The Impact of Delayed Symptomatic Treatment Implementation in the Intensive Care Unit
Abstract
:1. Introduction
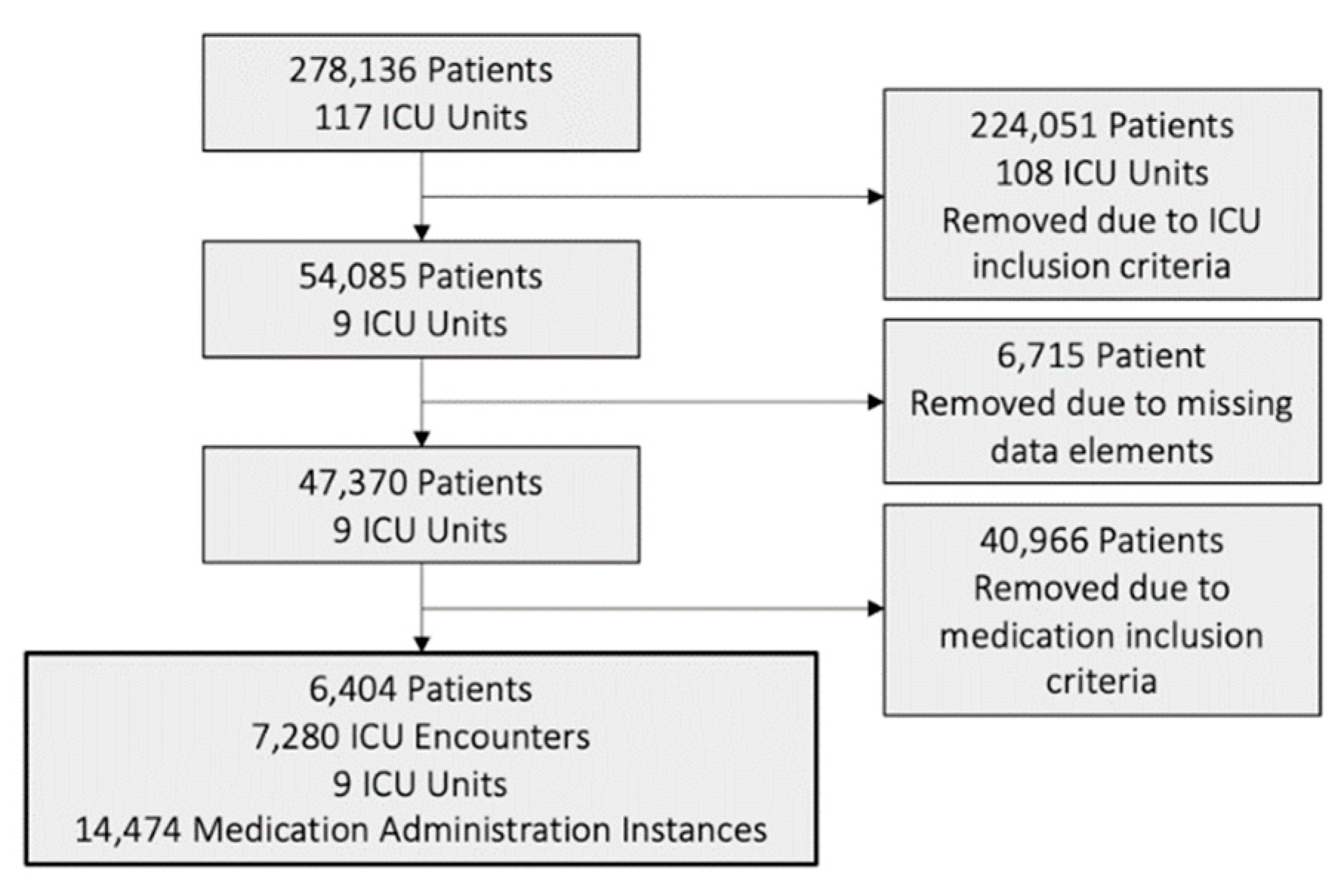
2. Materials and Methods
2.1. Setting
2.2. Measuring Medication Delay
2.3. Statistical Approach
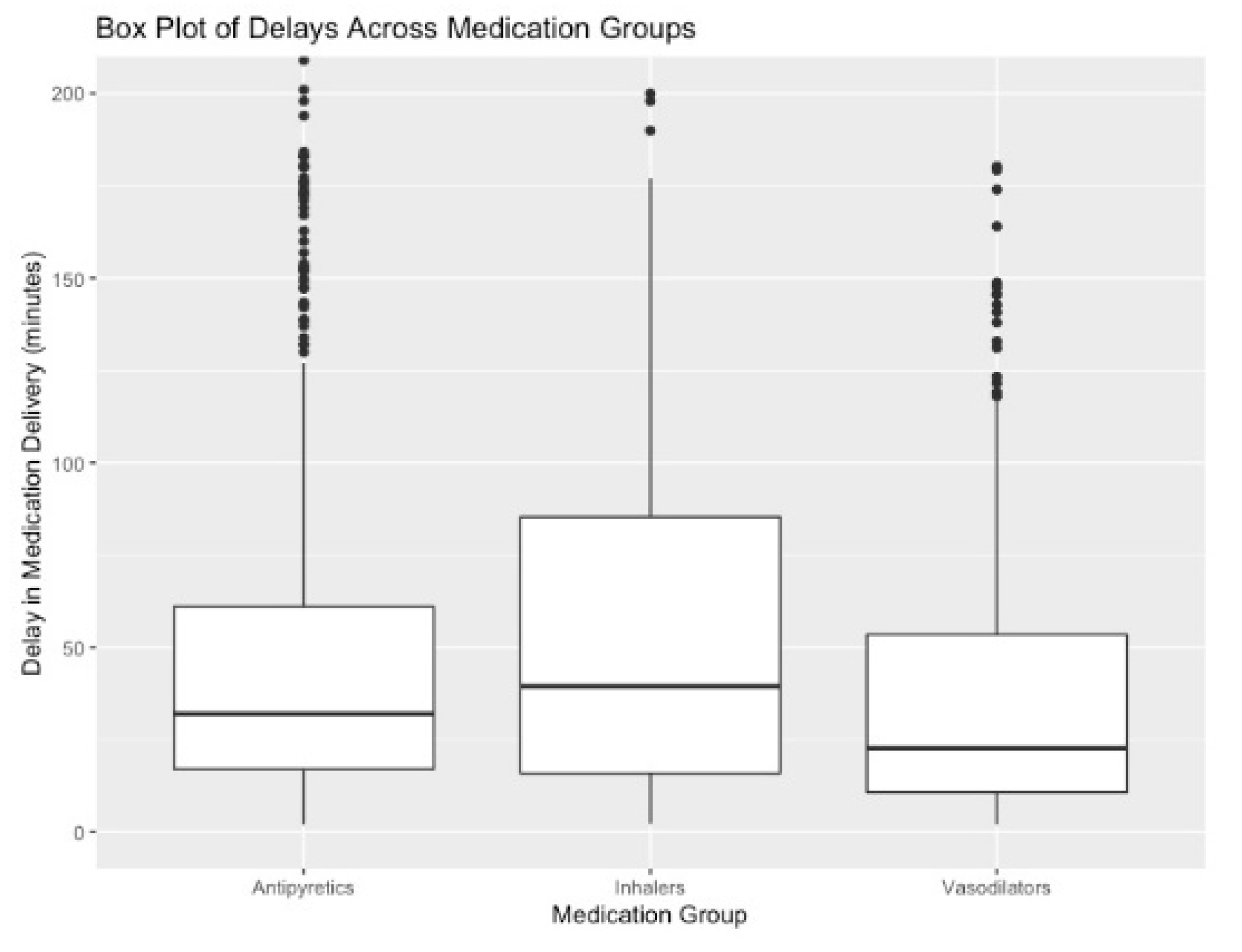
3. Results
3.1. Estimated Effect of Nursing Shift Change on Medication Delay
3.2. Estimated Effect of Medication Delay on Patient Vital Status
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Homsted, L. Institute of Medicine report: To err is human: Building a safer health care system. Fla. Nurse 2000, 48, 6. [Google Scholar]
- Leape, L.L.; Lawthers, A.G.; Brennan, T.A.; Johnson, W.G. Preventing Medical Injury. Qual. Rev. Bull. 1993, 19, 144–149. [Google Scholar] [CrossRef]
- Alhazzani, W.; Møller, M.H.; Arabi, Y.M.; Loeb, M.; Gong, M.N.; Fan, E.; Oczkowski, S.; Levy, M.M.; Derde, L.; Dzierba, A.; et al. Surviving Sepsis Campaign: Guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020, 46, 854–887. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Russell-Babin, K.; Wurmser, T. Transforming care through top-of-license practice. J. Excell. Nurs. Leadersh. 2016, 47, 24–28. [Google Scholar] [CrossRef]
- Lighthall, G.K.; Vazquez-Guillamet, C. Understanding Decision Making in Critical Care. Clin. Med. Res. 2015, 13, 156–168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jena, A.B.; Mann, N.C.; Wedlund, L.N.; Olenski, A. Delays in Emergency Care and Mortality during Major U.S. Marathons. N. Engl. J. Med. 2017, 376, 1441–1450. [Google Scholar] [CrossRef] [Green Version]
- Shen, Y.C.; Hsia, R.Y. Association between ambulance diversion and survival among patients with acute myocardial infarction. JAMA 2011, 305, 2440–2447. [Google Scholar] [CrossRef] [Green Version]
- Allon, G.; Deo, S.; Lin, W. The Impact of Size and Occupancy of Hospital on the Extent of Ambulance Diversion: Theory and Evidence. Oper. Res. 2013, 61, 544–562. [Google Scholar] [CrossRef]
- McIsaac, D.I.; Abdulla, K.; Yang, H.; Sundaresan, S.; Doering, P.; Vaswani, S.G.; Thavorn, K.; Forster, A.J. Association of delay of urgent or emergency surgery with mortality and use of health care resources: A propensity score–matched observational cohort study. Can. Med. Assoc. J. 2017, 189, E905–E912. [Google Scholar] [CrossRef] [Green Version]
- Werner, R.M.; Canamucio, A.; Marcus, S.C.; Terwiesch, C. Primary Care Access and Emergency Room Use Among Older Veterans. J. Gen. Intern. Med. 2014, 29 (Suppl S2), 689–694. [Google Scholar] [CrossRef] [Green Version]
- Pomerantz, A.; Cole, B.H.; Watts, B.V.; Weeks, W.B. Improving efficiency and access to mental health care: Combining integrated care and advanced access. Gen. Hosp. Psychiatry 2008, 30, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Song, H.; Tucker, A.L.; Graue, R.; Moravick, S.; Yang, J.J. Capacity Pooling in Hospitals: The Hidden Consequences of Off-Service Placement. Manag. Sci. 2020, 66, 3825–3842. [Google Scholar] [CrossRef]
- Donaldson, N.; Aydin, C.; Fridman, M. Predictors of Unit-Level Medication Administration Accuracy: Microsystem Impacts on Medication Safety. J. Nurs. Adm. 2014, 44, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Welton, J.M.; Kleiner, C.; Valdez, C.; Richardson, S.; Boyle, K.; Lucas, E. Using Time-Referenced Data to Assess Medication Administration Performance and Quality. J. Nurs. Adm. 2018, 48, 100–106. [Google Scholar] [CrossRef]
- Elganzouri, E.S.; Standish, C.A.; Androwich, I. Medication Administration Time Study (MATS): Nursing staff performance of medication administration. J. Nurs. Adm. 2009, 39, 204–210. [Google Scholar] [CrossRef]
- Norris, P.R.; Dawant, B.M. Closing the loop in ICU decision support: Physiologic event detection, alerts, and documentation. Proc. AMIA Symp. 2001, 9, 498–502. [Google Scholar] [CrossRef] [Green Version]
- McKenzie, M.S.; Auriemma, C.L.; Olenik, J.; Cooney, E.; Gabler, N.B.; Halpern, S.D. An Observational Study of Decision Making by Medical Intensivists. Crit. Care Med. 2015, 43, 1660–1668. [Google Scholar] [CrossRef]
- de Bock, B.A.; Willems, D.L.; Weinstein, H.C. Complexity perspectives on clinical decision making in an intensive care unit. J. Eval. Clin. Pract. 2017, 24, 308–313. [Google Scholar] [CrossRef]
- Drews, F.A.; Markewitz, B.A.; Stoddard, G.J.; Samore, M.H. Interruptions and Delivery of Care in the Intensive Care Unit. Hum. Factors 2019, 61, 564–576. [Google Scholar] [CrossRef] [Green Version]
- Heymann, A.; Radtke, F.; Schiemann, A.; Lütz, A.; MacGuill, M.; Wernecke, K.D.; Spies, C. Delayed Treatment of Delirium Increases Mortality Rate in Intensive Care Unit Patients. J. Int. Med Res. 2010, 38, 1584–1595. [Google Scholar] [CrossRef]
- Nagar, S.; Davey, N. Reducing avoidable time delays in immediate medication administration—learning from a failed intervention. BMJ Qual. Improv. Rep. 2015, 4, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, C.W.; Farias, V.F.; Escobar, G.J. The Impact of Delays on Service Times in the Intensive Care Unit. Manag. Sci. 2017, 63, 2049–2072. [Google Scholar] [CrossRef] [Green Version]
- Zilberberg, M.D.; Nathanson, B.H.; Sulham, K.; Fan, W.; Shorr, A.F. Daily cost of delay to adequate antibiotic treatment among patients surviving a hospitalization with community-onset Acinetobacter baumannii pneumonia or sepsis. Crit. Care 2017, 21, 1–2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agustin, M.; Price, L.L.; Andoh-Duku, A.; LaCamera, P. Impact of Delayed Admission to the Intensive Care Unit from the Emergency Department upon Sepsis Outcomes and Sepsis Protocol Compliance. Crit. Care Res. Pract. 2017, 2017, 9616545. [Google Scholar] [CrossRef] [PubMed]
- Corl, K.; Zeba, F.; Caffrey, A.R.; Hermenau, M.; Lopes, V.; Phillips, G.; Merchant, R.C.; Levy, M.M.; Laplante, K.L. Delay in Antibiotic Administration Is Associated With Mortality Among Septic Shock Patients With Staphylococcus aureus Bacteremia. Crit. Care Med. 2020, 48, 525–532. [Google Scholar] [CrossRef]
- Poon, E.G.; Keohane, C.A.; Yoon, C.S.; Ditmore, M.; Bane, A.; Levtzion-Korach, O.; Moniz, T.; Rothschild, J.M.; Kachalia, A.B.; Hayes, J.; et al. Effect of Bar-Code Technology on the Safety of Medication Administration. N. Engl. J. Med. 2010, 362, 1698–1707. [Google Scholar] [CrossRef] [Green Version]
- Kane-Gill, S.L.; Dasta, J.F.; Buckley, M.S.; Devabhakthuni, S.; Liu, M.; Cohen, H.; George, E.L.; Pohlman, A.S.; Agarwal, S.; Henneman, E.A.; et al. Clinical Practice Guideline: Safe Medication Use in the ICU. Crit. Care Med. 2017, 45, e877–e915. [Google Scholar] [CrossRef]
- Furnish, C.; Wagner, S.; Dangler, A.; Schwarz, K.; Trujillo, T.; Stolpman, N.; May, S. Evaluation of Medication Administration Timing-Are We Meeting Our Goals? J. Pharm. Pract. 2021, 34, 750–754. [Google Scholar] [CrossRef]
- Saposnik, G.; Redelmeier, D.; Ruff, C.C.; Tobler, P.N. Cognitive biases associated with medical decisions: A systematic review. BMC Med. Inform. Decis. Mak. 2016, 16, 138. [Google Scholar] [CrossRef] [Green Version]
- Couture, J.; Létourneau, A.; Dubuc, A.; Williamson, D. Evaluation of an Electrolyte Repletion Protocol for Cardiac Surgery Intensive Care Patients. Can. J. Hosp. Pharm. 2013, 66, 96–103. [Google Scholar] [CrossRef] [Green Version]
- Hajjaj, F.M.; Salek, M.S.; Basra, M.K.; Finlay, A.Y. Non-clinical influences on clinical decision-making: A major challenge to evidence-based practice. J. R. Soc. Med. 2010, 103, 178–187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ohlsson, H.; Merlo, J. Is physician adherence to prescription guidelines a general trait of health care practices or dependent on drug type?—A multilevel logistic regression analysis in South Sweden. Pharmacoepidemiol. Drug Saf. 2009, 18, 682–690. [Google Scholar] [CrossRef]
- Milchak, J.L.; Carter, B.L.; Ardery, G.; Dawson, J.D.; Harmston, M.; Franciscus, C.L.; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Physician Adherence to Blood Pressure Guidelines and Its Effect on Seniors. Pharmacotherapy 2008, 28, 843–851. [Google Scholar] [CrossRef] [PubMed]
- Oderda, G.M.; Shiozawa, A.; Walsh, M.; Hess, K.; Brixner, D.I.; Feehan, M.; Akhras, K. Physician Adherence to ACR Gout Treatment Guidelines: Perception Versus Practice. Postgrad. Med. 2014, 126, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Joseph, T.T.; DiMeglio, M.; Huffenberger, A.; Laudanski, K. Behavioural patterns of electrolyte repletion in intensive care units: Lessons from a large electronic dataset. Sci. Rep. 2018, 8, 11915. [Google Scholar] [CrossRef]
- O’Grady, N.P.; Barie, P.S.; Bartlett, J.G.; Bleck, T.; Carroll, K.; Kalil, A.C.; Linden, P.; Maki, D.G.; Nierman, D.; Pasculle, W.; et al. Guidelines for evaluation of new fever in critically ill adult patients: 2008 update from the American College of Critical Care Medicine and the Infectious Diseases Society of America. Crit. Care Med. 2008, 36, 1330–1349. [Google Scholar] [CrossRef] [PubMed]
- O’Grady, N.P.; Barie, P.S.; Bartlett, J.; Bleck, T.; Garvey, G.; Jacobi, J.; Linden, P.; Maki, D.G.; Nam, M. Practice Parameters for Evaluating Fever in Critically Ill Adult Patients. Crit. Care Med. 1998, 26, 392–408. [Google Scholar] [CrossRef] [PubMed]
- Anadani, M.; Arthur, A.S.; Tsivgoulis, G.; Simpson, K.N.; Alawieh, A.; Orabi, Y.; Goyal, N.; Alexandrov, A.V.; Maier, I.L.; Psychogios, M.; et al. Blood Pressure Goals and Clinical Outcomes after Successful Endovascular Therapy: A Multicenter Study. Ann. Neurol. 2020, 87, 830–839. [Google Scholar] [CrossRef] [PubMed]
- Blythe, R.; Cook, D.; Graves, N. Scepticaemia: The impact on the health system and patients of delaying new treatments with uncertain evidence; a case study of the sepsis bundle. F1000Res 2018, 7, 500. [Google Scholar] [CrossRef]
- Pruinelli, L.; Yadav, P.; Hangsleben, A.; Johnson, J.; Dey, S.; Mccarty, M.; Kumar, V.; Delaney, C.W.; Steinbach, M.; Westra, B.L.; et al. A Data Mining Approach to Determine Sepsis Guideline Impact on Inpatient Mortality and Complications. AMIA Jt. Summits Transl. Sci. Proc. 2016, 2016, 194–202. [Google Scholar]
- Romero, B.; Fry, M.; Roche, M. The impact of evidence-based sepsis guidelines on emergency department clinical practice: A pre-post medical record audit. J. Clin. Nurs. 2017, 26, 3588–3596. [Google Scholar] [CrossRef] [PubMed]
- Williams, L.-M.S.; Johnson, E.; Armaignac, D.L.; Nemeth, L.S.; Magwood, G.S. A Mixed Methods Study of Tele-ICU Nursing Interventions to Prevent Failure to Rescue of Patients in Critical Care. Telemed. E-Health 2019, 25, 369–379. [Google Scholar] [CrossRef]
- Pickering, B.W.; Gajic, O.; Ahmed, A.; Herasevich, V.; Keegan, M.T. Data Utilization for Medical Decision Making at the Time of Patient Admission to ICU. Crit. Care Med. 2013, 41, 1502–1510. [Google Scholar] [CrossRef] [PubMed]
- Starmer, A.J.; Spector, N.D.; Srivastava, R.; West, D.C.; Rosenbluth, G.; Allen, A.D.; Noble, E.L.; Tse, L.L.; Dalal, A.K.; Keohane, C.A.; et al. Changes in Medical Errors after Implementation of a Handoff Program. N. Engl. J. Med. 2014, 371, 1803–1812. [Google Scholar] [CrossRef] [PubMed]
- Starmer, A.J.; Sectish, T.C.; Simon, D.W.; Keohane, C.; McSweeney, M.E.; Chung, E.Y.; Yoon, C.S.; Lipsitz, S.R.; Wassner, A.J.; Harper, M.B.; et al. Rates of Medical Errors and Preventable Adverse Events Among Hospitalized Children Following Implementation of a Resident Handoff Bundle. JAMA 2013, 310, 2262–2270. [Google Scholar] [CrossRef] [Green Version]
- Smolders, M.; Laurant, M.; Verhaak, P.; Prins, M.; van Marwijk, H.; Penninx, B.; Wensing, M.; Grol, R. Which Physician and Practice Characteristics are Associated With Adherence to Evidence-Based Guidelines for Depressive and Anxiety Disorders? Med. Care 2010, 48, 240–248. [Google Scholar] [CrossRef] [Green Version]
- Djulbegovic, B.; Hamm, R.M.; Mayrhofer, T.; Hozo, I.; Hozo, I.; Van den Ende, J. Rationality, practice variation and person-centred health policy: A threshold hypothesis. J. Eval. Clin. Pract. 2015, 21, 1121–1124. [Google Scholar] [CrossRef] [Green Version]
- The R Project for Statistical Computing, CRAN. Available online: https://www.cran.com (accessed on 23 December 2021).
- Johnson, D.D.; Blumstein, D.T.; Fowler, J.H.; Haselton, M.G. The evolution of error: Error management, cognitive constraints, and adaptive decision-making biases. Trends Ecol. Evol. 2013, 28, 474–481. [Google Scholar] [CrossRef]
- Kushimoto, S.; Abe, T.; Ogura, H.; Shiraishi, A.; Saitoh, D.; Fujishima, S.; Mayumi, T.; Hifumi, T.; Shiino, Y.; Nakada, T.A.; et al. Impact of Body Temperature Abnormalities on the Implementation of Sepsis Bundles and Outcomes in Patients With Severe Sepsis: A Retrospective Sub-Analysis of the Focused Outcome Research on Emergency Care for Acute Respiratory Distress Syndrome, Sepsis and Trauma Study. Crit. Care Med. 2019, 47, 691–699. [Google Scholar]
- Westhorpe, R.N.; Ludbrook, G.L.; Helps, S.C. Crisis management during anaesthesia: Bronchospasm. Qual. Saf. Health Care 2005, 14, e7. [Google Scholar] [CrossRef] [Green Version]
- Pérez-Fernández, X.; Sabater-Riera, J.; Ballus-Noguera, J.; Cárdenas-Campos, P.; Moreno-González, G.; Alonso-Juste, V.; Corral-Velez, V.; Gutierrez-Arámbula, D.; Gumucio-Sanguino, V.; Betbesé-Roig, A.; et al. No impact of surviving sepsis campaign care bundles in reducing sepsis-associated acute kidney injury. Clin. Nephrol. 2017, 88, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.T.; Bussell, J.K. Medication Adherence: WHO Cares? Mayo Clin. Proc. 2011, 86, 304–314. [Google Scholar] [CrossRef] [Green Version]
- Pearson, D.J.; Sharma, A.; Lospinoso, J.A.; Morris, M.J.; McCann, E.T. Effects of Electrolyte Replacement Protocol Implementation in a Medical Intensive Care Unit. J. Intensiv. Care Med. 2016, 33, 574–581. [Google Scholar] [CrossRef]
- Volpp, K.G.; Troxel, A.B.; Mehta, S.J.; Norton, L.; Zhu, J.; Lim, R.; Wang, W.; Marcus, N.; Terwiesch, C.; Caldarella, K.; et al. Effect of Electronic Reminders, Financial Incentives, and Social Support on Outcomes After Myocardial Infarction: The HeartStrong Randomized Clinical Trial. JAMA Intern. Med. 2017, 177, 1093–1101. [Google Scholar] [CrossRef] [Green Version]
- Choudhry, N.K.; Krumme, A.A.; Ercole, P.M.; Girdish, C.; Tong, A.Y.; Khan, N.F.; Brennan, T.A.; Matlin, O.S.; Shrank, W.H.; Franklin, J.M. Effect of Reminder Devices on Medication Adherence: The REMIND Randomized Clinical Trial. JAMA Intern. Med. 2017, 177, 624–631. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Zhao, Y.; Canes, A.; Steinberg, D.; Lyashevska, O.; written on behalf of AME Big-Data Clinical Trial Collaborative Group. Predictive analytics with gradient boosting in clinical medicine. Ann. Transl. Med. 2019, 7, 152. [Google Scholar] [CrossRef]
- Schusterschitz, N.; Joannidis, M. Predictive Capacity of Severity Scoring Systems in the ICU. Contrib. Nephrol. 2007, 156, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Pierce, M.; Gudowski, S.; Roberts, K.; Scott, M.; Laudanski, K. Establishing a Telemedicine Respiratory Therapy Service (eRT) in the COVID-19 Pandemic. J. Cardiothorac. Vasc. Anesth. 2021, 35, 1268–1269. [Google Scholar] [CrossRef] [PubMed]
- Cirillo, D.; Catuara-Solarz, S.; Morey, C.; Guney, E.; Subirats, L.; Mellino, S.; Gigante, A.; Valencia, A.; Rementeria, M.J.; Chadha, A.S.; et al. Sex and gender differences and biases in artificial intelligence for biomedicine and healthcare. NPJ Digit. Med. 2020, 3, 1–11. [Google Scholar] [CrossRef]
- Yu, R. Stress potentiates decision biases: A stress induced deliberation-to-intuition (SIDI) model. Neurobiol. Stress 2016, 3, 83–95. [Google Scholar] [CrossRef] [Green Version]
| Medication Group | Medication Names Included in Group |
|---|---|
| Antipyretics | Acetaminophen, Acetaminophen Suppository, Acetaminophen Oral Liquid, Acetaminophen Tablet. |
| Inhalers | Albuterol Inhaler, Albuterol-Ipratropium Inhaler, Ipratropium-Albuterol Nebulization, Beclomethasone 80 micrograms Inhaler, Ipratropium Inhaler, Levalbuterol 0.63 mg/3 mL Solution, Tiotropium Bromide. |
| Vasodilators | Hydralazine, Hydralazine Injection. |
| Control Group | Controls |
|---|---|
| Unit/Hospital Level | Hospital |
| Unit | |
| Patient/Medication Level | Patient Gender |
| Patient Age | |
| Patient Complexity | |
| Primary Diagnosis Code | |
| Total ICU Stay Elapsed | |
| Pre-Order Health State | |
| Time-Related Controls | Year Medication Ordered |
| Month Medication Ordered | |
| Hour Medication Ordered |
| Measure | Summary Statistic (units) |
|---|---|
| Patient Age | 61.4 ± 15.8 ( ± SD) |
| Patient Gender | 43% Female |
| ICU Length of Stay | 6 ± 7 days ( ± SD); median length of stay of 3.7 days (interquartile range of 1.9 days to 7.2 days) |
| Discharge Destinations | 59% discharge to home; 33% discharge to a long-term care facility or nursing home; 8% of patients expire during the stay. |
| Model (1) Antipyretic Delay | Model (2) Inhaler Delay | Model (3) Vasodilator Delay | |
|---|---|---|---|
| Shift Change IV | 60.81 *** (3.14) | 39.51 *** (3.91) | 57.11 *** (2.06) |
| Other Pt Delay IV (mins) | 0.56 *** (0.01) | 0.76 *** (0.02) | 0.21 *** (0.01) |
| Pre-Vital Sign Controls | Yes | Yes | Yes |
| Unit Controls | Yes | Yes | Yes |
| Patient Controls | Yes | Yes | Yes |
| Time Controls | Yes | Yes | Yes |
| Observations | 14,474 | 14,474 | 14,474 |
| Adjusted R2 | 0.25 | 0.08 | 0.12 |
| F-Statistic | 1752.7 *** | 1117.6 *** | 1015.0 *** |
| Antipyretic Delay High Temp (F) | Inhaler Delay High RR (Bpm) | Vasodilator Delay High MAP (mmHg) | ||||
|---|---|---|---|---|---|---|
| Model (4) | Model (5) | Model (6) | Model (7) | Model (8) | Model (9) | |
| Medication Delay (min) | 0.54% * (0.22%) | 0.10%(0.08%) | 1.06% * (0.45%) | −0.05% (0.13%) | 2.99% *** (0.70%) | 1.05% *** (0.27%) |
| Year | −8.79% * (4.45%) | −9.14% * (4.44%) | −4.83% (2.78%) | −4.91% (2.78%) | 1.61%(2.92%) | 1.65%(2.91%) |
| Month | −2.44% * (1.22%) | −2.47% * (1.22%) | −1.22% (0.78%) | −1.16% (0.78%) | −0.05% (0.84%) | −0.06% (0.84%) |
| Hour | 0.23%(0.49%) | 0.29%(0.49%) | 0.04%(0.33%) | 0.05%(0.33%) | −0.90% * (0.37%) | −0.89% * (0.37%) |
| Gender: Male | 26.64% ** (8.18%) | 26.64% ** (8.17%) | −7.17% (5.05%) | −7.51% (5.04%) | 19.07% ** (5.57%) | 19.28% ** (5.57%) |
| Age | −1.00% *** (0.27%) | −1.00% *** (0.27%) | 0.40% * (0.18%) | 0.41% * (0.18%) | −0.72% *** (0.19%) | −0.72% *** (0.19%) |
| Comorbidities 1 | 1.03% ** (0.35%) | 1.04% ** (0.35%) | 1.16% *** (0.23%) | 1.15% *** (0.23%) | −0.56% * (0.26%) | −0.57% * (0.26%) |
| IV Used | Yes | No | Yes | No | Yes | No |
| Naïve OLS | No | Yes | No | Yes | No | Yes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meng, L.; Laudanski, K.; Restrepo, M.; Huffenberger, A.; Terwiesch, C. The Impact of Delayed Symptomatic Treatment Implementation in the Intensive Care Unit. Healthcare 2022, 10, 35. https://doi.org/10.3390/healthcare10010035
Meng L, Laudanski K, Restrepo M, Huffenberger A, Terwiesch C. The Impact of Delayed Symptomatic Treatment Implementation in the Intensive Care Unit. Healthcare. 2022; 10(1):35. https://doi.org/10.3390/healthcare10010035
Chicago/Turabian StyleMeng, Lesley, Krzysztof Laudanski, Mariana Restrepo, Ann Huffenberger, and Christian Terwiesch. 2022. "The Impact of Delayed Symptomatic Treatment Implementation in the Intensive Care Unit" Healthcare 10, no. 1: 35. https://doi.org/10.3390/healthcare10010035
APA StyleMeng, L., Laudanski, K., Restrepo, M., Huffenberger, A., & Terwiesch, C. (2022). The Impact of Delayed Symptomatic Treatment Implementation in the Intensive Care Unit. Healthcare, 10(1), 35. https://doi.org/10.3390/healthcare10010035







