Epidemiological Characteristics of Deaths from COVID-19 in Peru during the Initial Pandemic Response
Abstract
1. Introduction
2. Methods
- -
- National System of Deaths (SINADEF);
- -
- Database of RT-PCR test results (Netlab) and/or rapid tests (SISCOVID);
- -
- Clinical histories of hospitalized cases;
- -
- If complete information on death was not available from these sources, telephone communication was made with the epidemiologists of the regions, who performed a verbal autopsy in some cases.
3. Results
3.1. Epidemiological Characteristics
3.2. Stratified Analysis
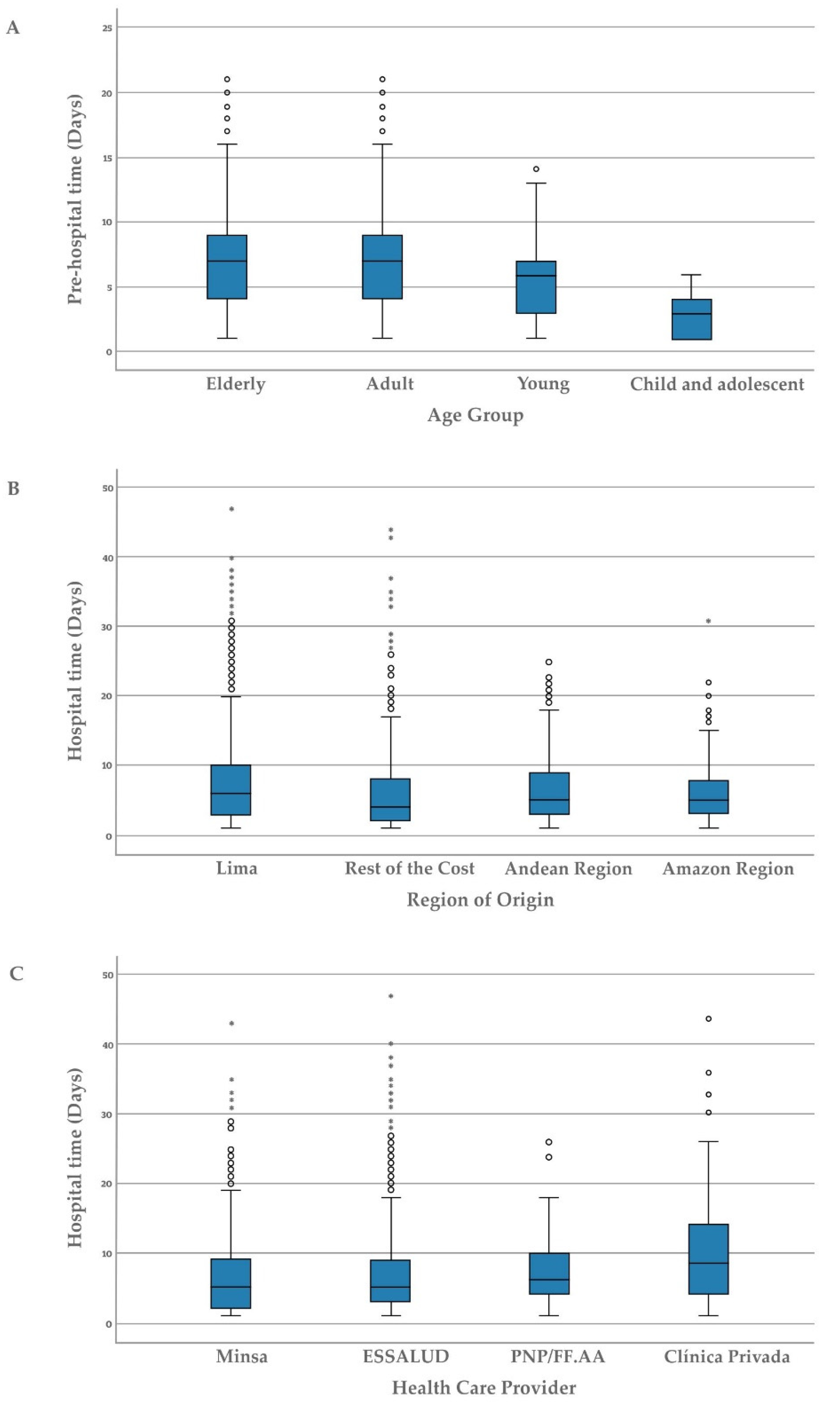
3.3. Analysis of Pre-Hospital and Hospital Times
3.3.1. Pre-Hospital Time
3.3.2. Hospitalized Time
| Characteristic | Pre-Hospital Time (Days) | Hospital Time (Days) | ||
|---|---|---|---|---|
| Mean ± Standard Deviation/Median (IQR) | p-Value | Mean ± Standard Deviation/Median (IQR) | p-Value | |
| Age Group | ||||
| Children and adolescents Ψ | 2.9 ± 1.7/3.0 (1.0–4.3) | 0.002 | 8.4 ± 9.4/5.0 (3.0–10.0) | <0.001 |
| Youth | 7.1 ± 6.4/7.0 (4.0–9.0) | 4.9 ± 3.5/4.0 (2.0–8.0) | ||
| Adults | 7.1 ± 3.9/7.0 (4.0–9.0) * | 7.9 ± 6.9/6.0 (3.0–10.3) | ||
| Seniors | 7.0 ± 4.2/7.0 (4.0–9.0) * | 6.4 ± 5.4/5.0 (3.0–8.0) μ | ||
| Gender | ||||
| Male Ψ | 7.1 ± 4.1/7.0 (4.0–9.0) | 0.037 | 7.1 ± 5.6/7.0 (3.0–10.0) | <0.001 |
| Female | 6.8 ± 4.1/6.0 (4.0–9.0) * | 6.3 ± 6.0/4.0 (2.0–8.0) * | ||
| Region of origin | ||||
| Lima Ψ | 7.1 ± 4.3/7.0 (4.0–9.0) | 0.156 | 7.9 ± 6.5/6.0 (3.0–10.0) | <0.001 |
| Rest of the coast | 7.0 ± 4.2/7.0 (4.0–10.0) | 5.8 ± 5.4/4.0 (2.0–8.0) * | ||
| Andean region | 6.6 ± 3.3/6.0 (4.0–8.0) | 6.5 ± 5.2/5.0 (3.0–9.0) * Ω | ||
| Amazon | 7.4 ± 3.7/7.0 (5.0–9.0) | 6.3 ± 4.8/5.0 (3.0–9.0) * Ω | ||
| Healthcare Provider | ||||
| Public hospital of the MINSA/GORE Ψ | 6.9 ± 4.1/6.0 (4.0–9.0) | 0.596 | 6.4 ± 5.5/5.0 (2.0–9.0) | <0.001 |
| EsSalud public hospital | 7.1 ± 4.1/7.0 (4.0–10.0) | 6.9 ± 6.0/5.0 (3.0–9.0) * | ||
| Hospital of PNP/FF.AA | 6.8 ± 3.9/7.0 (2.8–9.0) | 8.3 ± 6.2/6.0 (3.0–10.0) * ф | ||
| Private clinics | 7.1 ± 4.6/6.5 (4.0–9.0) | 10.5 ± 9.0/8.5 (4.0–14.3) * ф | ||
| Comorbidities | ||||
| Yes | 6.9 ± 4.1/7.0 (4.0–9.0) | 0.053 | 7.1 ± 6.4/5.0 (3.0–9.0) | 0.624 |
| No Ψ | 7.3 ± 4.2/7.0 (4.0–9.0) | 6.7 ± 5.5/5.0 (3.0–9.0) | ||
| Parameters | B | 95% Wald Confidence Interval | Contrast Hypothesis | |||
|---|---|---|---|---|---|---|
| Inferior | Superior | Wald Chi-Square | df | p Value * | ||
| Gender | 0.035 | −0.024 | 0.093 | 1.359 | 1 | 0.244 |
| Male | ||||||
| Female (Ref) | ||||||
| Age Group | ||||||
| Seniors | 0.866 | 0.528 | 1.204 | 25.233 | 1 | <0.001 |
| Adults | 0.873 | 0.534 | 1.212 | 25.477 | 1 | <0.001 |
| Youth | 0.501 | 0.012 | 0.991 | 4.030 | 1 | 0.045 |
| Children and adolescents (Ref) | ||||||
| Comorbidities | −0.058 | −0.110 | −0.005 | 4.662 | 1 | 0.031 |
| Yes | ||||||
| No (Ref) | ||||||
| Healthcare Provider | ||||||
| Public hospital of the MINSA/GORE | −0.027 | −0.187 | 0.133 | 0.108 | 1 | 0.743 |
| EsSalud public hospital | 0.020 | −0.140 | 0.180 | 0.058 | 1 | 0.810 |
| Hospital of PNP/FF.AA | −0.068 | −0.306 | 0.170 | 0.314 | 1 | 0.575 |
| Private clinics (Ref) | ||||||
| Region of origin | ||||||
| Amazon | 0.036 | −0.050 | 0.122 | 0.666 | 1 | 0.414 |
| Andean region | −0.103 | −0.187 | −0.019 | 5.778 | 1 | 0.016 |
| Rest of the coast | 0.004 | −0.054 | 0.063 | 0.022 | 1 | 0.883 |
| Lima (Ref) | ||||||
| Parameters | B | 95% Wald Confidence Interval | Contrast Hypothesis | |||
|---|---|---|---|---|---|---|
| Inferior | Superior | Wald Chi Square | df | p Value * | ||
| Gender | ||||||
| Male | 0.111 | 0.018 | 0.204 | 5.460 | 1 | 0.019 |
| Female (Ref) | ||||||
| Age Group | ||||||
| Seniors | 0.022 | −0.330 | 0.373 | 0.014 | 1 | 0.904 |
| Adults | 0.213 | −0.141 | 0.568 | 1.391 | 1 | 0.238 |
| Youth | −0.184 | −0.729 | 0.360 | 0.441 | 1 | 0.507 |
| Children and adolescents (Ref) | ||||||
| Comorbidities | ||||||
| Yes | 0.080 | 0.001 | 0.158 | 3.957 | 1 | 0.047 |
| No (Ref) | ||||||
| Healthcare Provider | ||||||
| Public hospital of the MINSA/GORE | −0.451 | −0.672 | −0.230 | 16.033 | 1 | <0.001 |
| EsSalud public hospital | −0.341 | −0.562 | −0.120 | 9.146 | 1 | 0.002 |
| Hospital of PNP/FF.AA | −0.274 | −0.589 | 0.041 | 2.915 | 1 | 0.088 |
| Private clinics (Ref) | ||||||
| Region of origin | ||||||
| Amazon | −0.150 | −0.288 | −0.013 | 4.594 | 1 | 0.032 |
| Andean region | −0.105 | −0.233 | 0.024 | 2.552 | 1 | 0.110 |
| Rest of the coast | −0.242 | −0.334 | −0.151 | 27.140 | 1 | <0.001 |
| Lima (Ref) | ||||||
| Pre-hospital time | ||||||
| 9 or more days | −0.089 | −0.196 | 0.019 | 2.589 | 1 | 0.108 |
| 4 to 8 days | −0.059 | −0.160 | 0.042 | 1.318 | 1 | 0.251 |
| 1 to 3 days (Ref) | ||||||
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Disclaimer
References
- Tran, B.X.; Ha, G.H.; Nguyen, L.H.; Vu, G.T.; Hoang, M.T.; Le, H.T.; Latkin, C.A.; Ho, C.S.H.; Ho, R.C. Studies of Novel Coronavirus Disease 19 (COVID-19) Pandemic: A Global Analysis of Literature. Int. J. Environ. Res. Public Health 2020, 17, 4095. [Google Scholar] [CrossRef] [PubMed]
- Koelle, K.; Martin, M.A.; Antia, R.; Lopman, B.; Dean, N.E. The changing epidemiology of SARS-CoV-2. Science 2022, 375, 1116–1121. [Google Scholar] [CrossRef] [PubMed]
- Sangrador, C.O.; Leiza, J.R.G.; Boillos, M.J.P.; Ara, F.P.; Lobato, M.P.L.; de Llano, J.M.A. Impact of COVID-19 on mortality in the autonomous community of Castilla y León (Spain). Gac. Sanit. 2021, 35, 459–464. [Google Scholar] [CrossRef] [PubMed]
- de Figueiredo, A.M.; Daponte, A.; de Figueiredo, D.C.M.M.; Gil-García, E.; Kalache, A. Case fatality rate of COVID-19: Absence of epidemiological pattern. Gac. Sanit. 2021, 35, 355–357. (In Spanish) [Google Scholar] [CrossRef]
- Cuadros, D.F.; Xiao, Y.; Mukandavire, Z.; Correa-Agudelo, E.; Hernández, A.; Kim, H.; MacKinnon, N.J. Spatiotemporal transmission dynamics of the COVID-19 pandemic and its impact on critical healthcare capacity. Health Place 2020, 64, 102404. [Google Scholar] [CrossRef] [PubMed]
- Rojas, D.; Saavedra, J.; Petrova, M.; Pan, Y.; Szapocznik, J. Predictors of COVID-19 Fatality: A Worldwide Analysis of the Pandemic over Time and in Latin America. J. Epidemiol. Glob. Health 2022, 12, 150–159. [Google Scholar] [CrossRef]
- Korean Society of Infectious Diseases and Korea Centers for Disease Control and Prevention. Analysis on 54 Mortality Cases of Coronavirus Disease 2019 in the Republic of Korea from January 19 to March 10, 2020. J. Korean Med. Sci. 2020, 35, e132. [Google Scholar] [CrossRef]
- García-Basteiro, A.L.; Chaccour, C.; Guinovart, C.; Llupià, A.; Brew, J.; Trilla, A.; Plasencia, A. Monitoring the COVID-19 epidemic in the context of widespread local transmisión. Lancet Respir. Med. 2020, 8, 440–442. [Google Scholar] [CrossRef]
- Ministerio de Agricultura y Riego del Perú. Perfil ambiental del Perú. Lima: MINAGRI. 2015. Available online: http://minagri.gob.pe/portal/datero/60-sector-agrario/introduccion/343-perfil-ambiental-del-peru (accessed on 12 October 2020).
- Jauregui-Fung, F.; Kenworthy, J.; Almaaroufi, S.; Pulido-Castro, N.; Pereira, S.; Golda-Pongratz, K. Anatomy of an Informal Transit City: Mobility Analysis of the Metropolitan Area of Lima. Urban Sci. 2019, 3, 67. [Google Scholar] [CrossRef]
- HelpAge International. Global AgeWatch Index 2015. Available online: https://www.helpage.org/global-agewatch/population-ageing-data/global-rankings-table/ (accessed on 18 August 2020).
- Instituto Nacional de Estadística e Informática: Perú: Enfermedades Transmisibles y No Transmisibles 2019. Lima: INEI. 2020. Available online: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1734/cap01.pdf (accessed on 16 September 2020).
- Loza, C.; Ramos, W. Análisis de la Situación de la Enfermedad Renal Crónica en el Perú, 2015. Lima: DGEMINSA. 2016. Available online: https://www.gob.pe/institucion/minsa/informes-publicaciones/285012-analisis-de-la-situacion-de-la-enfermedad-renal-cronica-en-el-peru-2015 (accessed on 16 September 2020).
- Piñeros, M.; Ramos, W.; Antoni, S.; Abriata, G.; Medina, L.E.; Miranda, J.J.; Payet, E.; Bray, F. Cancer patterns, trends, and transitions in Peru: A regional perspective. Lancet Oncol. 2017, 18, e573–e586. [Google Scholar] [CrossRef]
- Centro Nacional de Epidemiología, Prevención y Control de Enfermedades, Ministerio de Salud del Perú. Situación Actual “COVID-19“ al 20 de Mayo 2020. Lima: Ministerio de Salud del Perú. 2020. Available online: https://www.dge.gob.pe/portal/docs/tools/coronavirus/coronavirus200520.pdf (accessed on 18 August 2020).
- Lossio, J. COVID-19 in Peru: State and social responses. Hist. Cienc. Saude. Manguinhos 2021, 28, 581–585. (In Spanish) [Google Scholar] [CrossRef] [PubMed]
- Johns Hopkins University & Medicine. Mortality Analyses: Mortality in the Most Affected Countries. Baltimore: Johns Hopkins University. August 2020. Available online: https://coronavirus.jhu.edu/data/mortality (accessed on 31 August 2020).
- Salinas-Rodríguez, A.; Manrique-Espinoza, B.; Sosa-Rubí, S.G. Statistical analysis for count data: Use of healthcare services applications. Salud Publica Mex. 2009, 51, 397–406. [Google Scholar] [PubMed]
- Salvado, J.C. The Determinants of Health Care Utilization in Portugal: An Approach with Count Data Models. Swiss J. Econ. Stat. 2008, 144, 437–458. [Google Scholar] [CrossRef]
- Cevallos-Valdiviezo, H.; Vergara-Montesdeoca, A.; Zambrano-Zambrano, G. Measuring the impact of the COVID-19 outbreak in Ecuador using preliminary estimates of excess mortality, 17 March–22 October 2020. Int. J. Infect. Dis. 2021, 104, 297–299. [Google Scholar] [CrossRef]
- Ortiz-Prado, E.; Simbaña-Rivera, K.; Barreno, L.G.; Diaz, A.M.; Barreto, A.; Moyano, C.; Arcos, V.; Vásconez-González, E.; Paz, C.; Simbaña-Guaycha, F.; et al. Epidemiological, socio-demographic and clinical features of the early phase of the COVID-19 epidemic in Ecuador. PLoS Negl. Trop. Dis. 2021, 15, e0008958. [Google Scholar] [CrossRef] [PubMed]
- Baggio, J.A.O.; Machado, M.F.; Carmo, R.F.D.; Armstrong, A.D.C.; Santos, A.D.D.; Souza, C.D.F. COVID-19 in Brazil: Spatial risk, social vulnerability, human development, clinical manifestations and predictors of mortality—A retrospective study with data from 59 695 individuals. Epidemiol. Infect. 2021, 149, e100. [Google Scholar] [CrossRef] [PubMed]
- Cavalcante, J.R.; Cardoso-Dos-Santos, A.C.; Bremm, J.M.; Lobo, A.D.P.; Macário, E.M.; de Oliveira, W.K.; de França, G.V.A. COVID-19 in Brazil: Evolution of the epidemic up until epidemiological week 20 of 2020. Epidemiol. Serv. Saude. 2020, 29, e2020376. [Google Scholar] [CrossRef]
- Lu, L.; Zhong, W.; Bian, Z.; Li, Z.; Zhang, K.; Liang, B.; Zhong, Y.; Hu, M.; Lin, L.; Liu, J.; et al. A Comparison of Mortality-related Risk Factors of COVID-19, SARS, and MERS: A Systematic Review and Meta-analysis. J. Infect. 2020, 81, e18–e25. [Google Scholar] [CrossRef]
- Kang, S.J.; Jung, S.I. Age-Related Morbidity and Mortality among Patients with COVID-19. Infect. Chemother. 2020, 52, 154–164. [Google Scholar] [CrossRef]
- Bencivenga, L.; Rengo, G.; Varricchi, G. Elderly at time of COronaVIrus disease 2019 (COVID-19): Possible role of immunosenescence and malnutrition. Geroscience 2020, 42, 1089–1092. [Google Scholar] [CrossRef]
- Shahid, Z.; Kalayanamitra, R.; McClafferty, B.; Kepko, D.; Ramgobin, D.; Patel, R.; Aggarwal, C.S.; Vunnam, R.; Sahu, N.; Jain, R.; et al. COVID-19 and Older Adults: What We Know. J. Am. Geriatr. Soc. 2020, 68, 926–929. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.J.; Dong, X.; Cao, Y.Y.; Yuan, Y.D.; Yang, Y.B.; Yan, Y.Q.; Akdis, C.A.; Gao, Y.D. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy Eur. J. Allergy Clin. Immunol. 2020, 75, 1730–1741. [Google Scholar] [CrossRef] [PubMed]
- Yi, Y.; Lagniton, P.N.P.; Ye, S.; Li, E.; Xu, R.H. COVID-19: What has been learned and to be learned about the novel coronavirus disease. Int. J. Biol. Sci. 2020, 16, 1753–1766. [Google Scholar] [CrossRef] [PubMed]
- Jain, V.; Yuan, J.M. Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: A systematic review and meta-analysis. Int. J. Public Health 2020, 65, 533–546. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.-J.; Liang, W.-H.; Zhao, Y.; Liang, H.-R.; Chen, Z.-S.; Li, Y.-M.; Liu, X.-Q.; Chen, R.-C.; Tang, C.-L.; Wang, T.; et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: A nationwide análisis. Eur. Respir J. 2020, 55, 2000547. [Google Scholar] [CrossRef] [PubMed]
- Centro Nacional de Epidemiología, Prevención y Control de Enfermedades, Ministerio de Salud del Perú. Situación actual COVID-19 al 31 de Marzo 2020. Lima: CDC/MINSA. 2020. Available online: https://www.dge.gob.pe/portal/docs/tools/coronavirus/coronavirus310320.pdf (accessed on 15 October 2020).
- Centro Nacional de Epidemiología, Prevención y Control de Enfermedades, Ministerio de Salud del Perú. Situación actual COVID-19 al 30 de Abril 2020. Lima: CDC/MINSA. 2020. Available online: https://www.dge.gob.pe/portal/docs/tools/coronavirus/coronavirus300420.pdf (accessed on 15 October 2020).
- Padilla Machaca, P.M.; Cárdenas Ramírez, B.E.; Cabrejos, M.C.C. Impact of COVID-19 on liver disease and the public health in Peru [Spanish]. Rev. Gastroenterol. Peru. 2020, 40, 162–172. Available online: http://www.scielo.org.pe/scielo.php?pid=S1022-51292020000200162&script=sci_arttext (accessed on 1 September 2022). [CrossRef]
- Neyra-León, J.; Huancahuari-Nuñez, J.; Díaz-Monge, J.C.; Pinto, J.A. The impact of COVID-19 in the healthcare workforce in Peru. J. Public Health Policy 2020, 42, 182–184. [Google Scholar] [CrossRef]
- Tenorio-Mucha, J.; Lazo-Porras, M.; Monroy-Hidalgo, A.; Málaga, G.; Cárdenas, M.K. Prices of essential drugs for management and treatment of COVID-19 in public and private Peruvian pharmacies [Spanish]. Acta Med. Peru 2020, 37, 267–277. [Google Scholar] [CrossRef]
- Orellana, J.D.Y.; Cunha, G.M.D.; Marrero, L.; Horta, B.L.; Leite, I.D.C. Explosion in mortality in the Amazonian epicenter of the COVID-19 epidemic 19. Cad. Saude Publica 2020, 36, e00120020. [Google Scholar] [CrossRef]
- Croda, J.; de Oliveira, W.K.; Frutuoso, R.L.; Mandetta, L.H.; Baia-Da-Silva, D.C.; Brito-Sousa, J.D.; Monteiro, W.M.; Lacerda, M.V.G. COVID-19 in Brazil: Advantages of a socialized unified health system and preparation to contain cases. Rev. Soc. Bras. Med. Trop. 2020, 53, e20200167. [Google Scholar] [CrossRef]
- Spicer, N.; Agyepong, I.; Ottersen, T.; Jahn, A.; Ooms, G. ‘It’s far too complicated’: Why fragmentation persists in global health. Glob. Health 2020, 16, 60. [Google Scholar] [CrossRef] [PubMed]
- Vasquez-Elera, L.E.; Failoc-Rojas, V.E.; Martinez-Rivera, R.N.; Morocho-Alburqueque, N.; Temoche-Rivas, M.S.; Valladares-Garrido, M.J. Self-medication in hospitalized patients with COVID-19: A cross-sectional study in northern Peru. Germs 2022, 12, 46–53. [Google Scholar] [CrossRef]
- Soriano-Moreno, D.R.; Fernandez-Guzman, D.; Sangster-Carrasco, L.; Quispe-Vicuña, C.; Grados-Espinoza, P.; Ccami-Bernal, F.; Morocho-Alburqueque, N.; Coba-Villan, N.; Velasquez-Fernandez, R.; Nieto-Gutierrez, W. Factors Associated With Drug Consumption Without Scientific Evidence in Patients With Mild COVID-19 in Peru. J. Patient Saf. 2022; ahead to print. [Google Scholar] [CrossRef]
- Soriano-Moreno, D.R.; Fernandez-Guzman, D.; Ccami-Bernal, F.; Rojas-Miliano, C.; Nieto-Gutierrez, W. Factors associated with the consumption of chlorine dioxide to prevent and treat COVID-19 in the Peruvian population: A cross-sectional study. BMC Public Health 2021, 21, 2109. [Google Scholar] [CrossRef] [PubMed]
- Mejía, F.; Medina, C.; Cornejo, E.; Morello, E.; Vásquez, S.; Alave, J.; Schwalb, A.; Málaga, G. Oxygen saturation as a predictor of mortality in hospitalized adult patients with COVID-19 in a public hospital in Lima, Peru. PLoS ONE 2020, 15, e0244171. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Salud del Perú. Documento técnico: Plan Nacional de Vacunación contra la COVID-19. Lima: MINSA. 2020. Available online: https://www.gob.pe/institucion/minsa/normas-legales/1293043-848-2020-minsa (accessed on 21 January 2020).
- Loayza-Alarico, M.J.; De La Cruz -Vargas, J.A.; Ramos, W. Rapid response teams for epidemiological surveillance: Mitigation of the coronavirus pandemic in Perú, 2020. Rev. Fac. Med. Hum. 2020, 20, 519–521. [Google Scholar] [CrossRef]
- Chan, E.Y.Y.; Huang, Z.; Lo, E.S.K.; Hung, K.K.C.; Wong, E.L.Y.; Wong, S.Y.S. Sociodemographic Predictors of Health Risk Perception, Attitude and Behavior Practices Associated with Health-Emergency Disaster Risk Management for Biological Hazards: The Case of COVID-19 Pandemic in Hong Kong, SAR China. Int. J. Environ. Res. Public Health 2020, 17, 3869. [Google Scholar] [CrossRef]
- Navarro, J.C.; Arrivillaga-Henríquez, J.; Salazar-Loor, J.; Rodriguez-Morales, A.J. COVID-19 and dengue, co-epidemics in Ecuador and other countries in Latin America: Pushing strained health care systems over the Edge. Travel Med. Infect. Dis. 2020, 37, 101656. [Google Scholar] [CrossRef]
- Zhang, Z.; Yao, W.; Wang, Y.; Long, C.; Fu, X. Wuhan and Hubei COVID-19 mortality analysis reveals the critical role of timely supply of medical resources. J. Infect. 2020, 81, 147–178. [Google Scholar] [CrossRef]
| Characteristic | Frequency | % |
|---|---|---|
| Age Group | ||
| Children and adolescents | 18 | 0.5 |
| Youth | 26 | 0.6 |
| Adults | 1159 | 30.1 |
| Seniors | 2648 | 68.8 |
| Gender | ||
| Male | 2772 | 72.0 |
| Female | 1079 | 28.0 |
| Region of origin | ||
| Lima | 1645 | 42.7 |
| Rest of the coast | 1511 | 39.2 |
| Andes mountain range | 292 | 7.6 |
| Jungle | 403 | 10.5 |
| Place of occurrence of the death | ||
| Public hospital | 3071 | 79.8 |
| Private clinic | 78 | 2.0 |
| Home, accommodation, shelter, public road, | 686 | 17.8 |
| Transit to the hospital | ||
| Penitentiary institution | 16 | 0.4 |
| Diagnosis of comorbidities | ||
| Yes | 1211 | 31.4 |
| No | 2640 | 68.6 |
| Diagnosis with laboratory tests | ||
| RT-PCR | 1282 | 33.3 |
| Rapid test IgM detection/IgG | 2271 | 59.0 |
| Both tests | 298 | 7.7 |
| Region of Origin | Mortality Rate from COVID-19 * (per 100,000 People) |
|---|---|
| Lima | 14.0 |
| Rest of the coast | 18.1 |
| Andes mountain range | 3.1 |
| Jungle | 12.9 |
| Peru | 11.8 |
| Variable | X¯ ± SD/Frequency (%) | p-Value |
|---|---|---|
| Gender | 0.002 | |
| Male | 64.9 ± 14.0 | |
| Female | 66.5 ± 15.0 | |
| Region of origin | ||
| Lima | 65.6 ± 14.2 | 0.141 |
| Rest of the coast | 65.4 ± 14.3 | |
| Andes mountain range | 65.5 ± 13.6 | |
| Jungle | 63.8 ± 15.5 | |
| Diagnosis of comorbidities by age categories | ||
| Children and adolescents | 3/17 (17.6%) | 0.020 |
| Youth | 5/20 (25.0%) | |
| Adults | 332/1026 (32.4%) | |
| Seniors | 871/2358 (36.9%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramos, W.; Arrasco, J.; De La Cruz-Vargas, J.A.; Ordóñez, L.; Vargas, M.; Seclén-Ubillús, Y.; Luna, M.; Guerrero, N.; Medina, J.; Sandoval, I.; et al. Epidemiological Characteristics of Deaths from COVID-19 in Peru during the Initial Pandemic Response. Healthcare 2022, 10, 2404. https://doi.org/10.3390/healthcare10122404
Ramos W, Arrasco J, De La Cruz-Vargas JA, Ordóñez L, Vargas M, Seclén-Ubillús Y, Luna M, Guerrero N, Medina J, Sandoval I, et al. Epidemiological Characteristics of Deaths from COVID-19 in Peru during the Initial Pandemic Response. Healthcare. 2022; 10(12):2404. https://doi.org/10.3390/healthcare10122404
Chicago/Turabian StyleRamos, Willy, Juan Arrasco, Jhony A. De La Cruz-Vargas, Luis Ordóñez, María Vargas, Yovanna Seclén-Ubillús, Miguel Luna, Nadia Guerrero, José Medina, Isabel Sandoval, and et al. 2022. "Epidemiological Characteristics of Deaths from COVID-19 in Peru during the Initial Pandemic Response" Healthcare 10, no. 12: 2404. https://doi.org/10.3390/healthcare10122404
APA StyleRamos, W., Arrasco, J., De La Cruz-Vargas, J. A., Ordóñez, L., Vargas, M., Seclén-Ubillús, Y., Luna, M., Guerrero, N., Medina, J., Sandoval, I., Solis-Castro, M. E., & Loayza, M. (2022). Epidemiological Characteristics of Deaths from COVID-19 in Peru during the Initial Pandemic Response. Healthcare, 10(12), 2404. https://doi.org/10.3390/healthcare10122404






