type Metastatic Colorectal Cancer: A Systematic Review and Meta-Analysis. Healthcare. 2022; 10(2):217. https://doi.org/10.3390/healthcare10020217
Chicago/Turabian StyleHan, Yu Na, Yeo Jin Choi, and Sandy Jeong Rhie. 2022. "Tolerability on Serious Adverse Events of First-Line Bevacizumab and Cetuximab for RAS Wild-Type Metastatic Colorectal Cancer: A Systematic Review and Meta-Analysis" Healthcare 10, no. 2: 217. https://doi.org/10.3390/healthcare10020217
APA StyleHan, Y. N., Choi, Y. J., & Rhie, S. J. (2022). Tolerability on Serious Adverse Events of First-Line Bevacizumab and Cetuximab for RAS Wild-Type Metastatic Colorectal Cancer: A Systematic Review and Meta-Analysis. Healthcare, 10(2), 217. https://doi.org/10.3390/healthcare10020217






