Impact of COVID-19 Pandemic on Health-Related Quality of Life and Physical Activity of Patients in Hemodialysis
Abstract
1. Introduction
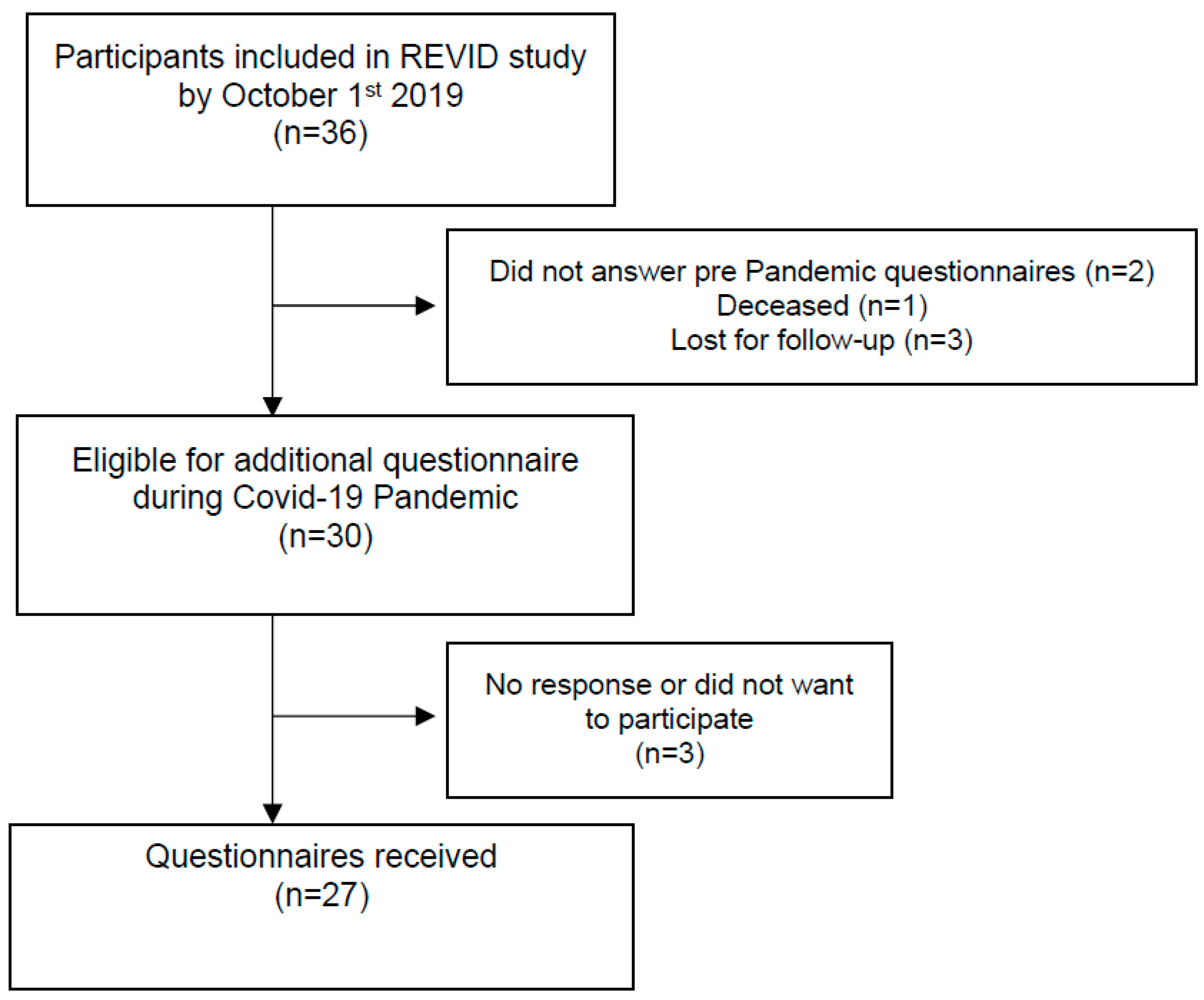
2. Materials and Methods
2.1. Demographic, Anthropometric and Laboratory Data
2.2. Health-Related Quality of Life and Physical Activity Level
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhang, Q.-L.; Wang, S.; Zhang, Y.; Meng, F. The effect of refined nursing intervention on patients undergoing maintenance hemodialysis in the hemodialysis center during the COVID-19 epidemic. BMC Nurs. 2021, 20, 66. [Google Scholar] [CrossRef] [PubMed]
- Emil-Marian, A.; Reka, K.; Adrian, M.V.; Septimiu, V.; Eliza-Mihaela, A.; Eliza, R. Impact of COVID-19 pandemic on Vascular Surgery Unit activity in Central Romania. Front. Surg. 2022, 9, 883935. [Google Scholar] [CrossRef] [PubMed]
- Robertson, E.; Hershenfield, K.; Grace, S.; Stewart, D.E. The Psychosocial Effects of Being Quarantined following Exposure to SARS: A Qualitative Study of Toronto Health Care Workers. Can. J. Psychiatry 2004, 49, 403–407. [Google Scholar] [CrossRef]
- Yamada, T.; Mikami, T.; Chopra, N.; Miyashita, H.; Chernyavsky, S.; Miyashita, S. Patients with chronic kidney disease have a poorer prognosis of coronavirus disease 2019 (COVID-19): An experience in New York City. Int. Urol. Nephrol. 2020, 52, 1405–1406. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.J.; Alqarni, K.A.; McGrath-Chong, M.E.; Bargman, J.M.; Chan, C.T. Anxiety and psychosocial impact during coronavirus disease 2019 in home dialysis patients. Nephrology 2022, 27, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Segura-Orti, E.; Koufaki, P.; Kouidi, E. Bridging the gap from research to practice for enhanced health-related quality of life in people with chronic kidney disease. Clin. Kidney J. 2021, 14, ii34–ii42. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.T.Q.; Cockwell, P.; Maxwell, A.P.; Griffin, M.; O’Brien, T.; O’Neill, C. Chronic kidney disease, health-related quality of life and their associated economic burden among a nationally representative sample of community dwelling adults in England. PLoS ONE 2018, 13, e0207960. [Google Scholar] [CrossRef]
- Østhus, T.B.H.; Preljevic, V.T.; Sandvik, L.; Leivestad, T.; Nordhus, I.H.; Dammen, T.; Os, I. Mortality and health-related quality of life in prevalent dialysis patients: Comparison between 12-items and 36-items short-form health survey. Health Qual. Life Outcomes 2012, 10, 46. [Google Scholar] [CrossRef]
- Chen, X.; Xu, Q.; Lin, H.; Zhu, J.; Chen, Y.; Zhao, Q.; Fu, C.; Wang, N. Quality of life during the epidemic of COVID-19 and its associated factors among enterprise workers in East China. BMC Public Health 2021, 21, 1370. [Google Scholar] [CrossRef]
- Voorend, C.G.N.; van Oevelen, M.; Nieberg, M.; Meuleman, Y.; Franssen, C.F.M.; Joosten, H.; Berkhout-Byrne, N.C.; Abrahams, A.C.; Mooijaart, S.P.; Bos, W.J.W.; et al. POLDER investigators Impact of the COVID-19 pandemic on symptoms of anxiety and depression and health-related quality of life in older patients with chronic kidney disease. BMC Geriatr. 2021, 21, 650. [Google Scholar] [CrossRef]
- Segura-Ortí, E.; Gordon, P.L.; Doyle, J.W.; Johansen, K.L. Correlates of Physical Functioning and Performance Across the Spectrum of Kidney Function. Clin. Nurs. Res. 2018, 27, 579–596. [Google Scholar] [CrossRef] [PubMed]
- Segura-Orti, E. Exercise in hemodialysis patients: A literature systematic review. Nefrologia 2010, 30, 236–246. [Google Scholar] [PubMed]
- Huang, M.; Lv, A.; Wang, J.; Xu, N.; Ma, G.; Zhai, Z.; Zhang, B.; Gao, J.; Ni, C. Exercise Training and Outcomes in Hemodialysis Patients: Systematic Review and Meta-Analysis. Am. J. Nephrol. 2019, 50, 240–254. [Google Scholar] [CrossRef] [PubMed]
- Lesser, I.A.; Nienhuis, C.P. The Impact of COVID-19 on Physical Activity Behavior and Well-Being of Canadians. Int. J. Environ. Res. Public Health 2020, 17, 3899. [Google Scholar] [CrossRef] [PubMed]
- Hall, G.; Laddu, D.R.; Phillips, S.A.; Lavie, C.J.; Arena, R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog. Cardiovasc. Dis. 2021, 64, 108–110. [Google Scholar] [CrossRef] [PubMed]
- Patterson, R.; McNamara, E.; Tainio, M.; de Sa, T.H.; Smith, A.D.; Sharp, S.J.; Edwards, P.; Woodcock, J.; Brage, S.; Wijndaele, K. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: A systematic review and dose response meta-analysis. Eur. J. Epidemiol. 2018, 33, 811–829. [Google Scholar] [CrossRef] [PubMed]
- Hishii, S.; Miyatake, N.; Nishi, H.; Katayama, A.; Ujike, K.; Koumoto, K.; Suzuki, H.; Hashimoto, H. Relationship between Sedentary Behavior and All-cause Mortality in Japanese Chronic Hemodialysis Patients: A Prospective Cohort Study. Acta Med. Okayama 2019, 73, 419–425. [Google Scholar]
- Alonso, J.; Regidor, E.; Barrio, G.; Prieto, L.; Rodríguez, C.; De La Fuente, L. Population reference values of the Spanish version of the Health Questionnaire SF-36. Med. Clín. 1998, 111, 410–416. [Google Scholar]
- Ware, J.; Kosinski, M.; Keller, S. SF-36 Physical and Mental Health Summary Scales: A User Manual; The Health Institute, New England Medical Center: Boston, MA, USA, 1994. [Google Scholar]
- Johansen, K.L.; Painter, P.; Kent-Braun, J.A.; Ng, A.V.; Carey, S.; Da Silva, M.; Chertow, G.M. Validation of questionnaires to estimate physical activity and functioning in end-stage renal disease. Kidney Int. 2001, 59, 1121–1127. [Google Scholar] [CrossRef]
- Jiménez, A.J.; Simó, V.E.; Periz, L.A.; Ortí, E.S. The Relationship between Physical Activity Levels and Functional Capacity in Patients with Advanced Chronic Kidney Disease. Clin. Nurs. Res. 2021, 30, 360–368. [Google Scholar] [CrossRef]
- Fix, A.; Daughton, D. Human Activity Profile (HAP) Manual; Psychological Assessment Resources Inc.: Odessa, FL, USA, 1986. [Google Scholar]
- Overend, T.; Anderson, C.; Sawant, A.; Perryman, B.; Locking-Cusolito, H. Relative and Absolute Reliability of Physical Function Measures in People with End-Stage Renal Disease. Physiother. Can. 2010, 62, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Keemss, J.; Sieland, J.; Pfab, F.; Banzer, W. Effects of COVID-19 Lockdown on Physical Performance, Sleep Quality, and Health-Related Quality of Life in Professional Youth Soccer Players. Front. Sports Act. Living 2022, 4, 875767. [Google Scholar] [CrossRef] [PubMed]
- Firat, M.; Vardar-Yagli, N.; Saglam, M.; Yildirim, T.; Erdem, Y. Quality of life and physical activity level in patients with chronic kidney disease during COVID-19 pandemic. Psychol. Health Med. 2022, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Segura-Orti, E.; Johansen, K.L. Exercise in End-Stage Renal Disease. Semin. Dial. 2010, 23, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Olmos, F.J. Programa de Ejercicio Mediante Realidad Virtual No-Inmersiva Intradiálisis. Ph.D. Thesis, Universidad de Murcia, Murcia, Spain, 2021. [Google Scholar]
- Lorant, V.; Smith, P.; Van den Broeck, K.; Nicaise, P. Psychological distress associated with the COVID-19 pandemic and suppression measures during the first wave in Belgium. BMC Psychiatry 2021, 21, 112. [Google Scholar] [CrossRef] [PubMed]
- Al Naamani, Z.; Gormley, K.; Noble, H.; Santin, O.; Al Maqbali, M. Fatigue, anxiety, depression and sleep quality in patients undergoing haemodialysis. BMC Nephrol. 2021, 22, 157. [Google Scholar] [CrossRef]
- Abdelghani, M.; Hamed, M.G.; Said, A.; Fouad, E. Evaluation of perceived fears of COVID-19 virus infection and its relationship to health-related quality of life among patients with diabetes mellitus in Egypt during pandemic: A developing country single-center study. Diabetol. Int. 2021, 13, 108–116. [Google Scholar] [CrossRef]
- Sahin, S.; Karsidag, S.; Cinar, N.; Ates, M.F.; Demir, S.; Eren, F.; Neyal, A.; Kisabay Ak, A.; Bora Tokcaer, A.; Erkoc Ataoglu, E.; et al. The Impact of the COVID-19 Lockdown on the Quality of Life in Chronic Neurological Diseases: The Results of a COVQoL-CND Study. Eur. Neurol. 2021, 84, 450–459. [Google Scholar] [CrossRef]
- Biviá-Roig, G.; Blasco-Sanz, R.; Boldó-Roda, A.; Vara, M.; Escrivá-Martínez, T.; Herrero, R.; La Rosa, V.; Baños, R.; Lisón, J. Efficacy of an Internet-Based Intervention to Promote a Healthy Lifestyle on the Reproductive Parameters of Overweight and Obese Women: Study Protocol for a Randomised Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 8312. [Google Scholar] [CrossRef]
- Kennedy, K.E.R.; Grandner, M.A. Sleep, Dreams, and Nightmares During the COVID-19 Pandemic. Am. J. Health Promot. 2021, 35, 1168–1173. [Google Scholar] [CrossRef]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; McDermott, D.; Schuch, F.; Smith, L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc. Med. 2021, 7, e000960. [Google Scholar] [CrossRef] [PubMed]
- De Villar, L.O.P.; García, S.A.; Pérez, M.J.L.; Cuenca, J.J.A.; Gramage, J.; Ortí, E.S. Cuantificación del deterioro funcional durante seis meses en pacientes renales en estadio terminal. Enferm. Nefrol. 2015, 18, 265–271. [Google Scholar] [CrossRef]
- Li, W.; Frydman, J.L.; Li, Y.; Liu, B. Characterizing delayed care among US older adults by self-rated health during the COVID-19 pandemic. Prev. Med. 2022, 164, 107308. [Google Scholar] [CrossRef] [PubMed]
| Variable (n = 27) | Demographics | |
|---|---|---|
| Age (years) | ||
| Mean (SD) | 73.4 | (14.1) |
| Median (1st Q–3rd Q) | 78 | (68.5–82) |
| Sex n (%) | ||
| Male | 17 | (63.0%) |
| Female | 10 | (37.0%) |
| Body Mass Index (kg/m2) | ||
| Mean (SD) | 27.8 | (6.5) |
| Median (1st Q–3rd Q) | 25.3 | (23.7–30.3) |
| Time on HD (years) | ||
| Mean (SD) | 7.0 | (6.0) |
| Median (1st Q–3rd Q) | 4 | (3–9) |
| Charlson’s Comorbidity | ||
| Mean (SD) | 7.8 | (2.4) |
| Median (1st Q–3rd Q) | 8 | (6–9) |
| Diabetes n (%) | ||
| No | 15 | (44.4%) |
| Yes | 12 | (55.6%) |
| Hypertension n (%) | ||
| No | 2 | (7.4%) |
| Yes | 25 | (92.6%) |
| Cardiopathy n (%) | ||
| No | 8 | (29.6%) |
| Yes | 19 | (70.4%) |
| COPD n (%) | ||
| No | 23 | (85.2%) |
| Yes | 4 | (14.8%) |
| Neoplasia n (%) | ||
| No | 21 (77.8%) | 21 (77.8%) |
| Yes | 6 (22.2%) | 6 (22.2%) |
| Blood flow (mL/min) | ||
| Mean (SD) | 364.2 | (36.1) |
| Median (1st Q–3rd Q) | 350 | (344–394) |
| Number of HD (sessions/week) | ||
| 2 | 2 | (7.4%) |
| 3 | 25 | (92.6%) |
| Vascular access | ||
| Arteriovenous fistula | 22 | (81.5%) |
| Central Venous Catheter | 5 | (18.5) |
| Dialysis technique | ||
| HDHF | 17 | (63%) |
| HFOL | 9 | (33.3%) |
| HDLF | 1 | (3.7%) |
| Hemodialysis Session | Pre-Pandemic | Post-Pandemic | ||
| Session duration (minutes) | ||||
| Mean (SD) | 230.2 | (8.6) | 231.2 | (7.2) |
| Median (1st Q–3rd Q) | 232 | (230–233) | 232 | (231–234) |
| Dry weight (Kg) | ||||
| Mean (SD) | 70.3 | (14.6) | 67.6 | (15.2) |
| Median (1st Q–3rd Q) | 68.5 | (59.7–77.1) | 64.5 | (57.4–74.5) |
| KtV sp | ||||
| Mean (SD) | 1.49 | (0.23) | 1.61 | (0.25) |
| Median (1st Q–3rd Q) | 1.50 | (1.31–1.66) | 1.55 | (1.42–1.75) |
| Heart rate (beats per minute) | ||||
| Mean (SD) | 67 | (9) | 68 | (9) |
| Median (1st Q–3rd Q) | 68 | (61–75) | 68 | (63.5–74.5) |
| Systolic blood pressure (mmHg) | ||||
| Mean (SD) | 143 | (16) | 145 | (22) |
| Median (1st Q–3rd Q) | 141 | (135–154) | 147 | (130–162) |
| Diastolic blood pressure (mmHg) | ||||
| Mean (SD) | 60 | (10) | 60 | (11) |
| Median (1st Q–3rd Q) | 59 | (52–67) | 59 | (53–67) |
| Biochemical Characteristics | Pre-Pandemic | Post-Pandemic | ||
| Hemoglobin (g/dL) | ||||
| Mean (SD) | 11.3 | (0.9) | 11.6 | (1.2) |
| Median (1st Q–3rd Q) | 11.2 | (10.8–11.6) | 11.8 | (11.2–12.5) |
| Albumin (g/dL) | ||||
| Mean (SD) | 4.1 | (0.3) | 3.9 | (0.4) |
| Median (min–max) | 4.0 | (3.8–4.2) | 3.9 | (3.8–4.2) |
| Phosphorus (mg/dL) | ||||
| Mean (SD) | 4.3 | (1.7) | 31.3 | (18.6) |
| Median (1st Q–3rd Q) | 4.1 | (3.2–5.4) | 37 | (10–48) |
| Ferritin (ng/mL) | ||||
| Mean (SD) | 525.6 | (312.0) | 539.5 | (291.2) |
| Median (1st Q–3rd Q) | 482 | (313–729.5) | 613 | (297.5–760) |
| PTH intacta (pg/mL) | ||||
| Mean (SD) | 273.8 | (200.9) | 244.2 | (126.3) |
| Median (1st Q–3rd Q) | 266 | (163.5–308.5) | 218 | (178–318) |
| Calcium (mg/dL) | ||||
| Mean (SD) | 9.1 | (0.8) | 8.5 | (0.6) |
| Median (1st Q–3rd Q) | 9.1 | (8.5–9.4) | 8.3 | (8.1–8.9) |
| Phosphorus (mg/dL) | ||||
| Mean (SD) | 4.3 | (1.7) | 31.3 | (18.6) |
| Median (1st Q–3rd Q) | 4.1 | (3.2–5.4) | 37 | (10–48) |
| Health-Related Quality of Life | Pre-Pandemic | Post-Pandemic | ||
| SF-36 Physical Function | ||||
| Mean (SD) | 52.1 | (30.1) | 36.4 | (34.3) |
| Median (1st Q–3rd Q) | 50 | (30–80) | 30 | (5–75) |
| SF-36 Role Physical | ||||
| Mean (SD) | 52.4 | (46.0) | 39.3 | (43.7) |
| Median (1st Q–3rd Q) | 75 | (0–100) | 25 | (0–75) |
| SF-36 Bodily Pain | ||||
| Mean (SD) | 64.8 | (40.8) | 61.4 | (33.3) |
| Median (1st Q–3rd Q) | 100 | (31–100) | 62 | (41–100) |
| SF-36 General Health | ||||
| Mean (SD) | 46.6 | (17.5) | 38.9 | (22.8) |
| Median (1st Q–3rd Q) | 45 | (40–57) | 30 | (30–50) |
| SF-36 Vitality | ||||
| Mean (SD) | 46.7 | (29.7) | 50.2 | (25.1) |
| Median (1st Q–3rd Q) | 50 | (20–65) | 50 | (40–70) |
| SF-36 Social Functioning | ||||
| Mean (SD) | 76.2 | (33.3) | 48.2 | (36.3) |
| Median (1st Q–3rd Q) | 100 | (62.5–100) | 37.5 | (25–87.5) |
| SF-36 Role Emotional | ||||
| Mean (SD) | 76.2 | (41.0) | 57.1 | (42.4) |
| Median (1st Q–3rd Q) | 100 | (66.7–100) | 66.7 | (0–100) |
| SF-36 Mental Health | ||||
| Mean (SD) | 71.0 | (27.0) | 64.8 | (22.7) |
| Median (1st Q–3rd Q) | 80 | (48–92) | 64 | (52–84) |
| SF-36 Physical Component Scale | ||||
| Mean (SD) | 37.5 | (11.1) | 34.0 | (11.6) |
| Median (1st Q–3rd Q) | 35.5 | (29.3–48.2) | 29.9 | (26.3–41.7) |
| SF-36 Mental Component Scale | ||||
| Mean (SD) | 49.1 | (13.3) | 43.8 | (12.3) |
| Median (1st Q–3rd Q) | 52.6 | (40.1–59.5) | 39.6 | (34.5–54.8) |
| Activity Level | Pre-Pandemic | Post-Pandemic | ||
| Average Activity Score | ||||
| Mean (SD) | 46.4 | (26.9) | 32.5 | (27.4) |
| Median (1st Q–3rd Q) | 51 | (28–71) | 28 | (7–52) |
| Maximal Activity Score | ||||
| Mean (SD) | 64.0 | (22.5) | 45.3 | (30.1) |
| Median (1st Q–3rd Q) | 69 | (67–75) | 63 | (12–71) |
| Estimate (CI 95%) | Standard Error | p Value | |
|---|---|---|---|
| SF-36 Physical Function | −15.714 (−24.245, −7.183) | 4.258 | 0.001 |
| SF-36 Role Physical | −13.095 (−37.911, 11.721) | 12.514 | 0.308 |
| SF-36 Bodily Pain | −3.429 (−14.86, 8.003) | 5.705 | 0.555 |
| SF-36 General Health | −7.762 (−15.898, 0.374) | 4.061 | 0.07 |
| SF-36 Vitality | 3.571 (−8.458, 1.812) | 4.501 | 0.437 |
| SF-36 Social Functioning | −27.976 (−42.631, −13.321) | 7.314 | 0.001 |
| SF-36 Role Emotional | −19.047 (−41.42, 3.325) | 11.168 | 0.104 |
| SF-36 Mental Health | −6.238 (−15.082, 2.606) | 4.414 | 0.173 |
| SF-36 Physical Component Scale | −3.569 (−7.083, −0.055) | 1.754 | 0.05 |
| SF-36 Mental Component Scale | −5.37 (−10.816, 0.076) | 2.718 | 0.062 |
| HAP Average Activity Score | −13.905 (−22.282, −5.528) | 4.181 | 0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Segura-Ortí, E.; Martínez-Olmos, F.J.; Ródenas-Pascual, Á.; Guillem-Giménez, E.; Vercher-Narbona, V.; Piñón-Ruiz, M.J.; Garcia-Testal, A. Impact of COVID-19 Pandemic on Health-Related Quality of Life and Physical Activity of Patients in Hemodialysis. Healthcare 2022, 10, 2217. https://doi.org/10.3390/healthcare10112217
Segura-Ortí E, Martínez-Olmos FJ, Ródenas-Pascual Á, Guillem-Giménez E, Vercher-Narbona V, Piñón-Ruiz MJ, Garcia-Testal A. Impact of COVID-19 Pandemic on Health-Related Quality of Life and Physical Activity of Patients in Hemodialysis. Healthcare. 2022; 10(11):2217. https://doi.org/10.3390/healthcare10112217
Chicago/Turabian StyleSegura-Ortí, Eva, Francisco J. Martínez-Olmos, Álvaro Ródenas-Pascual, Edgar Guillem-Giménez, Verónica Vercher-Narbona, Martha Jocelyne Piñón-Ruiz, and Alicia Garcia-Testal. 2022. "Impact of COVID-19 Pandemic on Health-Related Quality of Life and Physical Activity of Patients in Hemodialysis" Healthcare 10, no. 11: 2217. https://doi.org/10.3390/healthcare10112217
APA StyleSegura-Ortí, E., Martínez-Olmos, F. J., Ródenas-Pascual, Á., Guillem-Giménez, E., Vercher-Narbona, V., Piñón-Ruiz, M. J., & Garcia-Testal, A. (2022). Impact of COVID-19 Pandemic on Health-Related Quality of Life and Physical Activity of Patients in Hemodialysis. Healthcare, 10(11), 2217. https://doi.org/10.3390/healthcare10112217






