Impacts of Internet Use on Chinese Patients’ Trust-Related Primary Healthcare Utilization
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection
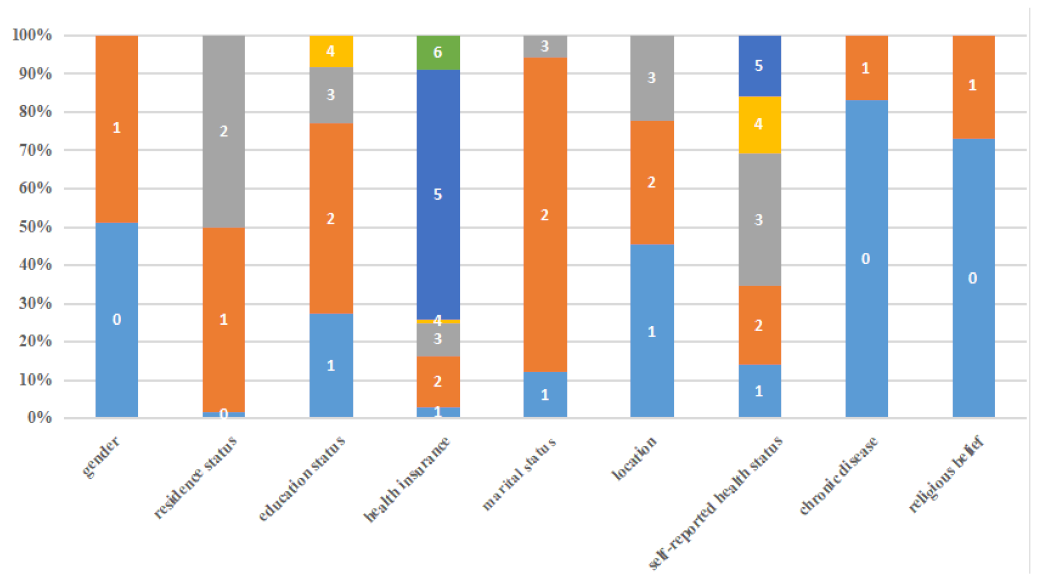
Variables
2.2. Statistical Analysis and Methodology
3. Results
3.1. The Impact of Patients’ Trust in Physicians and Internet Use
- (1)
- Other variables defined in Table 1 are also controlled, but not reported, in all specifications, * is interactive effect of patients’ trust in physicians and internet use on primary healthcare-seeking.
- (2)
- *** p < 0.01; ** p < 0.05; * p < 0.10.
| Primary Healthcare Seeking | dy/dx | Delta-Method Std. Err. | t | p | ||
|---|---|---|---|---|---|---|
| Internet use | 0.570 | |||||
| Patients’ trust in physicians | 0.0009 | |||||
| Patients’ trust in physicians | 1 | −0.002 (−0.003~−0.002) | 0.0002 | −14.86 | 0 | |
| 2 | −0.001 (−0.002~−0.0010) | 0.0002 | −7.5 | 0 | ||
| 3 | −0.0004 (−0.0008~0.00002) | 0.0002 | −1.84 | 0.04 | ||
| 4 | 0.0006 (0.00007~0.001) | 0.0002 | 2.25 | 0.024 | ||
| 5 | 0.001 (0.0009~0.001) | 0.0003 | 5.22 | 0 | ||
| 6 | 0.002 (0.002~0.003) | 0.0003 | 7.41 | 0 | ||
| 7 | 0.003 (0.003~0.004) | 0.0004 | 9.07 | 0 | ||
| 8 | 0.004 (0.004~0.005) | 0.0004 | 10.37 | 0 | ||
| 9 | 0.005 (0.004~0.006) | 0.0005 | 11.4 | 0 | ||
| 10 | 0.006 (0.005~0.007) | 0.0005 | 12.24 | 0 | ||
3.2. Effects of Urbanization, Aging, and Level of Primary Healthcare Service on Primary Healthcare Seeking
3.3. Robustness Checks
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, H.; Gusmano, M.K.; Cao, Q. An evaluation of the policy on community health organizations in China: Will the priority of new healthcare reform in China be a success? Health Policy 2011, 99, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Lu, J.; Hu, S.; Cheng, K.K.; De Maeseneer, J.; Meng, Q.; Mossialos, E.; Xu, D.R.; Yip, W.; Zhang, H.; et al. The primary health-care system in China. Lancet 2017, 390, 2584–2594. [Google Scholar] [CrossRef]
- Li, X.; Krumholz, H.M.; Yip, W.; Cheng, K.K.; De Maeseneer, J.; Meng, Q.; Mossialos, E.; Li, C.; Lu, J.; Su, M.; et al. Quality of primary health care in China: Challenges and recommendations. Lancet 2020, 395, 1802–1812. [Google Scholar] [CrossRef]
- Papp, R.; Borbas, I.; Dobos, E.; Bredehorst, M.; Jaruseviciene, L.; Vehko, T.; Balogh, S. Perceptions of quality in primary health care: Perspectives of patients and professionals based on focus group discussions. BMC Fam. Pract. 2014, 128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lori, J.R.; Rominski, S.D.; Perosky, J.E.; Munro, M.L.; Williams, G.; Bell, S.A.; Nyanplu, A.B.; Amarah, P.N.M.; Boyd, C.J. A case series study on the effect of Ebola on facility-based deliveries in rural Liberia. BMC Pregnancy Childbirth 2015, 15, 254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ajzen, I. The theory of planned behaviour: Reactions and reflections. Psychol Health 2011, 26, 1113–1127. [Google Scholar] [CrossRef]
- Dhagarra, D.; Goswami, M.; Kumar, G. Impact of Trust and Privacy Concerns on Technology Acceptance in Healthcare: An Indian Perspective. Int. J. Med. Inform. 2020, 141, 104164. [Google Scholar] [CrossRef]
- Pellegrini, C.A. Trust: The keystone of the patient-physician relationship. J. Am. Coll. Surg. 2017, 224, 95–102. [Google Scholar] [CrossRef]
- Mollering, G. Trust: Reason, Routine, Reflexivity; Emerald Group Publishing: Bradford, UK, 2006. [Google Scholar]
- Sousa-Duarte, F.; Brown, P.; Mendes, A.M. Healthcare professionals’ trust in patients: A review of the empirical and theoretical literatures. Sociol. Compass 2020, 14, e12828. [Google Scholar] [CrossRef]
- Schwei, R.J.; Kadunc, K.; Nguyen, A.L.; Jacobs, E.A. Impact of sociodemographic factors and previous interactions with the health care system on institutional trust in three racial/ethnic groups. Patient Educ. Couns. 2014, 96, 333–338. [Google Scholar] [CrossRef]
- Doty, A.M.B.; Powell, R.E.; Carr, B.G.; Nelson, D.B.; Rising, K.L. Identification of Approaches to Improve Patient Trust in Health Systems: A Group Concept Mapping Study. J. Healthc. Manag. 2018, 63, e116–e129. [Google Scholar] [CrossRef] [PubMed]
- Gur, A. Customer trust and perceived service quality in the healthcare sector: Customer aggressive behaviour as a mediator. J. Trust. Res. 2020, 10, 113–133. [Google Scholar] [CrossRef]
- Qadri, Y.A.; Nauman, A.; Zikria, Y.B.; Vasilakos, A.V.; Kim, S.W. The future of healthcare internet of things: A survey of emerging technologies. IEEE Commun. Surv. Tutor. 2020, 22, 1121–1167. [Google Scholar] [CrossRef]
- Sun, M.; Rasooly, A.; Fan, X.; Jian, W. Assessing the quality of primary healthcare for diabetes in China: Multivariate analysis using the China Health and Retirement Longitudinal Study (CHARLS) Database. BMJ Open 2020, 10, e035192. [Google Scholar] [CrossRef]
- Chua, R.Y.J.; Morris, I.M.W. From the head and the heart: Locating cognition- and affect-based trust in managers professional networks. Acad. Manag. J. 2008, 51, 436–452. [Google Scholar] [CrossRef] [Green Version]
- Skirbekk, H.; Middelthon, A.L.; Hjortdahl, P.; Finset, A. Mandates of trust in the physician-patient relationship. Qual. Health Res. 2011, 21, 1182–1190. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Yang, H.; He, J.; Lu, X.; Zhang, R. The Impact of Treatment-Related Internet Health Information Seeking on Patient Compliance. Telemedline e-Health 2020, 27, 513–524. [Google Scholar] [CrossRef] [PubMed]
- Silva, B.M.; Rodrigues, J.J.; de la Torre Díez, I.; López-Coronado, M.; Saleem, K. Mobile-health: A review of current state in 2015. J. Biomed. Inform. 2015, 56, 265–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rider, T.; Malik, M.; Chevassut, T. Haematology patients and the internet–The use of on-line health information and the impact on the patient–physician relationship. Patient Educ. Couns. 2014, 97, 223–238. [Google Scholar] [CrossRef]
- Ma, Q.; Sun, D.; Cui, F.; Zhai, Y.; Zhao, J.; He, X.; Shi, J.; Gao, J.; Li, M.; Zhang, W. Impact of the Internet on Medical Decisions of Chinese Adults: Longitudinal Data Analysis. J. Med. Internet Res. 2020, 22, e18481. [Google Scholar] [CrossRef]
- Marcinkiewicz, M.; Mahboobi, H. Impact of the Internet on the physician-patient relationship. Australas. Med. J. 2009, 1, 102–104. [Google Scholar]
- Lu, X.; Zhang, R.; Wu, W.; Shang, X.; Liu, M. Relationship between Internet health information and patient compliance based on trust: An empirical study. Med. Internet Res. 2018, 20, e253. [Google Scholar] [CrossRef] [PubMed]
- Bell, R.A.; Hu, X.; Orrange, S.E.; Kravitz, R.L. Lingering questions and doubts: Online information-seeking of support forum members following their medical visits. Patient Educ. Couns. 2011, 85, 525–528. [Google Scholar] [CrossRef] [PubMed]
- Spronk, S.; Stoopendaal, A.; Robben, P. An empirical study of how the Dutch healthcare regulator first formulates the concept of trust and then puts it into practice. BMC Health Serv. Res. 2019, 19, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Carter, M.A. Trust, power and vulnerability: A discourse on helping in nursing. Nurs. Clin. North Am. 2009, 44, 393–405. [Google Scholar] [CrossRef] [PubMed]
- Whetten, K.; Leserman, J.; Whetten, R.; Ostermann, J.; Thielman, N.; Swartz, M.; Stangl, D. Exploring lack of trust in care providers and the government as a barrier to health service use. Am. J. Public Health 2006, 96, 716–721. [Google Scholar] [CrossRef] [PubMed]
- Gilson, L. Trust in health care: Theoretical perspectives and research needs. J. Health Organ. Manag. 2006, 20, 359–375. [Google Scholar] [CrossRef]
- Wang, W.; Maitland, E.; Nicholas, S.; Haggerty, J. Determinants of Overall Satisfaction with Public Clinics in Rural China: Interpersonal Care Quality and Treatment Outcome. Int. J. Environ. Res. Public Health 2019, 16, 697. [Google Scholar] [CrossRef] [Green Version]
- Xie, Y.; Hu, J. An Introduction to the China Family Panel Studies (CFPS). Chin. Sociol. Rev. 2014, 47, 3–29. [Google Scholar] [CrossRef]
- Murray, B.; McCrone, S. An integrative review of promoting trust in the patient–primary care provider relationship. J. Adv. Nurs. 2015, 71, 3–23. [Google Scholar] [CrossRef]
- Zhou, Z.; Zhao, Y.; Shen, C.; Lai, S.; Nawaz, R.; Gao, J. Evaluating the effect of hierarchical medical system on health seeking behavior: A difference-in-differences analysis in China. Soc. Sci. Med. 2022, 268, 113372. [Google Scholar] [CrossRef] [PubMed]
- Calnan, M.; Rowe, R. Trust Matters in Healthcare; Open University Press, McGraw Hill Publication: London, UK, 2008. [Google Scholar]
- Honavar S, G. Patient–physician relationship–Communication is the key. Indian J. Ophthalmol, 2018; 66, 1527. [Google Scholar] [CrossRef]
- Baroudi, M.; Goicolea, I.; Hurtig, A.-K.; San-Sebastian, M. Social factors associated with trust in the health system in northern Sweden: A cross-sectional study. BMC Public Health 2022, 22, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Zeng, Y.; Zhang, Z.; Fu, C. The Impact of Internet Use on Health Outcomes of Rural Adults: Evidence from China. Int. J. Environ. Res. Public Health 2020, 17, 6502. [Google Scholar] [CrossRef] [PubMed]
- MassonIda, C.L.; Chen, I.Q.; Levine, J.A.; Shopshire, M.S.; Sorensen, J.L. Health-related internet use among opioid treatment patients. Addict. Behav. Rep. 2019, 9, 100157. [Google Scholar] [CrossRef]
- Kim, Y.Y.; Bae, J.; Lee, J.S. Effects of patients’ motives in choosing a provider on determining the type of medical institution. Patient Prefer. Adherence 2017, 11, 1933–1938. [Google Scholar] [CrossRef] [Green Version]
- Li, X.; Zhang, L.; Li, Z.; Tang, W. Patient Choice and Willingness Toward Gatekeepers as First-Contact Medical Institutions in Chinese Tiered Healthcare Delivery System: A Cross-Sectional Study. Front. Public Health. 2021, 9, 665282. [Google Scholar] [CrossRef]
- Wang, X.; Yang, H.; Duan, Z.; Pan, J. Spatial accessibility of primary health care in China: A case study in Sichuan Province. Soc. Sci. Med. 2018, 209, 14–24. [Google Scholar] [CrossRef]
- Song, H.; Zuo, X.; Cui, C.; Meng, K. The willingness of patients to make the first visit to primary care institutions and its influencing factors in Beijing medical alliances: A comparative study of Beijing’s medical resource-rich and scarce regions. BMC Health Serv. Res. 2019, 1. [Google Scholar] [CrossRef] [Green Version]
- Jahanshahloo, G.R.; Lotfi, F.H.; Izadikhah, M. An algorithmic method to extend TOPSIS for decision-making problems with interval data. Appl. Math. Comput. 2006, 175, 1375–1384. [Google Scholar] [CrossRef]
- Chamodrakas, I.; Leftheriotis, I.; Martakos, D. In-depth analysis and simulation study of an innovative fuzzy approach for ranking alternatives in multiple attribute decision making problems based on TOPSIS. Appl. Soft Comput. 2011, 11, 900–907. [Google Scholar] [CrossRef]
- Zhang, J.; Cheng, M.; Yu, Z. The service level of primary medical and health institutions in Shandong Province was evaluated based on TOPSIS method and RSR method. China Health Stat. 2019, 36, 277–279. [Google Scholar]
- Gbur, E.E.; Stroup, W.W.; McCarter, K.S.; Durham, S.; Young, L.J.; Christman, M.; West, M.; Kramer, M. Analysis of Generalized Linear Mixed Models in the Agricultural and Natural Resources Sciences; John Wiley & Sons: Hoboken, NJ, USA, 2020. [Google Scholar]
- Chen, H.; Liu, Y.; Li, Z.; Xue, D. Urbanization, economic development and health: Evidence from China’s labor-force dynamic survey. Int. J. Equity Health 2017, 16, 207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cropanzano, R.; Mitchell, M.S. Social exchange theory: An interdisciplinary review. J. Manag. 2005, 31, 874–900. [Google Scholar] [CrossRef] [Green Version]
- Hampshire, K.; Hamill, H.; Mariwah, S.; Mwanga, J.; Amoako-Ksakyi, D. The application of Signalling Theory to health-related trust problems: The example of herbal clinics in Ghana and Tanzania. Soc. Sci. Med. 2017, 188, 109–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, Y.; Ng, C.; Ghazalie, S.A.M.; Ngiam, J.; Tai, B.; Lim, M.; Hughes, K. Public Trust in Primary Care Physicians, the Medical Profession and the Healthcare System among Redhill Residents in Singapore. Ann. Acad. Med. 2007, 36, 655–661. [Google Scholar]
- Arnett, M.J.; Thorpe, R.J., Jr.; Gaskin, D.J.; Bowie, J.V.; LaVeist, T.A. Race, Medical Mistrust, and Segregation in Primary Care as Usual Source of Care: Findings from the Exploring Health Disparities in Integrated Communities Study. J. Urban Health Bull. N. Y. Acad. Med. 2016, 93, 456–467. [Google Scholar] [CrossRef] [Green Version]
- Rasiah, S.; Jaafar, S.; Yusof, S.; Ponnudurai, G.; Chung, K.P.Y.; Amirthalingam, S.D. A study of the nature and level of trust between patients and healthcare providers, its dimensions and determinants: A scoping review protocol. BMJ Open 2020, 10, e028061. [Google Scholar] [CrossRef] [Green Version]
- Wong, S.T.; Black, C.; Cutler, F.; Brooke, R.; Haggerty, J.L.; Levesque, J.F. Patient-reported confidence in primary healthcare: Are there disparities by ethnicity or language? BMJ Open 2014, 4, e003884. [Google Scholar] [CrossRef] [Green Version]
- Topp, S.M.; Chipukuma, J.M. How did rapid scale-up of HIV services impact on workplace and interpersonal trust in Zambian primary health centres: A case-based health systems analysis. BMJ Glob. Health 2016, 1, e000179. [Google Scholar] [CrossRef] [Green Version]
- Delmar, C. The excesses of care: A matter of understanding the asymmetry of power. Nurs. Philos. 2012, 13, 236–243. [Google Scholar] [CrossRef]
- Salsin, D.; Notelaers, G. The effect of exposure to bullying on turnover intentions: The role of perceived psychological contract violation and benevolent behaviour. Work Stress 2017, 31, 355–374. [Google Scholar] [CrossRef] [Green Version]
- Samal, L.; Saha, S.; Chander, G.; Korthuis, P.T.; Sharma, R.K.; Sharp, V.; Cohn, J.; Moore, R.D.; Beach, M.C. Internet health information seeking behavior and antiretroviral adherence in persons living with HIV/AIDS. AIDS Patient Care STDs. 2011, 25, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Thom, D.H.; Hessler, D.; Willard-Grace, R.; Bodenheimer, T.; Najmabadi, A.; Araujo, C.; Chen, E.H. Does health coaching change patients’ trust in their primary care provider? Patient Educ. Couns. 2014, 96, 135–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walther, J.B. Social Information Processing Theory. Engaging Theories in Interpersonal Communication: Multiple Perspectives; Routledge: Abingdon, OX, USA, 2008; p. 391. [Google Scholar]
- Joyce, G.K.; Shaw, A.; Murnane, L. Internet Usage within Healthcare: How College Students Use the Internet to Obtain Health Information. J. Consum. Health Internet 2019, 23, 366–377. [Google Scholar] [CrossRef]
- Couch, C. Descriptive Analysis of Patient Sexual Identity and Trust in the Doctor-Patient Relationship. Qual Health Res. 2017, 21, 1182–1190. [Google Scholar] [CrossRef] [PubMed]
- Berry, A.C.; Berry, B.; Wang, B.; Mulekar, M.; Kanar, O.; Nakshabendi, R.; Berry, N.; Kichler, K.; Sharma, V.; Kishore, V.; et al. Evaluation of Baseline Health Literacy for Diagnostic and Triage Accuracy of Online Symptom Checkers for Gastrointestinal Illnesses: 998. Off. J. Am. Coll. Gastroenterol. ACG. Available online: https://journals.lww.com/ajg/Fulltext/2016/10001/Evaluation_of_Baseline_Health_Literacy_for.998.aspx (accessed on 5 September 2022).
- Zhang, Y.; Sun, Y.; Kim, Y. The influence of individual differences on consumer’s selection of online sources for health information. Comput. Hum. Behav. 2017, 67, 303–312. [Google Scholar] [CrossRef]
- Lee, T.H.; Mcglynn, E.A.; Safran, D.G. A Framework for Increasing Trust Between Patients and the Organizations That Care for Them. JAMA J. Am. Med. Assoc. 2019, 321, 539–540. [Google Scholar] [CrossRef]
- Hale, T.M.; Cotten, S.R.; Drentea, P.; Goldner, M. Rural-urban differences in general and health-related Internet use. Am. Behav. Sci. 2010, 53, 1304–1325. [Google Scholar] [CrossRef]
- Perez, S.L.; Kravitz, R.L.; Bell, R.A.; Chan, M.S.; Paterniti, D.A. Characterizing internet health information seeking strategies by socioeconomic status: A mixed methods approach. BMC Med. Inform. Decis. Mak. 2016, 16, 107. [Google Scholar] [CrossRef] [Green Version]
- Norhayati, M.N.; Azlina, I. Patient satisfaction with doctor-patient interaction and its association with modifiable cardiovascular risk factors among moderately-high risk patients in primary healthcare. PeerJ 2017, 5, e2983. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.G.; Vortherms, S.A.; Hong, X. China’s Health Reform Update. Annu. Rev. Public Health 2017, 38, 431–448. [Google Scholar] [CrossRef] [PubMed]
| Description | Observation (N = 28,721) | Description (%/X ± SD) | |
|---|---|---|---|
| Dependent variables | |||
| The primary healthcare seeking | 1 = Primary care facilities | 18,292 | 63.7 |
| 0 = Otherwise | 10,429 | 36.3 | |
| Independent variables | |||
| Patients’ trust in physicians | 0~10 | 28,721 | 6.81 ± 2.345 |
| Internet use | Hours | 28,721 | 3.197 ± 8.124 |
| Control variables | |||
| Gender | 1 = Male | 14,048 | 48.9 |
| 0 = Female | 14,673 | 51.1 | |
| Age (years) | |||
| Residence status | 0 = Miss | 475 | 1.7 |
| 1 = Urban | 13,887 | 48.4 | |
| 2 = Rural | 14,359 | 50.0 | |
| Education status | 1 = Illiterate | 7850 | 27.3 |
| 2 = Primary school or Middle school | 14,275 | 49.7 | |
| 3 = High school/secondary school/technical school/Junior college | 4185 | 14.6 | |
| 4 = University or above | 2411 | 8.4 | |
| Health insurance | 1 = Public medical care | 855 | 3.0 |
| 2 = Urban employee medical insurance | 3813 | 13.3 | |
| 3 = Urban resident medical insurance (including one old and one small insurance) | 2486 | 8.7 | |
| 4 = Supplementary medical insurance | 209 | 0.7 | |
| 5 = New rural cooperative medical insurance | 18,790 | 65.4 | |
| 6 = None of the above | 2568 | 8.9 | |
| Marital status | 1 = Unmarried | 3470 | 12.1 |
| 2 = Married/living together | 23,605 | 82.2 | |
| 3 = Divorced/Widowed | 1646 | 5.7 | |
| Location | 1 = East | 13,023 | 45.3 |
| 2 = Central | 9289 | 32.3 | |
| 3 = West | 6409 | 22.3 | |
| Self-reported health status | 1= Excellent | 4050 | 14.1 |
| 2 = Very good | 5853 | 20.4 | |
| 3 = Good | 9975 | 34.7 | |
| 4 = Fair | 4296 | 15.0 | |
| 5 = Poor | 4542 | 15.8 | |
| Chronic disease | 1 = Yes | 4874 | 17.0 |
| 0 = No | 23,847 | 83.0 | |
| Religious belief | 1 = Yes | 7776 | 27.1 |
| 0 = No | 20,945 | 72.9 | |
| Heterogeneity analysis variables | |||
| Aging level | |||
| Urbanization level | |||
| PHC service level | The number of people covered by each PHC institution ) The number of PHC personnel per 10,000 people ) The number of beds in PHC institutions per 10,000 people ) The average number of diagnoses and treatments per year in each PHC institution ) The average number of hospital admissions per year in each PHC institution The utilization rate of hospital beds in community health service The utilization rate of hospital beds in township–village health centers | ||
| Primary Healthcare Seeking | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Patients’ trust in physicians | 0.055 (<0.01) | 0.048 (<0.01) | |
| Internet use | −0.002 (<0.01) | −0.0007 (<0.01) | |
| Patients’ trust in physicians * Internet use | 0.0008 (<0.01) |
| Patients’ Trust in Physicians | Internet Use | Patients’ Trust in Physicians * Internet Use | ||
|---|---|---|---|---|
| Primary healthcare seeking | ||||
| Low-level urbanization | Model 1 | 0.049 (<0.01) | ||
| Model 2 | −0.002 (<0.01) | |||
| Model 3 | 0.043 (<0.01) | −0.001 (<0.01) | 0.007 (<0.01) | |
| High-level urbanization | Model 1 | 0.062 (<0.01) | ||
| Model 2 | −0.002 (<0.01) | |||
| Model 3 | 0.054 (<0.01) | −0.004 (<0.01) | 0.009 (<0.01) | |
| Low-level aging | Model 1 | 0.053 (<0.01) | ||
| Model 2 | −0.002 (<0.01) | |||
| Model 3 | 0.048 (<0.01) | −0.008 (<0.01) | 0.007 (<0.01) | |
| High-level aging | Model 1 | 0.056 (<0.01) | ||
| Model 2 | −0.002 (<0.01) | |||
| Model 3 | 0.049 (<0.01) | −0.006 (<0.01) | 0.001 (<0.01) | |
| Low-level primary healthcare | Model 1 | 0.056 (<0.01) | ||
| Model 2 | −0.002 (<0.01) | |||
| Model 3 | 0.050 (<0.01) | −0.008 (<0.01) | 0.007 (<0.01) | |
| High-level of primary healthcare | Model 1 | 0.053 (<0.01) | ||
| Model 2 | −0.002 (<0.01) | |||
| Model 3 | 0.046 (<0.01) | −0.009 (<0.01) | 0.001 (<0.01) | |
| Primary Healthcare Seeking | Marginal Effects | Urbanization Level | Primary Healthcare Service Level | Aging Level | |||
|---|---|---|---|---|---|---|---|
| Low-Level | High-Level | Low-Level | High-Level | Low-Level | High-Level | ||
| Trust | Patients’ trust in physicians | 0.049 | 0.064 | 0.0586 | 0.0540 | 0.0551 | 0.0574 |
| Internet use | 0.0008 | 0.001 | 0.0009 | 0.0010 | 0.0007 | 0.0010 | |
| Primary Healthcare Seeking | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Patients’ trust in physicians | 0.295 (< 0.05) | 0.257 (0.003) | |
| Internet use | −0.019 (<0.01) | −0.016 (<0.01) | |
| Patients’ trust in physicians * Internet use | 0.005 (<0.01) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, J.; Bai, J.; Guo, Q.; Zhou, Z.; Yang, X.; Yu, Q. Impacts of Internet Use on Chinese Patients’ Trust-Related Primary Healthcare Utilization. Healthcare 2022, 10, 2114. https://doi.org/10.3390/healthcare10102114
Lu J, Bai J, Guo Q, Zhou Z, Yang X, Yu Q. Impacts of Internet Use on Chinese Patients’ Trust-Related Primary Healthcare Utilization. Healthcare. 2022; 10(10):2114. https://doi.org/10.3390/healthcare10102114
Chicago/Turabian StyleLu, Jiao, Jingyan Bai, Qingqing Guo, Zhongliang Zhou, Xiaowei Yang, and Qi Yu. 2022. "Impacts of Internet Use on Chinese Patients’ Trust-Related Primary Healthcare Utilization" Healthcare 10, no. 10: 2114. https://doi.org/10.3390/healthcare10102114
APA StyleLu, J., Bai, J., Guo, Q., Zhou, Z., Yang, X., & Yu, Q. (2022). Impacts of Internet Use on Chinese Patients’ Trust-Related Primary Healthcare Utilization. Healthcare, 10(10), 2114. https://doi.org/10.3390/healthcare10102114





