Medical Dispute Cases Caused by Errors in Clinical Reasoning: An Investigation and Analysis
Abstract
1. Introduction
2. Method
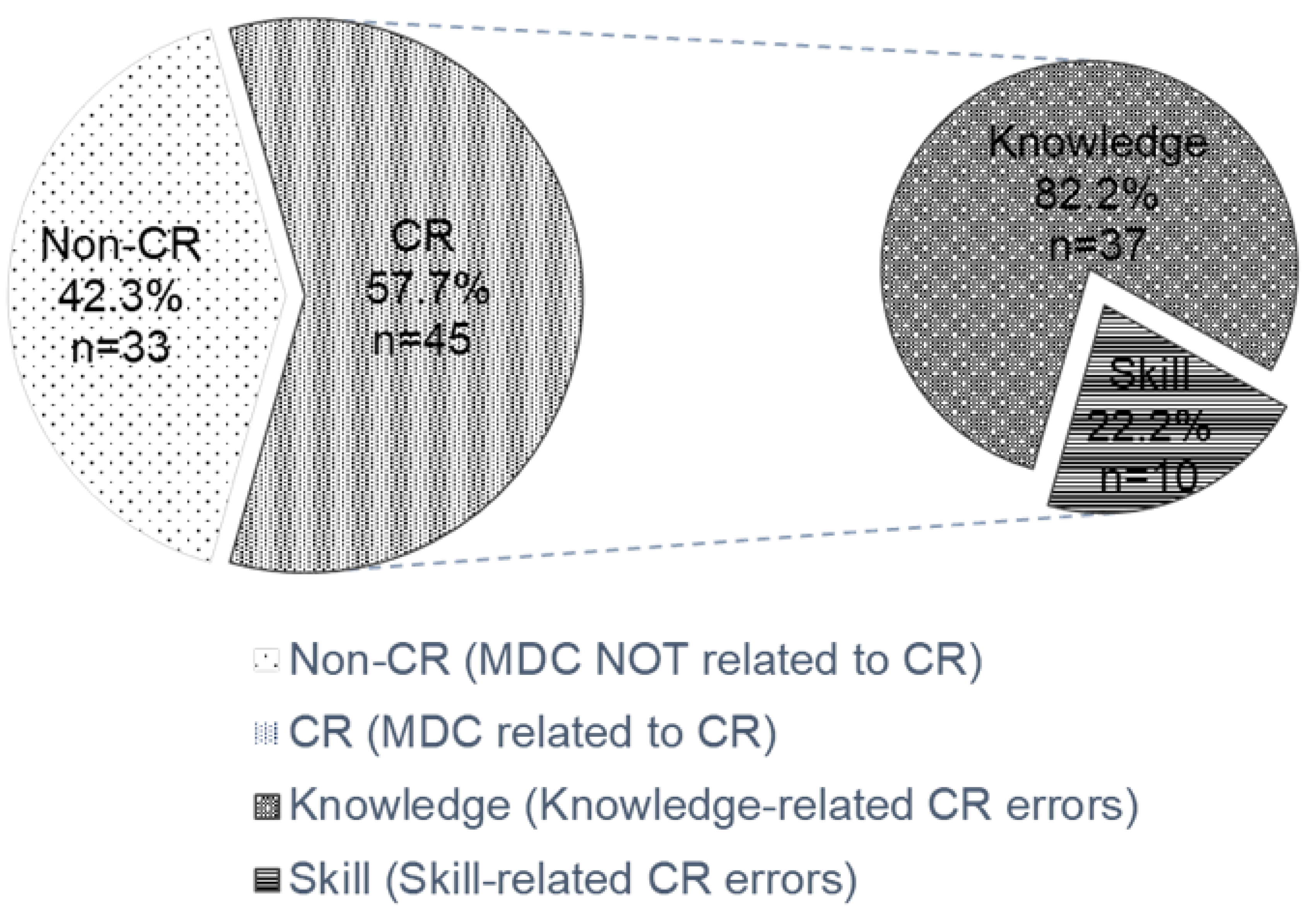
3. Results
4. Discussion
5. Implications
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hu, Y.-H.; Wang, C.-Y.; Huang, M.-S.; Lee, C.-H.; Wen, Y.-S. Analysis of the causes of surgery-related medical disputes in Taiwan: Need for acute care surgeons to improve quality of care. J. Chin. Med. Assoc. 2016, 79, 609–613. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, D.W.H.; Practice, H.K.P.; Lai, P.B.S. The practice of mediation to resolve clinical, bioethical, and medical malpractice disputes. Hong Kong Med. J. 2015, 21, 560–564. [Google Scholar] [CrossRef]
- Choi, J.W.; Kim, D.K.; Cho, C.K.; Park, S.J.; Son, Y.H. Trends in medical disputes involving anesthesia during July 2009–June 2018: An analysis of the Korean Society of Anesthesiologists database. Korean J. Anesthesiol. 2019, 72, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Jena, A.B.; Seabury, S.; Lakdawalla, D.; Chandra, A. Malpractice Risk According to Physician Specialty. N. Engl. J. Med. 2011, 365, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.-K.; Jeong, S.-J.; Kang, B.-K.; Lee, M.S. Medical dispute cases involving traditional Korean medical doctors: A survey. Eur. J. Integr. Med. 2014, 6, 497–501. [Google Scholar] [CrossRef]
- Wu, C.-Y.; Weng, H.-C.; Chen, R.-C. Time trends of assessments for medical dispute cases in Taiwan: A 20-year nationwide study. Intern. Med. J. 2013, 43, 1023–1030. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M. Evaluation of the third-party mediation mechanism for medical disputes in China. Med. Law 2011, 30, 401–415. [Google Scholar] [PubMed]
- Wu, C.; Lai, H.J.; Chen, R.C. Status of medicolegal problems in Taiwan. Formos. J. Med. 2009, 13, 1–8. [Google Scholar] [CrossRef]
- Kim, Y.D.; Moon, H.S. Review of Medical Dispute Cases in the Pain Management in Korea: A Medical Malpractice Liability Insurance Database Study. Korean J. Pain 2015, 28, 254–264. [Google Scholar] [CrossRef]
- Xu, P.; Fan, Z.; Li, T.; Wang, L.; Sun, Q.; Du, X.; Lian, B.; Zhang, L. Preventing surgical disputes through early detection and intervention: A case control study in China. BMC Health Serv. Res. 2015, 15, 5. [Google Scholar] [CrossRef][Green Version]
- Crone, K.G.; Muraski, M.B.; Skeel, J.D.; Love-Gregory, L.; Ladenson, J.H.; Gronowski, A.M. Between a Rock and a Hard Place: Disclosing Medical Errors. Clin. Chem. 2006, 52, 1809–1814. [Google Scholar] [CrossRef] [PubMed]
- Makary, M.A.; Daniel, M. Medical error—The third leading cause of death in the US. BMJ 2016, 353, i2139. [Google Scholar] [CrossRef] [PubMed]
- Melnyk, B.M.; Orsolini, L.; Tan, A.; Arslanian-Engoren, C.; Melkus, G.D.; Dunbar-Jacob, J.; Rice, V.H.; Millan, A.; Dunbar, S.B.; Braun, L.T.; et al. A National Study Links Nurses’ Physical and Mental Health to Medical Errors and Perceived Worksite Wellness. J. Occup. Environ. Med. 2018, 60, 126–131. [Google Scholar] [CrossRef]
- Kalra, J. Medical errors: An introduction to concepts. Clin. Biochem. 2004, 37, 1043–1051. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Y.; Zhang, L.; Yao, G.; Fang, Y. Analysis of current situation and influencing factor of medical disputes among different levels of medical institutions based on the game theory in Xiamen of China. Medicine 2018, 97, e12501. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System; Kohn, L.T., Corrigan, J.M., Donaldson, M.S., Eds.; National Academies Press (US): Washington, DC, USA, 2000. [Google Scholar]
- Graber, M.L. The incidence of diagnostic error in medicine. BMJ Qual. Saf. 2013, 22, ii21–ii27. [Google Scholar] [CrossRef]
- Berner, E.S.; Graber, M.L. Overconfidence as a Cause of Diagnostic Error in Medicine. Am. J. Med. 2008, 121, S2–S23. [Google Scholar] [CrossRef]
- Banning, M. Clinical reasoning and its application to nursing: Concepts and research studies. Nurse Educ. Pract. 2008, 8, 177–183. [Google Scholar] [CrossRef]
- Hoben, K.; Varley, R.; Cox, R. Clinical reasoning skills of speech and language therapy students. Int. J. Lang. Commun. Disord. 2007, 42, 123–135. [Google Scholar] [CrossRef]
- Norman, G.R.; Monteiro, S.; Sherbino, J.; Ilgen, J.S.; Schmidt, H.G.; Mamede, S. The Causes of Errors in Clinical Reasoning. Acad. Med. 2017, 92, 23–30. [Google Scholar] [CrossRef]
- Groves, M.; O’Rourke, P.; Alexander, H. Clinical reasoning: The relative contribution of identification, interpretation and hypothesis errors to misdiagnosis. Med. Teachnol. 2003, 25, 621–625. [Google Scholar] [CrossRef]
- Graber, M.L.; Kissam, S.; Payne, V.L.; Meyer, A.; Sorensen, A.; Lenfestey, N.; Tant, E.; Henriksen, K.; LaBresh, K.; Singh, H. Cognitive interventions to reduce diagnostic error: A narrative review. BMJ Qual. Saf. 2012, 21, 535–557. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, C.; Landry, M.; Xhignesse, M.; Voyer, G.; Tremblay-Lavoie, S.; Mamede, S.; Schmidt, H.; Rikers, R. Age-related decline and diagnostic performance of more and less prevalent clinical cases. Adv. Health Sci. Educ. 2015, 21, 561–570. [Google Scholar] [CrossRef] [PubMed]
- Thomas, E.J.; Petersen, L.A. Measuring errors and adverse events in health care. J. Gen. Intern. Med. 2003, 18, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Cutrer, W.B.; Sullivan, W.M.; Fleming, A.E. Educational Strategies for Improving Clinical Reasoning. Curr. Probl. Pediatr. Adolesc. Health Care 2013, 43, 248–257. [Google Scholar] [CrossRef]
- Nikopoulou-Smyrni, P.; Nikopoulos, C.K. A new integrated model of clinical reasoning: Development, description and preliminary assessment in patients with stroke. Disabil. Rehabil. 2007, 29, 1129–1138. [Google Scholar] [CrossRef]
- Thomas, E.J.; Studdert, D.M.; Burstin, H.R.; Orav, E.J.; Zeena, T.; Williams, E.J.; Howard, K.M.; Weiler, P.C.; Brennan, T.A. Incidence and Types of Adverse Events and Negligent Care in Utah and Colorado. Med. Care 2000, 38, 261–271. [Google Scholar] [CrossRef]
- Berge, K.V.D.; Mamede, S. Cognitive diagnostic error in internal medicine. Eur. J. Intern. Med. 2013, 24, 525–529. [Google Scholar] [CrossRef]
- Hwang, C.-Y.; Wu, C.-H.; Cheng, F.-C.; Yen, Y.-L.; Wu, K.-H. A 12-year analysis of closed medical malpractice claims of the Taiwan civil court. Medicine 2018, 97, e0237. [Google Scholar] [CrossRef]
- Watari, T.; Tokuda, Y.; Mitsuhashi, S.; Otuki, K.; Kono, K.; Nagai, N.; Onigata, K.; Kanda, H. Factors and impact of physicians’ diagnostic errors in malpractice claims in Japan. PLoS ONE 2020, 15, e0237145. [Google Scholar] [CrossRef]
- Liu, J.; Liu, P.; Gong, X.; Liang, F. Relating Medical Errors to Medical Specialties: A Mixed Analysis Based on Litigation Documents and Qualitative Data. Risk Manag. Health. Policy 2020, 13, 335–345. [Google Scholar] [CrossRef] [PubMed]
- Croskerry, P. From Mindless to Mindful Practice—Cognitive Bias and Clinical Decision Making. N. Engl. J. Med. 2013, 368, 2445–2448. [Google Scholar] [CrossRef] [PubMed]
- Benishek, L.E.; Weaver, S.J.; Newman-Toker, D.E. The Cognitive Psychology of Diagnostic Errors. Sci. Am. Neurol. 2015. [Google Scholar] [CrossRef]
- Petrucci, E.; Vittori, A.; Cascella, M.; Vergallo, A.; Fiore, G.; Luciani, A.; Pizzi, B.; Degan, G.; Fineschi, V.; Marinangeli, F. Litigation in Anesthesia and Intensive Care Units: An Italian Retrospective Study. Healthcare 2021, 9, 1012. [Google Scholar] [CrossRef] [PubMed]
- Ghaith, S.; Campbell, R.L.; Pollock, J.R.; Torbenson, V.E.; Lindor, R.A. Medical Malpractice Lawsuits Involving Trainees in Obstetrics and Gynecology in the USA. Healthcare 2022, 10, 1328. [Google Scholar] [CrossRef] [PubMed]
- Thiels, C.A.; Choudhry, A.J.; Ray-Zack, M.; Lindor, R.A.; Bergquist, J.; Habermann, E.; Zielinski, M.D. Medical Malpractice Lawsuits Involving Surgical Residents. JAMA Surg. 2018, 153, 8–13. [Google Scholar] [CrossRef]
- Khan, I.; Arsanious, M. Does the perception of severity of medical error differ between varying levels of clinical seniority? Adv. Med. Educ. Pract. 2018, 9, 443–452. [Google Scholar] [CrossRef]
- Mayer, R.E.; Smith, M.U. Toward a Unified Theory of Problem Solving: Views from the Content Domains. Am. J. Psychol. 1993, 106, 132. [Google Scholar] [CrossRef]
- Morra, M.; Braund, H.; Hall, A.K.; Szulewski, A. Cognitive load and processes during chest radiograph interpretation in the emergency department across the spectrum of expertise. AEM Educ. Train. 2021, 5, e10693. [Google Scholar] [CrossRef]
- Taylor, J.A.; Brownstein, D.; Christakis, D.A.; Blackburn, S.; Strandjord, T.P.; Klein, E.J.; Shafii, J. Use of Incident Reports by Physicians and Nurses to Document Medical Errors in Pediatric Patients. Pediatrics 2004, 114, 729–735. [Google Scholar] [CrossRef]
- Rowin, E.J.; Lucier, D.; Pauker, S.G.; Kumar, S.; Chen, J.; Salem, D.N. Does Error and Adverse Event Reporting by Physicians and Nurses Differ? Jt. Comm. J. Qual. Patient Saf. 2008, 34, 537–545. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare 26 June 2016. Available online: https://dep.mohw.gov.tw/doma/cp-2712-7681-106.html (accessed on 5 August 2018).
- Raveesh, B.N.; Nayak, R.B.; Kumbar, S.F. Preventing medico-legal issues in clinical practice. Ann. Indian Acad. Neurol. 2016, 19, 15. [Google Scholar] [CrossRef] [PubMed]
- TG, G. Preventive and improvement measures in medical disputes. Law Mon. 2011, 62, 66–74. [Google Scholar] [CrossRef]
- Eldarir, S.A.H.; Sebaae, H.A.E.; Feky, H.A.E.; Hussien, H.A.; Fadi, N.A.E.; Shaeer, I.E.H. An Introduction of OSCE versus Traditional Method in Nursing Education: Facul-ty Capacity Building & Students’ Perspectives. Am. J. Sci. 2010, 6, 1002–1014. [Google Scholar]
- Fanous, A.; Rappaport, J.; Young, M.; Park, Y.S.; Manoukian, J.; Nguyen, L.H.P.L.H.P. A longitudinal simulation-based ethical-legal curriculum for otolaryngology residents. Laryngoscope 2017, 127, 2501–2509. [Google Scholar] [CrossRef]
- Klein, M.; Otto, B.; Fischer, M.R.; Stark, R. Fostering medical students’ clinical reasoning by learning from errors in clinical case vignettes: Effects and conditions of additional prompting procedures to foster self-explanations. Adv. Health. Sci. Educ. 2019, 24, 331–351. [Google Scholar] [CrossRef]
- Dreifuerst, K.T. Using Debriefing for Meaningful Learning to Foster Development of Clinical Reasoning in Simulation. J. Nurs. Educ. 2012, 51, 326–333. [Google Scholar] [CrossRef]
- Cruess, R.L.; Cruess, S.R.; Boudreau, J.D.; Snell, L.; Steinert, Y. Reframing Medical Education to Support Professional Identity Formation. Acad. Med. 2014, 89, 1446–1451. [Google Scholar] [CrossRef]
- Young, M.; Thomas, A.; Lubarsky, S.; Ballard, T.; Gordon, D.; Gruppen, L.D.; Holmboe, E.; Ratcliffe, T.; Rencic, J.; Schuwirth, L.; et al. Drawing Boundaries. Acad. Med. 2018, 93, 990–995. [Google Scholar] [CrossRef]
- Simmons, B. Clinical reasoning: Concept analysis. J. Adv. Nurs. 2010, 66, 1151–1158. [Google Scholar] [CrossRef]
| Dispute Cases | Clinical Reasoning Related Cases | ||||
|---|---|---|---|---|---|
| Year | No. of Cases | Proportion (%) | No. of Cases | Proportion (%) | Proportion of Clinical Reasoning Related Cases by Year (%) |
| 2011 | 16 | 20.5 | 5 | 11.1 | 31.3 |
| 2012 | 19 | 24.4 | 11 | 24.4 | 57.9 |
| 2013 | 19 | 24.4 | 11 | 24.4 | 57.9 |
| 2014 | 16 | 20.5 | 11 | 24.4 | 68.8 |
| 2015 | 8 | 10.3 | 7 | 15.6 | 87.5 |
| Total | 78 | 100.0 | 45 | 100.0 | 57.7 |
| Dispute Cases | Clinical Reasoning Related Cases | ||||
| Healthcare Professionals | No. of Cases * | Proportion (%) | No. of Cases * | Proportion (%) | Proportion of Clinical Reasoning Related Cases by Profession (%) |
| Attending Physicians | 40 | 51.3 | 25 | 55.6 | 62.5 |
| Residents | 16 | 20.5 | 14 | 31.1 | 87.5 |
| Registered Nurses | 13 | 16.7 | 11 | 24.4 | 84.6 |
| Technicians | 3 | 11.5 | 2 | 4.4 | 66.7 |
| Dispute Cases | Clinical Reasoning Related Cases | ||||
|---|---|---|---|---|---|
| Causality * | Yes | 37 | 47.4% | 25 | 55.6% |
| No | 41 | 52.6% | 20 | 44.4% | |
| Total | 78 | 45 | |||
| Litigation | Yes | 19 | 24.4% | 12 | 26.7% |
| No | 59 | 75.6% | 33 | 73.3% | |
| Total | 78 | 45 | |||
| Specialties and Healthcare Professions | Number of Healthcare Professionals | Proportion | Healthcare Professionals Associated with Clinical Reasoning Dispute Cases | Proportion |
|---|---|---|---|---|
| Obstetrics and gynecology | 10 | 11.1% | 4 | 7.8% |
| General surgery | 8 | 8.9% | 5 | 9.8% |
| System-related (Instrument) | 9 | 10.0% | 1 | 2.0% |
| Emergency medicine | 7 | 7.8% | 3 | 5.9% |
| Nursing | 5 | 5.6% | 5 | 9.8% |
| Orthopedics | 5 | 5.6% | 5 | 9.8% |
| Plastic surgery | 4 | 4.4% | 2 | 3.9% |
| Internal medicine | 4 | 4.4% | 3 | 5.9% |
| Gastroenterology | 3 | 3.3% | 3 | 5.9% |
| Neurosurgery | 3 | 3.3% | 1 | 2.0% |
| Pulmonology | 3 | 3.3% | 1 | 2.0% |
| Anesthesiology | 3 | 3.3% | 1 | 2.0% |
| Dentistry | 3 | 3.3% | 2 | 3.9% |
| Neurology | 3 | 3.3% | 3 | 5.9% |
| Medical imaging | 2 | 2.2% | 1 | 2.0% |
| Traumatology | 2 | 2.2% | 1 | 2.0% |
| Psychiatry | 1 | 1.1% | 0 | 0.0% |
| Otorhinolaryngology | 2 | 2.2% | 1 | 2.0% |
| Radiology | 2 | 2.2% | 2 | 3.9% |
| Metabolism and endocrinology | 1 | 1.1% | 1 | 2.0% |
| Neonatology | 1 | 1.1% | 1 | 2.0% |
| Acupuncture | 1 | 1.1% | 0 | 0.0% |
| Cardiology | 1 | 1.1% | 1 | 2.0% |
| Cardiac surgery | 1 | 1.1% | 1 | 2.0% |
| Colorectal surgery | 1 | 1.1% | 1 | 2.0% |
| Health management center | 1 | 1.1% | 0 | 0.0% |
| Ophthalmology | 1 | 1.1% | 1 | 2.0% |
| Physical medicine and rehabilitation | 1 | 1.1% | 0 | 0.0% |
| Infectious disease | 1 | 1.1% | 0 | 0.0% |
| Pharmacy | 1 | 1.1% | 1 | 2.0% |
| Total | 90 | 100% | 51 | 100% |
| Job Position | Seniority (Years) | Number |
|---|---|---|
| Physicians | Over 25 | 0 |
| 21–25 | 5 | |
| 16–20 | 3 | |
| 11–15 | 6 | |
| 5–10 | 5 | |
| Less than 5 | 11 | |
| Residents | R6 | 0 |
| R5 | 2 | |
| R4 | 5 | |
| R3 | 3 | |
| R2 | 5 | |
| R1 | 2 |
| Hospital Branches | Number of Cases | Number of Beds |
|---|---|---|
| North centre | 43 | 4176 |
| North district | 1 | 1089 |
| South centre | 22 | 2680 |
| South district | 12 | 1384 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, C.-Y.; Lai, H.-Y.; Lee, C.-H.; Chen, M.-M. Medical Dispute Cases Caused by Errors in Clinical Reasoning: An Investigation and Analysis. Healthcare 2022, 10, 2224. https://doi.org/10.3390/healthcare10112224
Lee C-Y, Lai H-Y, Lee C-H, Chen M-M. Medical Dispute Cases Caused by Errors in Clinical Reasoning: An Investigation and Analysis. Healthcare. 2022; 10(11):2224. https://doi.org/10.3390/healthcare10112224
Chicago/Turabian StyleLee, Ching-Yi, Hung-Yi Lai, Ching-Hsin Lee, and Mi-Mi Chen. 2022. "Medical Dispute Cases Caused by Errors in Clinical Reasoning: An Investigation and Analysis" Healthcare 10, no. 11: 2224. https://doi.org/10.3390/healthcare10112224
APA StyleLee, C.-Y., Lai, H.-Y., Lee, C.-H., & Chen, M.-M. (2022). Medical Dispute Cases Caused by Errors in Clinical Reasoning: An Investigation and Analysis. Healthcare, 10(11), 2224. https://doi.org/10.3390/healthcare10112224





