Comparison of Iris-Claw Phakic Lens Implant versus Corneal Laser Techniques in High Myopia: A Five-Year Follow-Up Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
2.2. Data Collection
2.3. Description of the Surgical Techniques
2.4. Definition of Effectiveness and Safety Indexes
2.5. Statistical Analyses and Review Board Approval
3. Results
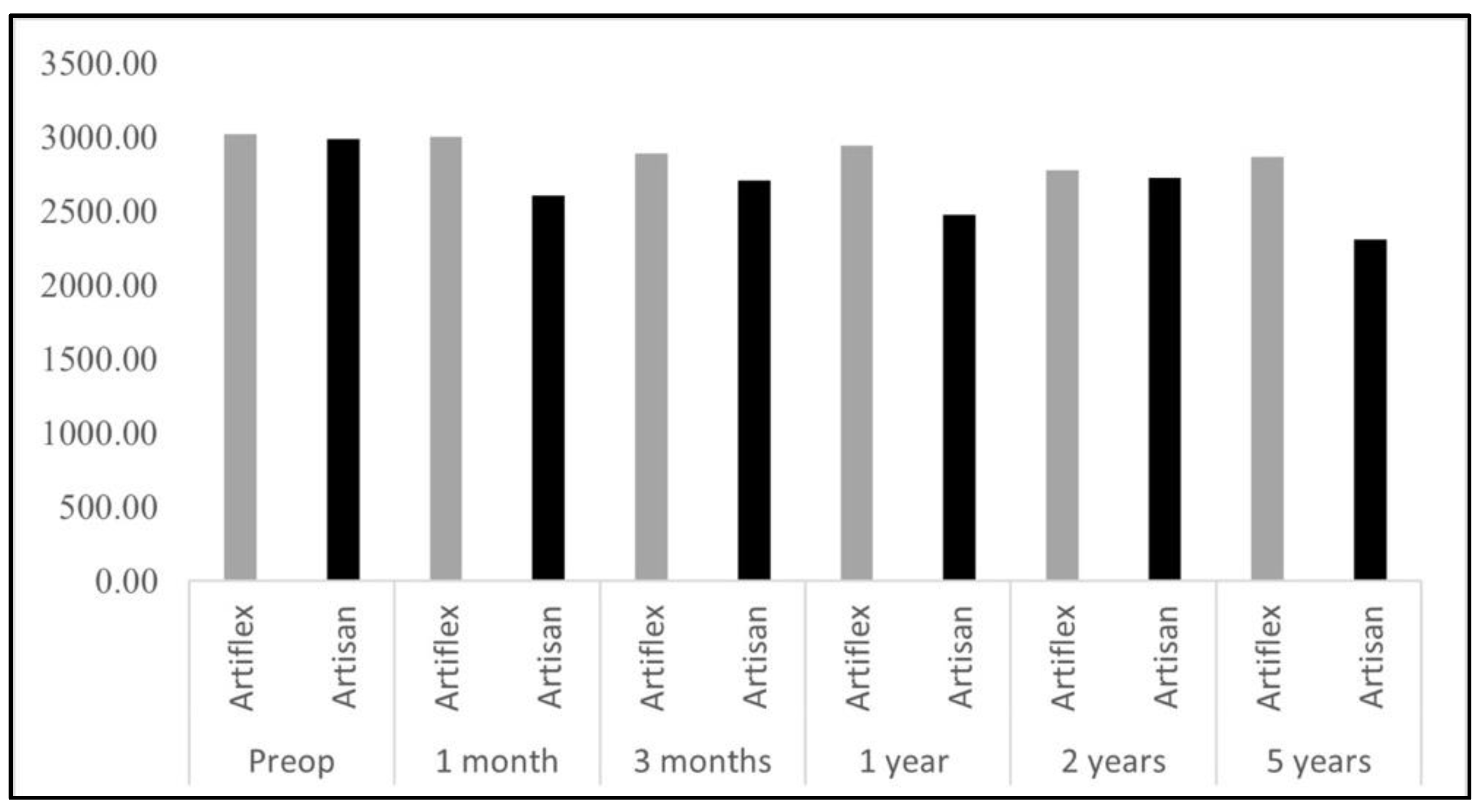
3.1. Descriptives and Comparisons between Surgical Techniques
3.2. Linear Regression Model
3.3. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Brien Holden Vision Institute Global Scientific Meeting on Myopia the Impact of Myopia and High Myopia; Report of the Joint World Health Organization; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Li, M.; Zhai, L.; Zeng, S.; Peng, Q.; Wang, J.; Deng, Y.; Xie, L.; He, Y.; Li, T. Lack of Association between LUM Rs3759223 Polymorphism and High Myopia. Optom. Vis. Sci. 2014, 91, 707–712. [Google Scholar] [CrossRef] [PubMed]
- Chang, L.; Pan, C.W.; Ohno-Matsui, K.; Lin, X.; Cheung, G.C.M.; Gazzard, G.; Koh, V.; Hamzah, H.; Tai, E.S.; Lim, S.C.; et al. Myopia-Related Fundus Changes in Singapore Adults with High Myopia. Am. J. Ophthalmol. 2013, 155, 991–999.e1. [Google Scholar] [CrossRef] [PubMed]
- Chuck, R.S.; Jacobs, D.S.; Lee, J.K.; Afshari, N.A.; Vitale, S.; Shen, T.T.; Keenan, J.D. Refractive Errors & Refractive Surgery Preferred Practice Pattern®. Ophthalmology 2018, 125, P1–P104. [Google Scholar] [CrossRef] [PubMed]
- Moriyama, M.; Ohno-Matsui, K.; Hayashi, K.; Shimada, N.; Yoshida, T.; Tokoro, T.; Morita, I. Topographic Analyses of Shape of Eyes with Pathologic Myopia by High-Resolution Three-Dimensional Magnetic Resonance Imaging. Ophthalmology 2011, 118, 1626–1637. [Google Scholar] [CrossRef]
- Ohno-Matsui, K. What Is the Fundamental Nature of Pathologic Myopia? Retina 2017, 37, 1043–1048. [Google Scholar] [CrossRef]
- Ohno-Matsui, K.; Lai, T.Y.Y.; Lai, C.C.; Cheung, C.M.G. Updates of Pathologic Myopia. Prog. Retin. Eye Res. 2016, 52, 156–187. [Google Scholar] [CrossRef]
- Ohno-Matsui, K.; Kawasaki, R.; Jonas, J.B.; Cheung, C.M.G.; Saw, S.M.; Verhoeven, V.J.M.; Klaver, C.C.W.; Moriyama, M.; Shinohara, K.; Kawasaki, Y.; et al. International Photographic Classification and Grading System for Myopic Maculopathy. Am. J. Ophthalmol. 2015, 159, 877–883.e7. [Google Scholar] [CrossRef]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.J.; Resnikoff, S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef]
- Kanthan, G.L.; Mitchell, P.; Rochtchina, E.; Cumming, R.G.; Wang, J.J. Myopia and the Long-Term Incidence of Cataract and Cataract Surgery: The Blue Mountains Eye Study. Clin. Exp. Ophthalmol. 2014, 42, 347–353. [Google Scholar] [CrossRef]
- Ikuno, Y. Overview of the Complications of High Myopia. Retina 2017, 37, 2347–2351. [Google Scholar] [CrossRef]
- Barrio, M. Icare Phakic Lens: Refractive Results, Surgical Technique, and Complications. 2013. Available online: https://eprints.ucm.es/id/eprint/22434/1/T34690.pdf (accessed on 10 August 2022).
- Kohnen, T.; Maxwell, W.A.; Holland, S. Correction of Moderate to High Myopia with a Foldable, Angle-Supported Phakic Intraocular Lens: Results from a 5-Year Open-Label Trial. Ophthalmology 2016, 123, 1027–1035. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Castillo, V.; Elies, D.; Boixadera, A.; García-Arumí, J.; Mauricio, J.; Cavero, L.; Coret, A. Silicone Posterior Chamber Phakic Intraocular Lens Dislocated into the Vitreous Cavity. J. Refract. Surg. 2004, 20, 773–777. [Google Scholar] [CrossRef] [PubMed]
- Vukich, J.A.; Duehr, D.; Sanders, D.R.; Doney, K.; Barnett, R.; Dulaney, D.; Perkins, S.; Rowen, S.L.; Steel, D.; Berkeley, R.; et al. U.S. Food and Drug Administration Clinical Trial of the Implantable Contact Lens for Moderate to High Myopia. Ophthalmology 2003, 110, 255–266. [Google Scholar] [CrossRef]
- Gimbel, H.V.; Ziémba, S.L. Management of Myopic Astigmatism with Phakic Intraocular Lens Implantation. J. Cataract Refract. Surg. 2002, 28, 883–886. [Google Scholar] [CrossRef]
- Dejaco-Ruhswurm, I.; Scholz, U.; Pieh, S.; Hanselmayer, G.; Lackner, B.; Italon, C.; Ploner, M.; Skorpik, C. Long-Term Endothelial Changes in Phakic Eyes with Posterior Chamber Intraocular Lenses. J. Cataract Refract. Surg. 2002, 28, 1589–1593. [Google Scholar] [CrossRef]
- ICL in Treatment of Myopia (ITM) Study Group. United States Food and Drug Administration Clinical Trial of the Implantable Collamer Lens (ICL) for Moderate to High Myopia: Three-Year Follow-Up. Ophthalmology 2004, 111, 1683–1692. [Google Scholar] [CrossRef]
- Kamiya, K.; Shimizu, K.; Igarashi, A.; Hikita, F.; Komatsu, M. Four-Year Follow-up of Posterior Chamber Phakic Intraocular Lens Implantation for Moderate to High Myopia. Arch. Ophthalmol. 2009, 127, 845–850. [Google Scholar]
- Doors, M.; Cals, D.W.J.K.; Berendschot, T.T.J.M.; de Brabander, J.; Hendrikse, F.; Webers, C.A.B.; Nuijts, R.M.M.A. Influence of Anterior Chamber Morphometrics on Endothelial Cell Changes after Phakic Intraocular Lens Implantation. J. Cataract Refract. Surg. 2008, 34, 2110–2118. [Google Scholar] [CrossRef]
- Menezo, J.L.; Peris-Martínez, C.; Cisneros, A.L.; Martínez-Costa, R. Phakic Intraocular Lenses to Correct High Myopia: Adatomed, Staar, and Artisan. J. Cataract Refract. Surg. 2004, 30, 33–44. [Google Scholar] [CrossRef]
- Alio, J.L.; Ismael, M.M.; Artola, A. Laser Epithelium Removal before Photorefractive Keratectomy. Refract. Corneal Surg. 1993, 9, 395. [Google Scholar] [CrossRef]
- Stern, D.; Puliafito, C.A.; Dobi, E.T.; Schoenlein, R.W.; Fujimoto, J.G.; Birngruber, R. Corneal Ablation by Nanosecond, Picosecond, and Femtosecond Lasers at 532 and 625 Nm. Arch. Ophthalmol. 1989, 107, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Ophtec Inc.; Groningen, N. Refractive Surgery Instruments. Available online: https://www.ophtec.com/products/refractive-surgery/instruments (accessed on 31 July 2022).
- Stulting, R.D.; John, M.E.; Maloney, R.K.; Assil, K.K.; Arrowsmith, P.N.; Thompson, V.M. Three-Year Results of Artisan/Verisyse Phakic Intraocular Lens Implantation: Results of the United States Food and Drug Administration Clinical Trial. Ophthalmology 2008, 115, 464–472.e1. [Google Scholar] [CrossRef] [PubMed]
- Gershoni, A.; Mimouni, M.; Livny, E.; Bahar, I. Z-LASIK and Trans-PRK for Correction of High-Grade Myopia: Safety, Efficacy, Predictability and Clinical Outcomes. Int. Ophthalmol. 2019, 39, 753–763. [Google Scholar] [CrossRef] [PubMed]
- van Gelder, R.N.; Steger-May, K.; Yang, S.H.; Rattanatam, T.; Pepose, J.S. Comparison of Photorefractive Keratectomy, Astigmatic PRK, Laser in Situ Keratomileusis, and Astigmatic LASIK in the Treatment of Myopia. J. Cataract Refract. Surg. 2002, 28, 462–476. [Google Scholar] [CrossRef]
- Hashemi, H.; Miraftab, M.; Ghaffari, R.; Asgari, S. Femtosecond-Assisted LASIK versus PRK: Comparison of 6-Month Visual Acuity and Quality Outcome for High Myopia. Eye Contact Lens 2016, 42, 354–357. [Google Scholar] [CrossRef]
- Hersh, P.S.; Brint, S.F.; Maloney, R.K.; Durrie, D.S.; Gordon, M.; Michelson, M.A.; Thompson, V.M.; Berkeley, R.B.; Schein, O.D.; Steinert, R.F. Photorefractive Keratectomy versus Laser in Situ Keratomileusis for Moderate to High Myopia: A Randomized Prospective Study. Ophthalmology 1998, 105, 1512–1523. [Google Scholar] [CrossRef]
- Sorkin, N.; Rosenblatt, A.; Smadja, D.; Cohen, E.; Santhiago, M.R.; Varssano, D.; Yatziv, Y. Early Refractive and Clinical Outcomes of High-Myopic Photorefractive Keratectomy as an Alternative to LASIK Surgery in Eyes with High Preoperative Percentage of Tissue Altered. J. Ophthalmol. 2019, 2019, 6513143. [Google Scholar] [CrossRef]
- Wen, D.; McAlinden, C.; Flitcroft, I.; Tu, R.; Wang, Q.; Alió, J.; Marshall, J.; Huang, Y.; Song, B.; Hu, L.; et al. Postoperative Efficacy, Predictability, Safety, and Visual Quality of Laser Corneal Refractive Surgery: A Network Meta-Analysis. Am. J. Ophthalmol. 2017, 178, 65–78. [Google Scholar] [CrossRef]
- Dick, H.B.; Budo, C.; Malecaze, F.; Güell, J.L.; Marinho, A.A.P.; Nuijts, R.M.M.A.; Luyten, G.P.M.; Menezo, J.L.; Kohnen, T. Foldable Artiflex Phakic Intraocular Lens for the Correction of Myopia: Two-Year Follow-up Results of a Prospective European Multicenter Study. Ophthalmology 2009, 116, 671–677. [Google Scholar] [CrossRef]
- Ozertürk, Y.; Kubaloglu, A.; Sari, E.S.; Koytak, A.; Capkin, M.; Akçay, L.; Evcili, P.S. Foldable Iris-Fixated Phakic Intraocular Lens Implantation for the Correction of Myopia: Two Years of Follow-Up. Indian J. Ophthalmol. 2012, 60, 23. [Google Scholar] [CrossRef]
- Cakir, I.; Demir, G.; Yildiz, B.K.; Öcal, M.C.; Yildirim, Y.; Agca, A. Efficacy and Safety of Iris-Supported Phakic Lenses (Verisyse) for the Treatment of High Myopia: 5-Year Results. Int. Ophthalmol. 2021, 41, 2837–2845. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, T.; Correia, F.F.; Franqueira, N.; Mendes, J.C.; Pinto, C.; Vaz, F. Long-Term Efficacy and Safety Results after Iris-Fixated Foldable Phakic Intraocular Lens for Myopia and Astigmatism: 6-Year Follow-Up. J. Cataract Refract. Surg. 2021, 47, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Charters, L. Iris-Fixated IOLs Are a Boon for Treating High Myopia. Ophthalmol. Times 2021, 46. [Google Scholar]
- Hashemi, H.; Miraftab, M.; Asgari, S. Comparison of the Visual Outcomes between PRK-MMC and Phakic IOL Implantation in High Myopic Patients. Eye 2014, 28, 1113–1118. [Google Scholar] [CrossRef][Green Version]
- Miraftab, M.; Hashemi, H.; Asgari, S. Matched Optical Quality Comparison of 3-Year Results of PRK–MMC and Phakic IOL Implantation in the Correction of High Myopia. Eye 2015, 29, 926–931. [Google Scholar] [CrossRef][Green Version]
- Wu, Q.; Li, Y.; Tang, L.; Wu, L.A.; Wang, C.Y.; Park, C.Y. Comparison of Rigid versus Foldable Iris-Fixed Phakic Intraocular Lens Implantation for High Myopia: A Systematic Review and Meta-Analysis. Medicine 2020, 99, e19030. [Google Scholar] [CrossRef] [PubMed]
- Yuan, X.; Ping, H.Z.; Hong, W.C.; Yin, D.; Ting, Z. Five-Year Follow-up after Anterior Iris-Fixated Intraocular Lens Implantation in Phakic Eyes to Correct High Myopia. Eye 2011, 26, 321–326. [Google Scholar] [CrossRef][Green Version]
- Martínez-Plaza, E.; López-Miguel, A.; Holgueras, A.; Barraquer, R.I.; Alió, J.L.; Maldonado, M.J. Phakic Intraocular Lenses: Recent Advances and Innovations. Arch. De La Soc. Española De Oftalmol. (Engl. Ed.) 2020, 95, 178–187. [Google Scholar] [CrossRef]
- Morral i Palau, M.; García-Arumí, J.; Guell Villanueva, J.L. Intraocular Lenses for the Phakic Eye with an Iridian Fixation for the Correction of Refractive Errors. 2009. Available online: https://www.tdx.cat/bitstream/handle/10803/4347/mmp1de1.pdf (accessed on 10 August 2022).
| N | Mean | SD * | 95% Confidence Interval | |||
|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | |||||
| Efficacy 1 month | PRK | 245 | 0.69 | 0.35 | 0.65 | 0.73 |
| FS-Lasik | 284 | 0.84 | 0.38 | 0.79 | 0.88 | |
| Artiflex | 70 | 1.03 | 0.59 | 0.89 | 1.18 | |
| Artisan | 5 | 0.88 | 0.49 | 0.28 | 1.48 | |
| Efficacy 3 months | PRK | 243 | 0.83 | 0.36 | 0.78 | 0.88 |
| FS-Lasik | 273 | 0.95 | 0.38 | 0.91 | 1 | |
| Artiflex | 71 | 1.07 | 0.48 | 0.94 | 1.19 | |
| Artisan | 6 | 0.97 | 0.45 | 0.50 | 1.44 | |
| Efficacy 1 year | PRK | 236 | 0.86 | 0.33 | 0.82 | 0.91 |
| FS-Lasik | 253 | 1.00 | 0.69 | 0.91 | 1.08 | |
| Artiflex | 53 | 1.15 | 0.44 | 1.02 | 1.27 | |
| Artisan | 8 | 1.30 | 0.35 | 1.01 | 1.59 | |
| Efficacy 2 year | PRK | 229 | 0.91 | 0.35 | 0.87 | 0.96 |
| FS-Lasik | 249 | 0.93 | 0.41 | 0.88 | 0.98 | |
| Artiflex | 24 | 1.16 | 0.37 | 1.00 | 1.31 | |
| Artisan | 4 | 0.91 | 0.56 | 0.01 | 1.81 | |
| Efficacy 5 year | PRK | 241 | 0.82 | 0.42 | 0.77 | 0.87 |
| FS-Lasik | 252 | 0.86 | 0.46 | 0.81 | 0.92 | |
| Artiflex | 35 | 1.10 | 0.24 | 1.01 | 1.18 | |
| Artisan | 2 | 1.40 | 0.10 | 0.46 | 2.33 | |
| Mean Differences | SD ** | p-Value | |||
|---|---|---|---|---|---|
| PRK | FS-Lasik | −0.15 * | 0.03 | <0.01 | |
| Artiflex | −0.34 * | 0.08 | <0.01 | ||
| Efficacy 1 month | Artisan | −0.19 | 0.22 | 1.000 | |
| FS-Lasik | Artiflex | −0.19 | 0.08 | 0.120 | |
| Artisan | −0.04 | 0.22 | 1.000 | ||
| Artiflex | Artisan | 0.15 | 0.23 | 1.000 | |
| PRK | FS-Lasik | −0.12 * | 0.03 | <0.01 | |
| Artiflex | −0.24 * | 0.06 | <0.01 | ||
| Efficacy 3 months | Artisan | −0.14 | 0.18 | 1.000 | |
| FS-Lasik | Artiflex | −0.11 | 0.06 | 0.560 | |
| Artisan | −0.02 | 0.18 | 1.000 | ||
| Artiflex | Artisan | 0.09 | 0.19 | 1.000 | |
| PRK | FS-Lasik | −0.13 | 0.05 | 0.060 | |
| Artiflex | −0.28 * | 0.07 | <0.01 | ||
| Artisan | −0.43 | 0.13 | 0.090 | ||
| Efficacy 1 year | Fs-Lasik | Artiflex | −0.15 | 0.08 | 0.410 |
| Artisan | −0.30 | 0.13 | 0.390 | ||
| Artiflex | Artisan | −0.15 | 0.14 | 0.970 | |
| PRK | FS-Lasik | −0.04 | 0.04 | 0.960 | |
| Artiflex | −0.28 * | 0.05 | <0.01 | ||
| Efficacy 5 year | Artisan | −0.58 | 0.08 | 0.410 | |
| FS-Lasik | Artiflex | −0.23 * | 0.05 | <0.01 | |
| Artisan | −0.53 | 0.08 | 0.430 | ||
| Artiflex | Artisan | −0.30 | 0.09 | 0.580 | |
| Mean | SD * | Standard Error | 95% Confidence Interval | |||
|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | |||||
| Safety 1 month | PRK | 0.90 | 0.32 | 0.02 | 0.86 | 0.94 |
| FS-Lasik | 1.09 | 0.34 | 0.02 | 1.05 | 1.13 | |
| Artiflex | 1.24 | 0.55 | 0.08 | 1.08 | 1.41 | |
| Artisan | 1.58 | 0.19 | 0.11 | 1.11 | 2.05 | |
| Total | 1.03 | 0.37 | 0.02 | 1.00 | 1.06 | |
| Safety 3 months | PRK | 1.03 | 0.35 | 0.02 | 0.98 | 1.07 |
| FS-Lasik | 1.16 | 0.38 | 0.02 | 1.11 | 1.20 | |
| Artiflex | 1.25 | 0.58 | 0.09 | 1.07 | 1.44 | |
| Artisan | 1.46 | 0.24 | 0.11 | 1.16 | 1.76 | |
| Total | 1.11 | 0.39 | 0.02 | 1.08 | 1.14 | |
| Safety 1 year | PRK | 1.07 | 0.36 | 0.02 | 1.02 | 1.11 |
| FS-Lasik | 1.22 | 0.67 | 0.04 | 1.14 | 1.30 | |
| Artiflex | 1.14 | 0.20 | 0.04 | 1.06 | 1.23 | |
| Artisan | 1.19 | 0.36 | 0.12 | 0.91 | 1.47 | |
| Total | 1.15 | 0.53 | 0.02 | 1.10 | 1.19 | |
| Safety 2 year | PRK | 1.10 | 0,4 | 0.03 | 1.05 | 1.15 |
| FS-Lasik | 1.20 | 0.44 | 0.03 | 1.14 | 1.25 | |
| Artiflex | 1.14 | 0.20 | 0.05 | 1.03 | 1.24 | |
| Artisan | 1.37 | 0.14 | 0.06 | 1.20 | 1.54 | |
| Total | 1.15 | 0.42 | 0.02 | 1.12 | 1.19 | |
| Safety 5 year | PRK | 1.14 | 0.39 | 0.02 | 1.10 | 1.19 |
| FS-Lasik | 1.24 | 0.50 | 0.03 | 1.18 | 1.30 | |
| Artiflex | 1.1 | 0.30 | 0.09 | 0.90 | 1.30 | |
| Artisan | 1.24 | 0.22 | 0.13 | 0.68 | 1.79 | |
| Total | 1.19 | 0.45 | 0.02 | 1.16 | 1.23 | |
| Mean Differences | SD * | p-Value | |||
|---|---|---|---|---|---|
| PRK | FS-Lasik | −0.18 | 0.03 | <0.01 | |
| Artiflex | −0.34 | 0.09 | <0.01 | ||
| Artisan | −0.68 | 0.11 | 0.200 | ||
| Safety 1 month | FS-Lasik | Artiflex | −0.16 | 0.09 | 0.530 |
| Artisan | −0.49 | 0.11 | 0.350 | ||
| Artiflex | Artisan | −0.34 | 0.14 | 0.460 | |
| PRK | FS-Lasik | −0.13 | 0.03 | <0.01 | |
| Artiflex | −0.23 | 0.10 | 0.200 | ||
| Artisan | −0.44 | 0.11 | 0.140 | ||
| Safety 3 months | FS-Lasik | Artiflex | −0.10 | 0.10 | 0.980 |
| Artisan | −0.30 | 0.11 | 0.390 | ||
| Artiflex | Artisan | −0.21 | 0.14 | 0.850 | |
| PRK | FS-Lasik | −0.15 | 0.05 | 0.020 | |
| Artiflex | −0.08 | 0.05 | 0.670 | ||
| Artisan | −0.12 | 0.12 | 0.990 | ||
| Safety 1 year | FS-Lasik | Artiflex | 0.08 | 0.06 | 0.880 |
| Artisan | 0.03 | 0.13 | 1.000 | ||
| Artiflex | Artisan | −0.04 | 0.13 | 1.000 | |
| PRK | FS-Lasik | −0.09 | 0.04 | 0.150 | |
| Artiflex | 0.04 | 0.09 | 1.000 | ||
| Artisan | −0.09 | 0.13 | 1.000 | ||
| Safety 5 year | FS-Lasik | Artiflex | 0.14 | 0.10 | 0.850 |
| Artisan | 0.00 | 0.13 | 1.000 | ||
| Artiflex | Artisan | −0.14 | 0.16 | 1.000 | |
| Coefficient | SD | t Value | p-Value | |
|---|---|---|---|---|
| Constant | 0.96 | 0.05 | 20.476 | <0.001 * |
| Sph Equival Preop | 0.04 | 0.01 | 10.716 | <0.001 * |
| Reference Technique = Femto-LASIK | ||||
| Technique = Phakic Lens | 0.43 | 0.04 | 10.316 | <0.001 * |
| Technique = PRK | −0.08 | 0.02 | −3.069 | <0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castro-Luna, G.; Sánchez-Liñán, N.; Alaskar, H.; Pérez-Rueda, A.; Nievas-Soriano, B.J. Comparison of Iris-Claw Phakic Lens Implant versus Corneal Laser Techniques in High Myopia: A Five-Year Follow-Up Study. Healthcare 2022, 10, 1904. https://doi.org/10.3390/healthcare10101904
Castro-Luna G, Sánchez-Liñán N, Alaskar H, Pérez-Rueda A, Nievas-Soriano BJ. Comparison of Iris-Claw Phakic Lens Implant versus Corneal Laser Techniques in High Myopia: A Five-Year Follow-Up Study. Healthcare. 2022; 10(10):1904. https://doi.org/10.3390/healthcare10101904
Chicago/Turabian StyleCastro-Luna, Gracia, Noelia Sánchez-Liñán, Hazem Alaskar, Antonio Pérez-Rueda, and Bruno José Nievas-Soriano. 2022. "Comparison of Iris-Claw Phakic Lens Implant versus Corneal Laser Techniques in High Myopia: A Five-Year Follow-Up Study" Healthcare 10, no. 10: 1904. https://doi.org/10.3390/healthcare10101904
APA StyleCastro-Luna, G., Sánchez-Liñán, N., Alaskar, H., Pérez-Rueda, A., & Nievas-Soriano, B. J. (2022). Comparison of Iris-Claw Phakic Lens Implant versus Corneal Laser Techniques in High Myopia: A Five-Year Follow-Up Study. Healthcare, 10(10), 1904. https://doi.org/10.3390/healthcare10101904






