Competence in Spiritual and Emotional Care: Learning Outcomes for the Evaluation of Nursing Students
Abstract
:1. Introduction
Main Aim
2. Materials and Methods
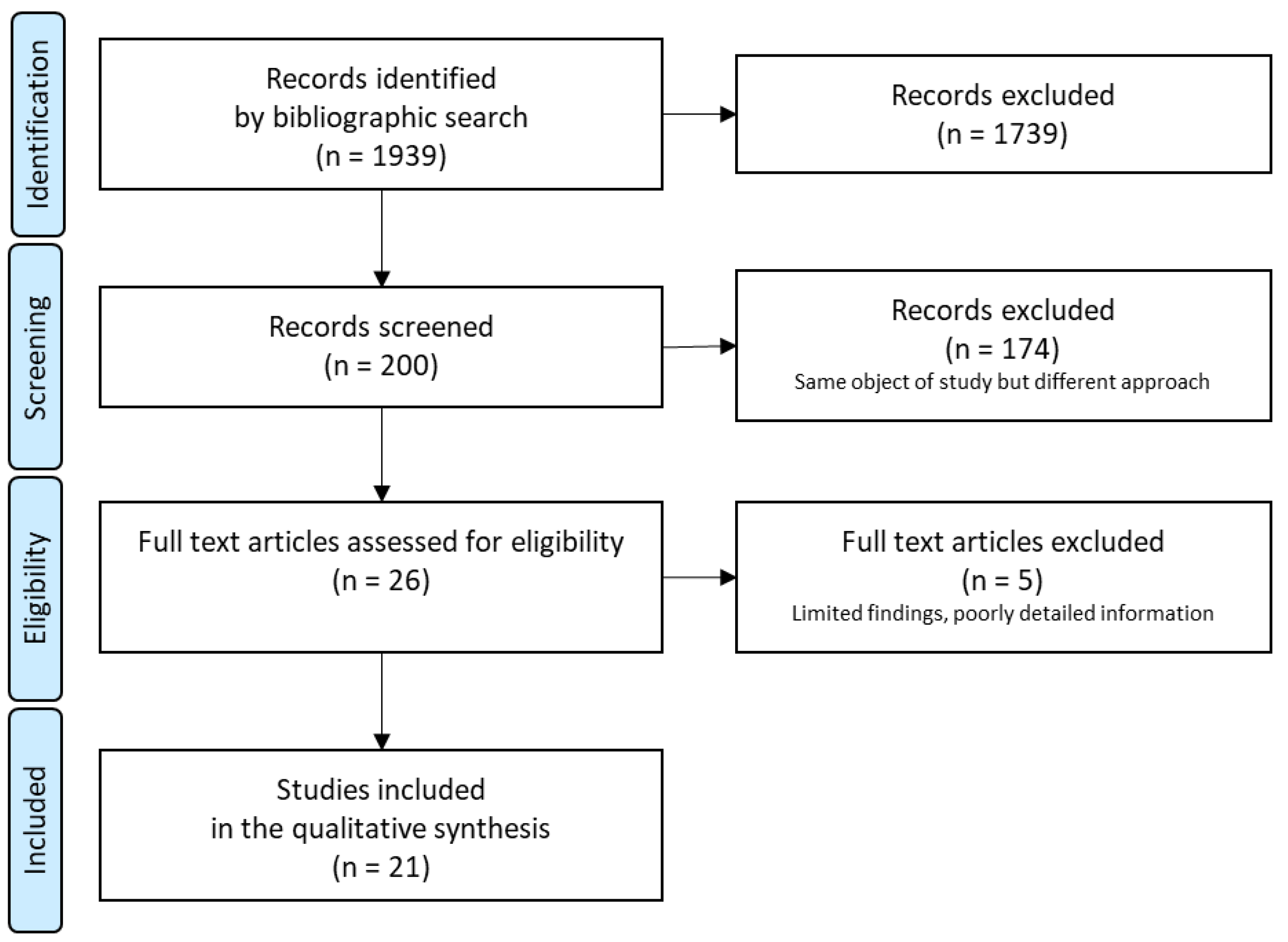
2.1. Design
2.2. Procedure
2.2.1. Phase I—Proposal Design
2.2.2. Phase II—Validation
- -
- Relevance: The expert considered the learning outcome appropriate and specific for its inclusion in the Nursing Degree curriculum;
- -
- Priority: The expert considered the importance of demonstrating the learning outcome during the training process that enables one to practice the nursing profession;
- -
- Clarity: The wording of the learning outcome was correct, clear, objective and consistent with the rest of the proposed outcomes.
2.3. Ethics
3. Results
3.1. Phase I—Proposal Design
3.2. Phase II—Validation
3.2.1. Assessment and Diagnosis
- -
- Identify the dimensions that spirituality encompasses, differentiating between spirituality and religion;
- -
- Perform a conceptualisation of the spiritual and emotional sphere of the person;
- -
- Carry out an assessment of the needs related to the spiritual and emotional area;
- -
- Show respect and closeness during the assessment of the person, creating an environment that is favourable to communication;
- -
- Recognise that the illness may affect the person’s values and beliefs;
- -
- Detect the presence of suffering in the person;
- -
- Assess the person’s spiritual well-being;
- -
- Perform a priority analysis on the information collected;
- -
- Identify nursing diagnoses related to the spiritual area;
- -
- Identify nursing diagnoses related to the emotional area;
- -
- Know the defining characteristics and related factors/ risk factors of nursing diagnoses related to the spiritual and emotional area;
- -
- Carry out a differential diagnosis between the different care problems in the spiritual area;
- -
- Carry out a differential diagnosis between the different care problems in the emotional area;
- -
- Make the record of the assessment and diagnosis of the spiritual and emotional area.
3.2.2. Planning
- -
- Select the outcomes criteria for each person taking into account their overall situation and their values and beliefs;
- -
- Select the interventions related to the spiritual and emotional area, establishing an order of priority;
- -
- Make a record of the planned care plan and the expected evolution of the person;
- -
- Carry out a care plan focused on coping with threats that may increase suffering;
3.2.3. Intervention
- -
- Dedicate time to the relationship with the person being cared for, maintaining continuity in the relationship;
- -
- Respect the needs and demands of privacy of the person, respecting moments of silence and solitude and moments of meeting with loved ones;
- -
- Facilitate the expression of feelings of guilt and forgiveness, identifying the painful feelings of guilt and directing the person in self-forgiveness;
- -
- Facilitate the spiritual growth of the person and their family, helping them to explore beliefs in relation to healing;
- -
- Facilitate religious practice, encouraging conversation about their interests, use and participation in rituals or practices that do not harm health;
- -
- Help the person in the acceptance and search for meaning in life;
- -
- Help the person recognise and express feelings such as anxiety, anger, or sadness;
- -
- Listen to the expression of feelings about the loss;
- -
- Help the person to control anger by identifying its causes, developing appropriate methods of expression and training in techniques that provide calm;
- -
- Help the person to enhance self-esteem, encouraging positive statements about oneself and facilitating an environment and activities that increase self-esteem;
- -
- Help the person to train assertiveness, monitoring levels of anxiety and discomfort related to behaviour change;
- -
- Help the person clarify the values and expectations that may be involved in making life decisions;
- -
- Help the person and their family to identify the areas of hope in life, reviewing the goals related to the object of hope and including them in the care plan;
- -
- Apply the counselling technique, helping the person to identify the problem or related factor, prioritising possible alternatives to the problem, considering their strengths and weaknesses;
- -
- Apply relaxation techniques;
- -
- Give emotional support to the person;
3.2.4. Evaluation and Quality
- -
- Monitor the person’s spiritual and emotional situation, through the selected indicators;
- -
- Monitor the person’s level of suffering through the selected indicators;
- -
- Evaluate the impact of care on the level of suffering of the person;
3.2.5. Communication and Interpersonal Relationship
- -
- Show hospitality in welcoming the person, showing interest in their values and expectations;
- -
- Create a climate of intimacy that allows communication on aspects of the spiritual and emotional area of the person;
- -
- Identify the situations in which the person requires spaces of silence and respect them;
- -
- Transmit truthfulness and use clear language without hesitation, responding to the person’s doubts;
- -
- Do not make judgments and respect the ontological dignity of the person when the values and beliefs are different from their own;
- -
- Plan care considering the moments of intimacy of the person;
- -
- Listen to the expression of feelings about the loss;
- -
- Carry out active listening avoiding barriers and using silence/listening to encourage expressing feelings, thoughts and concerns.
3.2.6. Knowledge and Intrapersonal Development of the Student
- -
- Reflect on one’s own vocation, vital values and attitudes, identifying positive and negative attitudes towards caring for the spiritual and emotional area;
- -
- Reflect on one’s own values and beliefs and identify how they influence caring for others;
- -
- Recognise one’s own limits and virtues in spiritual care;
- -
- Recognise the importance of spirituality in your life;
- -
- Recognise the signs of spiritual and emotional exhaustion;
- -
- Show personal knowledge by analysing one’s own strengths and weaknesses on a spiritual and emotional level;
- -
- Show self-awareness and emotional control, maintaining self-control in situations of personal suffering;
- -
- Show a proactive attitude of improvement on a personal level;
- -
- Find spaces to reflect and connect with yourself: meditation, directed imagination, relaxation;
- -
- Find solutions to the negative influence of one’s own values and beliefs in care;
- -
- Identify situations that cause stress;
- -
- Identify the signs and symptoms of “compassion fatigue” or “cost of caring”;
- -
- Relate sensations and experiences in stressful situations to the team;
- -
- Analyse how affects the situations of the people cared to one’s inner life and relationships;
- -
- Respect values and beliefs other than your own;
- -
- Ask for help in situations that you cannot control or resolve;
- -
- Learn to treat spiritual and emotional care problems identified in the person as a team.
4. Discussion
4.1. Limitations and Future Lines
4.2. Relevance to Clinical Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. WHO and Partners Call for Urgent Investment in Nurses. Available online: https://www.who.int/news-room/detail/07-04-2020-who-and-partners-call-for-urgent-investment-in-nurses (accessed on 1 May 2022).
- World Health Organization; International Council of Nurses, & Nursing Now. World Health Organization. State of the World’s Nursing 2020: Investing in Education, Jobs and Leadership; World Health Organization: Geneva, Switzerland, 2020; ISBN 978-92-4-000327-9. [Google Scholar]
- All-Party Parliamentary Group on Global Health (APPG). Triple Impact—How Developing Nursing Will Improve Health, Promote Gender Equality and Support Economic Growth; APPG: London, UK, 2016; Available online: https://globalhealth.inparliament.uk/sites/globalhealth.inparliament.uk/files/2020-12/DIGITAL%20APPG%20Triple%20Impact%20%283%29.pdf (accessed on 1 May 2022).
- Alligood, M.R. Nursing Theorists and Their Work, 9th ed.; Elsevier: St. Louis, MO, USA, 2018. [Google Scholar]
- World Health Organization. Nursing and Midwifery. Available online: https://www.who.int/health-topics/nursing#tab=tab_1 (accessed on 1 May 2022).
- Cooper, K.L.; Chang, E.; Sheehan, A.; Johnson, A. The impact of spiritual care education upon preparing undergraduate nursing students to provide spiritual care. Nurse Educ. Today 2013, 33, 1057–1061. [Google Scholar] [CrossRef]
- International Council of Nurses. The ICN Code of Ethics for Nurses; International Council of Nurses: Geneva, Switzerland, 2012. [Google Scholar]
- World Health Organization. COVID-19—China. Available online: https://www.who.int/emergencies/disease-outbreak-news/item/2020-DON229 (accessed on 1 May 2022).
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19–11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 1 May 2022).
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 1 May 2022).
- United Nations. Policy Brief: COVID-19 and the Need for Action on Mental Health; United Nations: New York, NY, USA, 2020; Available online: https://reliefweb.int/report/world/policy-brief-covid-19-and-need-action-mental-health-13-may-2020?gclid=Cj0KCQjwjIKYBhC6ARIsAGEds-JDpffXgVph9DKmNW3RZJzmtBfZu7AnHeFqClyn1IUPvoK73xa5Kl8aAnN-EALw_wcB (accessed on 1 May 2022).
- Ayuso Mateos, J.L.; Mediavilla, R.; McGreevy, K.R.; Bravo Ortiz, M.F. Informing the response to COVID-19 in Spain: Priorities for mental health research. Rev. De Psiquiatr. Y Salud Ment. 2021, 14, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Confederación Salud Mental España. Salud Mental y COVID-19: Un año de pandemia; Confederación Salud Mental España: Madrid, España, 2021. [Google Scholar]
- Halcomb, E.; Fernández, R.; Mursa, R.; Stephen, C.; Calma, K.; Ashley, C.; McInnes, S.; Desborough, J.; James, S.; Williams, A. Mental health, safety and support during COVID-19: A cross-sectional study of primary health care nurses. J. Nurs. Manag. 2022, 30, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Lake, E.T.; Narva, A.M.; Holland, S.; Smith, J.G.; Cramer, E.; Rosenbaum, K.; French, R.; Clark, R.; Rogowski, J.A. Hospital nurses’ moral distress and mental health during COVID-19. J. Adv. Nurs. 2022, 78, 799–809. [Google Scholar] [CrossRef] [PubMed]
- Leininger, M.M.; McFarland, M.R. Culture Care Diversity & Universality: A Worldwide Nursing Theory: A Worldwide Nursing Theory, 2nd ed.; Jones & Bartlett Learning: London, UK, 2005. [Google Scholar]
- Pacquiao, D.F.; Katz, J.R.; Sattler, V.; Zha, P.; Daub, K.F. Development of the Clients’ Perceptions of Providers’ Cultural Competency Instrument. J Transcult Nurs. 2021, 32, 539–550. [Google Scholar] [CrossRef] [PubMed]
- Campinha Bacote, J. Delivering patient-centered care in the midst of a cultural conflict: The role of cultural competence. OJIN Online J. Issues Nurs. 2011, 16, 5. [Google Scholar] [CrossRef]
- Aponte, J. Cultural competency in baccalaureate US nursing education: Hybrid course. Holist. Nurs. Pr. 2012, 26, 243–258. [Google Scholar] [CrossRef] [PubMed]
- van Leeuwen, R.; Cusveller, B. Nursing competencies for spiritual care. J. Adv. Nurs. 2004, 48, 234–246. [Google Scholar] [CrossRef] [PubMed]
- Chiang, Y.C.; Lee, H.C.; Chu, T.L.; Han, C.Y.; Hsiao, Y.C. A spiritual education course to enhance nursing students’ spiritual competencies. Nurse Educ. Pr. 2020, 49, 102907. [Google Scholar] [CrossRef] [PubMed]
- Ramezani, M.; Ahmadi, F.; Mohammadi, E.; Kazemnejad, A. Spiritual care in nursing: A concept analysis. Int. Nurs. Rev. 2014, 61, 211–219. [Google Scholar] [CrossRef]
- Baldacchino, D.R. Nursing competencies for spiritual care. J. Clin. Nurs. 2006, 15, 885–896. [Google Scholar] [CrossRef]
- Sawatzky, R.; Pesut, B. Attributes of Spiritual Care in Nursing Practice. J. Holist. Nurs. 2005, 23, 19–33. [Google Scholar] [CrossRef] [PubMed]
- Koenig, H.G. Religion, spirituality, and health: The research and clinical implications. ISRN Psychiatry 2012, 2012, 278730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewinson, L.P.; McSherry, W.; Kevern, P. Spirituality in pre-registration nurse education and practice: A review of the literature. Nurse Educ Today. 2015, 35, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Giske, T. How undergraduate nursing students learn to care for patients spiritually in clinical studies--a review of literature. J. Nurs. Manag. 2012, 20, 1049–1057. [Google Scholar] [CrossRef]
- Nardi, D.; Rooda, L. Spirituality-based nursing practice by nursing students: An exploratory study. J Prof Nurs. 2011, 27, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.G.; Voss, A.; Vahle, B.; Capp, S. Clinical Nursing Education: Using the FICA Spiritual History Tool to Assess Patients’ Spirituality. Nurse Educ. 2016, 41, E6–E9. [Google Scholar] [CrossRef] [PubMed]
- Jiménez Herrera, M.F.; Llauradó Serra, M.; Acebedo Urdiales, S.; Bazo Hernández, L.; Font Jiménez, I.; Axelsson, C. Emotions and feelings in critical and emergency caring situations: A qualitative study. BMC Nurs. 2020, 19, 60. [Google Scholar] [CrossRef] [PubMed]
- Lau, P.S.Y.; Wu, F.K.Y. Emotional Competence as a Positive Youth Development Construct: A Conceptual Review. Sci. World J. 2012, 1, 975189. [Google Scholar] [CrossRef] [Green Version]
- Waite, R.; McKinney, N.S. Capital We Must Develop: Emotional Competence Educating Pre-Licensure Nursing Students. Nurs. Educ. Perspect. 2016, 37, 101–103. [Google Scholar] [CrossRef]
- Kuven, B.M.; Giske, T. Talking about spiritual matters: First year nursing students’ experiences of an assignment on spiritual conversations. Nurse Educ. Today. 2019, 75, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.A. Nurse competence: A concept analysis. Int. J. Nurs. Knowl. 2012, 23, 172–182. [Google Scholar] [CrossRef]
- van Leeuwen, R.; Tiesinga, L.J.; Middel, B.; Post, D.; Jochemsen, H. The validity and reliability of an instrument to assess nursing competencies in spiritual care. J. Clin. Nurs. 2009, 18, 2857–2869. [Google Scholar] [CrossRef] [Green Version]
- Agencia Nacional de Evaluación de la Calidad y Acreditación (ANECA). Guía Para la Redacción, Puesta en Práctica y Evaluación de los Resultados del Aprendizaje; ANECA: Madrid, Spain, 2013. [Google Scholar]
- Boyer, L.; Pepin, J.; Dubois, S.; Descôteaux, R.; Robinette, L.; Déry, J.; Brunet, F.; Bolduc, J.; Deschênes, M.F. Adaptation and validation of a nursing competencies framework for clinical practice on a continuum of care from childhood to adulthood: A Delphi study. Nurse Educ, Today 2020, 93, 104530. [Google Scholar] [CrossRef] [PubMed]
- European Parliament. Directive 2013/55/EU of the European Parliament and of the Council of 20 November 2013 amending Directive 2005/36/EC on the Recognition of Professional Qualifications and Regulation (EU) No 1024/2012 on Administrative Cooperation through the Internal Market Information System (‘the IMI Regulation’). Available online: https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2013:354:0132:0170:en:PDF (accessed on 1 May 2022).
- Chiang, Y.C.; Lee, H.C.; Chu, T.L.; Han, C.Y.; Hsiao, Y.C. The impact of nurses’ spiritual health on their attitudes toward spiritual care, professional commitment, and caring. Nurs. Outlook. 2016, 64, 215–224. [Google Scholar] [CrossRef]
- Smith, S.M.; Buckner, M.; Jessee, M.A.; Robbins, V.; Horst, T.; Ivory, C.H. Impact of COVID-19 on New Graduate Nurses’ Transition to Practice: Loss or Gain? Nurse Educ. 2021, 46, 209–214. [Google Scholar] [CrossRef]
- Collado Boira, E.J.; Ruiz Palomino, E.; Salas Media, P.; Folch Ayora, A.; Muriach, M.; Baliño, P. “The COVID-19 outbreak”-An empirical phenomenological study on perceptions and psychosocial considerations surrounding the immediate incorporation of final-year Spanish nursing and medical students into the health system. Nurse Educ. Today. 2020, 92, 104504. [Google Scholar] [CrossRef] [PubMed]
- Mena Tudela, D.; González Chordá, V.M.; Andreu Pejó, L.; Mouzo Bellés, V.M.; Cervera Gasch, Á. Spanish nursing and medical students’ knowledge, confidence and willingness about COVID-19: A cross-sectional study. Nurse Educ. Today. 2021, 103, 104957. [Google Scholar] [CrossRef] [PubMed]
- Watson, J. Human Caring Science: A Theory of Nursing, 2nd ed.; Jones & Bartlett Learning: London, UK, 2012. [Google Scholar]
- Herdman, T.H.; Kamitsuru, S. NANDA International Nursing Diagnoses: Definitions and Classification, 2018–2020, 11th ed.; Thieme Publishers: New York, NY, USA, 2017. [Google Scholar]
- Marion, J.; Moorhead, S.; Bulechek, G.; Butcher, H.; Maas, M.; Swanson, E. NOC and NIC Linkages to NANDA-I and Clinical Conditions. Supporting Critical Reasoning and Quality Care, 3rd ed.; Mosby: St. Louis, MO, USA, 2011. [Google Scholar]
- Cone, P.H.; Giske, T. Teaching spiritual care--a grounded theory study among undergraduate nursing educators. J. Clin. Nurs. 2013, 22, 1951–1960. [Google Scholar] [CrossRef] [PubMed]
- Giske, T.; Cone, P.H. Opening up to learning spiritual care of patients: A grounded theory study of nursing students. J. Clin. Nurs. 2012, 21, 2006–2015. [Google Scholar] [CrossRef]
- Gómez del Pulgar García Madrid, M. Evaluación de Competencias en el Espacio Europeo de Educación Superior: Un Instrumento Para el Grado en Enfermería. Ph.D. Thesis, Universidad Complutense de Madrid, Madrid, Spain, 2013. [Google Scholar]
- O’Cathain, A.; Murphy, E.; Nicholl, J. The quality of mixed methods studies in health services research. J. Health Serv. Res. Policy 2008, 13, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ministerio de Ciencia e Innovación. Orden CIN/2134/2008, de 3 de Julio, Por la Que se Establecen los Requisitos Para la Verificación de los Títulos Universitarios Oficiales que Habiliten Para el Ejercicio de la Profesión de Enfermero. Madrid: Boletín Oficial del Estado no 174. 2008. Available online: https://www.boe.es/diario_boe/txt.php?id=BOE-A-2008-12388 (accessed on 1 May 2022).
- Gordon, M. Manual of Nursing Diagnosis; Jones &Bartlett: Burlington, MA, USA, 2016. [Google Scholar]
- Melander, L. Scenario Development in Transport Studies: Methodological Considerations and Reflections on Delphi studies. Futures 2018, 96, 68–78. [Google Scholar] [CrossRef]
- Meyer, C.L. How effectively are nurse educators preparing students to provide spiritual care? Nurse Educ. 2003, 28, 185–190. [Google Scholar] [CrossRef]
- Butcher, H.; Bulechek, G.; Dochterman, J.; Wagner, C. Nursing Interventions Classification (NIC), 7th ed.; Mosby: St. Louis, MO, USA, 2018. [Google Scholar]
- Hoffert, D.; Henshaw, C.; Mvududu, N. Enhancing the ability of nursing students to perform a spiritual assessment. Nurse Educ. 2007, 32, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Kalkim, A.; Sagkal Midilli, T.; Daghan, S. Nursing Students’ Perceptions of Spirituality and Spiritual Care and Their Spiritual Care Competencies. J. Hosp. Palliat. Nurs. 2018, 20, 286–295. [Google Scholar] [CrossRef]
- Crespo, A.; Gómez del Pulgar, M.; Hernández, S.; González, M.A.; Beneit, J.V. Agrupación de las Competencias del Enfermero Especialista en Enfermería del Trabajo Según el Proceso de Atención de Enfermería. Rev. Enfermería Del Trab. 2018, 8, 9–17. Available online: https://dialnet.unirioja.es/servlet/articulo?codigo=6536494 (accessed on 1 May 2022).
- Gómez del Pulgar García, M.; Pacheco del Cerro, E.; González Jurado, M.A.; Fernández, M.P.; Beneit Montesinos, J.V. Design and Content Validation of the “ECOEnf” Scale to Assess Nursing Competencies. Index Enfermería 2017, 26, 265–269. Available online: http://www.index-f.com/index-enfermeria/v26n4/11186.php (accessed on 1 May 2022).
- van Leeuwen, R.R.V.; Towards Nursing Competences in Spiritual care. University of Groningen. Available online: https://www.rug.nl/research/portal/files/14545572/c6.pdf (accessed on 1 May 2022).
- Taylor, E.J.; Testerman, N.; Hart, D. Teaching spiritual care to nursing students: An integrated model. J. Christ. Nurs. 2014, 31, 94–99. [Google Scholar] [CrossRef]
- González Aguña, A.; Fernández Batalla, M.; Gonzalo de Diego, B.; Jiménez Rodríguez, M.L.; Martínez Muñoz, M.L.; Santamaría García, J.M. Care Recommendations for the Chronic Risk of COVID-19: Nursing Intervention for Behaviour Changes. Int. J. Environ. Res. Public Health 2022, 19, 8532. [Google Scholar] [CrossRef]
- Mills, J.; Chapman, M. Compassion and self-compassion in medicine: Self-care for the caregivers. Am. Med. J. 2016, 9, 87–91. [Google Scholar] [CrossRef] [Green Version]
- Yazdani, M.; Rezaei, S.; Pahlavanzedeh, S. The effectiveness of stress management training program on depression, anxiety and stress of the nursing students. Iran. J. Nurs. Midwifery Res. 2010, 15, 208–215. [Google Scholar] [PubMed]
- Dobkin, P.; Hutchinson, T. Teaching mindfulness in medical school: Where are we now and where are we going? Med. Educ. 2013, 47, 768–779. [Google Scholar] [CrossRef] [PubMed]
- Hutchinson, T.A.; Dobkin, P. Mindful medical practise: Just another fad? Can. Fam. Physician 2009, 5, 778–779. [Google Scholar]
- Krasner, M.; Epstein, M.; Beckman, H.; Suchman, A. Association of an Educational Program in Mindful Communication with Burnout, Empathy, and Attitudes Among Primary Care Physicians. JAMA 2009, 302, 1284–1293. [Google Scholar] [CrossRef] [Green Version]
- Wilson, L.; Harper, D.C.; Tami Maury, I.; Zarate, R.; Salas, S.; Farley, J.; Warren, N.; Mendes, I.; Ventura, C. Global health competencies for nurses in the Americas. J. Prof. Nurs. 2012, 28, 213–222. [Google Scholar] [CrossRef]
| Code | Diagnostic Label |
|---|---|
| 00148 | Fear |
| 00124 | Hopelessness |
| 00066 | Spiritual distress |
| 00169 | Impaired religiosity |
| 00170 | Risk for impaired religiosity |
| 00054 | Risk for loneliness |
| 00147 | Death anxiety |
| 00120 | Situational low self-esteem |
| 00119 | Chronic low self-esteem |
| 00174 | Risk for compromised human dignity |
| 00214 | Impaired comfort |
| 00136 | Grieving |
| 00135 | Complicated grieving |
| 00172 | Risk for complicated grieving |
| 00121 | Readiness for enhanced hope |
| 00210 | Impaired resilience |
| 00175 | Moral distress |
| 00137 | Chronic sorrow |
| Age (Years) | Average (Range) | 51 (40–62) |
|---|---|---|
| Sex (n) | Female | 6 |
| Male | 1 | |
| Clinical Experience (years) | >15 | |
| Professional Profile (n) | Clinical | 1 |
| Teaching | 4 | |
| Management | 4 | |
| Research | 5 | |
| Academic Background (n) | PhD | 5 |
| Master | 2 | |
| Professional Experience (n) | Clinical | 7 |
| Teaching | 5 | |
| Management | 4 | |
| Research | 7 | |
| Teaching Experience (n) | Undergraduate | 5 |
| Post-graduate | 5 | |
| Other teaching experience | 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarrión-Bravo, J.A.; González-Aguña, A.; Abengózar-Muela, R.; Renghea, A.; Fernández-Batalla, M.; Santamaría-García, J.M.; Ruiz-Moral, R. Competence in Spiritual and Emotional Care: Learning Outcomes for the Evaluation of Nursing Students. Healthcare 2022, 10, 2062. https://doi.org/10.3390/healthcare10102062
Sarrión-Bravo JA, González-Aguña A, Abengózar-Muela R, Renghea A, Fernández-Batalla M, Santamaría-García JM, Ruiz-Moral R. Competence in Spiritual and Emotional Care: Learning Outcomes for the Evaluation of Nursing Students. Healthcare. 2022; 10(10):2062. https://doi.org/10.3390/healthcare10102062
Chicago/Turabian StyleSarrión-Bravo, Juan Antonio, Alexandra González-Aguña, Ricardo Abengózar-Muela, Alina Renghea, Marta Fernández-Batalla, José María Santamaría-García, and Roger Ruiz-Moral. 2022. "Competence in Spiritual and Emotional Care: Learning Outcomes for the Evaluation of Nursing Students" Healthcare 10, no. 10: 2062. https://doi.org/10.3390/healthcare10102062
APA StyleSarrión-Bravo, J. A., González-Aguña, A., Abengózar-Muela, R., Renghea, A., Fernández-Batalla, M., Santamaría-García, J. M., & Ruiz-Moral, R. (2022). Competence in Spiritual and Emotional Care: Learning Outcomes for the Evaluation of Nursing Students. Healthcare, 10(10), 2062. https://doi.org/10.3390/healthcare10102062







