Using Simulation Optimization to Solve Patient Appointment Scheduling and Examination Room Assignment Problems for Patients Undergoing Ultrasound Examination
Abstract
1. Introduction
2. Literature Review
2.1. Patient Appointment Scheduling
2.2. Hospital System Simulation
2.3. A Summary
3. Methodology
3.1. Research Problem
3.2. Research Procedure
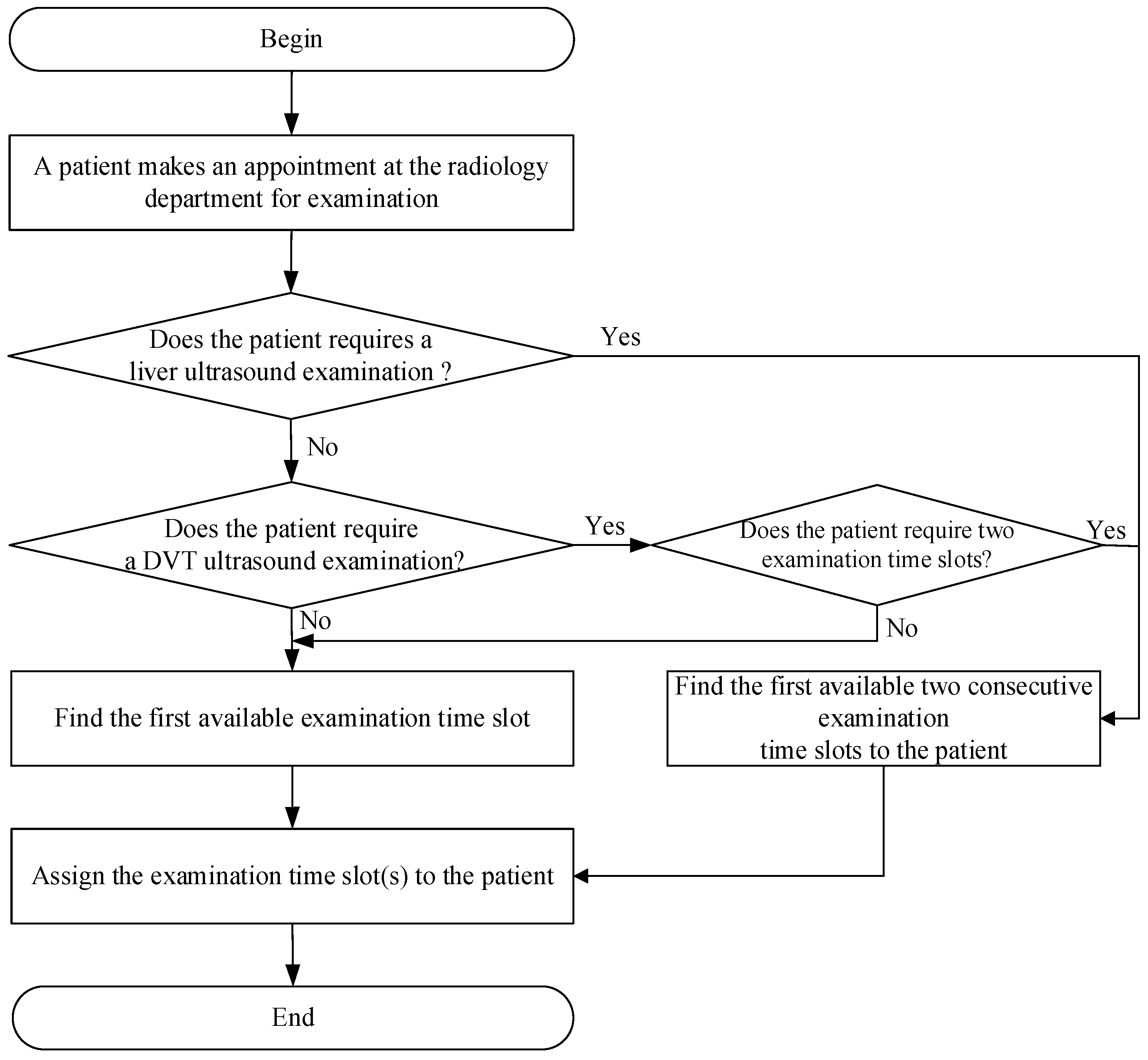
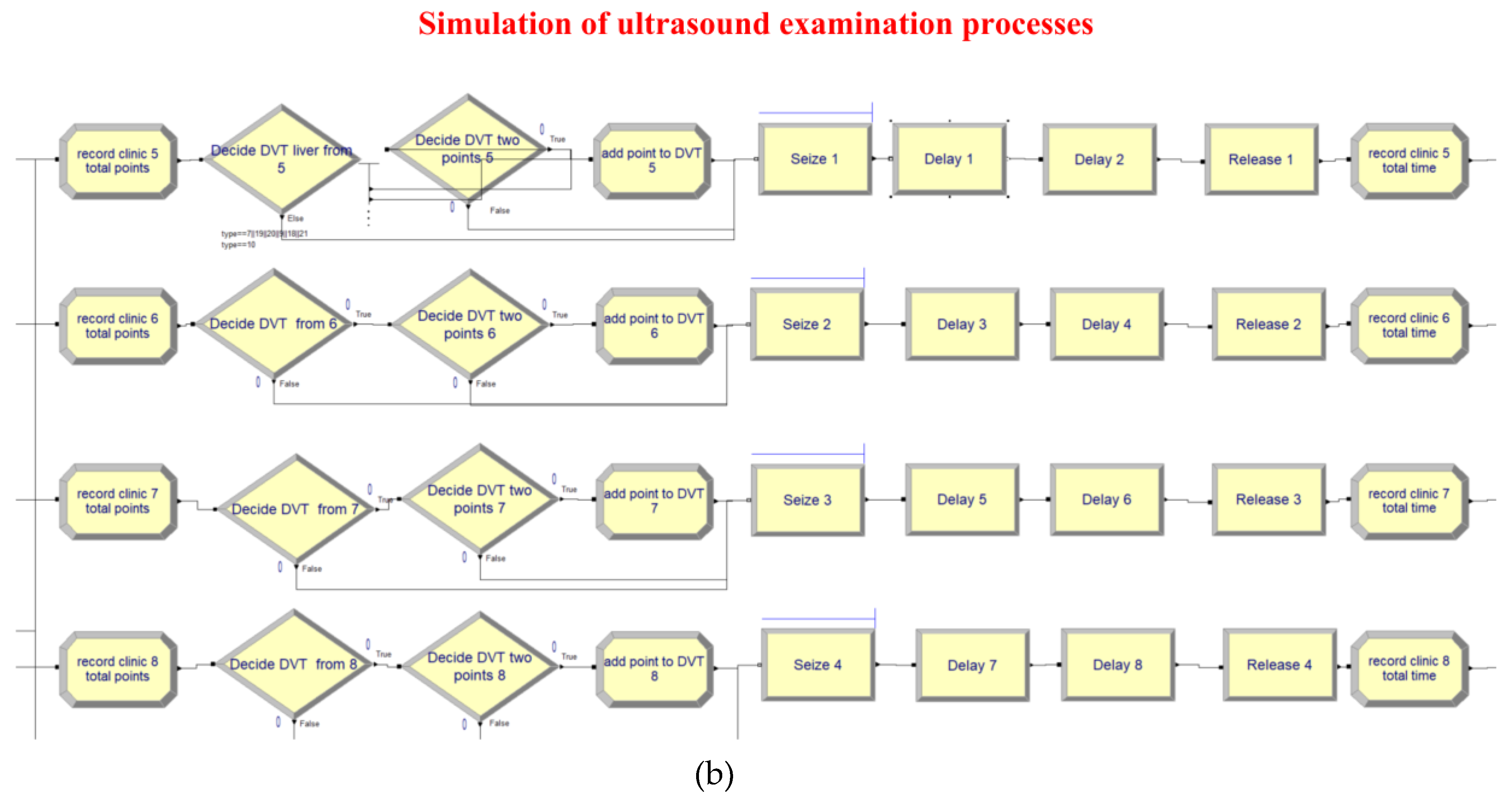
3.3. Appointment Scheduling Process for Patients Undergoing Ultrasound Examination
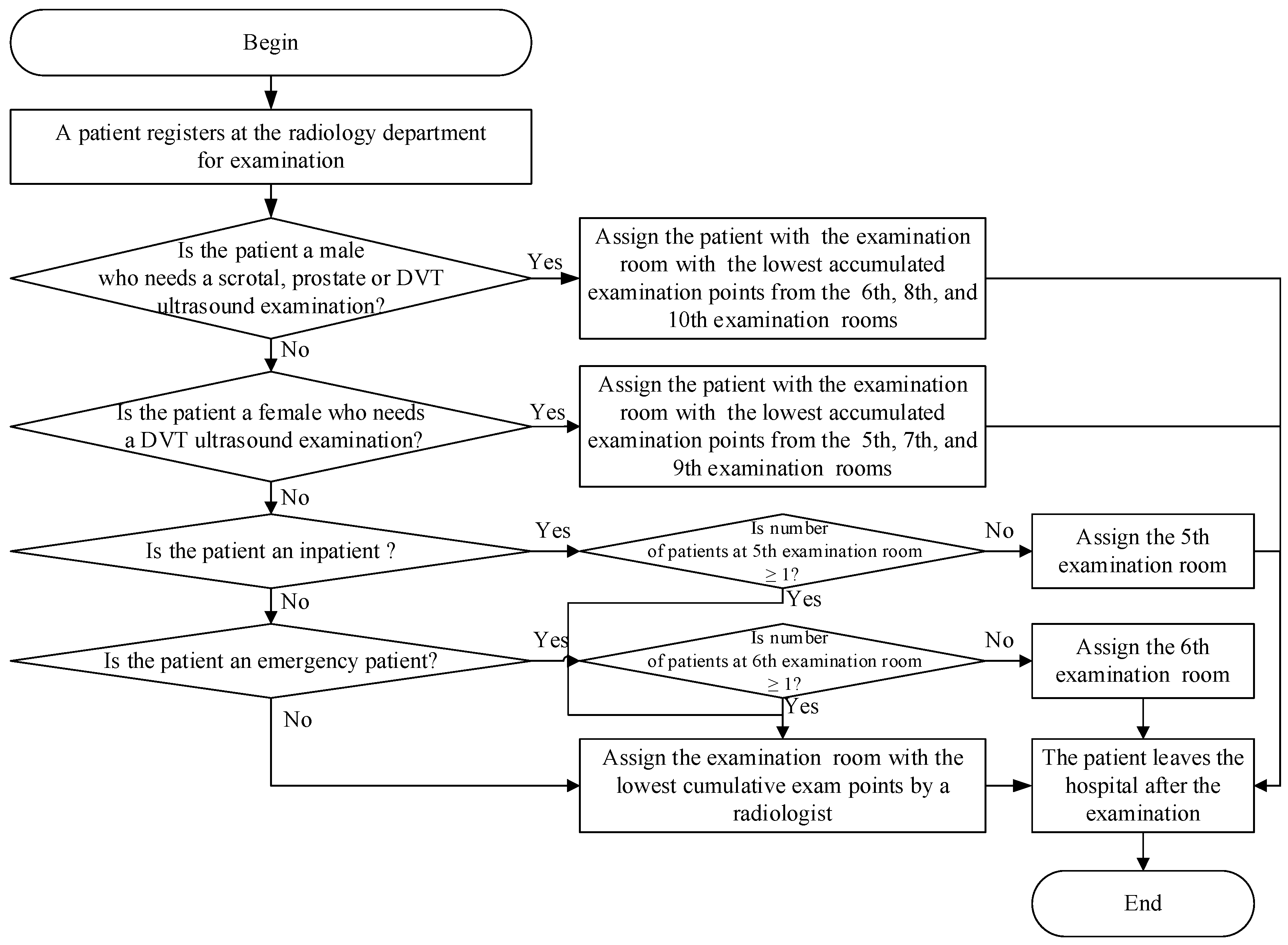
3.4. Examination Room Assignment for Patients Undergoing Ultrasound Examination
4. Analysis and Discussion
4.1. Background of Case Study
4.2. Data Regarding Patients Undergoing Ultrasound Examination
4.3. Data Fitting Analysis
4.4. Simulation Assumptions
- (1)
- Extremely small body parts were excluded from this study.
- (2)
- There was no degradation in service quality or time provided to patients.
- (3)
- We assumed that patients had received proper information during pre-examination procedures.
- (4)
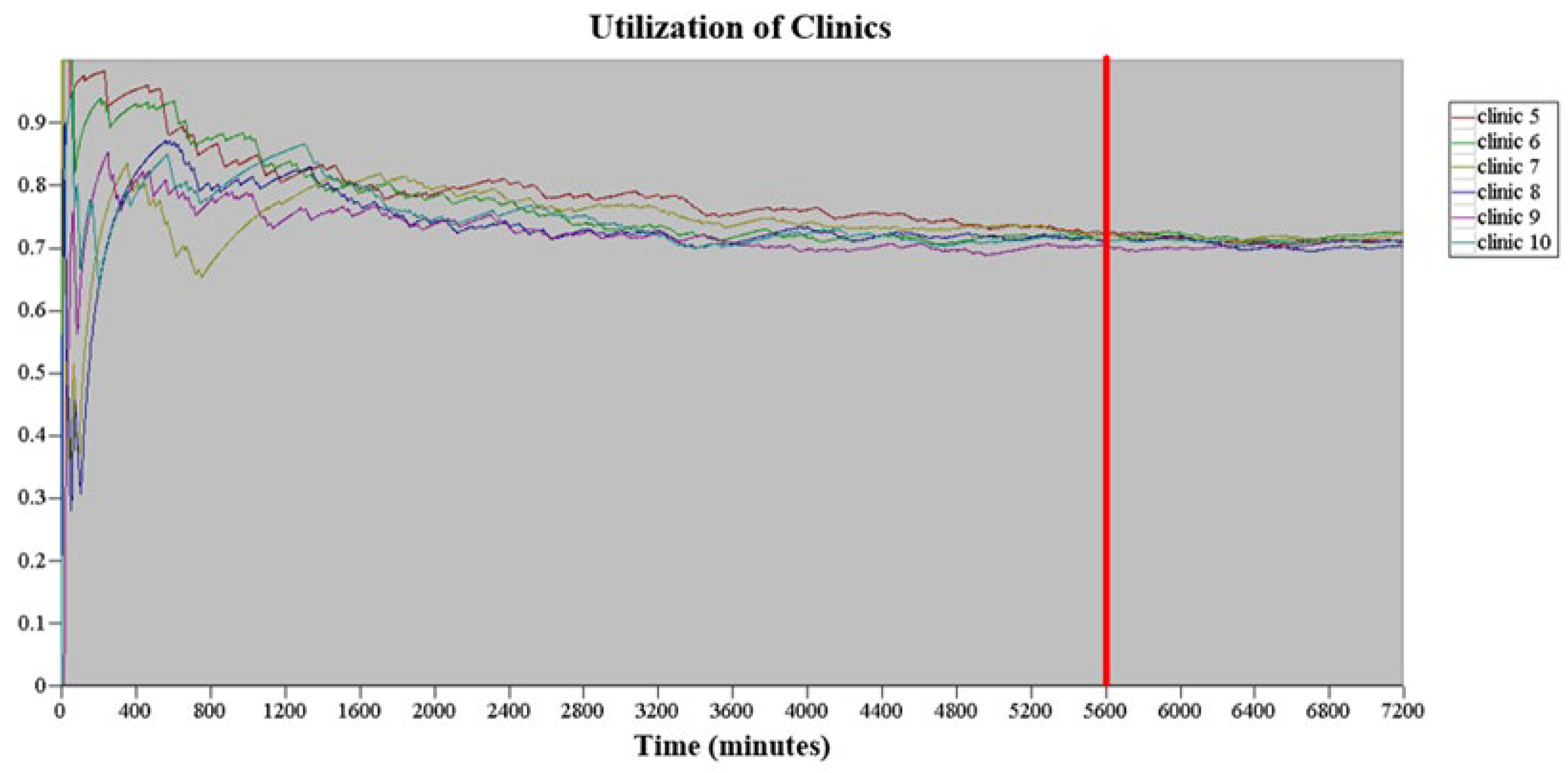
- This study only considered a particular time period of the ultrasound examination schedule, namely Monday to Friday from 8 am to 5 pm, with a break from 12 noon to 1 pm, totaling 8 h a day. The ultrasound examination time for outpatients, inpatients, and emergency patients regardless of the body parts accounted for 6.8% of the total examination time. Therefore, the actual daily simulation time was 93.2% of the total examination time, that is, 447.36 min (480 × 93.2%). The replication length of each simulation was 5 d (i.e., 2236.8 min). The simulation model in this study operated for 7200 min before analyzing the equipment utilization rate under steady-state conditions, as shown in Figure 3. When the simulation time reached 5600 min, no significant fluctuation was found in the equipment utilization rate. Therefore, the warm-up period of the simulation model in this study was set at 5600 min, and the replication length was 7836.8 min (5600 + 2236.8).
- (5)
- The simulated examination rooms were Examination Rooms 5 to 10, totaling six examination rooms. No difference was assumed to exist among the examination rooms, and the instruments and equipment available in all the examination rooms were identical. Furthermore, all types of ultrasound examinations could be performed in each examination room. The same probability distribution was used for the examination time for patients undergoing ultrasound examination of the same body parts in different examination rooms.
- (6)
- The examination times allocated by the ultrasound examination scheduler to patients undergoing liver and DVT ultrasound examinations were different from those allocated to patients undergoing ultrasound examination of other body parts. Based on the historical data regarding patients’ examinations, the examination time for 70% of patients undergoing DVT ultrasound examination was 20 min, whereas the examination time for 30% of patients undergoing DVT ultrasound examinations was 40 min. The examination time for patients undergoing liver ultrasound examination was 40 min, and the examination time for patients undergoing other ultrasound examination was 20 min.
- (7)
- To develop an appointment scheduling strategy that balanced the workload of radiological technologists, the ultrasound examination room team leader assigned various points for different workloads, where 1 point represented 20 min and 2 points represented 40 min. For example, the workload for handling 30% of patients undergoing DVT ultrasound examination was equivalent to 2 points.
- (8)
- The simulation model in this study assumed that the male-to-female radiological technologist ratio in the six examination rooms was 1:1.
- (9)
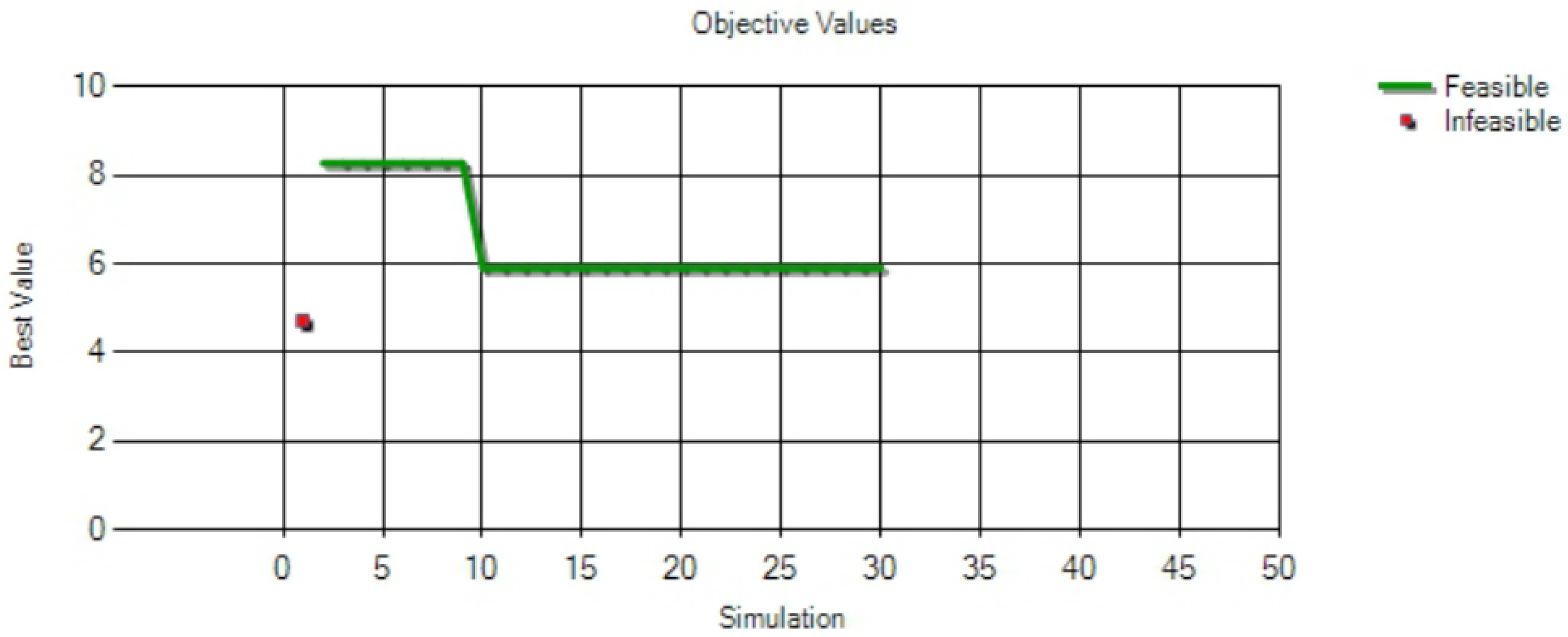
- This study initially set the number of replications to 30, and used the number of patients undergoing ultrasound examination who entered the system as an indicator of the number of replications. When the initial number of replications, n0, was set to be 30, the average () and standard deviation (SD) (s) of the number of patients entering the system at the 95% (i.e., α = 95%) confidence interval was obtained based on Equation (1) of the 30 replications, whereas the initial half-width (h0) was calculated based on Equation (2).
4.5. Waiting Time Analysis for Patients Undergoing the Ultrasound Examination
4.6. Verification and Validation of the Simulation Model
- (1)
- Verification
- (2)
- Validation
4.7. Scenario Analyses
4.8. Discussions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Chen, P.S.; Robielos, R.A.C.; Palana, P.K.V.C.; Valencia, P.L.L.; Chen, G.Y.H. Scheduling patients’ appointments: Allocation of healthcare service using simulation optimization. J. Healthc. Eng. 2015, 6, 259–280. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.-S.; Yang, K.-h.; Robielos, R.A.C.; Cancino, R.A.C.; Dizon, L.A.M. Patient referral mechanisms by using simulation optimization. Simul. Model. Pract. Theory 2016, 61, 14–27. [Google Scholar] [CrossRef]
- Issabakhsh, M.; Lee, S.; Kang, H.J. Scheduling patient appointment in an infusion center: A mixed integer robust optimization approach. Health Care Manag. Sci. 2021, 24, 117–139. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Lin, Q.; Zhao, P.Y.; Zhang, Q.Y.; Xu, K.; Chen, H.Y.; Hu, C.J.; Stuntz, M.; Li, H.; Liu, Y.L. Reducing waiting time and raising outpatient satisfaction in a Chinese public tertiary general hospital-an interrupted time series study. BMC Public Health 2017, 17, 668. [Google Scholar] [CrossRef]
- Sun, Y.F.; Raghavan, U.N.; Vaze, V.; Hall, C.S.; Doyle, P.; Richard, S.S.; Wald, C. Stochastic programming for outpatient scheduling with flexible inpatient exam accommodation. Health Care Manag. Sci. 2021, 24, 460–481. [Google Scholar] [CrossRef]
- Qiu, H.X.; Wang, D.J.; Wang, Y.Z.; Yin, Y.Q. MRI appointment scheduling with uncertain examination time. J. Comb. Optim. 2019, 37, 62–82. [Google Scholar] [CrossRef]
- Bentayeb, D.; Lahrichi, N.; Rousseau, L.M. Patient scheduling based on a service-time prediction model: A data-driven study for a radiotherapy center. Health Care Manag. Sci. 2019, 22, 768–782. [Google Scholar] [CrossRef]
- Cappanera, P.; Visintin, F.; Banditori, C.; Di Feo, D. Evaluating the long-term effects of appointment scheduling policies in a magnetic resonance imaging setting. Flex. Serv. Manuf. J. 2019, 31, 212–254. [Google Scholar] [CrossRef]
- Cayirli, T.; Veral, E. Outpatient scheduling in health care: A review of literature. Prod. Oper. Manag. 2003, 12, 519–549. [Google Scholar] [CrossRef]
- Improta, G.; Russo, M.A.; Triassi, M.; Converso, G.; Murino, T.; Santillo, L.C. Use of the AHP methodology in system dynamics: Modelling and simulation for health technology assessments to determine the correct prosthesis choice for hernia diseases. Math. Biosci. 2018, 299, 19–27. [Google Scholar] [CrossRef]
- Converso, G.; Improta, G.; Mignano, M.; Santillo, L.C. A simulation approach for agile production logic implementation in a hospital emergency unit. In Intelligent Software Methodologies, Tools and Techniques; Springer: Berlin/Heidelberg, Germany, 2015; pp. 623–634. [Google Scholar]
- Ponsiglione, A.M.; Romano, M.; Amato, F. A finite-state machine approach to study patients dropout from medical examinations. In Proceedings of the 2021 IEEE 6th International Forum on Research and Technology for Society and Industry (RTSI), Virtual, Naples, Italy, 6–9 September 2021. [Google Scholar]
- Improta, G.; Guizzi, G.; Ricciardi, C.; Giordano, V.; Ponsiglione, A.M.; Converso, G.; Triassi, M. Agile six sigma in healthcare: Case study at Santobono Pediatric Hospital. Int. J. Environ. Res. Public Health 2020, 17, 1052. [Google Scholar] [CrossRef]
- Pan, X.W.; Geng, N.; Xie, X.L. A stochastic approximation approach for managing appointments in the presence of unpunctual patients, multiple servers and no-shows. Int. J. Prod. Res. 2021, 59, 2996–3016. [Google Scholar] [CrossRef]
- Millhiser, W.P.; Veral, E.A. A decision support system for real-time scheduling of multiple patient classes in outpatient services. Health Care Manag. Sci. 2019, 22, 180–195. [Google Scholar] [CrossRef]
- Shnits, B.; Bendavid, I.; Marmor, Y.N. An appointment scheduling policy for healthcare systems with parallel servers and pre-determined quality of service. Omega-Int. J. Manag. Sci. 2020, 97, 102095. [Google Scholar] [CrossRef]
- Ahmed, M.A.; Alkhamis, T.M. Simulation optimization for an emergency department healthcare unit in Kuwait. Eur. J. Oper. Res. 2009, 198, 936–942. [Google Scholar] [CrossRef]
- Rau, C.L.; Tsai, P.F.; Liang, S.F.; Tan, J.C.; Syu, H.C.; Jheng, Y.L.; Ciou, T.S.; Jaw, F.S. Using discrete-event simulation in strategic capacity planning for an outpatient physical therapy service. Health Care Manag. Sci. 2013, 16, 352–365. [Google Scholar] [CrossRef]
- Hur, Y.; Bard, J.F.; Morrice, D.J. Appointment scheduling at a multidisciplinary outpatient clinic using stochastic programming. Nav. Res. Log. 2021, 68, 134–155. [Google Scholar] [CrossRef]
- Huang, W.T.; Chen, P.S.; Liu, J.J.; Chen, Y.R.; Chen, Y.H. Dynamic configuration scheduling problem for stochastic medical resources. J. Biomed. Inform. 2018, 80, 96–105. [Google Scholar] [CrossRef]
- Deceuninck, M.; De Vuyst, S.; Fiems, D. An efficient control variate method for appointment scheduling with patient unpunctuality. Simul. Model. Pract. Theory 2019, 90, 116–129. [Google Scholar] [CrossRef]
- Harris, S.L.; Samorani, M. On selecting a probabilistic classifier for appointment no-show prediction. Decis. Support Syst. 2021, 142, 113472. [Google Scholar] [CrossRef]
- Lee, S.J.; Heim, G.R.; Sriskandarajah, C.; Zhu, Y.X. Outpatient appointment block scheduling under patient heterogeneity and patient no-shows. Prod. Oper. Manag. 2018, 27, 28–48. [Google Scholar] [CrossRef]
- Kong, Q.X.; Li, S.; Liu, N.; Teo, C.P.; Yan, Z.Z. Appointment scheduling under time-dependent patient no-show behavior. Manag. Sci. 2020, 66, 3480–3500. [Google Scholar] [CrossRef]
- Braaksma, A.; Kortbeek, N.; Smid, K.; Sprengers, M.E.S. A reusable simulation model to evaluate the effects of walk-in for diagnostic examinations. Simul. Model. Pract. Theory 2017, 77, 317–337. [Google Scholar] [CrossRef]
- Klassen, K.J.; Yoogalingam, R. Improving performance in outpatient appointment services with a simulation optimization approach. Prod. Oper. Manag. 2009, 18, 447–458. [Google Scholar] [CrossRef]
- Chen, P.-S.; Lin, M.-H. Development of simulation optimization methods for solving patient referral problems in the hospital-collaboration environment. J. Biomed. Inform. 2017, 73, 148–158. [Google Scholar] [CrossRef]
- Wang, D.Y.; Morrice, D.J.; Muthuraman, K.; Bard, J.F.; Leykum, L.K.; Noorily, S.H. Coordinated scheduling for a multi-server network in outpatient pre-operative care. Prod. Oper. Manag. 2018, 27, 458–479. [Google Scholar] [CrossRef]
- Lee, S.; Lee, Y.H. Improving emergency department efficiency by patient scheduling using deep reinforcement learning. Healthcare 2020, 8, 77. [Google Scholar] [CrossRef]
- Moreno, M.S.; Blanco, A.M. A fuzzy programming approach for the multi-objective patient appointment scheduling problem under uncertainty in a large hospital. Comput. Ind. Eng. 2018, 123, 33–41. [Google Scholar] [CrossRef]
- Baesler, F.; Gatica, J.; Correa, R. Simulation optimisation for operating room scheduling. Int. J. Simul. Model. 2015, 14, 215–226. [Google Scholar] [CrossRef]
- Dios, M.; Molina-Pariente, J.M.; Fernandez-Viagas, V.; Andrade-Pineda, J.L.; Framinan, J.M. A decision support system for operating room scheduling. Comput. Ind. Eng. 2015, 88, 430–443. [Google Scholar] [CrossRef]
- Latorre-Núñez, G.; Lüer-Villagra, A.; Marianov, V.; Obreque, C.; Ramis, F.; Neriz, L. Scheduling operating rooms with consideration of all resources, post anesthesia beds and emergency surgeries. Comput. Ind. Eng. 2016, 97, 248–257. [Google Scholar] [CrossRef]
- Ozen, A.; Marmor, Y.; Rohleder, T.; Balasubramanian, H.; Huddleston, J.; Huddleston, P. Optimization and simulation of orthopedic spine surgery cases at Mayo clinic. Manuf. Serv. Oper. Manag. 2016, 18, 157–175. [Google Scholar] [CrossRef]
- Xiao, G.; Van Jaarsveld, W.; Dong, M.; Van De Klundert, J. Stochastic programming analysis and solutions to schedule overcrowded operating rooms in China. Comput. Oper. Res. 2016, 74, 78–91. [Google Scholar] [CrossRef]
- Liu, J.F.; Zhang, X.; Kong, J.; Wu, L.Y. The Impact of Teammates’ Online Reputations on Physicians’ Online Appointment Numbers: A Social Interdependency Perspective. Healthcare 2020, 8, 509. [Google Scholar] [CrossRef]
- Das, M.C.; Zakaria, M.; Cheng, F.; Xu, J.F. Appointment length with patients in medical consultations in Bangladesh: A hospital-based cross-sectional study. Healthcare 2021, 9, 1164. [Google Scholar] [CrossRef]
- Baril, C.; Gascon, V.; Cartier, S. Design and analysis of an outpatient orthopaedic clinic performance with discrete event simulation and design of experiments. Comput. Ind. Eng. 2014, 78, 285–298. [Google Scholar] [CrossRef]
- Bhattacharjee, P.; Ray, P.K. Patient flow modelling and performance analysis of healthcare delivery processes in hospitals: A review and reflections. Comput. Ind. Eng. 2014, 78, 299–312. [Google Scholar] [CrossRef]
- Wu, X.-D.; Khasawneh, M.T.; Yue, D.-M.; Chu, Y.-N.; Gao, Z.-T. A simulation study of outpatient scheduling with multiple providers and a single device. Int. J. Comput. Intell. Syst. 2014, 7, 15–25. [Google Scholar] [CrossRef]
- Huang, Y.L.; Marcak, J. Grid patient appointment template design to improve scheduling effectiveness. J. Healthc. Eng. 2015, 6, 239–258. [Google Scholar] [CrossRef]
- Huang, Y.L. The development of patient scheduling groups for an effective appointment system. Appl. Clin. Inform. 2016, 7, 43–58. [Google Scholar] [CrossRef][Green Version]
- Liu, N. Optimal choice for appointment scheduling window under patient no-show behavior. Prod. Oper. Manag. 2016, 25, 128–142. [Google Scholar] [CrossRef]
- Ma, X.; Saure, A.; Puterman, M.; Taylor, M.; Tyldesley, S. Capacity planning and appointment scheduling for new patient oncology consults. Health Care Manag. Sci. 2016, 19, 347–361. [Google Scholar] [CrossRef]
- Gavriloff, C.; Ostrowski-Delahanty, S.; Oldfield, K. The impact of lean six sigma methodology on patient scheduling. Nurs. Econ. 2017, 35, 189–193. [Google Scholar]
- Zeltyn, S.; Marmor, Y.N.; Mandelbaum, A.; Carmeli, B.; Greenshpan, O.; Mesika, Y.; Wasserkrug, S.; Vortman, P.; Shtub, A.; Tirza, L.; et al. Simulation-based models of emergency departments: Operational, tactical, and strategic staffing. ACM Trans. Modeling Comput. Simul. 2011, 21, 24. [Google Scholar] [CrossRef]
- Masselink, I.H.J.; van der Mijden, T.L.C.; Litvak, N.; Vanberkel, P.T. Preparation of chemotherapy drugs: Planning policy for reduced waiting times. Omega-Int. J. Manag. Sci. 2012, 40, 181–187. [Google Scholar] [CrossRef]
- Ferrand, Y.B.; Magazine, M.J.; Rao, U.S. Partially flexible operating rooms for elective and emergency surgeries. Decis. Sci. 2014, 45, 819–847. [Google Scholar] [CrossRef]
- Devapriya, P.; Stromblad, C.T.B.; Bailey, M.D.; Frazier, S.; Bulger, J.; Kemberling, S.T.; Wood, K.E. StratBAM: A discrete-event simulation model to support strategic hospital bed capacity decisions. J. Med. Syst. 2015, 39, 1–13. [Google Scholar] [CrossRef]
- Mallor, F.; Azcarate, C.; Barado, J. Optimal control of ICU patient discharge: From theory to implementation. Health Care Manag. Sci. 2015, 18, 234–250. [Google Scholar] [CrossRef]
- Rico, F.; Salari, E.; Centeno, G. Emergency departments nurse allocation to face a pandemic influenza outbreak. In Proceedings of the 2007 Winter Simulation Conference, Washington, DC, USA, 9–12 December 2007; pp. 1292–1298. [Google Scholar]
- Ramis, F.; Baesler, F.; Berho, E.; Neriz, L.; Sepúlveda, J. A simulator to improve waiting times at a medical imaging center. In Proceedings of the 2008 Winter Simulation Conference, Miami, FL, USA, 7–10 December 2008. [Google Scholar]
- Asgary, A.; Najafabadi, M.M.; Karsseboom, R.; Wu, J.H. A drive-through simulation tool for mass vaccination during COVID-19 pandemic. Healthcare 2020, 8, 469. [Google Scholar] [CrossRef]
- Wu, I.C.; Lin, Y.C.; Yien, H.W.; Shih, F.Y. Constructing constraint-based simulation system for creating emergency evacuation plans: A case of an outpatient chemotherapy area at a cancer medical center. Healthcare 2020, 8, 137. [Google Scholar] [CrossRef]
- Zou, B.; Lu, C.; Li, Y. Simulation of a hospital evacuation including wheelchairs based on modified cellular automata. Simul. Model. Pract. Theory 2020, 99, 102018. [Google Scholar] [CrossRef]
- Tamburis, O.; Esposito, C. Process mining as support to simulation modeling: A hospital-based case study. Simul. Model. Pract. Theory 2020, 104, 102149. [Google Scholar] [CrossRef]
- Tai, G.; Williams, P. Optimization of scheduling patient appointments in clinics using a novel modelling technique of patient arrival. Comput. Meth. Prog. Bio. 2012, 108, 467–476. [Google Scholar] [CrossRef]
- Shanker, A.; Kelton, D. Empirical input distributions: An alternative to standard input distributions in simulation modeling. In Proceedings of the 1991 Winter Simulation Conference, Phoenix, AZ, USA, 8–11 December 1991; pp. 978–985. [Google Scholar]


| References | Problem | Mathematical Model or Simulation Model | Methodology |
|---|---|---|---|
| Chen et al. [1] | Outpatient appointment scheduling | Mathematical model and discrete-event simulation model | System simulation with simulation optimization |
| Sun et al. [5] | Outpatient appointment scheduling | Mathematical model | Stochastic programming and heuristic algorithms |
| Qiu et al. [6] | Outpatient appointment scheduling | Mathematical model | Meta-heuristic algorithms |
| Cappanera et al. [8] | Outpatient appointment scheduling | Mathematical model | Heuristic algorithms |
| Pan et al. [14] | Outpatient appointment scheduling | Mathematical model | Stochastic programming and heuristic algorithms |
| Millhiser and Veral [15] | Outpatient appointment scheduling | Mathematical model and discrete-event simulation model | System simulation |
| Ahmed and Alkhamis [17] | Operating room scheduling | Mathematical model | System simulation with simulation optimization |
| Rau et al. [18] | Outpatient physical therapy service | Discrete-event simulation model | System simulation |
| Hur et al. [19] | Outpatient appointment scheduling | Mathematical model | Stochastic programming and heuristic algorithms |
| Huang et al. [20] | Operating room scheduling | Monte Carlo simulation | System simulation |
| Lee et al. [23] | Outpatient appointment scheduling | Mathematical model | Heuristic algorithms |
| Klassen and Yoogalingam [26] | Outpatient appointment scheduling | Mathematical model | Simulation optimization |
| Moreno and Blanco [30] | Outpatient appointment scheduling | Mathematical model | Mathematical software |
| Baesler et al. [31] | Operating room scheduling | Discrete-event simulation model | System simulation |
| Xiao et al. [35] | Operating room scheduling | Mathematical model | Stochastic programming and sample average approximation method |
| Baril et al. [38] | Outpatient orthopaedic clinic | Discrete-event simulation model | System simulation |
| Wu et al. [40] | Outpatient appointment scheduling | Discrete-event simulation model | System simulation |
| Liu [43] | Outpatient appointment scheduling | Mathematical model | Queueing theory |
| Ma et al. [44] | Outpatient appointment scheduling | Mathematical model | Heuristic algorithms |
| Ferrand et al. [48] | Operating room scheduling | Discrete-event simulation model | System simulation |
| Patient Category | Number of Patients | Percentage | Cumulative Percentage |
|---|---|---|---|
| Outpatient | 10,133 | 72.46% | 72.46% |
| Inpatient | 2794 | 19.98% | 92.43% |
| Emergency Patients | 1058 | 7.57% | 100.00% |
| Total | 13,985 | 100.00% |
| Performance Indicator | AS-IS Model | OptQuest Best Model |
|---|---|---|
| Patients’ arrival interval at the radiology department (Minute) | Empirical Value | 18 |
| Average total number of examined patients (Person) | 484.00 | 504.04 |
| Patient’s average waiting time (Minute) | 7.23 | 5.91 |
| Radiologist’s workload at the 5th examination room (equipment utilization rate) (%) | 71.39 | 74.62 |
| Radiologist’s workload at the 6th examination room (equipment utilization rate) (%) | 69.97 | 73.17 |
| Radiologist’s workload at the 7th examination room (equipment utilization rate) (%) | 69.44 | 72.37 |
| Radiologist’s workload at the 8th examination room (equipment utilization rate) (%) | 68.02 | 70.28 |
| Radiologist’s workload at the 9th examination room (equipment utilization rate) (%) | 68.93 | 72.15 |
| Radiologist’s workload at the 10th examination room (equipment utilization rate) (%) | 67.49 | 70.88 |
| Performance Indicator | AS-IS Model | TO-BE1 Model | TO-BE2 Model | |||
|---|---|---|---|---|---|---|
| Average | The Half-Width of 95% Confidence Interval | Average | The Half-Width of 95% Confidence Interval | Average | The Half-Width of 95% Confidence Interval | |
| Average total number of examined patients (Person) | 484.00 | 2.98 | 487.24 | 3.12 | 487.81 | 2.98 |
| Patient’s average waiting time (Minute) | 7.23 | 0.35 | 4.25 | 0.24 | 21.93 | 0.94 |
| Radiologist’s workload at the 5th examination room (equipment utilization rate) (%) | 71.39 | 0.01 | 69.68 | 0.01 | 87.74 | 0.01 |
| Radiologist’s workload at the 6th examination room (equipment utilization rate) (%) | 69.97 | 0.01 | 69.55 | 0.01 | 82.74 | 0.01 |
| Radiologist’s workload at the 7th examination room (equipment utilization rate) (%) | 69.44 | 0.01 | 69.52 | 0.01 | 54.73 | 0.02 |
| Radiologist’s workload at the 8th examination room (equipment utilization rate) (%) | 68.02 | 0.01 | 69.56 | 0.01 | 68.87 | 0.02 |
| Radiologist’s workload at the 9th examination room (equipment utilization rate) (%) | 68.93 | 0.01 | 69.59 | 0.01 | 55.06 | 0.01 |
| Radiologist’s workload at the 10th examination room (equipment utilization rate) (%) | 67.49 | 0.01 | 69.60 | 0.01 | 67.92 | 0.01 |
| Radiologist’s average workload (%) | 69.21 | - | 69.58 | - | 69.51 | - |
| SD of radiologist’s workload (%) | 1.40 | - | 0.06 | - | 13.69 | - |
| Performance Indicator | AS-IS Model | TO-BE1 Model | TO-BE3 Model | |||
|---|---|---|---|---|---|---|
| Average | The Half-Width of 95% Confidence Interval | Average | The Half-Width of 95% Confidence Interval | Average | The Half-Width of 95% Confidence Interval | |
| Average total number of examined patients (person) | 484.00 | 2.98 | 487.24 | 3.12 | 480.94 | 2.83 |
| Average patient’s waiting time (minute) | 7.23 | 0.35 | 4.25 | 0.24 | 5.26 | 0.27 |
| Radiologist’s workload at the 5th examination room (equipment utilization rate) (%) | 71.39 | 0.01 | 69.68 | 0.01 | 68.35 | 0.01 |
| Radiologist’s workload at the 6th examination room (equipment utilization rate) (%) | 69.97 | 0.01 | 69.55 | 0.01 | 68.00 | 0.01 |
| Radiologist’s workload at the 7th examination room (equipment utilization rate) (%) | 69.44 | 0.01 | 69.52 | 0.01 | 69.42 | 0.01 |
| Radiologist’s workload at the 8th examination room (equipment utilization rate) (%) | 68.02 | 0.01 | 69.56 | 0.01 | 68.69 | 0.01 |
| Radiologist’s workload at the 9th examination room (equipment utilization rate) (%) | 68.93 | 0.01 | 69.59 | 0.01 | 69.20 | 0.01 |
| Radiologist’s workload at the 10th examination room (equipment utilization rate) (%) | 67.49 | 0.01 | 69.60 | 0.01 | 69.09 | 0.01 |
| Radiologist’s average workload (%) | 69.21 | - | 69.58 | - | 68.79 | - |
| SD of radiologist’s workload (%) | 1.40 | - | 0.06 | - | 0.54 | - |
| Performance Indicator | AS-IS Model | TO-BE4 Model | ||
|---|---|---|---|---|
| Average | The Half-Width of 95% Confidence Interval | Average | The Half-Width of 95% Confidence Interval | |
| Average total number of examined patients (person) | 484.00 | 2.98 | 505.42 | 0.42 |
| Patient’s average waiting time (minute) | 7.23 | 0.35 | 4.11 | 0.22 |
| Radiologist’s workload at the 5th examination room (equipment utilization rate) (%) | 71.39 | 0.01 | 72.11 | 0.01 |
| Radiologist’s workload at the 6th examination room (equipment utilization rate) (%) | 69.97 | 0.01 | 71.75 | 0.01 |
| Radiologist’s workload at the 7th examination room (equipment utilization rate) (%) | 69.44 | 0.01 | 72.78 | 0.01 |
| Radiologist’s workload at the 8th examination room (equipment utilization rate) (%) | 68.02 | 0.01 | 72.54 | 0.01 |
| Radiologist’s workload at the 9th examination room (equipment utilization rate) (%) | 68.93 | 0.01 | 72.67 | 0.01 |
| Radiologist’s workload at the 10th examination room (equipment utilization rate) (%) | 67.49 | 0.01 | 72.24 | 0.01 |
| Radiologist’s average workload (%) | 69.21 | - | 72.35 | - |
| SD of radiologist’s workload (%) | 1.40 | - | 0.39 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, P.-S.; Chen, G.Y.-H.; Liu, L.-W.; Zheng, C.-P.; Huang, W.-T. Using Simulation Optimization to Solve Patient Appointment Scheduling and Examination Room Assignment Problems for Patients Undergoing Ultrasound Examination. Healthcare 2022, 10, 164. https://doi.org/10.3390/healthcare10010164
Chen P-S, Chen GY-H, Liu L-W, Zheng C-P, Huang W-T. Using Simulation Optimization to Solve Patient Appointment Scheduling and Examination Room Assignment Problems for Patients Undergoing Ultrasound Examination. Healthcare. 2022; 10(1):164. https://doi.org/10.3390/healthcare10010164
Chicago/Turabian StyleChen, Ping-Shun, Gary Yu-Hsin Chen, Li-Wen Liu, Ching-Ping Zheng, and Wen-Tso Huang. 2022. "Using Simulation Optimization to Solve Patient Appointment Scheduling and Examination Room Assignment Problems for Patients Undergoing Ultrasound Examination" Healthcare 10, no. 1: 164. https://doi.org/10.3390/healthcare10010164
APA StyleChen, P.-S., Chen, G. Y.-H., Liu, L.-W., Zheng, C.-P., & Huang, W.-T. (2022). Using Simulation Optimization to Solve Patient Appointment Scheduling and Examination Room Assignment Problems for Patients Undergoing Ultrasound Examination. Healthcare, 10(1), 164. https://doi.org/10.3390/healthcare10010164






