Ventilation Performance Evaluation of a Negative-Pressurized Isolation Room for Emergency Departments
Abstract
:1. Introduction
2. Methodology
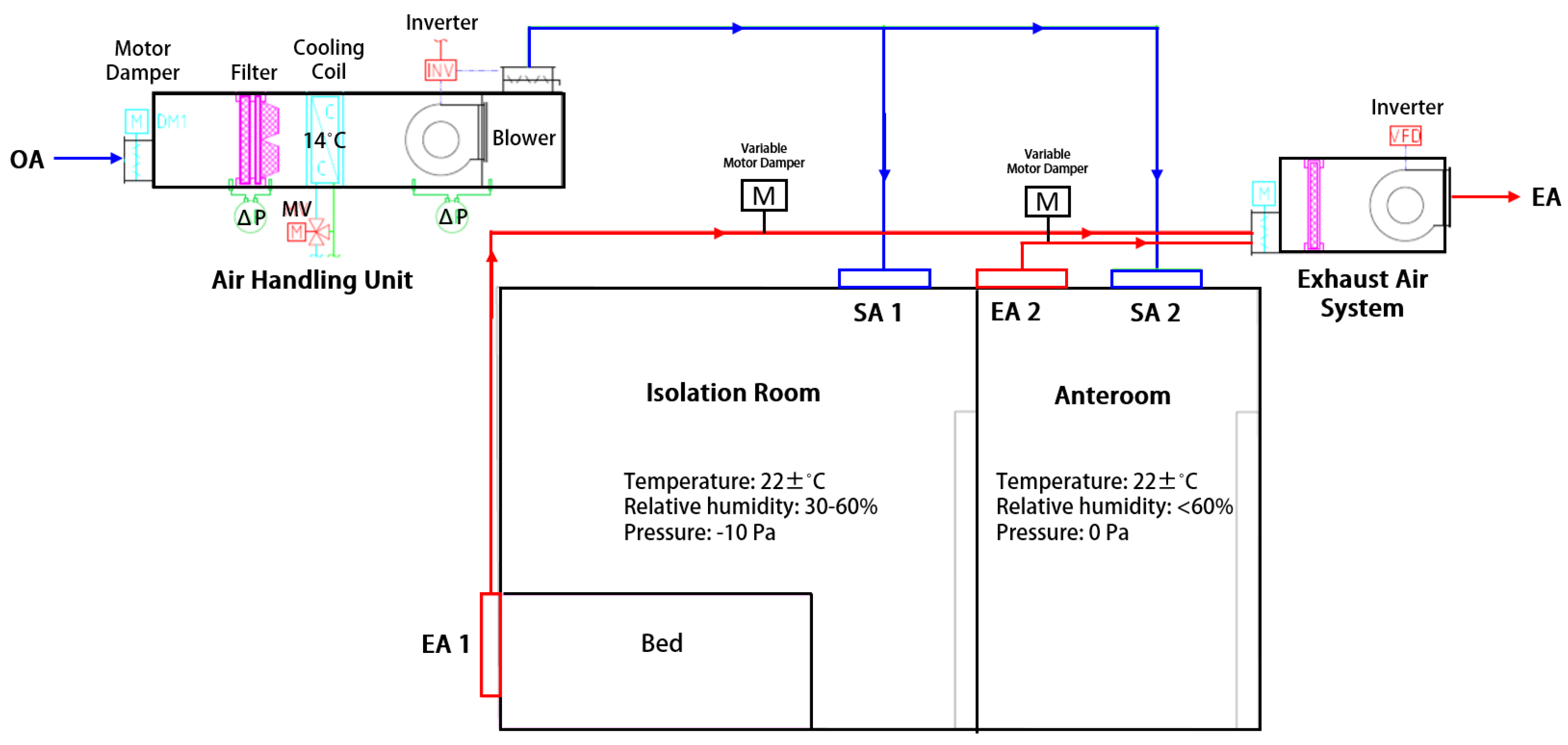
2.1. System Description
2.2. Field Measurements
2.3. CFD Simulation and Improvement Strategy
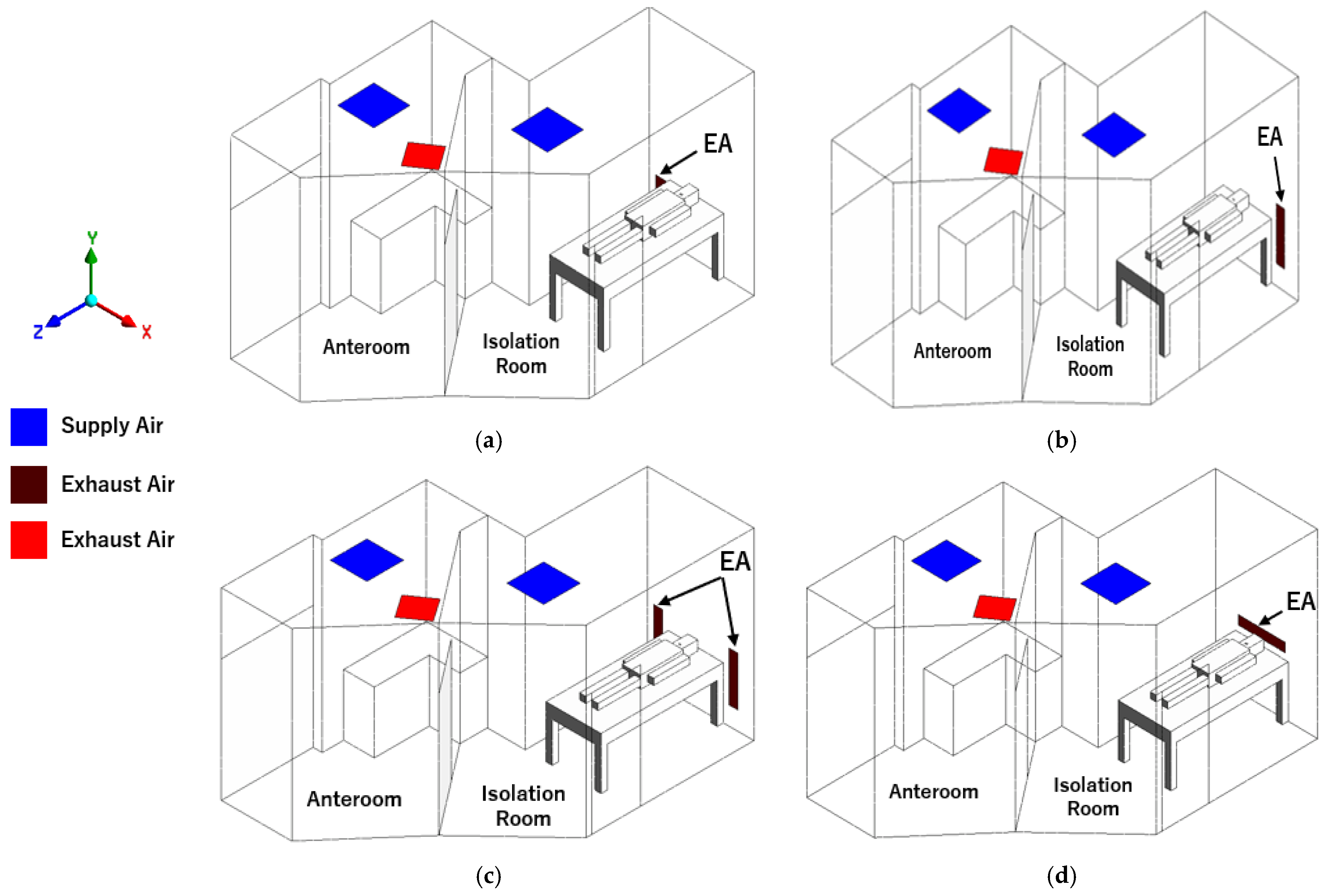
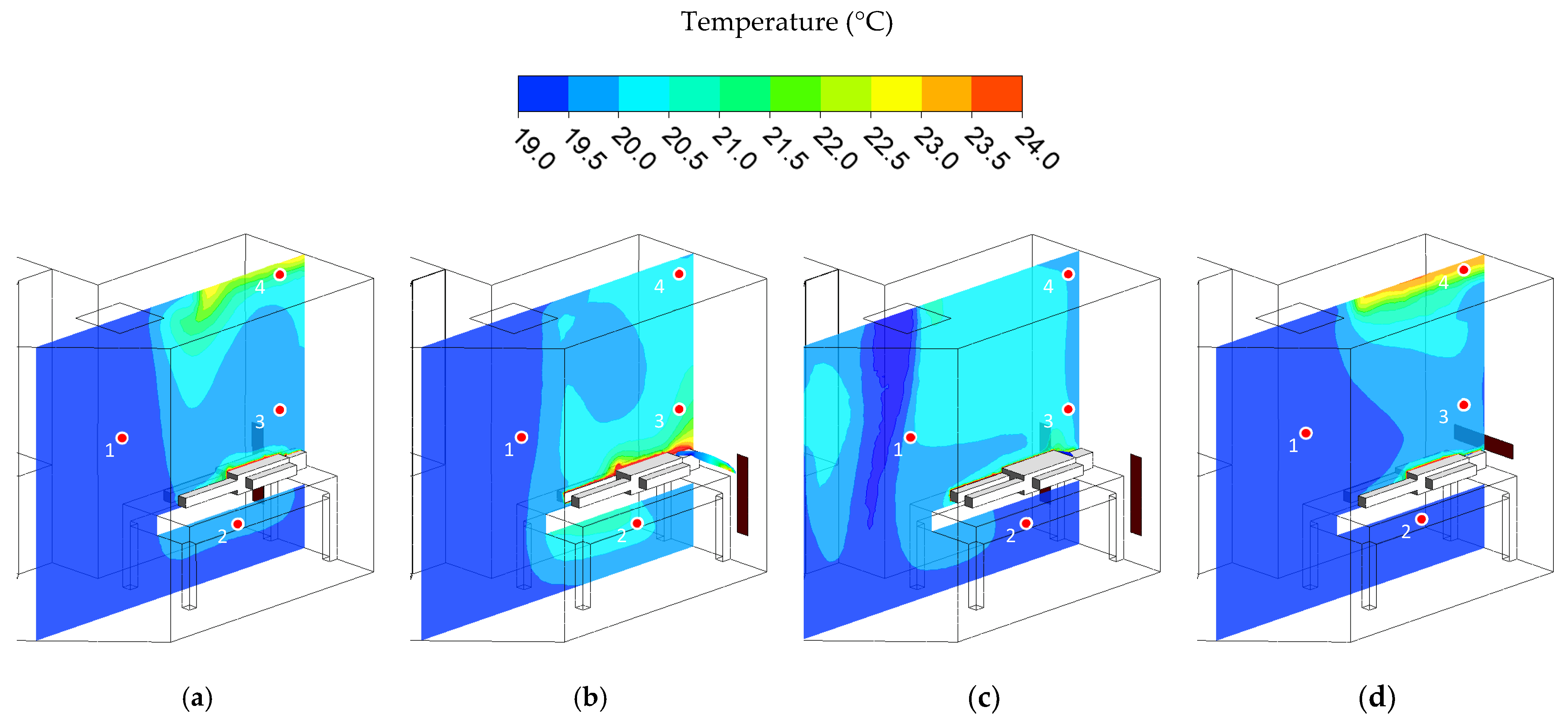
- Case 1: left wall-mounted exhaust air grille located about 300 mm above the floor. It will be the baseline case (Figure 2a).
- Case 2: right wall-mounted exhaust air grille, the reverse of case 1 (Figure 2b).
- Case 3: two wall-mounted exhaust air grilles are located beside the patient’s head. The total exhaust airflow rate is equal to the baseline case (Figure 2c).
- Case 4: wall-mounted exhaust air grilles located behind the patient’s head at 1000 mm above the floor (Figure 2d).
2.4. Boundary Condition
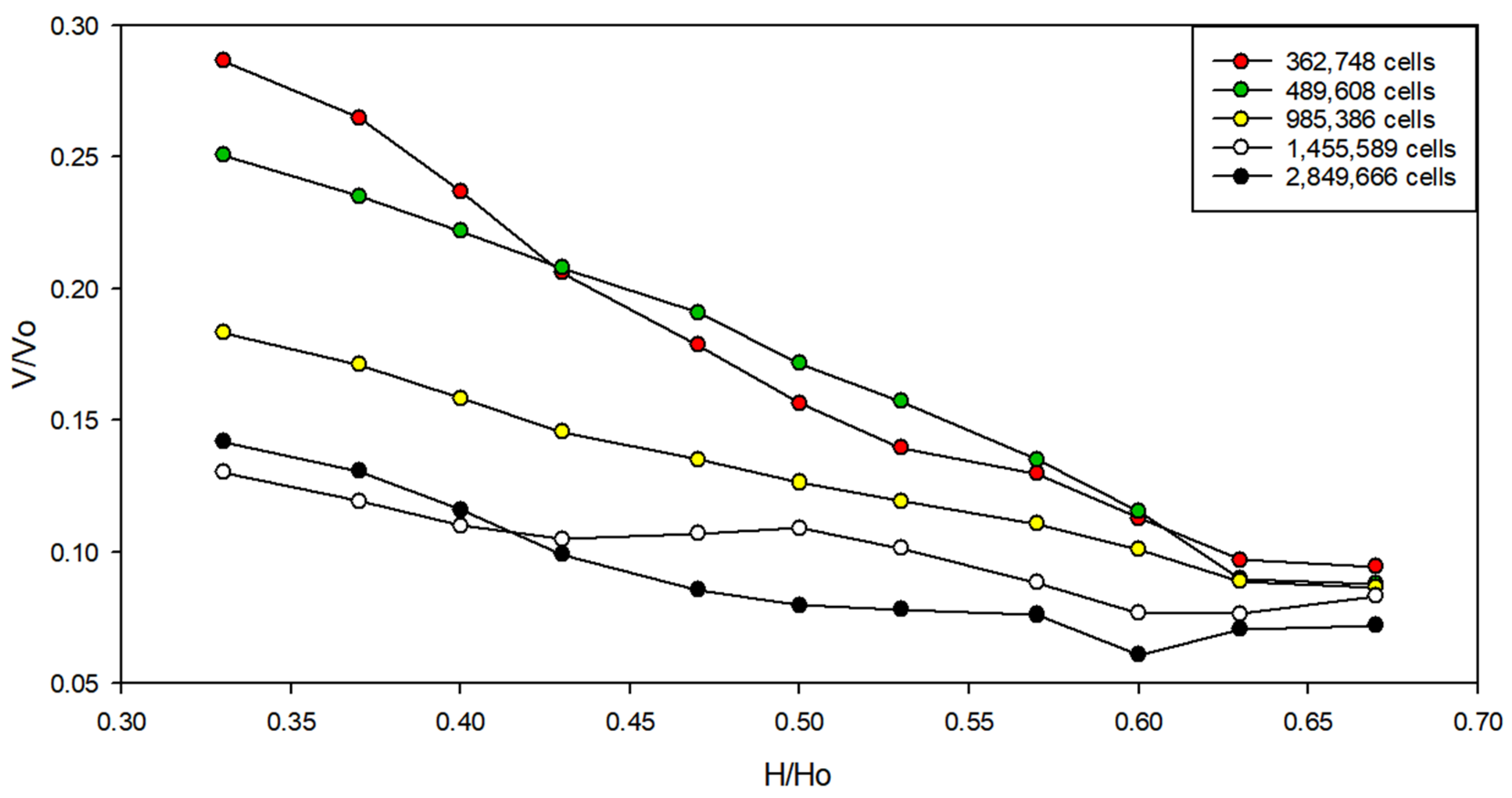
2.5. Grid Independence Test
3. Results and Discussion
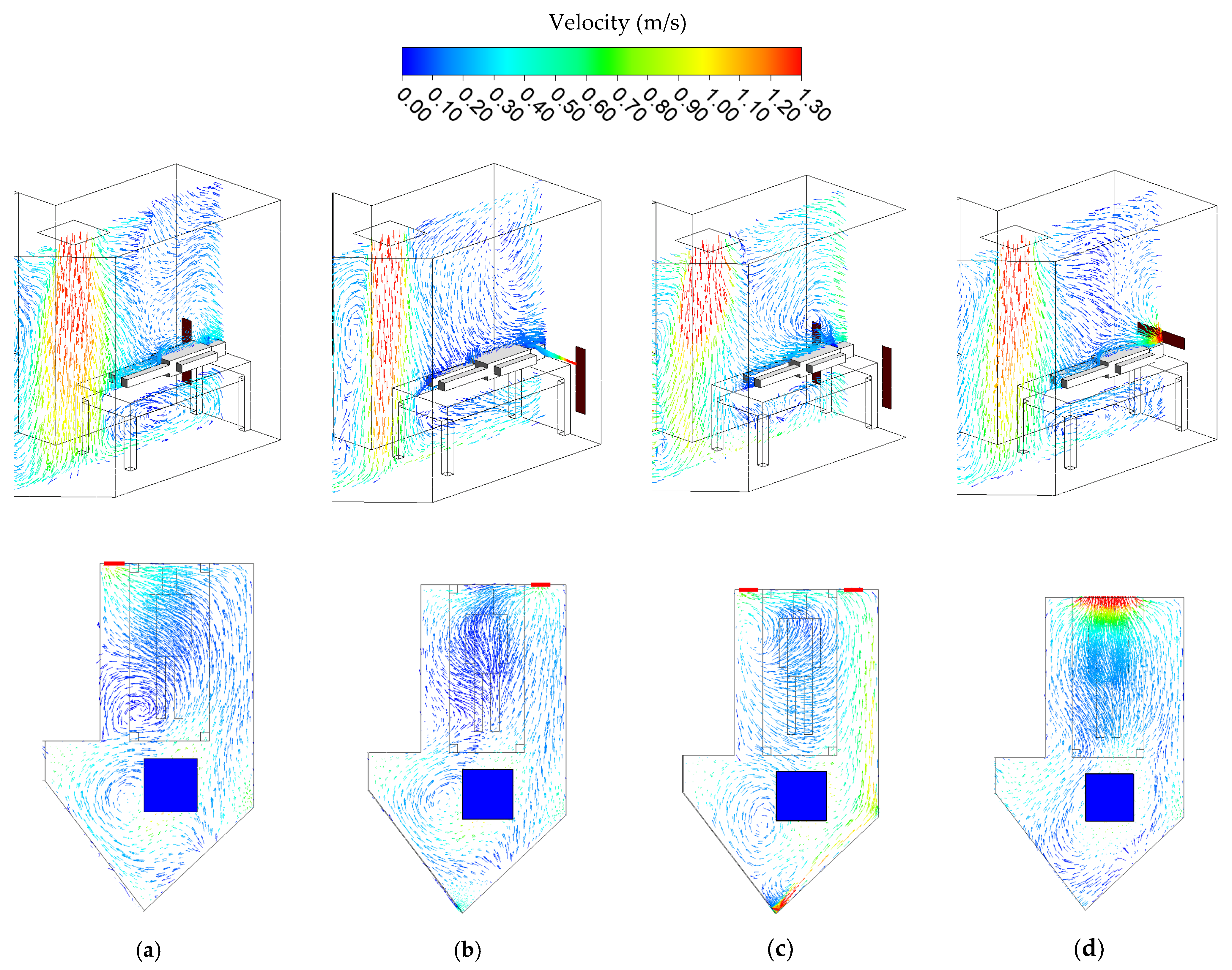
3.1. Airflow Distribution
3.2. Temperature Distribution
3.3. Concentration Distribution
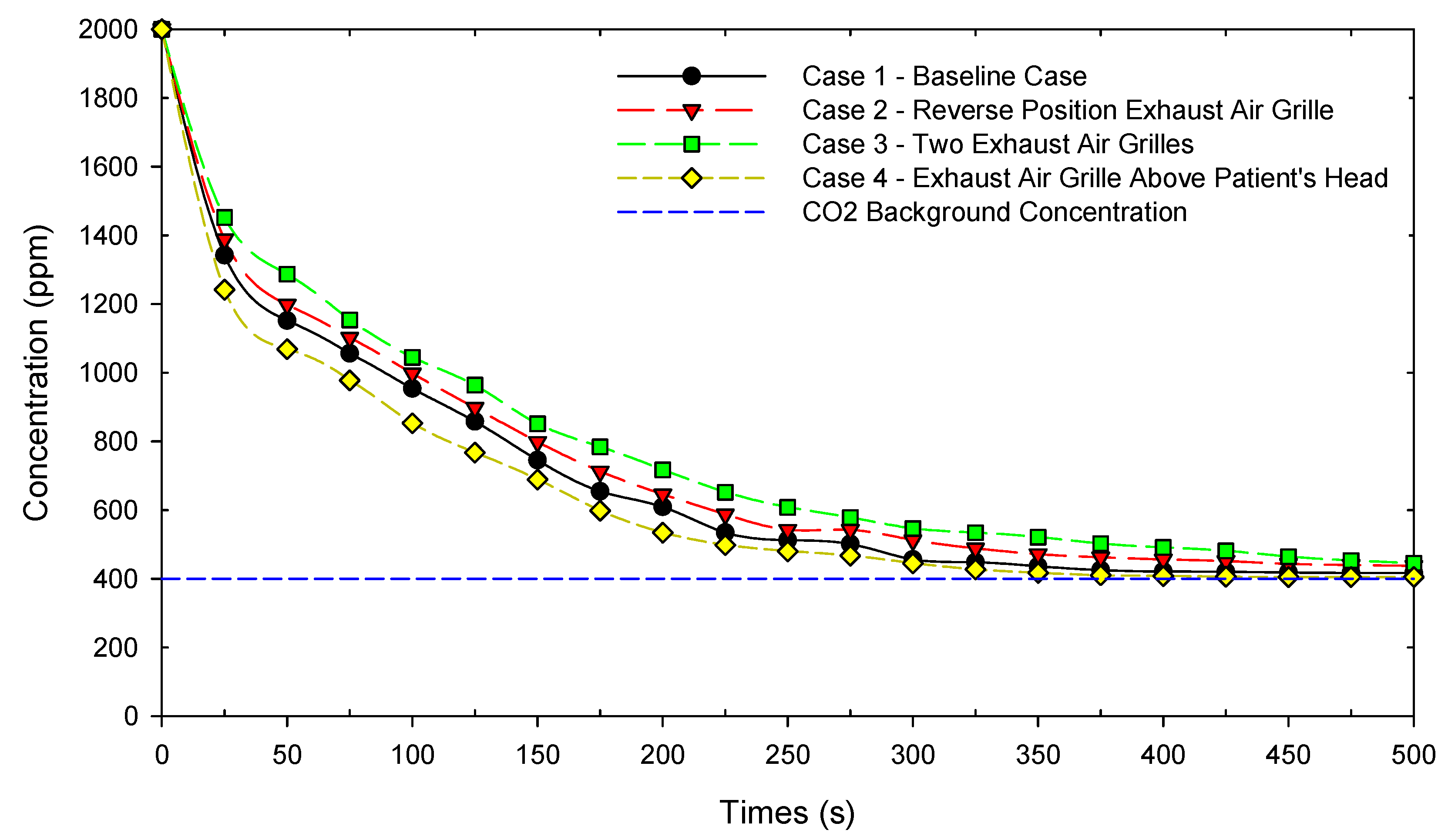
3.4. Concentration Contaminant Decay
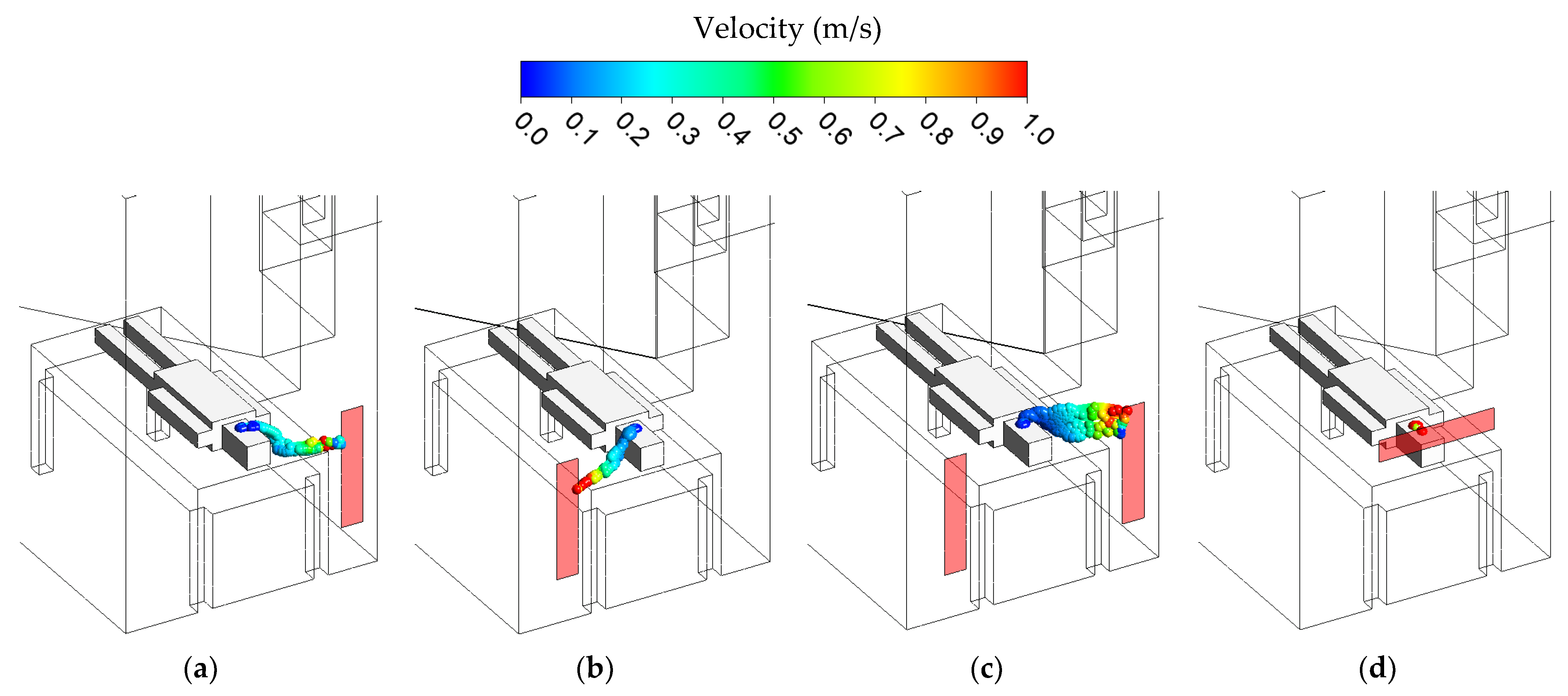
3.5. Bioaerosol Flow Path Model
3.6. Pressurization
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Tsai, L.H.; Chien, C.Y.; Chen, C.B.; Chaou, C.H.; Ng, C.J.; Lo, M.Y.; Seak, C.K.; Seak, J.C.Y.; Goh, Z.N.L.; Seak, C.J. Impact of the Coronavirus Disease 2019 Pandemic on an Emergency Department Service: Experience at the Largest Tertiary Center in Taiwan. Risk Manag. Healthc. Policy. 2021, 14, 771–777. [Google Scholar] [CrossRef]
- Cucinotta, D.W.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar]
- Liang, S.Y.; Theodoro, D.L.; Schuur, J.D.; Marschall, J. Infection prevention in the emergency department. Ann. Emerg. Med. 2014, 64, 299–313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gosbell, A.; Killen, A.; McCarthy, S. Australasian College for Emergency Medicine, Emergency Medicine Australasia and social media. Emerg. Med. Australas. 2012, 24, 463–464. [Google Scholar] [CrossRef] [PubMed]
- Seak, C.J.; Liu, Y.T.; Ng, C.J. Rapid responses in the emergency department of Linkou Chang Gung Memorial Hospital, Taiwan effectively prevent spread of COVID-19 among healthcare workers of emergency department during outbreak: Lessons learnt from SARS. Biomed. J. 2020, 43, 388–391. [Google Scholar] [CrossRef] [PubMed]
- Jensen, P.A.; Lambert, L.A.; Iademarco, M.F.; Ridzon, R. Guidelines for Preventing the Transmission of Mycobacterium Tuberculosis in Healthcare Settings; Department of Health and Human Services: Atlanta, GA, USA, 2005.
- ANSI/ASHRAE/ASHE Standard-170. Ventilation of Health Care Facilities; American Society of Heating, Refrigerating, and Air-Conditioning Engineers, Inc.: Atlanta, GA, USA, 2017. [Google Scholar]
- Institute of Labor, Occupational Safety and Health (ILOSH). Recommended Guidelines of Isolation Ward for SARS Patients; ILOSH: Taipei, Taiwan, 2016. Available online: https://www.ilosh.gov.tw/1261/1274/1276/8875/ (accessed on 5 June 2021).
- Sun, Z.; Wang, S. A CFD-based test method for control of indoor environment and space ventilation. Build. Environ. 2010, 45, 1441–1447. [Google Scholar] [CrossRef]
- Cheong, K.W.D.; Phua, S.Y. Development of ventilation design strategy for effective removal of pollutant in the isolation room of a hospital. Build. Environ. 2006, 41, 1161–1170. [Google Scholar] [CrossRef]
- Khankari, K. Patient room HVAC: Airflow path matters. ASHRAE J. 2016, 58, 16–27. [Google Scholar]
- Kao, P.H.; Yang, R.J. Virus diffusion in isolation rooms. J. Hosp. Infect. 2006, 62, 338–345. [Google Scholar] [CrossRef]
- Tung, Y.C.; Hu, S.C.; Tsai, T.I.; Chang, I.-L. An experimental study on ventilation efficiency of isolation room. Build. Environ. 2009, 44, 271–279. [Google Scholar] [CrossRef]
- Peng, S.; Chen, Q.; Liu, E. The role of computational fluid dynamics tools on investigation of pathogen transmission: Prevention and control. Sci. Total. Environ. 2020, 31, 142090. [Google Scholar] [CrossRef]
- Wang, F.; Chaerasari, C.; Rakshit, D.; Permana, I.; Kusnandar. Performance Improvement of a Negative-Pressurized Isolation Room for Infection Control. Healthcare 2021, 9, 1081. [Google Scholar] [CrossRef]
- Wang, F.; Permana, I.; Chaerasari, C.; Panigrahi, B.; Rakshit, D. Infection Control Improvement of a Negative-Pressurized Pediatric Intensive Care Unit. Healthcare 2021, 9, 1500. [Google Scholar] [CrossRef]
- Shih, Y.C.; Chiu, C.C.; Wang, O. Dynamic airflow simulation within an isolation room. Build. Environ. 2007, 42, 3194–3209. [Google Scholar] [CrossRef]
- Melhado, M.A.; Hensen, J.L.M.; Loomans, M.G.L.C. Literature review of staff thermal comfort and patient thermal risks in operating rooms. In Proceedings of the 8th International Healthy Buildings Conference, Lisboa, Portugal, 4–8 June 2006; Volume 1, pp. 11–14. [Google Scholar]
- Al-Benna, S. Negative pressure rooms and COVID-19. J. Perioper. Pract. 2021, 31, 18–23. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC) Taiwan. Use of quarantine to prevent transmission of severe acute respiratory syndrome--Taiwan. Morb. Mortal. Wkly. Rep. 2003, 52, 680–683. [Google Scholar]
- ANSYS. Ansys Fluent, Workbench 2020 R2. Available online: https://www.scribd.com/document/478910198/ANSYS-FluentTutorial-Guide-2020-R2-pdf (accessed on 6 March 2021).
- Wang, F.J.; Permana, I.; Rakhsit, D.; Azizah, R.S. Thermal Performance Improvement and Contamination Control Strategies in an Operating Room. J. Adv. Therm. Sci. Res. 2021, 8, 30–40. [Google Scholar] [CrossRef]
- Cui, S.; Cohen, M.; Stabat, P.; Marchio, D. CO2 tracer gas concentration decay method for measuring air change rate. Build. Environ. 2015, 84, 162–169. [Google Scholar] [CrossRef]
- Green Econometrics, Economic Analysis and Analytics for Sustainability and Process Improvement. 3 Metrics to Guide Air Quality Health & Safety. Available online: https://greenecon.net/3-metrics-to-guide-air-quality-health-safety/carbon-footprint.html (accessed on 20 July 2021).
- Minnesota Department of Health United States. Carbon dioxide (CO2). Available online: https://www.health.state.mn.us/communities/environment/air/toxins/co2.html (accessed on 15 June 2021).
- Deng, X.; Gong, G.; He, X.; Shi, X.; Mo, L. Control of exhaled SARS-CoV-2-laden aerosols in the interpersonal breathing microenvironment in a ventilated room with limited space air stability. J. Environ. Sci. 2021, 108, 175–187. [Google Scholar] [CrossRef] [PubMed]
- Tung, Y.C.; Shih, Y.C.; Hu, S.C. Numerical study on the dispersion of airborne contaminants from an isolation room in the case of door opening. Appl. Therm. Eng. 2009, 29, 1544–1551. [Google Scholar] [CrossRef] [PubMed]
- Suresh, K.; Regalla, S.P. Effect of mesh parameters in finite element simulation of single point incremental sheet forming process. Proc. Mat. Sci. 2014, 6, 376–382. [Google Scholar] [CrossRef] [Green Version]
- Wang, F.; Permana, I.; Rakshit, D.; Prasetyo, B.Y. Investigation of airflow distribution and contamination control with different schemes in an operating room. Atmosphere 2021, 12, 1639. [Google Scholar] [CrossRef]


| Location | Temperature (°C) | Air Flow Rate (CMH) | Air Changes Hour (ACH) | Pressure (Pa) |
|---|---|---|---|---|
| SA-1 | 18.1 | 291 | 16.76 | Anteroom → E.D. −10.2 |
| EA-1 | 24.0 | 350 |
| Parameter | Type | Value |
|---|---|---|
| Supply air | Velocity inlet Discrete phase: escape | Velocity: 1.28 m/s Temperature: 18.1 °C Concentration: 400 ppm |
| Exhaust air | Pressure outlet Discrete phase: trap | Temperature: 24 °C Pressure: −10.0 Pa |
| Exhaled air by patient | Velocity inlet | Velocity inlet: 1.12 m/s Temperature: 37 °C Patient’s exhale: 45,000 ppm |
| Bioaerosol | DPM: Injection | Velocity: 1.5 m/s Flowrate: 0.17 kg/s Particle Size: 1–5 µm, median 2.5 µm |
| Patient | Wall | Heat flux: 34.87 W/m2 |
| Previous Grid Value | New Grid Value | Relative Error (%) |
|---|---|---|
| 2,849,666 | 1,219,351 | 1.34 |
| 1,455,589 | 514,414 | 1.83 |
| 985,386 | 263,380 | 2.74 |
| 489,608 | 78,038 | 5.27 |
| 362,748 | 32,922 | 10.02 |
| Location | Case 1 | Case 2 | Case 3 | Case 4 |
|---|---|---|---|---|
| Point 1 | 19.13 | 19.15 | 19.67 | 19.10 |
| Point 2 | 19.55 | 20.28 | 19.82 | 19.35 |
| Point 3 | 20.25 | 20.52 | 20.65 | 20.24 |
| Point 4 | 20.35 | 20.33 | 20.42 | 20.87 |
| Location | Case 1 | Case 2 | Case 3 | Case 4 |
|---|---|---|---|---|
| Point 1 | 400.49 | 401.14 | 407.33 | 400.15 |
| Point 2 | 468.45 | 471.35 | 478.59 | 432.35 |
| Point 3 | 494.34 | 565.12 | 604.32 | 480.42 |
| Point 4 | 589.25 | 520.3 | 576.33 | 550.15 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, F.; Permana, I.; Chaerasari, C.; Lee, K.; Chang, T.; Rakshit, D. Ventilation Performance Evaluation of a Negative-Pressurized Isolation Room for Emergency Departments. Healthcare 2022, 10, 193. https://doi.org/10.3390/healthcare10020193
Wang F, Permana I, Chaerasari C, Lee K, Chang T, Rakshit D. Ventilation Performance Evaluation of a Negative-Pressurized Isolation Room for Emergency Departments. Healthcare. 2022; 10(2):193. https://doi.org/10.3390/healthcare10020193
Chicago/Turabian StyleWang, Fujen, Indra Permana, Citra Chaerasari, Kwowhei Lee, Tongbou Chang, and Dibakar Rakshit. 2022. "Ventilation Performance Evaluation of a Negative-Pressurized Isolation Room for Emergency Departments" Healthcare 10, no. 2: 193. https://doi.org/10.3390/healthcare10020193
APA StyleWang, F., Permana, I., Chaerasari, C., Lee, K., Chang, T., & Rakshit, D. (2022). Ventilation Performance Evaluation of a Negative-Pressurized Isolation Room for Emergency Departments. Healthcare, 10(2), 193. https://doi.org/10.3390/healthcare10020193








