Vascular Risk Factors in Ischemic Stroke Survivors: A Retrospective Study in Catalonia, Spain
Abstract
1. Introduction
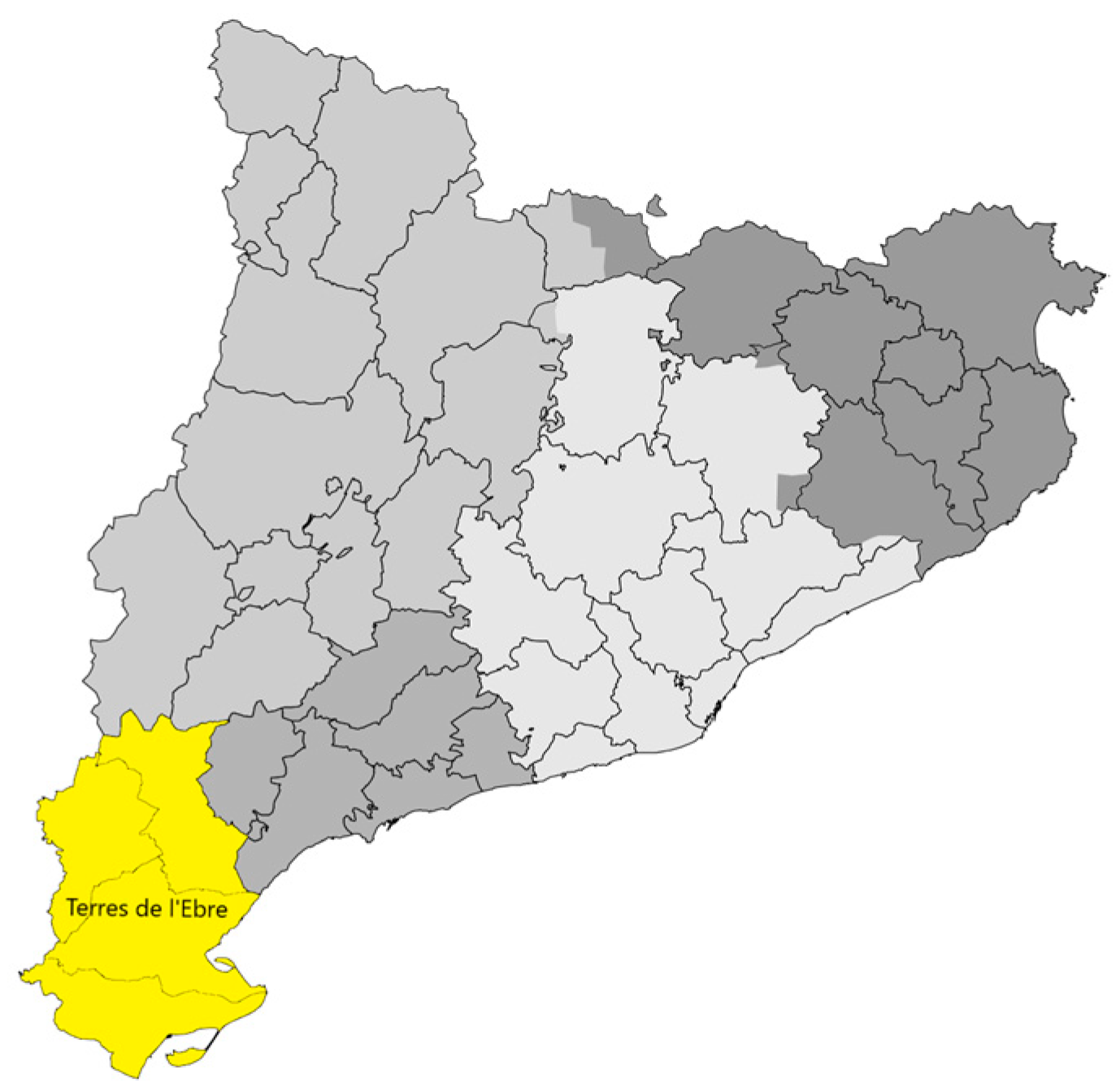
2. Materials and Methods
Data Analysis
3. Results
4. Discussions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boulanger, M.; Béjot, Y.; Rothwell, P.M.; Touzé, E. Long-term risk of myocardial infarction compared to recurrent stroke after transient ischemic attack and ischemic stroke: Systematic review and meta-analysis. J. Am. Heart Assoc. 2018, 7, e007267. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Estadística. Instituto Nacional de Estadística Estadística de Defunciones Según la Causa de Muerte; INE: Madrid, Spain, 2021; pp. 1–8. [Google Scholar]
- Kleindorfer, D.O.; Towfighi, A.; Chaturvedi, S.; Cockroft, K.M.; Gutierrez, J.; Lombardi-Hill, D.; Kamel, H.; Kernan, W.N.; Kittner, S.J.; Leira, E.C.; et al. Guideline for the Prevention of Stroke in Patients with Stroke and Transient Ischemic Attack; A Guideline from the American Heart Association; American Stroke Association: Dallas, TX, USA, 2021. [Google Scholar]
- Poggesi, A.; Insalata, G.; Papi, G.; Rinnoci, V.; Donnini, I.; Martini, M.; Falsini, C.; Hakiki, B.; Romoli, A.; Barbato, C.; et al. Gender differences in post-stroke functional outcome at discharge from an intensive rehabilitation hospital. Eur. J. Neurol. 2021, 28, 1601–1608. [Google Scholar] [CrossRef]
- Zeng, X.; Deng, A.; Ding, Y. The INTERSTROKE study on risk factors for stroke. Lancet 2017, 389, 7–13. [Google Scholar] [CrossRef]
- Instituto de Estadística de Cataluña Población en Cataluña y por Provincias. Available online: https://www.idescat.cat/pub/?id=aec&n=245&lang=es (accessed on 20 April 2022).
- Bristol-Myers Squibb El Atlas del Ictus. Cataluña. 2019. Available online: https://www.sen.es/images/2020/atlas/Informes_comunidad/Informe_ICTUS_Cataluna.pdf (accessed on 20 April 2022).
- Ministerio de Sanidad eCIE10ES. Available online: https://eciemaps.mscbs.gob.es/ecieMaps/browser/metabuscador.html (accessed on 20 April 2022).
- Jovin, T.G.; Chamorro, A.; Cobo, E.; De Miquel, M.A.; Molina, C.A.; Rovira, A.; San Román, L.; Serena, J.; Abilleira, S.; Ribó, M.; et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N. Engl. J. Med. 2015, 372, 2296–2306. [Google Scholar] [CrossRef] [PubMed]
- 5È. Audit Clínic de l’Ictus. Catalunya 2018/2019. 2021. Available online: https://canalsalut.gencat.cat/web/.content/_A-Z/I/ictus/prof/documents/arxius/5e-audit-ictus.pdf (accessed on 8 July 2022).
- Rojas, J.I.; Zurrú, M.C.; Romano, M.; Patrucco, L.C. Acute ischemic stroke in patients aged 80 or older. Medicina 2007, 67, 701–704. [Google Scholar] [PubMed]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2018, 49, e46–e110. [Google Scholar] [CrossRef] [PubMed]
- Norrving, B.; Bray, B.D.; Asplund, K.; Heuschmann, P.; Langhorne, P.; Rudd, A.G.; Wagner, M.; Wiedmann, S.; Wolfe, C.D.A. Cross-national key performance measures of the quality of acute stroke care in Western Europe. Stroke 2015, 46, 2891–2895. [Google Scholar] [CrossRef]
- Dahl, S.; Hjalmarsson, C.; Andersson, B. Sex differences in risk factors, treatment, and prognosis in acute stroke. Womens Health 2020, 16. [Google Scholar] [CrossRef]
- Giroud, M.; Delpont, B.; Daubail, B.; Blanc, C.; Durier, J.; Giroud, M.; Béjot, Y. Temporal Trends in Sex Differences with Regard to Stroke Incidence: The Dijon Stroke Registry (1987–2012). Stroke 2017, 48, 846–849. [Google Scholar] [CrossRef]
- Girijala, R.L.; Sohrabji, F.; Bush, R.L. Sex differences in stroke: Review of current knowledge and evidence. Vasc. Med. 2017, 22, 135–145. [Google Scholar] [CrossRef]
- Roy-O’Reilly, M.; McCullough, L.D. Age and sex are critical factors in ischemic stroke pathology. Endocrinology 2018, 159, 3120–3131. [Google Scholar] [CrossRef] [PubMed]
- Bonkhoff, A.K.; Karch, A.; Weber, R.; Wellmann, J.; Berger, K. Female Stroke: Sex Differences in Acute Treatment and Early Outcomes of Acute Ischemic Stroke. Stroke 2021, 52, 406–415. [Google Scholar] [CrossRef]
- López Espuela, F.; Portilla Cuenca, J.C.; Leno Díaz, C.; Párraga Sánchez, J.M.; Gamez-Leyva, G.; Casado Naranjo, I. Sex differences in long-term quality of life after stroke: Influence of mood and functional status. Neurologia 2020, 35, 470–478. [Google Scholar] [CrossRef]
- Arboix, A.; Massons, J.; García-Eroles, L.; Oliveres, M. Ictus en adultos jóvenes: Rasgos clínicos y frecuencia de presentación en 280 pacientes según el subtipo etiológico. Med. Clin. 2016, 146, 207–211. [Google Scholar] [CrossRef] [PubMed]
- Avan, A.; Digaleh, H.; Di Napoli, M.; Stranges, S.; Behrouz, R.; Shojaeianbabaei, G.; Amiri, A.; Tabrizi, R.; Mokhber, N.; Spence, J.D.; et al. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: An ecological analysis from the Global Burden of Disease Study 2017. BMC Med. 2019, 17, 191. [Google Scholar] [CrossRef] [PubMed]
- Vivanco-Hidalgo, R.M.; Abilleira, S.; Salvat-Plana, M.; Ribera, A.; Gallofré, G.; Gallofré, M. Innovation in systems of care in acute phase of ischemic stroke. The experience of the catalan stroke programme. Front. Neurol. 2018, 9, 427. [Google Scholar] [CrossRef] [PubMed]
- Gonzalvo-Cirac, M. La transición de la Mortalidad en el Siglo XX: El Caso de Tarragona. Master’s Thesis, UIC Barcelona, Barcelona, Spain, 2010. [Google Scholar]
- Satuè Gracia, E.M. Epidemiología de la Enfermedad Cerebrovascular Isquémica en Mayores de 60 Años del Área de Tarragona: Datos del Estudio CAPAMIS. Ph.D. Thesis, Universitat Rovira Virgili, Tarragona, Spain, 2018. [Google Scholar]
- Séculi, E.; Brugulat, P.; Medina, A.; Juncà, S.; Tresserras, R.; Salleras, L. La detección de factores de riesgo cardiovascular en la red reformada de atención primaria en Cataluña. Comparación entre los años 1995 y 2000. Atención Primaria 2003, 31, 156–162. [Google Scholar] [CrossRef]
- Emdin, C.A.; Wong, C.X.; Hsiao, A.J.; Altman, D.G.; Peters, S.A.E.; Woodward, M.; Odutayo, A.A. Atrial fibrillation as risk factor for cardiovascular disease and death in women compared with men: Systematic review and meta-analysis of cohort studies. BMJ 2016, 352, h7013. [Google Scholar] [CrossRef] [PubMed]
- Erratum: Heart disease and stroke statistics-2011 update: A report from the American Heart Association (Circulation (2011) 123 (e18-e209)). Circulation 2011, 123, e240. [CrossRef]
- Peters, S.A.; Huxley, R.R.; Woodward, M. Diabetes as a risk factor for stroke in women compared with men: A systematic review and meta-analysis of 64 cohorts, including 775,385 individuals and 12,539 strokes. Lancet 2014, 383, 1973–1980. [Google Scholar] [CrossRef]
- Roger, V.L.; Go, A.S.; Lloyd-Jones, D.M.; Adams, R.J.; Berry, J.D.; Brown, T.M.; Carnethon, M.R.; Dai, S.; de Simone, G.; Ford, E.S.; et al. Heart Disease and Stroke Statistics—2011 Update: A Report From the American Heart Association RD on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2011, 123, 18–209. [Google Scholar] [CrossRef] [PubMed]
| Population (n = 2054) | Dx 2011-15 (n = 829) | Dx 2016-20 (n = 1225) | p-Value | |
|---|---|---|---|---|
| Diagnostic age, years (IQR) | 76 (67–83) | 75 (65–82) | 77 (68–84) | <0.001 |
| Age group n (%) | 0.013 | |||
| <55 | 194 (9.44) | 85 (10.25) | 109 (8.90) | |
| 55–80 | 1139 (55.45) | 484 (58.38) | 655 (53.47) | |
| >80 | 721 (35.10) | 260 (31.36) | 461 (37.63) | |
| Sex n (%) | 0.962 | |||
| Men | 1157 (56.33) | 468 (56.45) | 689 (56.24) | |
| Women | 897 (43.67) | 361 (43.55) | 536 (43.76) | |
| No. VRFs n (%) | 0.284 | |||
| 1–2 | 1160 (56.48) | 456 (55.01) | 704 (57.47) | |
| 3–4 | 813 (39.58) | 344 (41.50) | 469 (38.29) | |
| >4 | 81 (3.94) | 29 (3.50) | 52 (4.24) | |
| VRF type n (%) | 0.243 | |||
| HPN | 1788 (35.86) | 725 (35.42) | 1063 (36.17) | |
| Dyslipidemia | 1300 (26.07) | 535 (26.14) | 765 (26.03) | |
| Heart disease and AF | 753 (15.10) | 289 (14.12) | 464 (15.79) | |
| Hyperglycemia and DM | 313 (6.28) | 134 (6.55) | 179 (6.09) | |
| Overweight and obesity | 627 (12.58) | 270 (13.19) | 357 (12.15) | |
| Alcoholism | 74 (1.48) | 29 (1.42) | 45 (1.53) | |
| Smoking | 131 (2.63) | 65 (3.18) | 66 (2.25) |
| VRF (n = 4986) n (%) | <55 | 55–80 | >80 | p-Value |
|---|---|---|---|---|
| HPN | 144 (34.87) | 998 (34.31) | 646 (38.82) | <0.001 |
| Dyslipidemia | 117 (28.33) | 766 (26.33) | 417 (25.06) | <0.001 |
| Heart disease and AF | 30 (7.26) | 404 (13.89) | 319 (19.17) | <0.001 |
| Hyperglycemia and DM | 28 (6.78) | 205 (7.05) | 80 (4.81) | <0.001 |
| Overweight and obesity | 73 (17.68) | 394 (13.54) | 160 (9.62) | <0.001 |
| Alcoholism | 14 (3.39) | 52 (1.79) | 8 (0.48) | <0.001 |
| Smoking | 7 (1.69) | 90 (3.09) | 34 (2.04) | <0.001 |
| VRF Number (n = 2054) n (%) | <55 | 55–80 | >80 | p-Value |
|---|---|---|---|---|
| 1–2 | 130 (67.01) | 591 (51.89) | 439 (60.89) | <0.001 |
| 3–4 | 60 (30.93) | 487 (42.76) | 266 (36.89) | |
| >4 | 4 (2.06) | 61 (5.35) | 16 (2.22) |
| Age Groups | <55 | p | 55–80 | p | >80 | p | |||
|---|---|---|---|---|---|---|---|---|---|
| Men 135 (69.59) | Women 59 (30.41) | Men 736 (64.62) | Women 403 (35.38) | Men 286 (39.67) | Women 435 (60.33) | ||||
| 1-2 VRFs (n = 644) | 89 (65.93) | 41 (69.49) | 0.891 | 378 (51.36) | 213 (52.85) | 0.113 | 177 (61.89) | 262 (60.23) | 0.121 |
| 3-4 VRFs (n = 453) | 43 (31.85) | 17 (28.81) | 311 (42.26) | 176 (43.67) | 99 (34.62) | 167 (38.39) | |||
| >4 VRFs (n = 60) | 3 (2.22) | 1 (1.69) | 47 (6.39) | 14 (3.47) | 10 (3.50) | 6 (1.38) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reverté-Villarroya, S.; Suñer-Soler, R.; Zaragoza-Brunet, J.; Martín-Ozaeta, G.; Esteve-Belloch, P.; Payo-Froiz, I.; Sauras-Colón, E.; Lopez-Espuela, F. Vascular Risk Factors in Ischemic Stroke Survivors: A Retrospective Study in Catalonia, Spain. Healthcare 2022, 10, 2219. https://doi.org/10.3390/healthcare10112219
Reverté-Villarroya S, Suñer-Soler R, Zaragoza-Brunet J, Martín-Ozaeta G, Esteve-Belloch P, Payo-Froiz I, Sauras-Colón E, Lopez-Espuela F. Vascular Risk Factors in Ischemic Stroke Survivors: A Retrospective Study in Catalonia, Spain. Healthcare. 2022; 10(11):2219. https://doi.org/10.3390/healthcare10112219
Chicago/Turabian StyleReverté-Villarroya, Silvia, Rosa Suñer-Soler, Jose Zaragoza-Brunet, Gisela Martín-Ozaeta, Patricia Esteve-Belloch, Iago Payo-Froiz, Esther Sauras-Colón, and Fidel Lopez-Espuela. 2022. "Vascular Risk Factors in Ischemic Stroke Survivors: A Retrospective Study in Catalonia, Spain" Healthcare 10, no. 11: 2219. https://doi.org/10.3390/healthcare10112219
APA StyleReverté-Villarroya, S., Suñer-Soler, R., Zaragoza-Brunet, J., Martín-Ozaeta, G., Esteve-Belloch, P., Payo-Froiz, I., Sauras-Colón, E., & Lopez-Espuela, F. (2022). Vascular Risk Factors in Ischemic Stroke Survivors: A Retrospective Study in Catalonia, Spain. Healthcare, 10(11), 2219. https://doi.org/10.3390/healthcare10112219








