Trends in Hospital Admissions for Mental, Behavioural and Neurodevelopmental Disorders in England and Wales between 1999 and 2019: An Ecological Study
Abstract
1. Introduction
2. Methods
2.1. Data Sources and Study Population
2.2. Data Analysis
3. Results
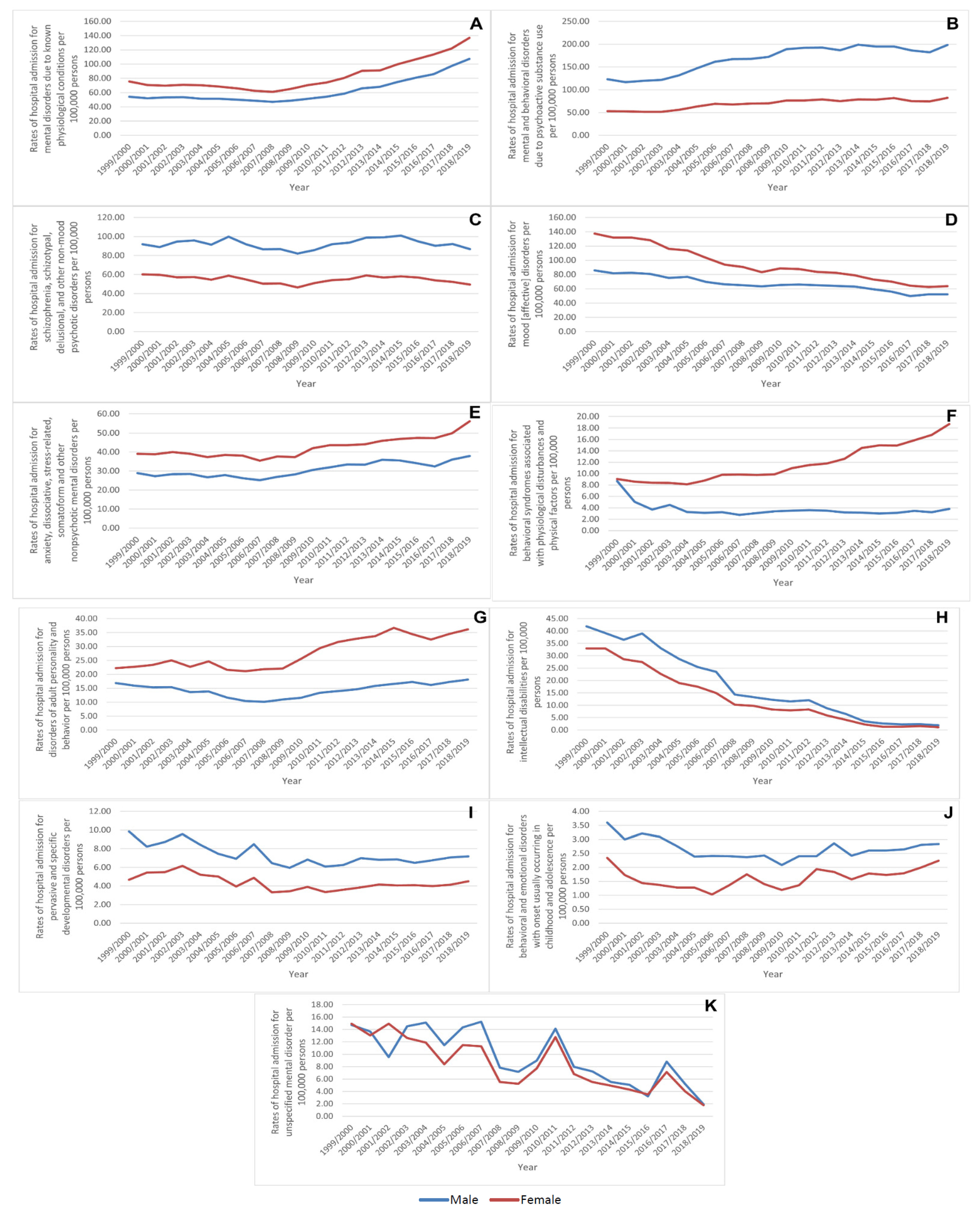
3.1. Mental, Behavioural and Neurodevelopmental Disorders Admission Rate by Gender
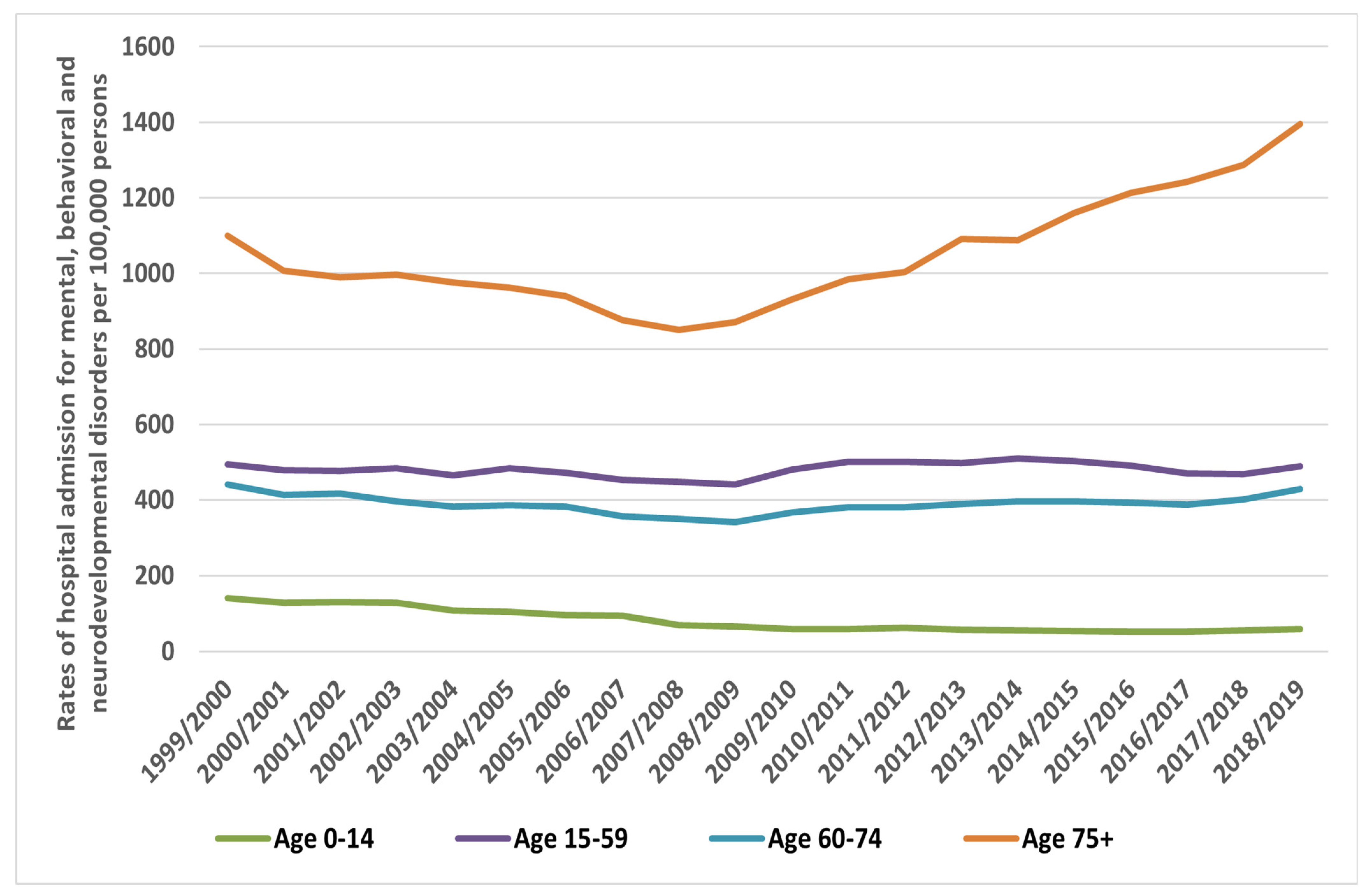
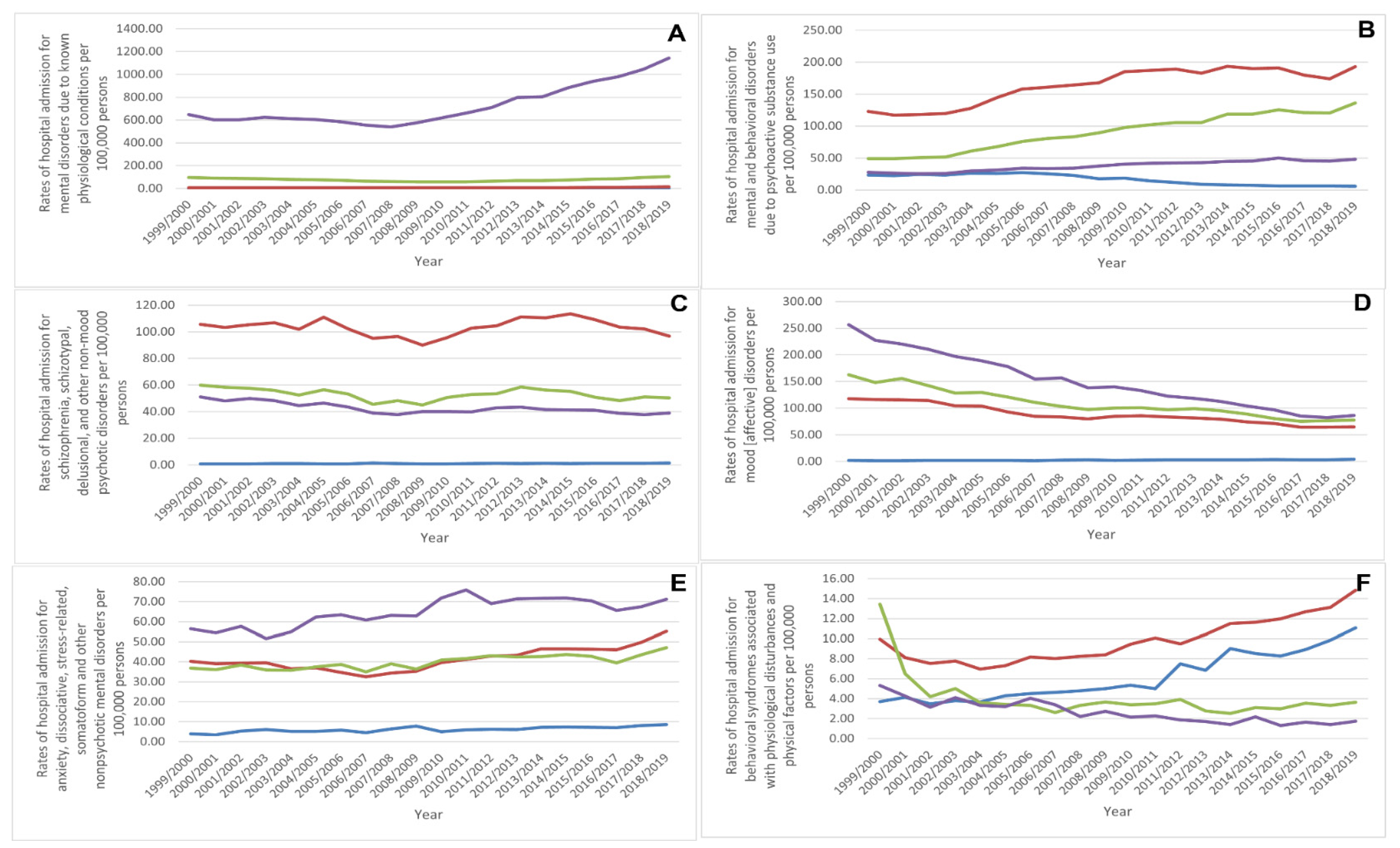
3.2. Mental, Behavioural and Neurodevelopmental Disorders Hospital Admission Rate by Age Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mental Health Foundation. Fundamental Facts About Mental Health 2016. Available online: https://www.mentalhealth.org.uk/explore-mental-health/publications/fundamental-facts-about-mental-health-2016 (accessed on 22 July 2022).
- Mental Health Foundation. UK and Worldwide: Mental Health Statistics. Available online: https://www.mentalhealth.org.uk/explore-mental-health/statistics/uk-worldwide-statistics (accessed on 22 July 2022).
- Leach, M.J.; Jones, M.; Bressington, D.; Jones, A.; Nolan, F.; Muyambi, K.; Gillam, M.; Gray, R. The association between community mental health nursing and hospital admissions for people with serious mental illness: A systematic review. Syst. Rev. 2020, 9, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Vigo, D.; Thornicroft, G.; Atun, R. Estimating the true global burden of mental illness. Lancet Psychiatry 2016, 3, 171–178. [Google Scholar] [CrossRef]
- Heslin, K.C.; Elixhauser, A.; Steiner, C.A. Hospitalizations Involving Mental and Substance Use Disorders among Adults, 2012. In Healthcare Cost and Utilization Project (hcup) Statistical Briefs; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2015. [Google Scholar]
- McDermott, K.W.; Elixhauser, A.; Sun, R. Trends in Hospital Inpatient Stays in the United States, 2005–2014; Healthcare Cost and Utilization Project; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2017; pp. 1–18.
- HM Government. No Health Without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages; Department of Health and Social Care: London, UK, 2011; pp. 1–103.
- Al-Daghastani, T.; Naser, A.Y. Hospital admission profile related to poisoning by, adverse effect of and underdosing of psychotropic drugs in england and wales: An ecological study. Saudi Pharm. J. 2022, 30, 1262–1272. [Google Scholar] [CrossRef]
- Alrawashdeh, H.M.; Naser, A.Y.; Alwafi, H.; AbuAlhommos, A.K.; Jalal, Z.; Paudyal, V.; Abdulmannan, D.M.; Hassanin, F.F.; Hemmo, S.I.; Sarireh, F.A. Trends in hospital admission due to diseases of the eye and adnexa in the past two decades in england and wales: An ecological study. Int. J. Gen. Med. 2022, 15, 1097–1110. [Google Scholar] [CrossRef] [PubMed]
- Al-shehri, H.; Dahmash, D.T.; Rochow, N.; Alturki, B.; Alrajhi, D.; Alayed, F.; Alhazani, F.; Alsuhibany, H.; Naser, A.Y. Hospital admission profile of neonates for conditions originating in the perinatal period in england and wales between 1999–2020: An ecological study. Int. J. Gen. Med. 2022, 15, 1973–1984. [Google Scholar] [CrossRef]
- Hemmo, S.I.; Naser, A.Y.; Alwafi, H.; Mansour, M.M.; Alanazi, A.F.R.; Jalal, Z.; Alsairafi, Z.K.; Paudyal, V.; Alomari, E.; Al-Momani, H.; et al. Hospital admissions due to ischemic heart diseases and prescriptions of cardiovascular diseases medications in england and wales in the past two decades. Int. J. Environ. Res. Public Health 2021, 18, 7041. [Google Scholar] [CrossRef]
- Naser, A.Y.; Alrawashdeh, H.M.; Alwafi, H.; AbuAlhommos, A.K.; Jalal, Z.; Paudyal, V.; Alsairafi, Z.K.; Salawati, E.M.; Samannodi, M.; Sweiss, K.; et al. Hospital admission trends due to viral infections characterised by skin and mucous membrane lesions in the past two decades in england and wales: An ecological study. Int. J. Environ. Res. Public Health 2021, 18, 11649. [Google Scholar] [CrossRef]
- Naser, A.Y.; Alwafi, H.; Hemmo, S.I.; Alrawashdeh, H.M.; Alqahtani, J.S.; Alghamdi, S.M.; Ali, M.K.M. Trends in hospital admissions due to neoplasms in england and wales between 1999 and 2019: An ecological study. Int. J. Environ. Res. Public Health 2022, 19, 8054. [Google Scholar] [CrossRef]
- Naser, A.Y.; Mansour, M.M.; Alanazi, A.F.R.; Sabha, O.; Alwafi, H.; Jalal, Z.; Paudyal, V.; Dairi, M.S.; Salawati, E.M.; Alqahtan, J.S.; et al. Hospital admission trends due to respiratory diseases in england and wales between 1999 and 2019: An ecologic study. BMC Pulm. Med. 2021, 21, 356. [Google Scholar] [CrossRef]
- Naser, A.Y.; Wang, Q.; Wong, L.Y.L.; Ilomaki, J.; Bell, J.S.; Fang, G.; Wong, I.C.K.; Wei, L. Hospital admissions due to dysglycaemia and prescriptions of antidiabetic medications in england and wales: An ecological study. Diabetes Ther. 2018, 9, 153–163. [Google Scholar] [CrossRef]
- Sweiss, K.; Naser, A.Y.; Alrawashdeh, H.M.; Alharazneh, A. Hospital admissions due to vasomotor and allergic rhinitis in england and wales between 1999 and 2019: An ecological study. Ir. J. Med. Sci. 2022, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Sweiss, K.; Naser, A.Y.; Samannodi, M.; Alwafi, H. Hospital admissions due to infectious and parasitic diseases in england and wales between 1999 and 2019: An ecological study. BMC Infect. Dis. 2022, 22, 398. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.M.; Naser, A.; AbuAlhommos, A.K.; Al-Daghastani, T.; Alrawashdeh, H.M.; Ali, S.M.; Alwafi, H.; Alqurashi, M.; Ahmed, A.B.; Albarqi, H. Hospital admissions secondary to diseases of the blood, blood-forming organs, and immune system in england and wales. Cureus 2022, 14, 1–10. [Google Scholar]
- Naser, A.Y.; Dahmash, E.Z.; Al-Daghastani, T.; Alwafi, H.; Hamdah, S.A.; Alsairafi, Z.K.; Alsaleh, F.M. An ecological analysis of hospitalization patterns for diseases of the nervous system in england and wales over the last 20 years. Healthcare 2022, 10, 1670. [Google Scholar] [CrossRef]
- Health and Social Care Information Centre (HSCIC). Hospital Episode Statistics. Available online: http://content.digital.nhs.uk/hes (accessed on 13 January 2021).
- NHS Wales Informatics Service. Annual Pedw Data Tables. Available online: http://www.infoandstats.wales.nhs.uk/page.cfm?pid=41010&orgid=869 (accessed on 13 January 2021).
- ICD10 Codes. Icd-10-Cm Codes. Available online: https://www.aapc.com/codes/icd-10-codes-range/ (accessed on 22 July 2022).
- Office for National Statistics (ONS). Population Estimates. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland (accessed on 13 January 2021).
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the global burden of disease study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef]
- Whiteford, H.A.; Degenhardt, L.; Rehm, J.; Baxter, A.J.; Ferrari, A.J.; Erskine, H.E.; Charlson, F.J.; Norman, R.E.; Flaxman, A.D.; Johns, N.; et al. Global burden of disease attributable to mental and substance use disorders: Findings from the global burden of disease study 2010. Lancet 2013, 382, 1575–1586. [Google Scholar] [CrossRef]
- Fløvig, J.C.; Vaaler, A.E.; Morken, G. Substance use at admission to an acute psychiatric department. Nord. J. Psychiatry 2009, 63, 113–119. [Google Scholar] [CrossRef]
- Hayes, R.D.; Chang, C.K.; Fernandes, A.; Broadbent, M.; Lee, W.; Hotopf, M.; Stewart, R. Associations between substance use disorder sub-groups, life expectancy and all-cause mortality in a large british specialist mental healthcare service. Drug Alcohol Depend. 2011, 118, 56–61. [Google Scholar] [CrossRef]
- Rani, F.; Murray, M.L.; Byrne, P.J.; Wong, I.C. Epidemiologic features of antipsychotic prescribing to children and adolescents in primary care in the united kingdom. Pediatrics 2008, 121, 1002–1009. [Google Scholar] [CrossRef]
- Naser, A.Y.; Alwafi, H.; Al-Daghastani, T.; Hemmo, S.I.; Alrawashdeh, H.M.; Jalal, Z.; Paudyal, V.; Alyamani, N.; Almaghrabi, M.; Shamieh, A. Drugs utilization profile in england and wales in the past 15 years: A secular trend analysis. BMC Prim. Care 2022, 23, 239. [Google Scholar] [CrossRef]
- Kariisa, M.; Scholl, L.; Wilson, N.; Seth, P.; Hoots, B. Drug overdose deaths involving cocaine and psychostimulants with abuse potential-united states, 2003–2017. MMWR. Morb. Mortal. Wkly. Rep. 2019, 68, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Susło, R.; Hanczyc, P.; Drobnik, J. Review of changes in amount of hospitalizations related to poisoning by chosen psychotropic drugs (t43 icd-10) in lower silesia region of poland in years 2006–2012. ARC J. Anesthesiol. 2016, 1, 25–32. [Google Scholar]
- Reith, D.M.; Edmonds, L. Assessing the role of drugs in suicidal ideation and suicidality. CNS Drugs 2007, 21, 463–472. [Google Scholar] [CrossRef]
- Kessing, L.V.; Hansen, M.G.; Andersen, P.K. Course of illness in depressive and bipolar disorders. Naturalistic study, 1994–1999. Br. J. Psychiatry 2004, 185, 372–377. [Google Scholar] [CrossRef]
- Joas, E.; Karanti, A.; Song, J.; Goodwin, G.M.; Lichtenstein, P.; Landén, M. Pharmacological treatment and risk of psychiatric hospital admission in bipolar disorder. Br. J. Psychiatry J. 2017, 210, 197–202. [Google Scholar] [CrossRef]
- Riecher-Rössler, A. Sex and gender differences in mental disorders. The lancet. Psychiatry 2017, 4, 8–9. [Google Scholar] [PubMed]
- Thompson, A.; Shaw, M.; Harrison, G.; Ho, D.; Gunnell, D.; Verne, J. Patterns of hospital admission for adult psychiatric illness in england: Analysis of hospital episode statistics data. Br. J. Psychiatry 2004, 185, 334–341. [Google Scholar] [CrossRef]
- Boyd, A.; de Velde, S.V.; Vilagut, G.; de Graaf, R.; O’Neill, S.; Florescu, S.; Alonso, J.; Kovess-Masfety, V.; EU-WMH Investigators. Gender differences in mental disorders and suicidality in europe: Results from a large cross-sectional population-based study. J. Affect. Disord. 2015, 173, 245–254. [Google Scholar] [CrossRef]
- Riecher-Rössler, A. Prospects for the classification of mental disorders in women. Eur. Psychiatry 2010, 25, 189–196. [Google Scholar] [CrossRef]
- Hall, A.; Hay, P.J. Eating disorder patient referrals from a population region 1977–1986. Psychol. Med. 1991, 21, 697–701. [Google Scholar] [CrossRef]
- Hay, P.J.; Bacaltchuk, J. Extracts from “clinical evidence”: Bulimia nervosa. BMJ (Clin. Res. Ed.) 2001, 323, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Low, L.F.; Draper, B. Hospitalization patterns for psychiatric disorders across the lifespan in australia from july 1998 to june 2005. Psychiatr. Serv. 2009, 60, 113–116. [Google Scholar] [CrossRef] [PubMed]
- National Health Services. Hospital Admissions for Drug-Related Mental and Behavioural Disorders Fall by 12 Per Cent in a Year. Available online: https://digital.nhs.uk/news-and-events/latest-news/hospital-admissions-for-drug-related-mental-and-behavioural-disorders-fall-by-12-per-cent-in-a-year (accessed on 22 July 2022).
- Bardach, N.S.; Coker, T.R.; Zima, B.T.; Murphy, J.M.; Knapp, P.; Richardson, L.P.; Edwall, G.; Mangione-Smith, R. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics 2014, 133, 602–609. [Google Scholar] [CrossRef] [PubMed]
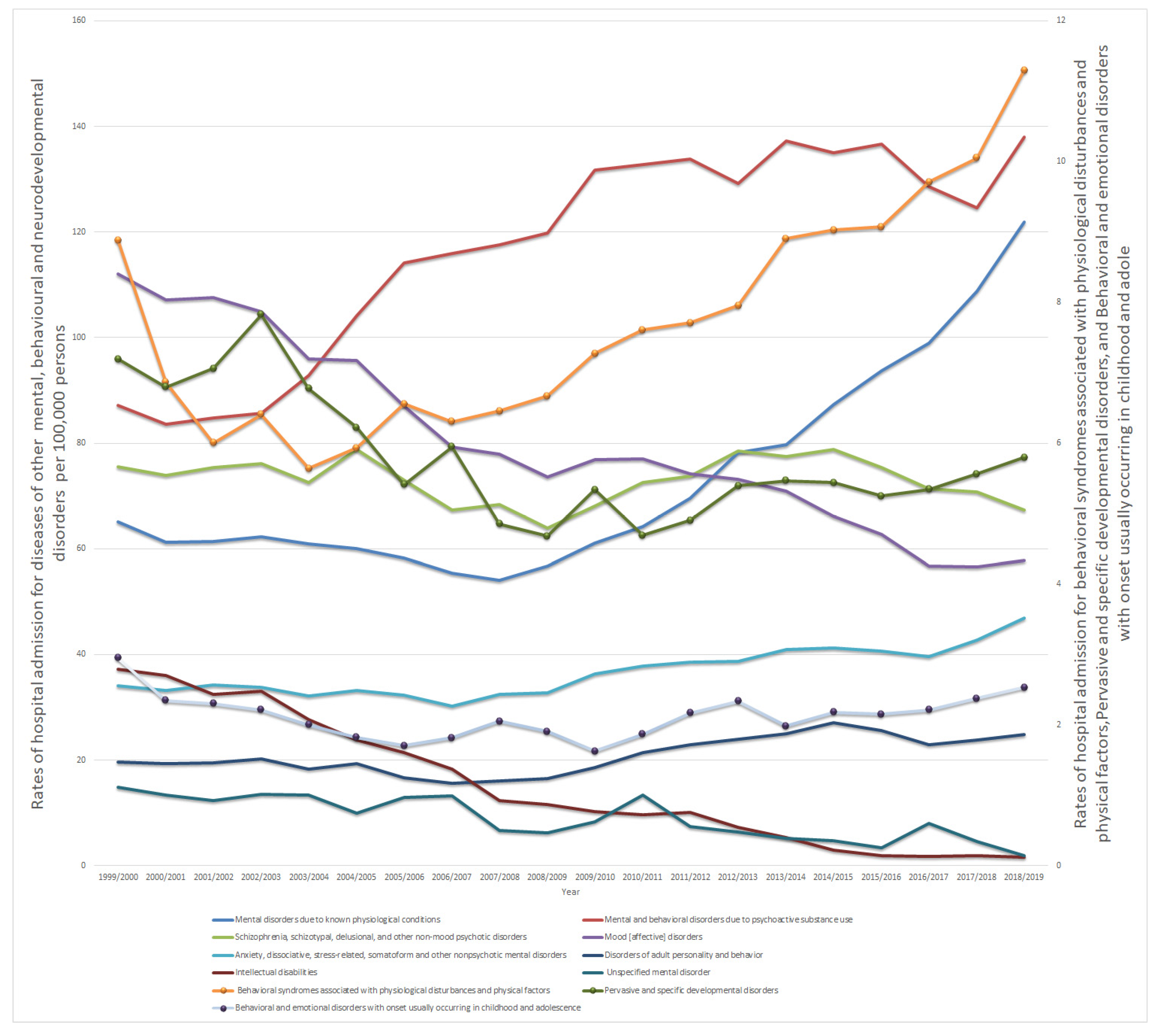


| ICD10 Code | Description | Percentage from Total Number of Admissions |
|---|---|---|
| F01–F09 | Mental disorders due to known physiological conditions | 16.7% |
| F10–F19 | Mental and behavioral disorders due to psychoactive substance use | 26.6% |
| F20–F29 | Schizophrenia, schizotypal, delusional, and other non-mood psychotic disorders | 16.5% |
| F30–F39 | Mood [affective] disorders | 18.1% |
| F40–F48 | Anxiety, dissociative, stress-related, somatoform and other nonpsychotic mental disorders | 8.3% |
| F50–F59 | Behavioral syndromes associated with physiological disturbances and physical factors | 1.8% |
| F60–F69 | Disorders of adult personality and behavior | 4.8% |
| F70–F79 | Intellectual disabilities | 3.4% |
| F80–F89 | Pervasive and specific developmental disorders | 1.3% |
| F90–F98 | Behavioral and emotional disorders with onset usually occurring in childhood and adolescence | 0.5% |
| F99–F99 | Unspecified mental disorder | 2.0% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naser, A.Y.; Dahmash, E.Z.; Alqahtani, J.S.; Alsairafi, Z.K.; Alsaleh, F.M.; Alwafi, H. Trends in Hospital Admissions for Mental, Behavioural and Neurodevelopmental Disorders in England and Wales between 1999 and 2019: An Ecological Study. Healthcare 2022, 10, 2191. https://doi.org/10.3390/healthcare10112191
Naser AY, Dahmash EZ, Alqahtani JS, Alsairafi ZK, Alsaleh FM, Alwafi H. Trends in Hospital Admissions for Mental, Behavioural and Neurodevelopmental Disorders in England and Wales between 1999 and 2019: An Ecological Study. Healthcare. 2022; 10(11):2191. https://doi.org/10.3390/healthcare10112191
Chicago/Turabian StyleNaser, Abdallah Y., Eman Zmaily Dahmash, Jaber S. Alqahtani, Zahra K. Alsairafi, Fatemah M. Alsaleh, and Hassan Alwafi. 2022. "Trends in Hospital Admissions for Mental, Behavioural and Neurodevelopmental Disorders in England and Wales between 1999 and 2019: An Ecological Study" Healthcare 10, no. 11: 2191. https://doi.org/10.3390/healthcare10112191
APA StyleNaser, A. Y., Dahmash, E. Z., Alqahtani, J. S., Alsairafi, Z. K., Alsaleh, F. M., & Alwafi, H. (2022). Trends in Hospital Admissions for Mental, Behavioural and Neurodevelopmental Disorders in England and Wales between 1999 and 2019: An Ecological Study. Healthcare, 10(11), 2191. https://doi.org/10.3390/healthcare10112191








