Approaching Sarcopenic Obesity in Young and Middle-Aged Female Adults in Weight Management Settings: A Narrative Review
Abstract
:1. Introduction
2. Materials and Methods
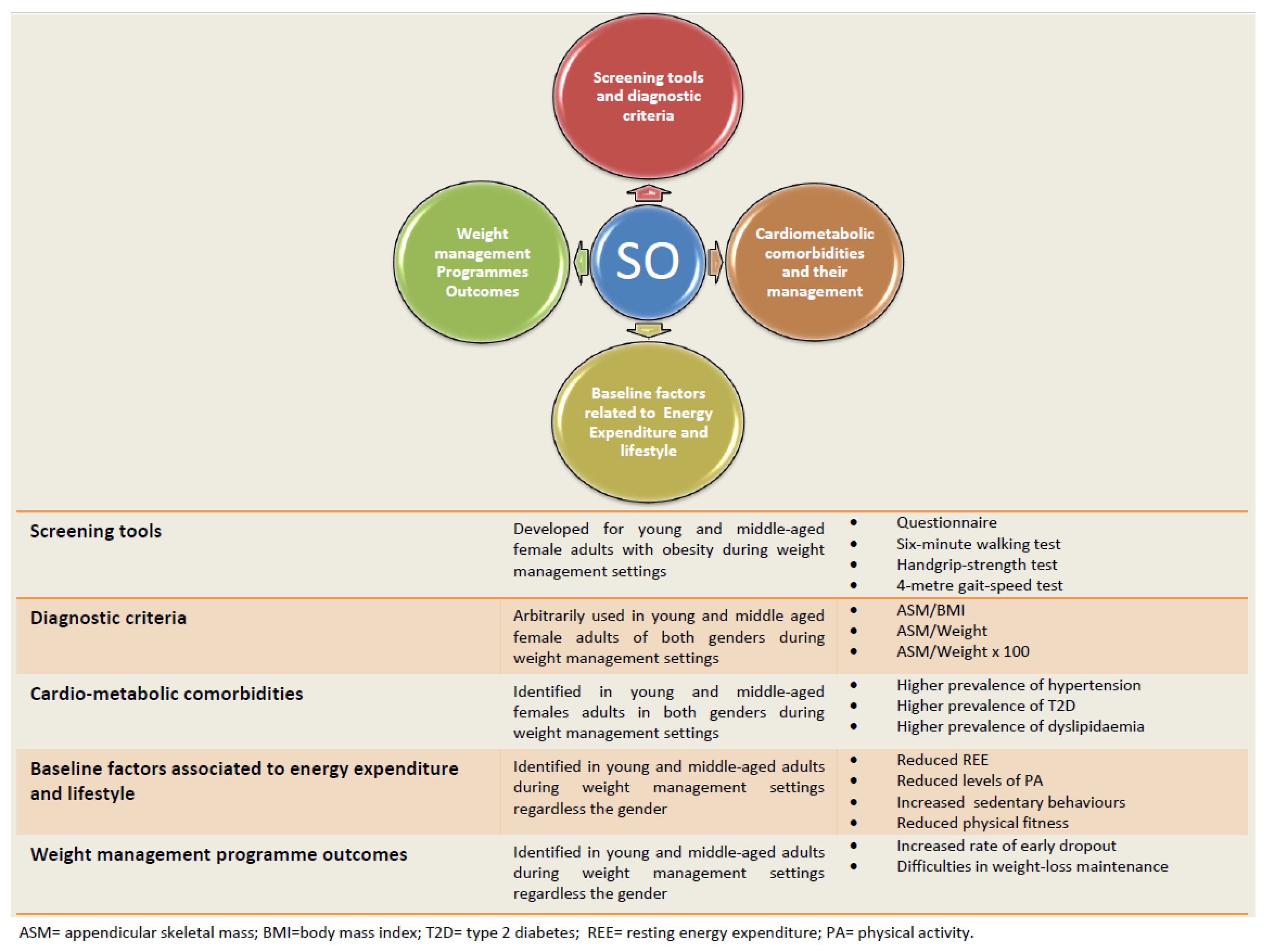
3. Results
3.1. Simple Tools for Screening Female Patients with Obesity at a Higher Risk of SO
- The six-minute walk test is usually performed to objectively evaluate functional exercise capacity and can serve as an index of patients’ daily activities. The test is performed along a straight corridor with a 30-m walking course. A brightly colored tape is used to mark the walking course every two meters, as well as the starting, end and turnaround points for each 60 m lap. Patients are instructed to walk as far as possible for six minutes and are allowed to stop or rest during the test if necessary. The participants’ respiratory rate and oxygen saturation are measured before the start and at the end of the test. The distance traveled is measured by counting the number of full laps. The cut-off point for screening for SO in this population is set at 470 m, with a sensitivity of 78% and specificity of 54% [13] (Table 1).
- The handgrip-strength test is performed to measure muscle strength using a calibrated dynamometer. The measure is usually taken on both hands and the maximum value (kg) is recorded. The cut-off point for screening for SO in this population is set at 23.5 kg, with a sensitivity of 77% and specificity of 61% [13] (Table 1).
- The 4-m gait-speed test is an objective measure of walking performance. It is usually performed on a flat course with 4 m marked out with tape. The participant is positioned with the toes just touching the start line and instructed to walk at their own pace. A stopwatch is started when the participant begins to move and stopped when the participant’s lead foot completely crosses the 4-m line. A cut-off point of 3.30 s has been identified for screening for SO in this population, with a sensitivity of 61% and specificity of 55% [13] (Table 1).
3.2. Accurate Assessment to Reject/Confirm a Diagnosis of SO
| Screening | Tool | Cut-Off for Females |
|---|---|---|
| Bissonnette et al. [12] | Questionnaire | ≥2.45 |
| El Ghoch et al. [13] | Six-minute walking test | 470 m |
| El Ghoch et al. [13] | Handgrip-strength test | 23.5 kg |
| El Ghoch et al. [13] | 4-meter gait-speed test | 3.30 s (gait speed = 1.2 m/s) |
| Diagnosis | ||
| Levine and Crimmins [23] | ASM/Weight × 100 | <19.43 |
| Oh et al. [24] | ASM/Weight × 100 | <23.4 |
| Batsis et al. [26] | ASM/BMI | <0.512 |
3.3. Management of SO-Related Comorbidities
3.4. SO and Weight Management Outcomes
- Early dropout: Defined as the interruption of the weight loss treatment and the main contributor to the failure of weight loss programs. The dropout rate can reach nearly 80% in some weight loss programs [39].
- Long-term weight loss maintenance (>12 months): Defined as intentional weight loss of at least 10% of body weight that is kept off for at least one year. Failure to maintain the weight lost during the weight loss phase, and a return to baseline body weight after three years of follow-up, is common regardless of the nature of the weight loss treatment and can occur in up to 70% of patients [40].
| First Author | Study Design | Sample | Mean Age | Mean BMI | Treatment Setting/Follow-Up | Outcome | Finding |
|---|---|---|---|---|---|---|---|
| El Ghoch et al. [13] | Cross-sectional study | N = 147 females (54 SO/93 Non SO) | 52.7 ± 12.5 years | 38.3 ± 6.7 kg/m2 | Inpatient and/or outpatient | Physical fitness | Significantly reduced in patients SO vs. Non SO. |
| Kreidieh et al. [36] | Cross-sectional study | N = 111 of both genders (55 SO/56 Non SO) | 37.12 ± 15.58 years | 36.27 ± 5.13 kg/m2 | Outpatient | Measured daily steps | SO group displayed significantly higher prevalence of inactivity (<5000 daily steps), and they had a lower mean number of daily steps than those in the group without SO. |
| Tannir et al. [37] | Cross-sectional study | N = 89 of both genders (39 SO/50 Non SO) | 40.62 ± 15.96 years | 34.93 ± 4.68 kg/m2 | Outpatient | REE | SO patients displayed a significantly lower REE/Weight than those in the group without SO. |
| Kreidieh et al. [41] | Longitudinal study | N = 103 of both genders (45 SO/58 Non SO) | 35.07 ± 26.44 years | 34.91 ± 6.81 kg/m2 | Outpatient—6-month follow-up | Early dropout rate | The presence of SO at baseline increases the risk of dropout at six months. |
| El Masri et al. [42] | Longitudinal study | N = 46 of both genders (21 SO/26 Non SO) | 44.25 ± 15.85 years | 35.71 ± 4.84 kg/m2 | Outpatient—6 and >12-month |
| At 6-month follow-up, patients with SO did not display a significant difference in terms of WL%, when compared to those without SO. After a longer term (i.e., >12 months), the WL% appeared to be significantly lower in the SO vs. non-SO |
4. Discussion
4.1. Findings
4.2. Clinical Implications
4.3. Strengths and Limitations
4.4. New Directions for Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Malafarina, V.; Uriz-Otano, F.; Iniesta, R.; Gil-Guerrero, L. Sarcopenia in the elderly: Diagnosis, physiopathology and treatment. Maturitas 2012, 71, 109–114. [Google Scholar] [CrossRef]
- Collaborators GBDO; Afshin, A.; Forouzanfar, M.H.; Reitsma, M.B.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [PubMed]
- Zamboni, M.; Mazzali, G.; Fantin, F.; Rossi, A.; Di Francesco, V. Sarcopenic obesity: A new category of obesity in the elderly. Nutr. Metab. Cardiovasc. Dis. 2008, 18, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Barazzoni, R.; Bischoff, S.C.; Boirie, Y.; Busetto, L.; Cederholm, T.; Dicker, D.; Toplak, H.; Van Gossum, A.; Yumuk, V.; Vettor, R. Sarcopenic obesity: Time to meet the challenge. Clin. Nutr. 2018, 11, 294–305. [Google Scholar]
- El Ghoch, M.; Calugi, S.; Dalle Grave, R. Sarcopenic Obesity: Definition, Health Consequences and Clinical Management. Open Nutr. J. 2018, 12, 70–73. [Google Scholar] [CrossRef]
- Batsis, J.A.; Cook, S.B. Is the whole not greater than the sum of its parts? The case of sarcopenic obesity. Am. J. Clin. Nutr. 2017, 106, 14–15. [Google Scholar] [CrossRef] [Green Version]
- Rossi, A.P.; Rubele, S.; Calugi, S.; Caliari, C.; Pedelini, F.; Soave, F.; Chignola, E.; Bazzani, P.V.; Mazzali, G.; Grave, R.D.; et al. Weight Cycling as a Risk Factor for Low Muscle Mass and Strength in a Population of Males and Females with Obesity. Obesity 2019, 7, 1068–1075. [Google Scholar] [CrossRef] [PubMed]
- Cooper, A.J.; Gupta, S.R.; Moustafa, A.F.; Chao, A. Sex/Gender Differences in Obesity Prevalence, Comorbidities, and Treatment. Curr. Obes. Rep. 2021, 10, 458–466. [Google Scholar] [CrossRef] [PubMed]
- Kreidieh, D.; Itani, L.; El Masri, D.; Tannir, H.; Citarella, R.; El Ghoch, M. Association between Sarcopenic Obesity, Type 2 Diabetes, and Hypertension in Overweight and Obese Treatment-Seeking Adult Women. J. Cardiovasc. Dev. Dis. 2018, 5, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Green, B.N.; Johnson, C.D.; Adams, A. Writing narrative literature reviews for peer-reviewed journals: Secrets of the trade. J. Sport. Chiropr. Rehabil. 2001, 15, 5–19. [Google Scholar] [CrossRef] [Green Version]
- Narrative Review Checklist. Available online: https://www.elsevier.com/__data/promis_misc/ANDJNarrativeReviewChecklistpdf (accessed on 1 September 2022).
- Bissonnette, D.J.; Burk, B.N.; Hadley, M.; Knoblich, P. Pilot study for the development of a screening questionnaire to detect sarcopenic obesity. Int. J. Obes. 2022, 46, 1328–1331. [Google Scholar] [CrossRef] [PubMed]
- El Ghoch, M.; Rossi, A.P.; Calugi, S.; Rubele, S.; Soave, F.; Zamboni, M.; Chignola, E.; Mazzali, G.; Bazzani, P.V.; Dalle Grave, R. Physical performance measures in screening for reduced lean body mass in adult females with obesity. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Donini, L.M.; Busetto, L.; Bischoff, S.C.; Cederholm, T.; Ballesteros-Pomar, M.D.; Batsis, J.A.; Bauer, J.M.; Boirie, Y.; Cruz-Jentoft, A.J.; Dicker, D.; et al. Definition and Diagnostic Criteria for Sarcopenic Obesity: ESPEN and EASO Consensus Statement. Obes. Facts 2022, 15, 321–335. [Google Scholar] [CrossRef] [PubMed]
- Stenholm, S.; Harris, T.B.; Rantanen, T.; Visser, M.; Kritchevsky, S.B.; Ferrucci, L. Sarcopenic obesity: Definition, cause and consequences. Curr. Opin. Clin. Nutr. Metab. Care 2008, 11, 693–700. [Google Scholar] [CrossRef] [Green Version]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [Green Version]
- Fielding, R.A.; Vellas, B.; Evans, W.J.; Bhasin, S.; Morley, J.E.; Newman, A.B.; Abellan van Kan, G.; Andrieu, S.; Bauer, J.; Breuille, D.; et al. Sarcopenia: An undiagnosed condition in older adults. Current consensus definition: Prevalence, etiology, and consequences. International working group on sarcopenia. J. Am. Med. Dir. Assoc. 2011, 12, 249–256. [Google Scholar] [CrossRef] [Green Version]
- Chen, L.K.; Liu, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Bahyah, K.S.; Chou, M.Y.; Chen, L.Y.; Hsu, P.S.; Krairit, O.; et al. Sarcopenia in Asia: Consensus report of the Asian Working Group for Sarcopenia. J. Am. Med. Dir. Assoc. 2014, 15, 95–101. [Google Scholar] [CrossRef]
- Johnson Stoklossa, C.A.; Sharma, A.M.; Forhan, M.; Siervo, M.; Padwal, R.S.; Prado, C.M. Prevalence of Sarcopenic Obesity in Adults with Class II/III Obesity Using Different Diagnostic Criteria. J. Nutr. Metab. 2017, 2017, 7307618. [Google Scholar] [CrossRef]
- Bouchard, D.R.; Dionne, I.J.; Brochu, M. Sarcopenic/obesity and physical capacity in older men and women: Data from the Nutrition as a Determinant of Successful Aging (NuAge)-the Quebec longitudinal Study. Obesity 2009, 17, 2082–2088. [Google Scholar] [CrossRef]
- Poggiogalle, E.; Lubrano, C.; Sergi, G.; Coin, A.; Gnessi, L.; Mariani, S.; Lenzi, A.; Donini, L. Sarcopenic Obesity and Metabolic Syndrome in Adult Caucasian Subjects. J. Nutr. Health Aging 2016, 20, 958–963. [Google Scholar] [CrossRef]
- Zoico, E.; Di Francesco, V.; Guralnik, J.M.; Mazzali, G.; Bortolani, A.; Guariento, S.; Sergi, G.; Bosello, O.; Zamboni, M. Physical disability and muscular strength in relation to obesity and different body composition indexes in a sample of healthy elderly women. Int. J. Obes. Relat. Metab. Disord. 2004, 28, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Levine, M.E.; Crimmins, E.M. The impact of insulin resistance and inflammation on the association between sarcopenic obesity and physical functioning. Obesity 2012, 20, 2101–2106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oh, C.; Jho, S.; No, J.K.; Kim, H.S. Body composition changes were related to nutrient intakes in elderly men but elderly women had a higher prevalence of sarcopenic obesity in a population of Korean adults. Nutr. Res. 2015, 35, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.N.; Yang, S.J.; Yoo, H.J.; Lim, K.I.; Kang, H.J.; Song, W.; Seo, J.A.; Kim, S.G.; Kim, N.H.; Baik, S.H.; et al. Prevalence of sarcopenia and sarcopenic obesity in Korean adults: The Korean sarcopenic obesity study. Int. J. Obes. 2009, 33, 885–892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Batsis, J.; Mackenzie, T.A.; Lopez-Jimenez, F.; Bartels, S.J. Prevalence of sarcopenic obesity using FNIH criteria in the US population: NHANES 1999–2004. In The Gerontological Society of America; Oxford University Press Inc.: Oxford, MI, USA, 2015. [Google Scholar]
- Bouchonville, M.F.; Villareal, D.T. Sarcopenic obesity: How do we treat it? Curr. Opin. Endocrinol. Diabetes Obes. 2013, 20, 412–419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atkins, J.L.; Wannamethee, S.G. The effect of sarcopenic obesity on cardiovascular disease and all-cause mortality in older people. Rev. Clin. Gerontol. 2015, 25, 86–97. [Google Scholar] [CrossRef]
- Khadra, D.; Itani, L.; Tannir, H.; Kreidieh, D.; El Masri, D.; El Ghoch, M. Association between sarcopenic obesity and higher risk of type 2 diabetes in adults: A systematic review and meta-analysis. World J. Diabetes 2019, 10, 311–323. [Google Scholar] [CrossRef]
- Srikanthan, P.; Hevener, A.L.; Karlamangla, A.S. Sarcopenia exacerbates obesity-associated insulin resistance and dysglycemia: Findings from the National Health and Nutrition Examination Survey III. PLoS ONE 2010, 5, e10805. [Google Scholar] [CrossRef]
- Solem, R.C. Limitation of a cross-sectional study. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 205. [Google Scholar] [CrossRef] [Green Version]
- Muscogiuri, G.; Barrea, L.; Caprio, M.; Ceriani, F.; Chavez, A.O.; El Ghoch, M.; Frias-Toral, E.; Mehta, R.J.; Mendez, V.; Paschou, S.A.; et al. Nutritional guidelines for the management of insulin resistance. Crit. Rev. Food Sci. Nutr. 2021, 62, 6947–6960. [Google Scholar] [CrossRef]
- Barrea, L.; Vetrani, C.; Caprio, M.; El Ghoch, M.; Frias-Toral, E.; Mehta, R.J.; Mendez, V.; Moriconi, E.; Paschou, S.A.; Pazderska, A.; et al. Nutritional management of type 2 diabetes in subjects with obesity: An international guideline for clinical practice. Crit. Rev. Food. Sci. Nutr. 2021, 1–13. [Google Scholar] [CrossRef]
- Brinks, J.; Fowler, A.; Franklin, B.A.; Dulai, J. Lifestyle Modification in Secondary Prevention: Beyond Pharmacotherapy. Am. J. Lifestyle Med. 2016, 11, 137–152. [Google Scholar] [CrossRef]
- Muller, M.J.; Enderle, J.; Bosy-Westphal, A. Changes in Energy Expenditure with Weight Gain and Weight Loss in Humans. Curr. Obes. Rep. 2016, 5, 413–423. [Google Scholar] [CrossRef] [Green Version]
- Kreidieh, D.; Itani, L.; El Masri, D.; Tannir, H.; El Ghoch, M. Association Between Reduced Daily Steps and Sarcopenic Obesity in Treatment-Seeking Adults With Obesity. Front. Endocrinol. 2020, 11, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tannir, H.; Kreidieh, D.; Itani, L.; El Masri, D.; El Ghoch, M. Reduction of Resting Energy Expenditure and Sarcopenic Obesity in Adults with Overweight and Obesity: A Brief Report. Curr. Diabetes Rev. 2020, 16, 376–380. [Google Scholar] [CrossRef]
- Mastino, D.; Robert, M.; Betry, C.; Laville, M.; Gouillat, C.; Disse, E. Bariatric Surgery Outcomes in Sarcopenic Obesity. Obes. Surg. 2016, 26, 2355–2362. [Google Scholar] [CrossRef]
- Moroshko, I.; Brennan, L.; O’Brien, P. Predictors of dropout in weight loss interventions: A systematic review of the literature. Obes. Rev. 2011, 12, 912–934. [Google Scholar] [CrossRef] [PubMed]
- MacLean, P.S.; Wing, R.R.; Davidson, T.; Epstein, L.; Goodpaster, B.; Hall, K.D.; Levin, B.E.; Perri, M.G.; Rolls, B.J.; Rosenbaum, M.; et al. NIH working group report: Innovative research to improve maintenance of weight loss. Obesity 2015, 23, 7–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kreidieh, D.; Itani, L.; Tannir, H.; El Masri, D.; El Ghoch, M. Sarcopenic Obesity Predicts Early Attrition in Treatment-Seeking Patients with Obesity: A Longitudinal Pilot Study. J. Cardiovasc. Dev. Dis. 2020, 7, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El Masri, D.; Itani, L.; Tannir, H.; Kreidieh, D.; El Ghoch, M. The Relationship between Sarcopenic Obesity, Weight-Loss and Maintenance Outcomes during Obesity Management: Are Additional Strategies Required? Clin. Pract. 2021, 11, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Ji, T.; Li, Y.; Ma, L. Sarcopenic Obesity: An Emerging Public Health Problem. Aging Dis. 2022, 13, 379–388. [Google Scholar] [PubMed]
- Petersen, K.S.; Flock, M.R.; Richter, C.K.; Mukherjea, R.; Slavin, J.L.; Kris-Etherton, P.M. Healthy Dietary Patterns for Preventing Cardiometabolic Disease: The Role of Plant-Based Foods and Animal Products. Curr. Dev. Nutr. 2017, 1, cdn.117.001289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Varkevisser, R.D.M.; van Stralen, M.M.; Kroeze, W.; Ket, J.C.F.; Steenhuis, I.H.M. Determinants of weight loss maintenance: A systematic review. Obes. Rev. 2019, 20, 171–211. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pellegrini, M.; Itani, L.; Rossi, A.P.; Kreidieh, D.; El Masri, D.; Tannir, H.; El Ghoch, M. Approaching Sarcopenic Obesity in Young and Middle-Aged Female Adults in Weight Management Settings: A Narrative Review. Healthcare 2022, 10, 2042. https://doi.org/10.3390/healthcare10102042
Pellegrini M, Itani L, Rossi AP, Kreidieh D, El Masri D, Tannir H, El Ghoch M. Approaching Sarcopenic Obesity in Young and Middle-Aged Female Adults in Weight Management Settings: A Narrative Review. Healthcare. 2022; 10(10):2042. https://doi.org/10.3390/healthcare10102042
Chicago/Turabian StylePellegrini, Massimo, Leila Itani, Andrea P. Rossi, Dima Kreidieh, Dana El Masri, Hana Tannir, and Marwan El Ghoch. 2022. "Approaching Sarcopenic Obesity in Young and Middle-Aged Female Adults in Weight Management Settings: A Narrative Review" Healthcare 10, no. 10: 2042. https://doi.org/10.3390/healthcare10102042
APA StylePellegrini, M., Itani, L., Rossi, A. P., Kreidieh, D., El Masri, D., Tannir, H., & El Ghoch, M. (2022). Approaching Sarcopenic Obesity in Young and Middle-Aged Female Adults in Weight Management Settings: A Narrative Review. Healthcare, 10(10), 2042. https://doi.org/10.3390/healthcare10102042









