The Impact of Depression on the Functional Outcome of the Elderly Stroke Victim from a Gender Perspective: A Systematic Review
Abstract
:1. Introduction
1.1. Problem Statement
1.2. Importance of Occupational Therapy
2. Materials and Methods
2.1. Information Sources
2.2. Search Strategy
2.3. Selection Criteria
3. Results
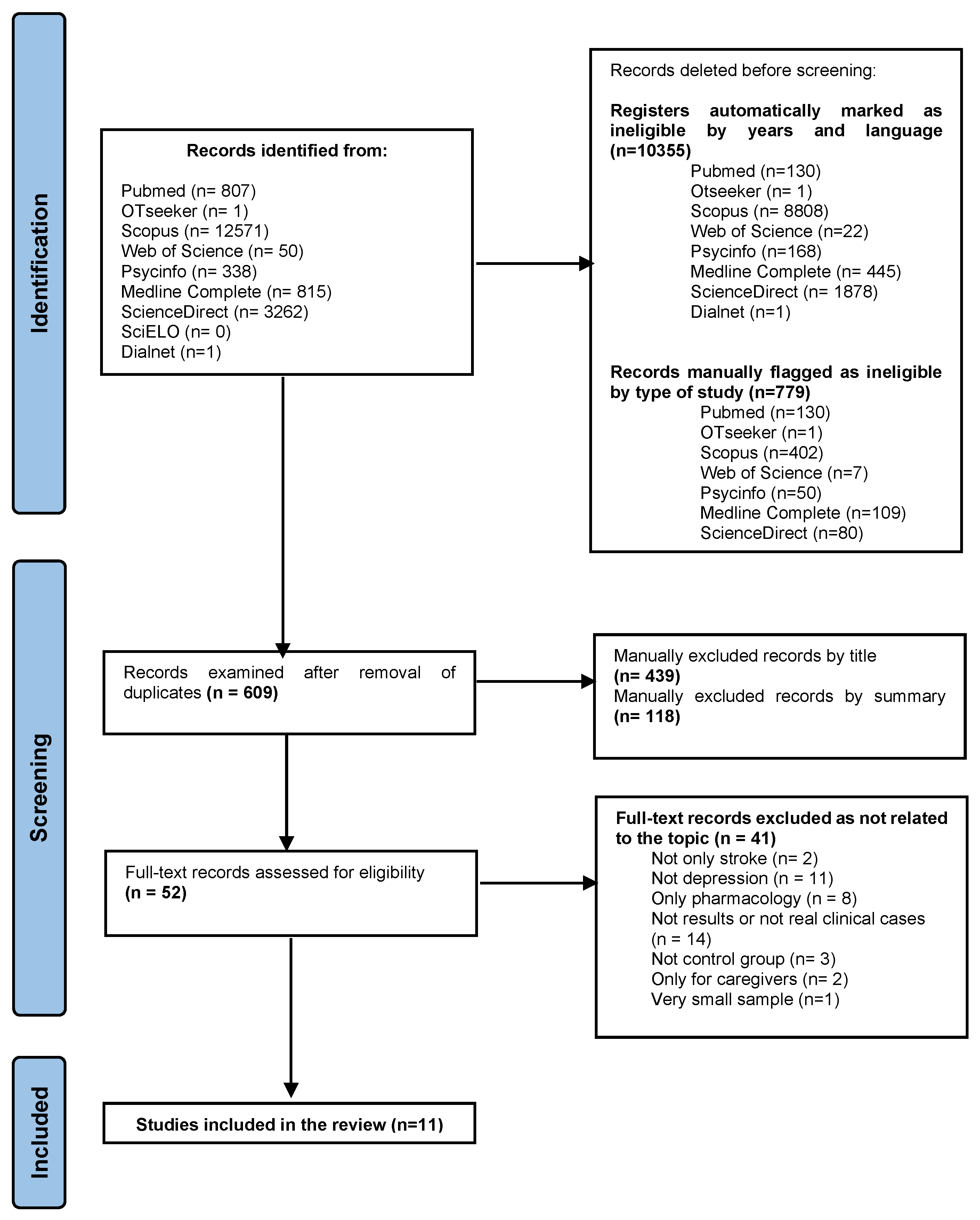
3.1. Search Results
3.2. Characteristics of Included Trials
3.3. Included Studies
3.4. Quality of Trials
4. Discussion
4.1. Impact of Depression on Functionality and Recovery
4.2. Impact of Depression on Women Versus Men
4.3. The Need for Occupational Therapy Approach in Physical and Mental Rehabilitation
5. Limitations
6. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Flach, C.; Muruet, W.; Wolfe, C.D.A.; Bhalla, A.; Douiri, A. Risk and Secondary Prevention of Stroke Recurrence: A Population-Base Cohort Study. Stroke 2020, 51, 2435–2444. [Google Scholar] [CrossRef] [PubMed]
- Vincent-Onabajo, G.; Adamu, A. Prevalence of Recurrent Stroke among a Rehabilitation Cohort in Nigeria. P.R. Health Sci. J. 2019, 38, 181–184. [Google Scholar]
- Matías-Guiu, J. La investigación en epidemiología del ictus en España. ¿Estudios de base poblacional o utilización de aproximaciones a partir del CMBD? Rev. Esp. Cardiol. 2007, 60, 563–564. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Guzmán, J.; Egido, J.; Gabriel-Sánchez, R.; Barberà, G.; Fuentes, B.; Pérez, C.; Abilleira, S. Incidence of Strokes in Spain. Methodological Foundations of the Iberictus Study. Rev. De Neurol. 2008, 47, 617–623. [Google Scholar]
- Gómez-Moreno, L. Evolución del daño cerebral en un paciente tras un ictus isquémico bilateral. DCN 2017, 4, 25. [Google Scholar] [CrossRef]
- Concepción, O.; Fleita, M.; Barrero, Y.; Velázquez, N.; Rojas-Fuentes, J. Depresión Post–Ictus: Frecuencia y Factores Determinantes. Rev. Cuba. De Neurol. Y Neurocir. 2012, 2, 9–16. [Google Scholar]
- Pérez-Menéndez, A. Atlas del Ictus en España; Sociedad Española de Neurología: Barcelona, Spain, 2019. [Google Scholar]
- Tsalta-Mladenov, M.; Andonova, S. Health-Related Quality of Life after Ischemic Stroke: Impact of Sociodemographic and Clinical Factors. Neurol Res. 2021, 43, 553–561. [Google Scholar] [CrossRef]
- Medeiros, G.C.; Roy, D.; Kontos, N.; Beach, S.R. Post-Stroke Depression: A 2020 Updated Review. Gen. Hosp. Psychiatry 2020, 66, 70–80. [Google Scholar] [CrossRef]
- Álvarez-Sabin, J.; Masjuan-Vallejo, J. Comprender El Ictus: (Infarto y Hemorragia Cerebral); Amat Editorial: Barcelona, Spain, 2013. [Google Scholar]
- Sivolap, Y.P.; Damulin, I.V. Stroke and depression. Zh. Nevrol. Psikhiatr. Im. S. S. Korsakova. 2019, 119, 143–147. [Google Scholar] [CrossRef]
- Zoch-Zannini, C.E. Depresión. 2002, p. 14. Available online: https://www.binasss.sa.cr/bibliotecas/bhp/textos/depresion2005.pdf (accessed on 10 September 2022).
- Alexopoulos, G.S. Depression in the Elderly. Lancet 2005, 365, 1961–1970. [Google Scholar] [CrossRef]
- Haast, R.A.; Gustafson, D.R.; Kiliaan, A.J. Sex Differences in Stroke. J. Cereb. Blood Flow Metab. 2012. [Google Scholar] [CrossRef] [Green Version]
- Gibson, C.L. Cerebral Ischemic Stroke: Is Gender Important? J. Cereb. Blood Flow Metab. 2013, 33, 1355–1361. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibson, C.; Attwood, L. The Impact of Gender on Stroke Pathology and Treatment. Neurosci. Biobehav. Rev. 2016, 67, 119–124. [Google Scholar] [CrossRef]
- Dafer, R.M.; Rao, M.; Shareef, A.; Sharma, A. Poststroke Depression. Top. Stroke Rehabil. 2008, 15, 13–21. [Google Scholar] [CrossRef]
- Das, J.; Rajanikant, G.K. Post Stroke Depression: The Sequelae of Cerebral Stroke. Neurosci. Biobehav. Rev. 2018, 90, 104–114. [Google Scholar] [CrossRef]
- Mazure, C.M.; Weinberger, A.H.; Pittman, B.; Sibon, I.; Swendsen, J. Gender and Stress in Predicting Depressive Symptoms Following Stroke. Cerebrovasc. Dis. 2014, 38, 240–246. [Google Scholar] [CrossRef] [Green Version]
- López-Espuela, F.; Jiménez-Gracia, M.A.; Blanco-Gazapo, M.A.; Gavilán-Iglesias, T.; Portilla-Cuenca, J.C.; Pedrera-Zamorano, J.D. Depresión Postictus: Factores Que Afectan al Estado de Ánimo. Rev. Científica De La Soc. Española De Enfermería Neurológica 2011, 34, 32–38. [Google Scholar] [CrossRef]
- Espárrago-Llorca, G.; Castilla-Guerra, L.; Fernández Moreno, M.C.; Ruiz Doblado, S.; Jiménez Hernández, M.D. Depresión Post Ictus: Una Actualización. Neurología 2015, 30, 23–31. [Google Scholar] [CrossRef]
- Paolucci, S. Advances in Antidepressants for Treating Post-Stroke Depression. Expert Opin. Pharmacother. 2017, 18, 1011–1017. [Google Scholar] [CrossRef]
- Benavente, O.R.; White, C.L.; Pearce, L.; Pergola, P. The Secondary Prevention of Small Subcortical Strokes (SPS3) Study. Int. J. Stroke 2011, 6, 164–175. [Google Scholar] [CrossRef]
- Loubinoux, I.; Kronenberg, G.; Endres, M.; Schumann-Bard, P.; Freret, T.; Filipkowski, R.K.; Kaczmarek, L.; Popa-Wagner, A. Post-Stroke Depression: Mechanisms, Translation and Therapy. J. Cell. Mol. Med. 2012, 16, 1961–1969. [Google Scholar] [CrossRef]
- Facucho-Oliveira, J.; Esteves-Sousa, D.; Espada-Santos, P.; Moura, N.; Albuquerque, M.; Fraga, A.M.; Sousa, S.; Cintra, P.; Mendonça, L.; Pita, F. Depression after Stroke. Pract. Neurol. 2021, 21, 384–391. [Google Scholar] [CrossRef] [PubMed]
- Belagaje, S.R. Stroke Rehabilitation. Continuum 2017, 23, 238–253. [Google Scholar] [CrossRef]
- Coleman, E.R.; Moudgal, R.; Lang, K.; Hyacinth, H.I.; Awosika, O.O.; Kissela, B.M.; Feng, W. Early Rehabilitation After Stroke: A Narrative Review. Curr. Atheroscler. Rep. 2017, 19, 59. [Google Scholar] [CrossRef] [Green Version]
- Langhorne, P.; Pollock, A.; in Conjunction with The Stroke Unit Trialists’ Collaboration. What Are the Components of Effective Stroke Unit Care? Age Ageing 2002, 31, 365–371. [Google Scholar] [CrossRef] [Green Version]
- AOTA 2020 Occupational Therapy Code of Ethics. Am. J. Occup. Ther. 2020, 74, 7413410005p1–7413410005p13. [CrossRef]
- Paolucci, S.; Gandolfo, C.; Provinciali, L.; Torta, R.; Toso, V.; DESTRO Study Group. The Italian Multicenter Observational Study on Post-Stroke Depression (DESTRO). J. Neurol. 2006, 253, 556–562. [Google Scholar] [CrossRef]
- Legg, L.; Drummond, A.; Leonardi-Bee, J.; Gladman, J.R.F.; Corr, S.; Donkervoort, M.; Edmans, J.; Gilbertson, L.; Jongbloed, L.; Logan, P.; et al. Occupational Therapy for Patients with Problems in Personal Activities of Daily Living after Stroke: Systematic Review of Randomised Trials. BMJ 2007, 335, 922. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Matos, A.P.; Pegorari, M.S. How to Classify Clinical Trials Using the PEDro Scale? J. Lasers Med. Sci. 2020, 11, 1–2. [Google Scholar] [CrossRef] [Green Version]
- Zhang, S.-H.; Wang, Y.-L.; Zhang, C.-X.; Zhang, C.-P.; Xiao, P.; Li, Q.-F.; Liang, W.-R.; Pan, X.-H.; Zhou, M.-C. Effect of Interactive Dynamic Scalp Acupuncture on Post-Stroke Cognitive Function, Depression, and Anxiety: A Multicenter, Randomized, Controlled Trial. Chin. J. Integr. Med. 2022, 28, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Niu, Y.; Sheng, S.; Chen, Y.; Ding, J.; Li, H.; Shi, S.; Wu, J.; Ye, D. The Efficacy of Group Acceptance and Commitment Therapy for Preventing Post-Stroke Depression: A Randomized Controlled Trial. J. Stroke Cerebrovasc. Dis. 2022, 31, 106225. [Google Scholar] [CrossRef] [PubMed]
- Taravati, S.; Capaci, K.; Uzumcugil, H.; Tanigor, G. Evaluation of an Upper Limb Robotic Rehabilitation Program on Motor Functions, Quality of Life, Cognition, and Emotional Status in Patients with Stroke: A Randomized Controlled Study. Neurol. Sci. 2022, 43, 1177–1188. [Google Scholar] [CrossRef]
- Lin, R.-C.; Chiang, S.-L.; Heitkemper, M.M.; Weng, S.-M.; Lin, C.-F.; Yang, F.-C.; Lin, C.-H. Effectiveness of Early Rehabilitation Combined With Virtual Reality Training on Muscle Strength, Mood State, and Functional Status in Patients With Acute Stroke: A Randomized Controlled Trial. Worldviews Evid. Based Nurs. 2020, 17, 158–167. [Google Scholar] [CrossRef]
- Wang, X.; Li, J.; Wang, C.; Lv, J. The Effects of Mindfulness-Based Intervention on Quality of Life and Poststroke Depression in Patients with Spontaneous Intracerebral Hemorrhage in China. Int. J. Geriatr. Psychiatry 2020, 35, 572–580. [Google Scholar] [CrossRef]
- West, A.; Simonsen, S.A.; Jennum, P.; Cyril Hansen, N.; Schønsted, M.; Zielinski, A.; Sander, B.; Iversen, H.K. An Exploratory Investigation of the Effect of Naturalistic Light on Fatigue and Subjective Sleep Quality in Stroke Patients Admitted for Rehabilitation: A Randomized Controlled Trial. NeuroRehabilitation 2019, 45, 187–200. [Google Scholar] [CrossRef] [Green Version]
- Olukolade, O.; Osinowo, H.O. Efficacy of Cognitive Rehabilitation Therapy on Poststroke Depression among Survivors of First Stroke Attack in Ibadan, Nigeria. Behav. Neurol. 2017, 2017, 4058124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, J.; Lin, M.; Zhao, J.; Bi, S.; Ni, Z.; Shang, X. Different Interventions for Post-Ischaemic Stroke Depression in Different Time Periods: A Single-Blind Randomized Controlled Trial with Stratification by Time after Stroke. Clin. Rehabil. 2017, 31, 71–81. [Google Scholar] [CrossRef]
- Chun, M.H.; Chang, M.C.; Lee, S.-J. The Effects of Forest Therapy on Depression and Anxiety in Patients with Chronic Stroke. Int. J. Neurosci. 2017, 127, 199–203. [Google Scholar] [CrossRef]
- Kongkasuwan, R.; Voraakhom, K.; Pisolayabutra, P.; Maneechai, P.; Boonin, J.; Kuptniratsaikul, V. Creative Art Therapy to Enhance Rehabilitation for Stroke Patients: A Randomized Controlled Trial. Clin. Rehabil. 2016, 30. [Google Scholar] [CrossRef] [PubMed]
- Chaiyawat, P.; Kulkantrakorn, K. Randomized Controlled Trial of Home Rehabilitation for Patients with Ischemic Stroke: Impact upon Disability and Elderly Depression. Psychogeriatr. Off. J. Jpn. Psychogeriatr. Soc. 2012, 12, 193–199. [Google Scholar] [CrossRef]
- Verhagen, A. PEDro Scale Spanish. 1998. Available online: https://www.pedro.org.au/wp-content/uploads/PEDro_scale.pdf(accessed on 10 September 2022).
- García-Perdomo, H.A. Conceptos fundamentales de las revisiones sistemáticas/metaanálisis. Urol. Colomb. 2015, 24, 28–34. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, L.; Nugent, N.; Biros, L. Occupational Therapy Practice in Hospital-Based Stroke Rehabilitation? Scand. J. Occup. Ther. 2012, 19, 132–139. [Google Scholar] [CrossRef] [PubMed]

| Database | Search Strategy | Results |
|---|---|---|
| Pubmed | ((“stroke”) AND (“depression”)) AND (“treatment outcome”) | 807 |
| Otseeker | [Any Field] like ‘“stroke”‘ AND [Any Field] like ’”depression”‘ AND [Any Field] like ’”treatment outcome”‘ | 1 |
| Scopus | “stroke” AND ”depression” AND ”treatment outcome” | 12,571 |
| Web of Science | ((ALL = (“stroke”)) AND ALL = (“depression”)) AND ALL = (“treatment outcome”) | 50 |
| Psycinfo | Stroke AND ”depression” AND ”treatment outcome” | 338 |
| Medline Complete | “stroke” AND ”depression” AND ”treatment outcome” | 815 |
| Science Direct | Stroke AND ”depression” AND ”treatment outcome” | 3262 |
| SciELO | “stroke” and “depression” and ”treatment outcome” | 0 |
| Dialnet | Stroke AND ”depression” AND ”treatment outcome” | 1 |
| 17,845 |
| Database | Search Filters | Final Strategy | Results |
|---|---|---|---|
| Pubmed | Randomized Controlled Trial, in the last 10 years, English, Spanish | (“stroke” [All Fields] AND “depression” [All Fields] AND “treatment outcome” [All Fields])) | 130 |
| OTseeker | without filters | [AnyField] like ’”stroke”‘ AND [Any Field] like ’”depression”‘ AND [Any Field] like ’”treatment outcome”‘ | 1 |
| Scopus | Limit-to2012– 2022, English, Spanish | “stroke” AND “depression” AND “treatment outcome” | 402 |
| Web of Science | Publication Years: 2012– 2022, English | ((ALL = (“stroke”)) AND ALL = (“depression”)) AND ALL = (“treatment outcome)) | 7 |
| Psycinfo | 2012–2022, English | “stroke” AND ”depression” AND ”treatment outcome” | 50 |
| Medline Complete | Limit to 2012-2022 English | “stroke” AND “depression” AND “treatment outcome” | 109 |
| Science Direct | 2012–2022 | stroke AND ”depression” AND ”treatment outcome” | 80 |
| Dialnet | without filters | stroke AND ”depression” AND “treatment outcome” | 0 |
| TOTAL | 779 |
| Author/Year | Study Type | Population | Study Group | Intervention Characteristics | Measures | Results | PEDro Scale |
|---|---|---|---|---|---|---|---|
| Shao-hua, Zhang et al. (2022) [34] | Multicentre Random iZed Controlled Trial | n = 660 | Patients with cognitive disorders after stroke divided into IDSA group (interactive dynamic scalp acupuncture; n = 218), SSCT group (simple combined therapy; n = 222) and TSA group (traditional scalp acupuncture; n = 220). | 2 months (all received conventional medication and physical rehabilitation. The IDSA group received extra computer-based cognitive training). | MoCA, MMSE, HAMD, HAMA, PSQI, MBI | For the SCT and TSA groups, MMSE and MoCA scores were higher. For the IDSA group, HAMA, PSQI and HAMD scores were lower from the second month onward. This group improved in dysfunctionality and dependence (p < 0.01) | 8/10 |
| Niu, Yunlian et al. (2022) [35] | Randomized Controlled Trial | n = 104 | Stroke patients receiving G-ACT psychological therapy n = 52) versus the group receiving usual care only n = 52). | Evaluation of the intervention at 2 weeks, 1 month, and 3 months (5 sessions of 45–50 min of therapy with a specialist during hospitalization). | HAMD, NIHSS, BI | Depressive symptoms decreased in the intervention group, as did the IB score (p = 0.018). However, at 3 months the IB measures were similar between groups, so the intervention did not improve the prognosis for functionality (p = 0.191) | 7/10 |
| Taravati, Sahel et al. (2021) [36] | Blinded Randomized Controlled Study | n = 37 | Patients with hemiplegia due to stroke divided into a study group with conventional rehabilitation and a robotic-based rehabilitation system (n = 17) and a control group with only conventional rehabilitation (n = 20). | 4 weeks (5 days a week for each type of rehabilitation). | Fulg-Meyer, MoCA, CES- Depression questionnaire | The decrease in depression and the increase in hand strength and function of the patients in the study group are noteworthy (p < 0.05) Both groups improved the respective MoCA and Fulg- Meyer | 9/10 |
| Lin, Ruei-Ching et al. (2020) [37] | Randomized Controlled Trial | n = 143 | Hospitalized stroke patients ( n= 38) received 5 extra days of virtual reality training. | 21 days (5 sesh/week of early rehabilitation; 2 times/day) | MRCScale, HADS, PASS, BI | The experimental group increased muscle strength along with anxiety (p = 0.003) and depression (p = 0.001). | 9/10 |
| Wang, Xiaoyu et al. (2020) [38] | Randomized Controlled Trial | n= 134 | Patients who had suffered an intracranial hemorrhage received mindfulness-based cognitive therapy (n = 67) versus the control group (n = 67). | 8 weeks (2-h group sessions based on adaptive thoughts, feelings, and experiences). | CES-Dq, MAAS, FACT-Br, NIHSS | In the intervention group, significant changes were found in depression (p > 0.01), mindfulness (p < 0.01), social and emotional well-being (p < 0.05), and quality of life (p < 0.05). | 8/10 |
| West, Anders et al. (2019) [39] | Quasi-Randomized Controlled Trial | n = 71 | Stroke patients in a rehabilitation unit equipped with daylight (n = 39) versus stroke patients in a rehabilitation unit with standard indoor lighting (n = 32). | 1 year (simulation of the rhythm of natural light 24 h, being dim until 07:00, maximum until 15:00, and dimmed until 22:00 when it was switched off). | HAMD, HADS, WHO-5, MoCA | The group exposed to natural light had a significant decrease in post-stroke depression and an increase in well-being at discharge (p = 0.046). Post-stroke anxiety was also reduced (p = 0.045). There were no significant differences in cognition. | 5/10 |
| Olukolade, Olugbemi. Osinowo, Helen O. (2017) [40] | Randomized Controlled Trial | n = 30 | Patients with first stroke divided into groups of n = 10 according to the different interventions: group A (cognitive rehabilitation therapy); group B (psychoeducation); group C (usual care). | 3.5 months (group A: 9 sessions; group B: 9 sessions; group C: waiting list for care). | BDI, LESS | Cognitive rehabilitation therapy has a greater effect on post-stroke depression (p < 0.001) than psychoeducation and usual care. It is suggested that the type of intervention is influential in detecting post-stroke depression both at baseline and after treatment. | 9/10 |
| Gao, Jie et al. (2016) [41] | Blinded Randomized Controlled Trial | n = 274 | A: both placebo medication and psychological therapy (n = 91); B: citalopram and psychological therapy with a non-specialist physician (n = 91); C: placebo medication and psychological therapy with a specialist (n = 92). | 3 months (A: discussions twice a week; B: discussions twice a week; C: 2 h of session per week over the 3 months). Sessions of 1 h of Bobath Therapy were held 4/week. | HAMD, MES, BI, BDI, MS, FIM, | Group B improved in depression and melancholy (p < 0.05). In fact, this same group had greater adverse effects due to the drug received. | 8/10 |
| Chun, Min-Ho et al. (2016) [42] | Randomized Controlled Trial | n = 59 | Patients with chronic stroke were included in forest group (n = 30) versus urban group (n = 29). | 4 days and 3 nights (the forest group worked on meditation in the forest while the urban group stayed in a hotel). | BDI, HAMD, STAI | The forest group showed a decrease in BDI, HAMD, and SATI scores (p < 0.05). See the need to manage psychological conditions (anxiety and depression) in this population. | 9/10 |
| Kongkasuwan, Ratcharinetal (2015) [43] | Randomized Controlled Trial | n = 118 | Stroke patients (older than 50 years old) received only conventional physical therapy (n = 59) versus patients who received conventional physical therapy and creative art therapy (n = 59). | 4 weeks (20 sessions of conventional physical therapy and 8 sessions of creative art therapy of 1.5–2 h in groups of 5–10 patients). | AMT, MBI, HADS, PTQoLq | The creative art therapy group improved functionality, depression (p < 0.001), and quality of life (p < 0.001) after the intervention. There were no significant differences in anxiety and mental state (p = 0.123). | 9/10 |
| Chaiyawat, Pakaratee. Kulkantrakorn, Kongkiat. (2012) [44] | Randomized Controlled Trial | n = 60 | Stroke patients received home exercise program (n = 30) versus the control group who only received home rehabilitation instructions (n = 30). | 6 months (intervention group receives physiotherapy, education, counseling versus problem-solving). | BI, HADS, TMSE | Barthel (p < 0.03) and HADS (p < 0.01) scores improved after 2 years. Depression was associated with dependency and quality of life. The higher HADS score of the control group showed a lower BI score. | 9/10 |
| Nº Subjects | Measures | |||||
|---|---|---|---|---|---|---|
| Source, Year | Intervention Group (a) | Control Group (b) | TOTAL (c) | IIG(a) | ICG(b) | RR |
| Shao-hua, Zhang et al. (2022) | 218 + 222 * | 220 | 660 | 0.33 | 0.33 | 1 |
| Niu, Yunlian et al. (2022 | 52 | 52 | 104 | 0.5 | 0.5 | 1 |
| Taravati, Sahel et al. (2021) | 17 | 20 | 37 | 0.46 | 0.54 | 0.85 |
| Lin, Ruei-Ching et al. (2020) | 38 | 107 | 143 | 0.26 | 0.75 | 0.35 |
| Wang, Xiaoyu et al. (2020) | 67 | 67 | 134 | 0.64 | 0.64 | 1 |
| West, Anders et al. (2019) | 39 | 32 | 71 | 0.55 | 0.63 | 0.87 |
| Olukolade, Olugbemi. Osinowo, Helen O. (2017) | 10 + 10 * | 10 | 30 | 0.33 | 0.33 | 1 |
| Gao, Jie et al. (2016) | 91 + 92 * | 91 | 274 | 0.33 | 0.33 | 1 |
| Chun, Min-Ho et al. (2016) | 30 | 20 | 59 | 0.51 | 0.34 | 1.5 |
| Kongkasuwan, Ratcharin et al. (2015) | 59 | 59 | 118 | 0.5 | 0.5 | 1 |
| Chaiyawat, Pakaratee. Kulkantrakorn, Kongkiat. (2012) | 30 | 30 | 60 | 0.5 | 0.5 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Franco-Urbano, M.S.; Rodríguez-Martínez, M.d.C.; García-Pérez, P. The Impact of Depression on the Functional Outcome of the Elderly Stroke Victim from a Gender Perspective: A Systematic Review. Healthcare 2022, 10, 2110. https://doi.org/10.3390/healthcare10102110
Franco-Urbano MS, Rodríguez-Martínez MdC, García-Pérez P. The Impact of Depression on the Functional Outcome of the Elderly Stroke Victim from a Gender Perspective: A Systematic Review. Healthcare. 2022; 10(10):2110. https://doi.org/10.3390/healthcare10102110
Chicago/Turabian StyleFranco-Urbano, María Salud, María del Carmen Rodríguez-Martínez, and Patricia García-Pérez. 2022. "The Impact of Depression on the Functional Outcome of the Elderly Stroke Victim from a Gender Perspective: A Systematic Review" Healthcare 10, no. 10: 2110. https://doi.org/10.3390/healthcare10102110
APA StyleFranco-Urbano, M. S., Rodríguez-Martínez, M. d. C., & García-Pérez, P. (2022). The Impact of Depression on the Functional Outcome of the Elderly Stroke Victim from a Gender Perspective: A Systematic Review. Healthcare, 10(10), 2110. https://doi.org/10.3390/healthcare10102110





