Exploring the Feelings of Nurses during Resuscitation—A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Instruments
2.3. Scale Validity
2.4. Ethical Considerations
2.5. Statistical Analysis
3. Results
3.1. Sample Description
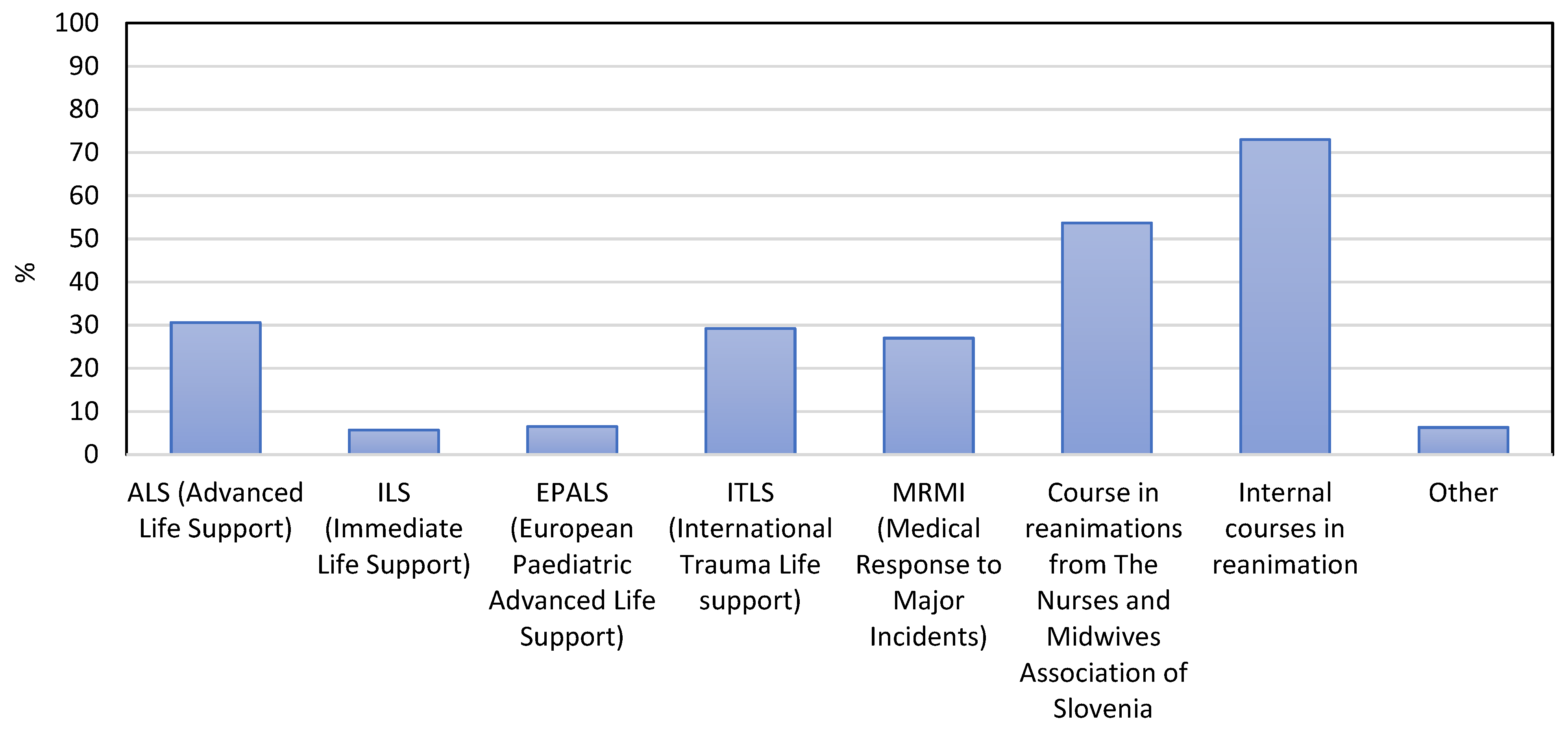
3.2. Education and Experience with Resuscitation
3.3. Analysis of Questionnaires
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Perkins, G.D.; Graesner, J.T.; Semeraro, F.; Olasveengen, T.; Soar, J.; Lott, C.; Van de Voorde, P.; Madar, J.; Zideman, D.; Mentzelopoulos, S.; et al. European Resuscitation Council Guidelines 2021: Executive summary. Resuscitation 2021, 161, 1–60. [Google Scholar] [CrossRef]
- Twibell, R.; Siela, D.; Riwitis, C.; Neal, A.; Waters, N. A qualitative study of factors in nurses’ and physicians’ decision-making related to family presence during resuscitation. J. Clin. Nurs. 2018, 27, e320–e334. [Google Scholar] [CrossRef]
- Aldabagh, M.; Wagle, S.; Cesa, M.; Yu, A.; Farooq, M.; Goldberg, Y. Survival of In-Hospital Cardiac Arrest in COVID-19 Infected Patients. Healthcare 2021, 9, 1315. [Google Scholar] [CrossRef]
- Hansen, C.; Lauridsen, K.G.; Schmidt, A.S.; Løfgren, B. Decision-making in cardiac arrest: Physicians’ and nurses’ knowledge and views on terminating resuscitation. Open Access Emerg. Med. 2018, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Gräsner, J.-T.; Herlitz, J.; Tjelmeland, I.B.M.; Wnent, J.; Masterson, S.; Lilja, G.; Bein, B.; Böttiger, B.W.; Rosell-Ortiz, F.; Nolan, J.P.; et al. European Resuscitation Council Guidelines 2021: Epidemiology of cardiac arrest in Europe. Resuscitation 2021, 161, 61–79. [Google Scholar] [CrossRef] [PubMed]
- Olasveengen, T.M.; Semeraro, F.; Ristagno, G.; Castren, M.; Handley, A.; Kuzovlev, A.; Monsieurs, K.G.; Raffay, V.; Smyth, M.; Soar, J.; et al. European Resuscitation Council Guidelines 2021: Basic Life Support. Resuscitation 2021, 161, 98–114. [Google Scholar] [CrossRef] [PubMed]
- Panesar, S.S.; Ignatowicz, A.M.; Donaldson, L.J. Errors in the management of cardiac arrests: An observational study of patient safety incidents in England. Resuscitation 2014, 85, 1759–1763. [Google Scholar] [CrossRef]
- Soar, J.; Böttiger, B.W.; Carli, P.; Couper, K.; Deakin, C.D.; Djärv, T.; Lott, C.; Olasveengen, T.; Paal, P.; Pellis, T.; et al. European Resuscitation Council Guidelines 2021: Adult advanced life support. Resuscitation 2021, 161, 115–151. [Google Scholar] [CrossRef] [PubMed]
- Stokes, F.; Zoucha, R. Nurses’ Participation in Limited Resuscitation: Gray Areas in End of Life Decision-Making. AJOB Empir. Bioeth. 2021, 12, 239–252. [Google Scholar] [CrossRef]
- Gräsner, J.-T.; Wnent, J.; Herlitz, J.; Perkins, G.D.; Lefering, R.; Tjelmeland, I.; Koster, R.W.; Masterson, S.; Rossell-Ortiz, F.; Maurer, H.; et al. Survival after out-of-hospital cardiac arrest in Europe—Results of the EuReCa TWO study. Resuscitation 2020, 148, 218–226. [Google Scholar] [CrossRef]
- Andersen, L.W.; Holmberg, M.J.; Berg, K.M.; Donnino, M.W.; Granfeldt, A. In-Hospital Cardiac Arrest. JAMA 2019, 321, 1200. [Google Scholar] [CrossRef] [PubMed]
- Mentzelopoulos, S.D.; Couper, K.; Voorde, P.V.; Druwé, P.; Blom, M.; Perkins, G.D.; Lulic, I.; Djakow, J.; Raffay, V.; Lilja, G.; et al. European Resuscitation Council Guidelines 2021: Ethics of resuscitation and end of life decisions. Resuscitation 2021, 161, 408–432. [Google Scholar] [CrossRef]
- Douw, G.; Schoonhoven, L.; Holwerda, T.; Huisman-De Waal, G.; Van Zanten, A.R.H.; Van Achterberg, T.; Van Der Hoeven, J.G. Nurses’ worry or concern and early recognition of deteriorating patients on general wards in acute care hospitals: A systematic review. Crit. Care 2015, 19, 230. [Google Scholar] [CrossRef] [PubMed]
- Hinderer, K.A. Reactions to patient death: The lived experience of critical care nurses. Dimens. Crit. Care Nurs. 2012, 31, 252–259. [Google Scholar] [CrossRef]
- Chang, S.-H.; Huang, C.-H.; Shih, C.-L.; Lee, C.-C.; Chang, W.-T.; Chen, Y.-T.; Lee, C.-H.; Lin, Z.-Y.; Tsai, M.-S.; Hsu, C.-Y.; et al. Who survives cardiac arrest in the intensive care units? J. Crit. Care 2009, 24, 408–414. [Google Scholar] [CrossRef]
- Gershengorn, H.B.; Li, G.; Kramer, A.; Wunsch, H. Survival and functional outcomes after cardiopulmonary resuscitation in the intensive care unit. J. Crit. Care 2012, 27, 421.e9–421.e17. [Google Scholar] [CrossRef]
- Nolan, J.P.; Monsieurs, K.G.; Bossaert, L.; Böttiger, B.W.; Greif, R.; Lott, C.; Madar, J.; Olasveengen, T.M.; Roehr, C.C.; Semeraro, F.; et al. European Resuscitation Council COVID-19 guidelines executive summary. Resuscitation 2020, 153, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Defilippis, E.M.; Ranard, L.S.; Berg, D.D. Cardiopulmonary Resuscitation During the COVID-19 Pandemic. Circulation 2020, 141, 1833–1835. [Google Scholar] [CrossRef]
- Chahar, P.; Marciniak, D. Cardiopulmonary resuscitation in COVID-19 patients. Clevel. Clin. J. Med. 2020, 65, 109879. [Google Scholar] [CrossRef]
- Kapoor, I.; Prabhakar, H.; Mahajan, C. Cardiopulmonary resuscitation in COVID-19 patients—To do or not to? J. Clin. Anesth. 2020, 65, 109879. [Google Scholar] [CrossRef] [PubMed]
- Carmassi, C.; Foghi, C.; Dell’Oste, V.; Cordone, A.; Bertelloni, C.A.; Bui, E.; Dell’Osso, L. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: What can we expect after the COVID-19 pandemic. Psychiatry Res. 2020, 292, 113312. [Google Scholar] [CrossRef] [PubMed]
- Li, J.-H.; Chen, T.-W.; Lee, H.-F.; Shih, W.-M. The Effects of Emergency Room Violence toward Nurse′s Intention to Leave—Resilience as a Mediator. Healthcare 2021, 9, 507. [Google Scholar] [CrossRef] [PubMed]
- Amini, R.; Mohammadi, N.; Karaji, F.; Tapak, L. Frequency of the Type of Workplace Violence Against Hamadan Medical Emergency Technicians and Its Relationship with Individual and Occupational Variables, 2018. Avicenna J. Nurs. Midwifery Care 2020, 27, 381–393. [Google Scholar] [CrossRef][Green Version]
- Dwyer, T.; Mosel Williams, L. Nurses’ behaviour regarding CPR and the theories of reasoned action and planned behaviour. Resuscitation 2002, 52, 85–90. [Google Scholar] [CrossRef]
- Riley, K.; Middleton, R.; Wilson, V.; Molloy, L. Voices from the ‘resus room’: An integrative review of the resuscitation experiences of nurses. J. Clin. Nurs. 2021. [Google Scholar] [CrossRef] [PubMed]
- Kerasiotis, B.; Motta, R. Assessment of PTSD symptoms in emergency room, intensive care unit, and general floor nurses. Int. J. Emerg. Ment. Health 2004, 6, 121–133. [Google Scholar]
- Desbiens, J.F.; Fillion, L. Coping strategies, emotional outcomes and spiritual quality of life in palliative care nurses. Int. J. Palliat. Nurs. 2007, 13, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Mealer, M.L.; Shelton, A.; Berg, B.; Rothbaum, B.; Moss, M. Increased Prevalence of Post-traumatic Stress Disorder Symptoms in Critical Care Nurses. Am. J. Respir. Crit. Care Med. 2007, 175, 693–697. [Google Scholar] [CrossRef]
- McMeekin, D.E.; Hickman, R.L.; Douglas, S.L.; Kelley, C.G. Stress and Coping of Critical Care Nurses After Unsuccessful Cardiopulmonary Resuscitation. Am. J. Crit. Care 2017, 26, 128–135. [Google Scholar] [CrossRef]
- Raosoft. Sample Size Calculator. Available online: http://www.raosoft.com/samplesize.html (accessed on 12 October 2021).
- NIJZ. Izvajalci Zdravstvene Dejavnosti 2020. Available online: https://www.nijz.si/sl/podatki/prva-objava-izvajalci-zdravstvene-dejavnosti-2020 (accessed on 10 October 2021).
- Cole, F.L.; Slocumb, E.M.; Mastey, J.M. A measure of critical care nurses’ post-code stress. J. Adv. Nurs. 2001, 34, 281–288. [Google Scholar] [CrossRef]
- Arshid, M.; Lo, T.-Y.M.; Reynolds, F. Quality of cardio-pulmonary resuscitation (CPR) during paediatric resuscitation training: Time to stop the blind leading the blind. Resuscitation 2009, 80, 558–560. [Google Scholar] [CrossRef]
- Adams, B.D.; Zeiler, K.; Jackson, W.O.; Hughes, B. Emergency medicine residents effectively direct inhospital cardiac arrest teams. Am. J. Emerg. Med. 2005, 23, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Bradley, P.; Cooper, S.; Duncan, F. A mixed-methods study of interprofessional learning of resuscitation skills. Med. Educ. 2009, 43, 912–922. [Google Scholar] [CrossRef]
- Cole, E.; Crichton, N. The culture of a trauma team in relation to human factors. J. Clin. Nurs. 2006, 15, 1257–1266. [Google Scholar] [CrossRef] [PubMed]
- Hoff, W.S.; Reilly, P.M.; Rotondo, M.F.; DiGiacomo, J.C.; Schwab, C.W. The importance of the command-physician in trauma resuscitation. J. Trauma 1997, 43, 772–777. [Google Scholar] [CrossRef]
- Streiff, S.; Tschan, F.; Hunziker, S.; Buehlmann, C.; Semmer, N.K.; Hunziker, P.; Marsch, S. Leadership in medical emergencies depends on gender and personality. Simul. Healthc. 2011, 6, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Fernandez Castelao, E.; Russo, S.G.; Riethmüller, M.; Boos, M. Effects of team coordination during cardiopulmonary resuscitation: A systematic review of the literature. J. Crit. Care 2013, 28, 504–521. [Google Scholar] [CrossRef]
- Olasveengen, T.M.; Lund-Kordahl, I.; Steen, P.A.; Sunde, K. Out-of hospital advanced life support with or without a physician: Effects on quality of CPR and outcome. Resuscitation 2009, 80, 1248–1252. [Google Scholar] [CrossRef] [PubMed]
- Vicente, V.; Johansson, A.; Ivarsson, B.; Todorova, L.; Möller, S. The Experience of Using Video Support in Ambulance Care: An Interview Study with Physicians in the Role of Regional Medical Support. Healthcare 2020, 8, 106. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Brazil, J.; Ozkaynak, M.; Desanto, K. Evaluative Research of Technologies for Prehospital Communication and Coordination: A Systematic Review. J. Med. Syst. 2020, 44, 100. [Google Scholar] [CrossRef] [PubMed]
- Jensen, F.B.; Ladefoged, K.T.; Lindskou, T.A.; Søvsø, M.B.; Christensen, E.F.; Teli, M. Understanding the Effect of Electronic Prehospital Medical Records in Ambulances: A Qualitative Observational Study in a Prehospital Setting. Int. J. Environ. Res. Public Health 2021, 18, 2330. [Google Scholar] [CrossRef]
- Mooney. Clinical Practice Guidelines for Pre-Hospital Emergency Care, 2nd ed.; Pre-Hospital Emergency Care Council: Naas, Ireland, 2011; Volume 3, p. 170. [Google Scholar]
- Knox, S.; Cullen, W.; Dunne, C. Continuous Professional Competence (CPC) for Irish paramedics and advanced paramedics: A national study. BMC Med. Educ. 2014, 14, 41. [Google Scholar] [CrossRef]
- Mikkelsen, S.; Kruger, A.J.; Zwisler, S.T.; Brochner, A.C. Outcome following physician supervised prehospital resuscitation: A retrospective study. BMJ Open 2015, 5, e006167. [Google Scholar] [CrossRef] [PubMed]
- Spencer, S.A.; Nolan, J.P.; Osborn, M.; Georgiou, A. The presence of psychological trauma symptoms in resuscitation providers and an exploration of debriefing practices. Resuscitation 2019, 142, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Wang, H.; Xie, J.; Zhang, J.; Li, H.; Liu, S.; Li, Q.; Yang, Y.; Huang, Y. Burnout in ICU doctors and nurses in mainland China—A national cross-sectional study. J. Crit. Care 2021, 62, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, K.C.C.D.; Batista, J.B.V.; Azevedo, R.C.D.; Araújo, A.L.B.D.; Barros, E.D.O.; Rodrigues, M.D.S.D. National scientific production on Burnout Syndrome in ICU nurses and physicians: A bibliometric study. Rev. Assoc. Méd. Bras. 2019, 65, 722–729. [Google Scholar] [CrossRef]
- Da Silva, J.L.; Soares Rda, S.; Costa Fdos, S.; Ramos Dde, S.; Lima, F.B.; Teixeira, L.R. Psychosocial factors and prevalence of burnout syndrome among nursing workers in intensive care units. Rev. Bras. Ter. Intensiv. 2015, 27, 125–133. [Google Scholar] [CrossRef]
- Tennyson, C.D. Family presence during resuscitation: Updated review and clinical pearls. Geriatr. Nurs. 2019, 40, 645–647. [Google Scholar] [CrossRef]
- Monks, J.; Flynn, M. Care, compassion and competence in critical care: A qualitative exploration of nurses’ experience of family witnessed resuscitation. Intensiv. Crit. Care Nurs. 2014, 30, 353–359. [Google Scholar] [CrossRef]
- Toronto, C.E.; Larocco, S.A. Family perception of and experience with family presence during cardiopulmonary resuscitation: An integrative review. J. Clin. Nurs. 2019, 28, 32–46. [Google Scholar] [CrossRef]
- Fulbrook, P.; Albarran, J.W.; Latour, J.M. A European survey of critical care nurses’ attitudes and experiences of having family members present during cardiopulmonary resuscitation. Int. J. Nurs. Stud. 2005, 42, 557–568. [Google Scholar] [CrossRef] [PubMed]
- Porter, J.E.; Cooper, S.J.; Taylor, B. Family presence during resuscitation (FPDR): A survey of emergency personnel in Victoria, Australia. Australas. Emerg. Nurs. J. 2015, 18, 98–105. [Google Scholar] [CrossRef]
- Stewart, S.A. Parents’ Experience during a Child’s Resuscitation: Getting through It. J. Pediatr. Nurs. 2019, 47, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Koželj, A.; Strauss, M.; Strnad, M. Experiencing Stress among Nurses during Resuscitation Procedure and Legal Obligations for Healthcare Workers in Slovenia. Med. Law Soc. 2020, 13, 237–262. [Google Scholar] [CrossRef]
- Dyson, E.; Smith, G.B. Common faults in resuscitation equipment—Guidelines for checking equipment and drugs used in adult cardiopulmonary resuscitation. Resuscitation 2002, 55, 137–149. [Google Scholar] [CrossRef]
- Hohenstein, C.; Rupp, P.; Fleischmann, T. Critical incidents during prehospital cardiopulmonary resuscitation: What are the problems nobody wants to talk about? Eur. J. Emerg Med. 2011, 18, 38–40. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, N.; Jones, R.; Abdel-Latif, M. Attitudes of Doctors and Nurses toward Patient Safety within Emergency Departments of a Saudi Arabian Hospital: A Qualitative Study. Healthcare 2019, 7, 44. [Google Scholar] [CrossRef] [PubMed]
- Hunziker, S.; Pagani, S.; Fasler, K.; Tschan, F.; Semmer, N.K.; Marsch, S. Impact of a stress coping strategy on perceived stress levels and performance during a simulated cardiopulmonary resuscitation: A randomized controlled trial. BMC Emerg. Med. 2013, 13, 8. [Google Scholar] [CrossRef]
| Age and Work Experience | Min | Max | MV |
|---|---|---|---|
| Age | 20 | 61 | 36.2 |
| Years of service in healthcare | 1 | 41 | 13.8 |
| Years of service in the emergency area | 1 | 40 | 10.6 |
| Approximated Number of Resuscitations per Year | With a Physician | Without Physician | ||
|---|---|---|---|---|
| n | % | n | % | |
| None | 25 | 5.5 | 203 | 44.4 |
| 1–5 | 203 | 44.4 | 223 | 48.8 |
| 6–10 | 133 | 29.1 | 23 | 5.0 |
| 11–15 | 43 | 9.4 | 4 | 0.9 |
| 16–20 | 22 | 4.8 | 2 | 0.4 |
| >20 | 31 | 6.8 | 2 | 0.4 |
| Experiencing Resuscitation with or without the Presence of a Physician | n | % |
|---|---|---|
| The presence or absence of a physician does not affect my experience of resuscitation | 63 | 13.9 |
| I find resuscitation easier when a physician is present | 95 | 20.9 |
| I find resuscitation more difficult when a physician is present | 10 | 2.2 |
| It depends on the physician’s knowledge and ability to lead a team | 278 | 61.2 |
| Without the presence of a physician, resuscitation is not performed | 8 | 1.8 |
| No. | Items | MV | SD |
|---|---|---|---|
| 1 | When my hands shake during a code | 2.4 | 1.3 |
| 2 | When my peers are quick to notice and point out that I made a mistake | 2.3 | 1.3 |
| 3 | When I feel like I didn’t function well during a code | 3.2 | 1.3 |
| 4 | When more than one doctor gives orders during a code | 3.2 | 1.4 |
| 5 | When I lose my confidence during a code | 2.8 | 1.3 |
| 6 | When a patient’s family thinks I can keep him/her alive | 2.8 | 1.3 |
| 7 | When I am unable to make a properly functioning piece of equipment operate during a code | 3.4 | 1.4 |
| 8 | When hospital policies/procedures are conflicting | 3.2 | 1.4 |
| 9 | When we code a patient, I believe we should not code | 3.0 | 1.4 |
| 10 | When I have trouble reading the ECG | 3.0 | 1.3 |
| 11 | When I code some patients only because hospital policy says I must | 3.0 | 1.4 |
| 12 | When a nurse manager/supervisor criticizes me when I’ve done my best | 3.4 | 1.4 |
| 13 | When a nurse manager doesn’t provide assistance during a code | 3.4 | 1.3 |
| 14 | When I wonder if I made a mistake | 2.9 | 1.2 |
| 15 | When I am not permitted time to regroup and pick myself up after a code | 3.0 | 1.4 |
| 16 | When people think I can function appropriately immediately after a code | 2.8 | 1.4 |
| 17 | When I code someone young | 3.7 | 1.4 |
| 18 | When no one talks about the code after it is over | 2.7 | 1.4 |
| 19 | When I think I might have missed a sign or symptom that would have helped me predict that the patient would code | 3.3 | 1.3 |
| 20 | When the patient dies | 2.8 | 1.3 |
| Source of Stress | Min | Max | MV | SD |
|---|---|---|---|---|
| From feeling discomposed | 4 | 20 | 11.2 | 3.8 |
| From feeling oppressed | 3 | 15 | 8.6 | 3.4 |
| From feeling uncertain | 3 | 10 | 8.5 | 3.0 |
| From feeling burdened | 3 | 15 | 9.5 | 3.3 |
| From feeling morally conflicted | 2 | 10 | 6.0 | 2.4 |
| Source of Stress | Discomposed | Oppressed | Uncertain | Burdened | Moral Conflict | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Years of service in healthcare | ||||||||||
| Years of service | 0.98 (0.96–1.00) | 0.040 | 1.01 (0.99–1.03) | 0.311 | 0.98 (0.96–1.00) | 0.053 | 1.01 (0.99–1.02) | 0.424 | 1.01 (0.99–1.03) | 0.251 |
| Sex | ||||||||||
| Female | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |||||
| Male | 0.56 (0.37–0.85) | 0.006 | 0.60 (0.40–0.90) | 0.012 | 0.45 (0.30–0.68) | <0.001 | 0.45 (0.30–0.68) | <0.001 | 0.57 (0.38–0.86) | 0.008 |
| Area of employment | ||||||||||
| Other * | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |||||
| Prehospital | 1.16 (0.51–2.68) | 0.727 | 1.49 (0.65–3.44) | 0.361 | 1.13 (0.49–2.61) | 0.802 | 0.79 (0.34–1.83) | 0.575 | 1.44 (0.62–3.33) | 0.387 |
| Hospital | 1.81 (0.76–4.32) | 0.203 | 3.11 (1.30–7.48) | 0.012 | 2.18 (0.91–5.21) | 0.097 | 1.09 (0.46–2.60) | 0.885 | 2.10 (0.87–5.06) | 0.096 |
| The approximate number of resuscitations per year with physician supervision | ||||||||||
| 0 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |||||
| 1–5 | 0.75 (0.34–1.63) | 0.555 | 0.66 (0.30–1.43) | 0.391 | 1.14 (0.52–2.49) | 0.566 | 1.04 (0.48–2.27) | 0.790 | 0.99 (0.45–2.17) | 0.961 |
| 6–10 | 0.65 (0.29–1.48) | 0.384 | 0.54 (0.24–1.22) | 0.215 | 0.89 (0.39–2.02) | 0.996 | 1.05 (0.46–2.37) | 0.761 | 0.93 (0.41–2.10) | 0.843 |
| 11–15 | 0.77 (0.30–1.96) | 0.668 | 0.91 (0.36–2.32) | 0.966 | 1.48 (0.58–3.76) | 0.308 | 1.43 (0.56–3.64) | 0.364 | 1.71 (0.67–4.37) | 0.264 |
| 16–20 | 0.72 (0.24–2.14) | 0.479 | 0.87 (0.29–2.57) | 0.714 | 1.00 (0.34–2.96) | 0.908 | 1.94 (0.65–5.76) | 0.342 | 2.07 (0.69–6.21) | 0.318 |
| >20 | 0.66 (0.25–1.77) | 0.503 | 0.42 (0.16–1.13) | 0.117 | 0.94 (0.35–2.52) | 0.872 | 1.09 (0.40–2.92) | 0.745 | 0.96 (0.35–2.59) | 0.900 |
| The approximate number of resuscitations per year without physician supervision | ||||||||||
| 0 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |||||
| 1–5 | 1.01 (0.69–1.46) | 0.997 | 1.29 (0.89–1.88) | 0.190 | 1.28 (0.88–1.86) | 0.197 | 1.08 (0.74–1.56) | 0.699 | 1.43 (0.98–2.09) | 0.061 |
| >6 | 0.85 (0.40–1.80) | 0.318 | 1.02 (0.48–2.16) | 0.390 | 0.74 (0.35–1.58) | 0.437 | 0.76 (0.36–1.61) | 0.467 | 1.17 (0.55–2.50) | 0.684 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koželj, A.; Šikić Pogačar, M.; Fijan, S.; Strauss, M.; Poštuvan, V.; Strnad, M. Exploring the Feelings of Nurses during Resuscitation—A Cross-Sectional Study. Healthcare 2022, 10, 5. https://doi.org/10.3390/healthcare10010005
Koželj A, Šikić Pogačar M, Fijan S, Strauss M, Poštuvan V, Strnad M. Exploring the Feelings of Nurses during Resuscitation—A Cross-Sectional Study. Healthcare. 2022; 10(1):5. https://doi.org/10.3390/healthcare10010005
Chicago/Turabian StyleKoželj, Anton, Maja Šikić Pogačar, Sabina Fijan, Maja Strauss, Vita Poštuvan, and Matej Strnad. 2022. "Exploring the Feelings of Nurses during Resuscitation—A Cross-Sectional Study" Healthcare 10, no. 1: 5. https://doi.org/10.3390/healthcare10010005
APA StyleKoželj, A., Šikić Pogačar, M., Fijan, S., Strauss, M., Poštuvan, V., & Strnad, M. (2022). Exploring the Feelings of Nurses during Resuscitation—A Cross-Sectional Study. Healthcare, 10(1), 5. https://doi.org/10.3390/healthcare10010005







