Association between Perceived Trusted of COVID-19 Information Sources and Mental Health during the Early Stage of the Pandemic in Bangladesh
Abstract
:1. Introduction
1.1. Literature Review
1.1.1. Misinformation and Mental Health
1.1.2. Sources and Impacts of Misinformation during the COVID-19 Pandemic
1.1.3. The COVID-19 Pandemic, Misinformation, and Mental Health in Bangladesh
1.2. Current Study
- RQ 1.
- How does perceived trust in sources of COVID-19 information vary by demographic/residency characteristics and frontline service provider status?
- RQ 2.
- To what extent does perceived trust in sources of COVID-19 information relate to COVID-19 stressors and mental health?
- RQ 3.
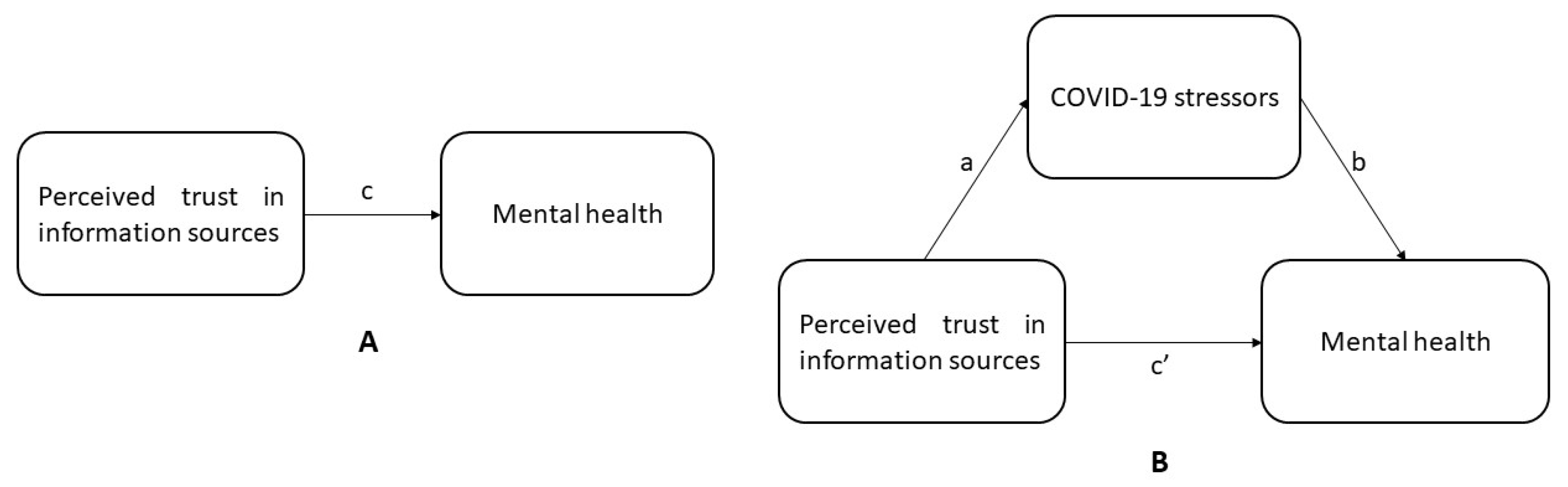
- Do COVID-19 stressors mediate associations between perceived trust in sources of COVID-19 information and mental health?
2. Materials and Methods
2.1. Study Design and Respondents
2.2. Survey Measures
2.2.1. Perceived Trust in Information Sources
2.2.2. COVID-19 Related Stressors
2.2.3. Mental Health
2.2.4. Covariates
2.3. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Variations in Perceived Trust in Information Sources by Demographics, Residency, and Frontline Service Provider Status
3.3. Associations between Perceived Trust in Information Sources, COVID-19 Related Stressors, and Mental Health
3.4. Mediating Effects of COVID-19 Related Stressors on Perceived Trust in Information Sources and Mental Health
4. Discussion
4.1. Summary of Study and Main Findings
4.2. Implications of Study Findings
4.3. Study Limitations and Future Research Recommendations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Questionnaire
- What is your gender?
- Female
- Male
- What is your age group?
- ≤30
- >30
- What is your educational qualification?
- School level (Primary/SSC or equivalent)
- College level (HSC or equivalent)
- Undergraduate
- Graduate
- Postgraduate
- Other:
- What is your current area of residence?
- Urban (City/Municipality/town area)
- Rural (village)
- What is your current household status? (You can select more than one of the below options if applicable)
- Living alone
- Living with family (including spouse, children, or extended family)
- Living with non-family members (e.g., housemates or college/university accommodation or supported accommodation)
- What is your current occupation?
- Unemployed
- Student
- Government
- Non-government
- Healthcare
- Pharmaceuticals
- Banker
- Police
- Housewife
- Self-employed
- Other (please specify)
- Do you or have you engaged in any frontline roles during the COVID-19 pandemic?
- Yes
- No
- 8.
- From where have you received information about COVID-19? (You can select more than one options if applicable)
- Government health agency websites (e.g., IEDCR, DG Health, Ministry of Health)
- International agencies (e.g., WHO)
- Health professional (i.e., doctor, nurse, health workers etc.)
- Friends or family
- Social media (e.g., Twitter, Facebook, YouTube, Instagram)
- Newspapers
- Television, Radio
- University website
- Online news portal
- Other…
- 9.
- How reliable is COVID-19 information from the following sources?
- Government health agencies (e.g., IEDCR, DG health)
- Not at all A little Quite a lot A great deal
- International health agencies (e.g., WHO)
- Not at all A little Quite a lot A great deal
- Healthcare personnel
- Not at all A little Quite a lot A great deal
- Social media (e.g., Twitter, Facebook, YouTube, Instagram)
- Not at all A little Quite a lot A great deal
- Newspapers
- Not at all A little Quite a lot A great deal
- Television, Radio
- Not at all A little Quite a lot A great deal
- Online news portals
- Not at all A little Quite a lot A great deal
- 10.
- Did you experience any of the following worrisome situations during COVID-19?
- Quarantine or self-isolation.
- Yes No
- Family, relative, or close acquaintances diagnosed with COVID-19 in the last two weeks.
- Yes No
- Overhearing someone discussing negative news about the severity of COVID-19.
- Yes No
- Believing that COVID-19 interfered with your daily activities.
- Yes No
- 11.
- Over the last 2 weeks, how often have you been bothered by any of the following problems?
- Feeling nervous or anxious
- Not at all Several days More than half of the days Almost everyday
- Not able to stop or control worrying
- Not at all Several days More than half of the days Almost everyday
- Worrying too much about different things
- Not at all Several days More than half of the days Almost everyday
- Having trouble to relax body and mind
- Not at all Several days More than half of the days Almost everyday
- Being so restless that it is hard to sit quietly
- Not at all Several days More than half of the days Almost everyday
- Becoming easily annoyed or irritable
- Not at all Several days More than half of the days Almost everyday
- Feeling afraid as if something awful might happen
- Not at all Several days More than half of the days Almost everyday
- 12.
- Perceived stress during COVID-19In the last four weeks of lockdown how often you felt?
- ……unable to control the important things in your life
- Never Almost never Sometimes Fairly often Very Often
- ……confident about your ability to handle your personal problems
- Never Almost never Sometimes Fairly often Very Often
- ……things were going your way
- Never Almost never Sometimes Fairly often Very Often
- ……difficulties were piling up so high that you could not overcome them
- Never Almost never Sometimes Fairly often Very Often
References
- Hua, J.; Shaw, R. Corona virus (COVID-19) “infodemic” and emerging issues through a data lens: The case of china. Int. J. Environ. Res. Public Health 2020, 17, 2309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taheri, M.S.; Falahati, F.; Radpour, A.; Karimi, V.; Sedaghat, A.; Karimi, M.A. Role of Social Media and Telemedicine in Diagnosis & Management of COVID-19; An Experience of the Iranian Society of Radiology. Arch. Iran Med. Acad. Med. Sci. I.R. Iran 2020, 23, 285–286. [Google Scholar] [CrossRef] [Green Version]
- WHO Weekly Operational Update on COVID-19—4 August 2021. Available online: https://www.who.int/publications/m/item/weekly-operational-update-on-covid-19---4-august-2021 (accessed on 5 August 2021).
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef] [Green Version]
- Bilal; Latif, F.; Bashir, M.F.; Komal, B.; Tan, D. Role of electronic media in mitigating the psychological impacts of novel coronavirus (COVID-19). Psychiatry Res. 2020, 289, 113041. [Google Scholar] [CrossRef]
- Mia, M.A.; Griffiths, M.D. Can South Asian Countries Cope with the Mental Health Crisis Associated with COVID-19? Int. J. Ment. Health Addict. 2021, 1–10. [Google Scholar] [CrossRef]
- Patwary, M.M.; Hossain, M.R.; Shuvo, F.K.; Ashraf, S.; Sultana, R.; Alam, M.A. Protecting Sanitation Workers in Low-Middle Income Countries Amid COVID-19. Ann. Work Expo. Health 2021. [Google Scholar] [CrossRef]
- Hopman, J.; Allegranzi, B.; Mehtar, S. Managing COVID-19 in Low- and Middle-Income Countries. JAMA J. Am. Med. Assoc. 2020, 323, 1549–1550. [Google Scholar] [CrossRef]
- Ippolito, G.; Hui, D.S.; Ntoumi, F.; Maeurer, M.; Zumla, A. Toning down the 2019-nCoV media hype—and restoring hope. Lancet Respir. Med. 2020, 8, 230–231. [Google Scholar] [CrossRef] [Green Version]
- Smith, G.D.; Ng, F.; Ho Cheung Li, W. COVID-19: Emerging compassion, courage and resilience in the face of misinformation and adversity. J. Clin. Nurs. 2020, 29, 1425–1428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiao, Y.; Torok, M.E. Taking the right measures to control COVID-19. Lancet Infect. Dis. 2020, 20, 523–524. [Google Scholar] [CrossRef] [Green Version]
- Chou, W.Y.S.; Oh, A.; Klein, W.M.P. Addressing Health-Related Misinformation on Social Media. JAMA J. Am. Med. Assoc. 2018, 320, 2417–2418. [Google Scholar] [CrossRef] [PubMed]
- Cuan-Baltazar, J.Y.; Muñoz-Perez, M.J.; Robledo-Vega, C.; Pérez-Zepeda, M.F.; Soto-Vega, E. Misinformation of COVID-19 on the internet: Infodemiology study. JMIR Public Health Surveill. 2020, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bendau, A.; Petzold, M.B.; Pyrkosch, L.; Mascarell Maricic, L.; Betzler, F.; Rogoll, J.; Große, J.; Ströhle, A.; Plag, J. Associations between COVID-19 related media consumption and symptoms of anxiety, depression and COVID-19 related fear in the general population in Germany. Eur. Arch. Psychiatry Clin. Neurosci. 2021, 271, 283–291. [Google Scholar] [CrossRef]
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 2020, 15, e0231924. [Google Scholar] [CrossRef]
- Lewis, T. Seeking health information on the internet: Lifestyle choice or bad attack of cyberchondria? Media Cult. Soc. 2016, 28, 521–539. [Google Scholar] [CrossRef]
- Silver, R.C.; Holman, E.A.; Andersen, J.P.; Poulin, M.; McIntosh, D.N.; Gil-Rivas, V. Mental- and Physical-Health Effects of Acute Exposure to Media Images of the September 11, 2001, Attacks and the Iraq War. Psychol. Sci. 2013. [Google Scholar] [CrossRef] [Green Version]
- CNN Fearing Coronavirus, Arizona Man Dies after Taking a Form of Chloroquine Used in Aquariums—CNN. Available online: https://edition.cnn.com/2020/03/23/health/arizona-coronavirus-chloroquine-death/index.html (accessed on 3 December 2021).
- Garfin, D.R.; Silver, R.C.; Holman, E.A. The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychol. 2020, 39, 355–357. [Google Scholar] [CrossRef]
- Hassan, T.; Alam, M.M.; Wahab, A.; Hawlader, M.D. Prevalence and associated factors of internet addiction among young adults in Bangladesh. J. Egypt. Public Health Assoc. 2020, 95. [Google Scholar] [CrossRef]
- Bastani, P.; Bahrami, M.A. COVID-19 Related Misinformation on Social Media: A Qualitative Study from Iran (Preprint). J. Med. Internet Res. 2020. [Google Scholar] [CrossRef]
- BBC Social Media Firms Fail to Act on COVID-19 Fake News—BBC News. Available online: https://www.bbc.com/news/technology-52903680 (accessed on 2 December 2021).
- Li, H.O.Y.; Bailey, A.; Huynh, D.; Chan, J. YouTube as a source of information on COVID-19: A pandemic of misinformation? BMJ Glob. Health 2020, 5. [Google Scholar] [CrossRef]
- Naeem, S.B.; Bhatti, R.; Khan, A. An exploration of how fake news is taking over social media and putting public health at risk. Health Info. Libr. J. 2021, 38, 143–149. [Google Scholar] [CrossRef]
- WHO Call for Action: Managing the Infodemic. Available online: https://www.who.int/news/item/11-12-2020-call-for-action-managing-the-infodemic (accessed on 10 December 2020).
- Zandifar, A.; Badrfam, R. Iranian mental health during the COVID-19 epidemic. Asian J. Psychiatr. 2020, 51, 101990. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, A.R.; Murad, H.R. The impact of social media on panic during the COVID-19 pandemic in iraqi kurdistan: Online questionnaire study. J. Med. Internet Res. 2020, 22, e19556. [Google Scholar] [CrossRef] [PubMed]
- Chu, L.; Fung, H.H.; Tse, D.C.K.; Tsang, V.H.L.; Zhang, H.; Mai, C. Obtaining Information from Different Sources Matters during the COVID-19 Pandemic. Gerontologist 2021. [Google Scholar] [CrossRef]
- Mongkhon, P.; Ruengorn, C.; Awiphan, R.; Thavorn, K.; Hutton, B.; Wongpakaran, N.; Wongpakaran, T.; Nochaiwong, S. Exposure to COVID-19-related information and its association with mental health problems in thailand: Nationwide, cross-sectional survey study. J. Med. Internet Res. 2021, 23, e25363. [Google Scholar] [CrossRef]
- Ko, C.H.; Yen, C.F.; Yen, J.Y.; Yang, M.J. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry Clin. Neurosci. 2006, 60, 397–403. [Google Scholar] [CrossRef] [Green Version]
- Valkenburg, P.M.; Peter, J. The differential susceptibility to media effects model. J. Commun. 2013, 63, 221–243. [Google Scholar] [CrossRef]
- Thompson, R.R.; Garfin, D.R.; Holman, E.A.; Silver, R.C. Distress, Worry, and Functioning following a Global Health Crisis: A National Study of Americans’ Responses to Ebola. Clin. Psychol. Sci. 2017, 5, 513–521. [Google Scholar] [CrossRef] [Green Version]
- Thompson, R.R.; Jones, N.M.; Holman, E.A.; Silver, R.C. Media exposure to mass violence events can fuel a cycle of distress. Sci. Adv. 2019, 5. [Google Scholar] [CrossRef] [Green Version]
- Zhao, N.; Zhou, G. Social Media Use and Mental Health during the COVID-19 Pandemic: Moderator Role of Disaster Stressor and Mediator Role of Negative Affect. Appl. Psychol. Health Well-Being 2020, 12, 1019–1038. [Google Scholar] [CrossRef] [PubMed]
- Houston, J.B.; Spialek, M.L.; First, J. Disaster media effects: A systematic review and synthesis based on the differential susceptibility to media effects model. J. Commun. 2018, 68, 734–757. [Google Scholar] [CrossRef]
- IEDCR. Institute of Epidemiology Disease Control and Research 2020. COVID-19 Status Bangladesh. Available online: https://www.iedcr.gov.bd (accessed on 7 May 2020).
- Anwar, S.; Nasrullah, M.; Hosen, M.J. COVID-19 and Bangladesh: Challenges and How to Address Them. Front. Public Health 2020. [Google Scholar] [CrossRef]
- Hossain, M.R.; Patwary, M.M.; Sultana, R.; Browning, M.H.E.M. Psychological Distress among Healthcare Professionals during the Early Stages of the COVID-19 Outbreak in Low Resource Settings: A Cross-Sectional Study in Bangladesh. Front. Public Health 2021, 9. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, M.; Begum, S.; Ahmed, T. Vulnerabilities to COVID-19 in Bangladesh and a Reconsideration of Sustainable Development Goals. Sustainability 2020, 12, 5296. [Google Scholar] [CrossRef]
- Patwary, M.M.; Bardhan, M.; Disha, A.S.; Kabir, M.P.; Hossain, M.R.; Alam, M.A.; Haque, M.Z.; Billah, S.M. The Impact of COVID-19 Pandemic on Mental Health of University Student: A Cross-Sectional Study in Bangladesh. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Worldometer Bangladesh COVID: 1,353,695 Cases and 22,652 Deaths—Worldometer. Available online: https://www.worldometers.info/coronavirus/country/bangladesh/ (accessed on 9 August 2021).
- Chisty, M.A.; Islam, M.A.; Munia, A.T.; Rahman, M.M.; Rahman, N.N.; Mohima, M. Risk perception and information-seeking behavior during emergency: An exploratory study on COVID-19 pandemic in Bangladesh. Int. J. Disaster Risk Reduct. 2021, 65. [Google Scholar] [CrossRef] [PubMed]
- Patwary, M.M.; Bardhan, M.; Disha, A.S.; Hasan, M.; Haque, M.Z.; Sultana, R.; Hossain, M.R.; Browning, M.H.E.M.; Alam, M.A.; Sallam, M. Determinants of COVID-19 Vaccine Acceptance among the Adult Population of Bangladesh Using the Health Belief Model and the Theory of Planned Behavior Model. Vaccines 2021, 9, 1393. [Google Scholar] [CrossRef]
- Hossain, Z.; Hashmi, Y.; Mezbah-ul-Islam, M. ICT Facilities and Literacy in Rural Non-Government Secondary School Libraries of Bangladesh. Sch. Libr. Worldw. 2019, 25, 66–80. [Google Scholar]
- Al-Zaman, M.S. COVID-19-related online misinformation in Bangladesh. J. Health Res. 2021, 35, 364–368. [Google Scholar] [CrossRef]
- Barua, Z.; Barua, S.; Aktar, S.; Kabir, N.; Li, M. Effects of misinformation on COVID-19 individual responses and recommendations for resilience of disastrous consequences of misinformation. Prog. Disaster Sci. 2020, 8. [Google Scholar] [CrossRef]
- Aziz, A.; Islam, M.M.; Zakaria, M. COVID-19 exposes digital divide, social stigma, and information crisis in Bangladesh. Media Asia 2020, 47, 144–151. [Google Scholar] [CrossRef]
- Shawki, A. Govt Asks Facebook to Delete Pages Spreading COVID-19 Rumours. Available online: https://www.tbsnews.net/coronavirus-chronicle/covid-19-bangladesh/govt-asks-facebook-delete-pages-spreading-covid-19-rumours (accessed on 2 December 2021).
- Al-Zaman, M.S.; Sayeed Al-Zaman, M. Healthcare crisis in Bangladesh during the COVID-19 pandemic. Am. J. Trop. Med. Hyg. 2020, 103, 1357–1359. [Google Scholar] [CrossRef]
- Fakhruddin, B.; Blanchard, K.; Ragupathy, D. Are we there yet? The transition from response to recovery for the COVID-19 pandemic. Prog. Disaster Sci. 2020, 7. [Google Scholar] [CrossRef] [PubMed]
- Sultana, S.; Fussell, S.R. Dissemination, Situated Fact-checking, and Social Effects of Misinformation among Rural Bangladeshi Villagers During the COVID-19 Pandemic. Proc. ACM Human-Comput. Interact. 2021, 5, 1–34. [Google Scholar] [CrossRef]
- Laato, S.; Islam, A.K.M.N.; Islam, M.N.; Whelan, E. What drives unverified information sharing and cyberchondria during the COVID-19 pandemic? Eur. J. Inf. Syst. 2020, 29, 288–305. [Google Scholar] [CrossRef]
- Main, A.; Zhou, Q.; Ma, Y.; Luecken, L.J.; Liu, X. Relations of sars-related stressors and coping to chinese college students’ psychological adjustment during the 2003 beijing sars epidemic. J. Couns. Psychol. 2011, 58, 410–423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herrero, J.; Meneses, J. Short Web-based versions of the perceived stress (PSS) and Center for Epidemiological Studies-Depression (CESD) Scales: A comparison to pencil and paper responses among Internet users. Comput. Human Behav. 2006, 22, 830–846. [Google Scholar] [CrossRef]
- Mitchell, A.M.; Crane, P.A.; Kim, Y. Perceived stress in survivors of suicide: Psychometric properties of the perceived stress scale. Res. Nurs. Health 2008, 31, 576–585. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis, Second Edition: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2018; ISBN 9781462534654. [Google Scholar]
- George, D.; Mallery, P. IBM SPSS Statistics 26 Step by Step: A Simple Guide and Reference; Routledge: London, UK, 2019. [Google Scholar] [CrossRef]
- Salman, A.; Al-Ghadban, F.; Sigodo, K.O.; Taher, A.K.; Chun, S. The psychological and social impacts of curfew during the COVID-19 outbreak in kuwait: A cross-sectional study. Sustainability 2021, 13, 8464. [Google Scholar] [CrossRef]
- Ho, H.Y.; Chen, Y.L.; Yen, C.F. Different impacts of COVID-19-related information sources on public worry: An online survey through social media. Internet Interv. 2020, 22, 100350. [Google Scholar] [CrossRef] [PubMed]
- Ni, M.Y.; Yang, L.; Leung, C.M.C.; Li, N.; Yao, X.I.; Wang, Y.; Leung, G.M.; Cowling, B.J.; Liao, Q. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in wuhan, China: Cross-sectional survey. JMIR Ment. Health 2020, 7, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Shokri, A.; Moradi, G.; Piroozi, B.; Darvishi, S.; Amirihosseini, S.; Veysi, A.; Manafi, F.; Bolbanabad, A.M. Perceived stress due to COVID-19 in Iran: Emphasizing the role of social networks. Med. J. Islam. Repub. Iran 2020, 34. [Google Scholar] [CrossRef]
- Moore, R.; Zielinski, M.J.; Thompson, R.G.; Willis, D.E.; Purvis, R.S.; McElfish, P.A. “This Pandemic Is Making Me More Anxious about My Welfare and the Welfare of Others:” COVID-19 Stressors and Mental Health. Int. J. Environ. Res. Public Health 2021, 18, 5680. [Google Scholar] [CrossRef]
- De Coninck, D.; Frissen, T.; Matthijs, K.; d’Haenens, L.; Lits, G.; Champagne-Poirier, O.; Carignan, M.E.; David, M.D.; Pignard-Cheynel, N.; Salerno, S.; et al. Beliefs in Conspiracy Theories and Misinformation About COVID-19: Comparative Perspectives on the Role of Anxiety, Depression and Exposure to and Trust in Information Sources. Front. Psychol. 2021, 12, 1–13. [Google Scholar] [CrossRef]
- Chun Wong, F.H.; Liu, T.; Yi Leung, D.K.; Zhang, A.Y.; Hong Au, W.S.; Kwok, W.W.; Shum, A.K.Y.; Yan Wong, G.H.; Lum, T.Y.S. Consuming information related to COVID-19 on social media among older adults and its association with anxiety, social trust in information, and COVID-safe behaviors: Cross-sectional telephone survey. J. Med. Internet Res. 2021, 23, e26570. [Google Scholar] [CrossRef] [PubMed]
- Henderson, G. How Much Time Does the Average Person Spend on Social Media? Available online: https://www.digitalmarketing.org/blog/how-much-time-does-the-average-person-spend-on-social-media (accessed on 10 December 2021).
- Azad, M.A.K. Bangladesh—Media Landscapes. Available online: https://medialandscapes.org/country/bangladesh (accessed on 10 December 2021).
- Tsai, J.Y.; Phua, J.; Pan, S.; Yang, C.C. Intergroup contact, COVID-19 news consumption, and the moderating role of digital media trust on prejudice toward asians in the United States: Cross-sectional study. J. Med. Internet Res. 2020, 15, 11–24. [Google Scholar] [CrossRef]
- Tusev, A.; Tonon, L.; Capella, M. The Initial Mental Health Effects of the COVID-19 Pandemic Across Some Ecuadorian Provinces. Investigatio 2020, 15, 11–24. [Google Scholar] [CrossRef]
- Lowrey, W. Media Dependency During a Large-Scale Social Disruption: The Case of September 11. Mass Commun. Soc. 2004, 7, 339–357. [Google Scholar] [CrossRef]
- Liu, C.; Liu, Y. Media exposure and anxiety during COVID-19: The mediation effect of media vicarious traumatization. Int. J. Environ. Res. Public Health 2020, 17, 4720. [Google Scholar] [CrossRef]
- Ball-Rokeach, S.J.; Defleur, M.L. A Dependency Model of Mass-Media Effects. Communic. Res. 1976, 3, 3–21. [Google Scholar] [CrossRef]
- Melki, J.; Tamim, H.; Hadid, D.; Makki, M.; El Amine, J.; Hitti, E. Mitigating infodemics: The relationship between news exposure and trust and belief in COVID-19 fake news and social media spreading. PLoS ONE 2021, 16, e0252830. [Google Scholar] [CrossRef] [PubMed]
- Ramsey, S.D.; Zeliadt, S.B.; Arora, N.K.; Potosky, A.L.; Blough, D.K.; Hamilton, A.S.; Van Den Eeden, S.K.; Oakley-Girvan, I.; Penson, D.F. Access to Information Sources and Treatment Considerations Among Men With Local Stage Prostate Cancer. Urology 2009, 74, 509–515. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ko, N.Y.; Lu, W.H.; Chen, Y.L.; Li, D.J.; Wang, P.W.; Hsu, S.T.; Chen, C.C.; Lin, Y.H.; Chang, Y.P.; Yen, C.F. COVID-19-related information sources and psychological well-being: An online survey study in Taiwan. Brain. Behav. Immun. 2020, 87, 153–154. [Google Scholar] [CrossRef] [PubMed]

| Variables | n (%); M (±SD) |
|---|---|
| Gender | |
| Male | 432 (58.06) |
| Female | 312 (41.94) |
| Age | |
| ≤30 | 697 (93.68) |
| >30 | 47 (6.32) |
| Education level | |
| Low (≤college degree) | 51 (6.85) |
| High (>college degree) | 693 (93.15) |
| Urbanicity | |
| Urban | 645 (86.89) |
| Rural | 99 (13.31) |
| Living with family | |
| Yes | 564 (75.81) |
| No | 180 (24.19) |
| Frontline service provider | |
| Yes | 175 (23.52) |
| No | 569 (76.48) |
| COVID-19 related stressors | 2.57 (±1.04) |
| Mental health | |
| Anxiety (GAD-7) | 9.39 (±5.68) |
| Perceived stress (PSS-4) | 6.73 (±2.41) |
| Variables | Health Media, n (%) | Social Media, n (%) | Traditional Media, n (%) | |||
|---|---|---|---|---|---|---|
| High | Low | High | Low | High | Low | |
| Gender | ||||||
| Male | 331 (76.62) | 101 (23.38) | 136 (31.48) | 296 (68.62) | 324 (75.00) | 108 (25) |
| Female | 254 (81.41) | 58 (18.59) | 91 (29.17) | 221 (70.83) | 224 (71.79) | 88 (28.21) |
| Age | ||||||
| ≤30 | 548 (78.62) | 149 (21.38) | 209 (29.99) | 488 (70.01) | 511 (73.31) | 186 (26.69) |
| >30 | 37 (78.72) | 10 (21.28) | 18 (38.30) | 29 (61.70) | 37 (78.72) | 10 (21.28) |
| Education level | ||||||
| Low (≤college degree) | 43 (84.31) | 8 (15.69) | 19 (37.25) * | 32 (62.75) | 41 (80.39) * | 10 (19.61) |
| High (>college degree) | 542 (78.21) | 151 (21.79) | 208 (30.01) | 485 (69.99) | 507 (73.16) | 186 (26.84) |
| Urbanicity | ||||||
| Urban | 516 (80.00) ** | 129 (20.00) | 198 (30.70) * | 447 (69.30) | 477 (73.95) * | 168 (26.05) |
| Rural | 69 (69.70) | 30 (30.30) | 29 (29.29) | 70 (70.71) | 71 (71.72) | 28 (28.28) |
| Living with family | ||||||
| Yes | 453 (80.32) * | 120 (21.28) | 171 (30.32) | 393 (69.68) | 411 (72.87) * | 153 (27.13) |
| No | 132 (73.33) | 39 (21.67) | 56 (31.11) | 124 (68.89) | 137 (76.11) | 43 (23.89) |
| Frontline service provider | ||||||
| Yes | 141 (80.57) | 43 (24.57) | 45 (25.71) | 130 (74.29) | 124 (70.86) | 51 (29.14) |
| No | 444 (78.03) | 116 (20.39) | 182 (31.99) | 387 (68.01) | 424 (74.52) | 145 (25.48) |
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. COVID-19 related stressors | 1 | |||||
| 2. Perceived trust in health media | 0.24 ** | 1 | ||||
| 3. Perceived trust in social media | 0.15 | 0.49 ** | 1 | |||
| 4. Perceived trust in traditional media | 0.24 ** | 0.64 ** | 0.46 ** | 1 | ||
| 5. Anxiety (GAD-7) | 0.21 ** | 0.08 * | 0.03 * | 0.14 ** | 1 | |
| 6. Perceived stress (PSS-4) | −0.04 | −0.05 * | −0.001 * | −0.07 * | 0.04 | 1 |
| Variables | Anxiety (GAD-7) | Perceived Stress (PSS-4) |
|---|---|---|
| Adjusted B (95%CI) | ||
| Perceived trust in health media | −0.03 (−1.18–1.10) | 0.04 (−0.28–0.70) |
| Perceived trust in social media | 0.03 (0.27–0.97) * | 0.01 (−0.34–0.47) * |
| Perceived trust in traditional media | 0.09 (0.17–2.26) * | −0.08 (−0.89–0.03) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patwary, M.M.; Bardhan, M.; Browning, M.H.E.M.; Disha, A.S.; Haque, M.Z.; Billah, S.M.; Kabir, M.P.; Hossain, M.R.; Alam, M.A.; Shuvo, F.K.; et al. Association between Perceived Trusted of COVID-19 Information Sources and Mental Health during the Early Stage of the Pandemic in Bangladesh. Healthcare 2022, 10, 24. https://doi.org/10.3390/healthcare10010024
Patwary MM, Bardhan M, Browning MHEM, Disha AS, Haque MZ, Billah SM, Kabir MP, Hossain MR, Alam MA, Shuvo FK, et al. Association between Perceived Trusted of COVID-19 Information Sources and Mental Health during the Early Stage of the Pandemic in Bangladesh. Healthcare. 2022; 10(1):24. https://doi.org/10.3390/healthcare10010024
Chicago/Turabian StylePatwary, Muhammad Mainuddin, Mondira Bardhan, Matthew H. E. M. Browning, Asma Safia Disha, Md. Zahidul Haque, Sharif Mutasim Billah, Md. Pervez Kabir, Md. Riad Hossain, Md. Ashraful Alam, Faysal Kabir Shuvo, and et al. 2022. "Association between Perceived Trusted of COVID-19 Information Sources and Mental Health during the Early Stage of the Pandemic in Bangladesh" Healthcare 10, no. 1: 24. https://doi.org/10.3390/healthcare10010024
APA StylePatwary, M. M., Bardhan, M., Browning, M. H. E. M., Disha, A. S., Haque, M. Z., Billah, S. M., Kabir, M. P., Hossain, M. R., Alam, M. A., Shuvo, F. K., & Salman, A. (2022). Association between Perceived Trusted of COVID-19 Information Sources and Mental Health during the Early Stage of the Pandemic in Bangladesh. Healthcare, 10(1), 24. https://doi.org/10.3390/healthcare10010024










