“The Light at the End of the Tunnel”: Experiences of LGBTQ+ Adults in Portuguese Healthcare
Abstract
1. Introduction
2. Material and Methods
2.1. Procedure
2.2. Participant’s Information
2.3. Research Design
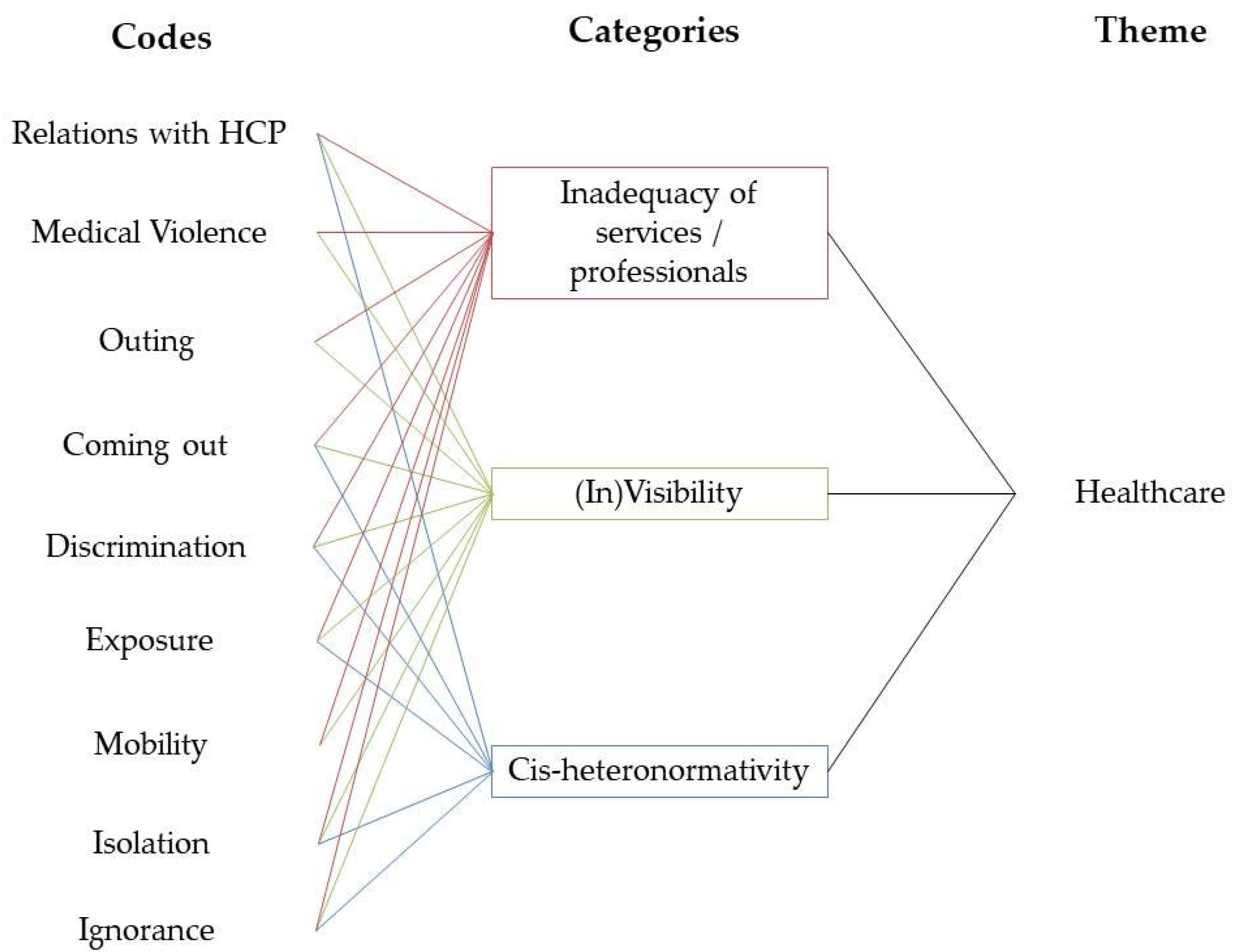
3. Results
3.1. Heteronormativity and Prejudices
“If I go to the gynaecologist [...] or an appointment for STDs, to do the routine test, the questions are not made for me. Also, they ask how many persons I had sex with in the last six months, that’s ridiculous! I can tell how many risky relationships I had but I’m not supposed to tell how many partners I was with!”Jasmim, 30–39
“The doctor suddenly told me “I was looking into it with the person that deals with papers and stuff, she knows about your case, I did my research and when the time comes everything will be easy, you’ll just have to proceed with an adoption”. And you know when you get shocked? You’re not expecting this...I wanted to say something at the moment but I couldn’t say anything, I just kept thinking...an adoption? I went home and said, “When the time comes we’ll see what happens”.Graça, 20–29
“In the islands, we have this issue, I cannot recommend a doctor for a trans person. Last week a colleague called me, she needed a recommendation [for a trans person] [...] I was flustered, scared, because the person was expelled from home, in a state of emotional fragility: we need to be very careful. My colleague said: “We have to be careful, what doctor can he see? If the doctor is not willing to make it work, the guy will be destroyed. [...] It must be a doctor with an open mind, not one of those that would say “Take a pill and go home, you’re just depressed”. But I didn’t know anyone.”Emanuel, 20–29
“The nurse started to ask if I had had a sexual relationship, the usual. And I answered as always. She asked if it was with my girlfriend and I answered: “No, with my boyfriend”. So she stood up and went to ask the doctor whether homosexuals could donate blood and the doctor said they couldn’t. The doctor came to me…[…]I felt furious. […] The most ridiculous thing the doctor said was: “A homosexual man cannot give blood because anal sex causes a higher risk of contagion with HIV”. And this is just completely stupid”.Jorge, 20–29
“I was at the doctor for a routine check. She asked me if I used condoms and I said: “No, I don’t need to, I have a girlfriend”. She knows about my illness, fibromyalgia…and she asked me whether the fact of being lesbian had to do with fibromyalgia! […] She said my illness could have something to do with the fact that I had to hide it to many people…and maybe on an emotional level it had had an impact”.Julia, 30–39
3.2. Shedding Light over LGBTQ+ (in)visibility
“In the beginning doctors didn’t believe in my pain. So… but when I finally found a doctor that took my situation seriously, who is a specialist in people with chronic pain, he asked me if I had an active sexual life. Because it was a good thing, because I need to do back exercise.“Lisa, 20–29y
“It was the people at the health centre that spoke to me, in public, about the case, and there I understood the reason why that boy, that teenager, didn’t want to get [HIV] tested or anything like that.”Zé, 40–49y
“The worst part of my sister not accepting [my sexual orientation] was the fact that my niece, that is a [healthcare provider], also stopped speaking to me. (…)When she [sister] thinks like that I think “well… she is in her 60 s, poor wretch, let her be”. But a [healthcare provider], in her 30 s thinking the same way… to me… well, it hurts a lot”.Marta, 50–59y
“It was alone, because here [where she lives] I am the only one who transitioned from boy to girl. So I was alone on this path. I searched for a psychiatrist Dr. [name of the doctor] and then yes. She was the one that helped me a lot and redirected me to [name of the city]. And it was where they diagnosed me as such. So there it was… there I really found the light at the end of the tunnel”.Margarida, 30–39y
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dolezal, L.; Käll, L.F.; McCormack, D.; Oikkonen, V.; Shildrick, M. Introduction: Queering Health and Biomedicine. Lambda Nord. 2021, 26, 7–18. [Google Scholar] [CrossRef]
- Nowakowski, A.; Sumerau, J.E.; Lampe, N.M. Transformations in Queer, Trans, and Intersex Health and Aging; Lexington Books: London, UK, 2020. [Google Scholar]
- Zeeman, L.; Aranda, K.; Grant, A. (Eds.) Queering Health: Critical Challenges to Normative Health and Healthcare; PCCS Books: Monmouth, UK, 2014. [Google Scholar]
- Rich, A. Compulsory Heterosexuality and Lesbian Existence; Antelope Publications: Denver, CO, USA, 1980. [Google Scholar]
- Butler, J. Bodies That Matter: On the Discursive Limits of ‘Sex’; Routledge: New York, NY, USA, 1993. [Google Scholar]
- Ilga Portugal. Saúde Em Igualdade. 2015. Retrieved 25 April 2020. Available online: https://igualdadenasaude.ilga-portugal.pt/ (accessed on 4 November 2021).
- Johnson, A.H.; Hill, I.; Beach-Ferrara, J.; Rogers, B.A.; Bradford, A. Common Barriers to Healthcare for Transgender People in the U.S. Southeast. Int. J. Transgender Health 2020, 21, 70–78. [Google Scholar] [CrossRef]
- Koh, C.S.; Kang, M.; Usherwood, T. I Demand to Be Treated as the Person I Am: Experiences of Accessing Primary Health Care for Australian Adults Who Identify as Gay, Lesbian, Bisexual, Transgender or Queer. Sex. Health 2014, 11, 258–264. [Google Scholar] [CrossRef]
- Pieri, M. The Sound That You Do Not See. Notes on Queer and Disabled Invisibility. Sex. Cult. 2019, 558. [Google Scholar] [CrossRef]
- Davy, Z.; Siriwardena, A.N. To Be or Not to Be LGBT in Primary Health Care: Health Care for Lesbian, Gay, Bisexual, and Transgender People. Br. J. Gen. Pract. 2012, 62, 491–492. [Google Scholar] [CrossRef][Green Version]
- Alcaire, R. LGBTQI+ Healthcare (in) Equalities in Portugal: What Can We Learn from Asexuality. Healthcare 2021, 9, 583. [Google Scholar] [CrossRef]
- Hilário, A.P. (Re) Making Gender in the Clinical Context: A Look at How Ideologies Shape the Medical Construction of Gender Dysphoria in Portugal. Soc. Theory Health 2019, 17, 463–480. [Google Scholar] [CrossRef]
- Ilga-Europe. Annual Review of the Human Rights Situation of Lesbian, Gay, Bisexual, Trans, and Intersex People in Portugal Covering the Period of January to December 2020. 2021. Available online: https://www.ilga-europe.org/sites/default/files/2020/portugal.pdf (accessed on 5 November 2021).
- DGS-Direção Geral da Saúde. Estratégia Nacional de Saúde Para as Pessoas Lésbicas, Gays, Bissexuais, Trans e Intersexo. 2019. Retrieved 21 March 2020. Available online: https://www.dgs.pt/documentos-e-publicacoes/estrategia-de-saude-para-as-pessoas-lesbicas-gays-bissexuais-trans-e-intersexo-lgbti-pdf.aspx (accessed on 5 November 2021).
- Crowhurst, I. The Fallacy of the Instrumental Gate? Contextualising the Process of Gaining Access through Gatekeepers. Int. J. Soc. Res. Methodol. 2013, 16, 463–475. [Google Scholar] [CrossRef]
- Heckathorn, D.D.; Cameron, C.J. Network Sampling: From Snowball and Multiplicity to Respondent-Driven Sampling. Annu. Rev. Sociol. 2017, 43, 101–119. [Google Scholar] [CrossRef]
- Mason, J. Qualitative Researching, 2nd ed.; SAGE Publications: London, UK, 2002. [Google Scholar]
- Atkinson, R. The Life Story Interview; Sage Publication: London, UK, 1998. [Google Scholar]
- Thille, P.H.; Rotteau, L.; Webster, F. More than Words: Methods to Elicit Talk in Interviews. Fam. Pract. 2021, 38, 545–547. [Google Scholar] [CrossRef]
- Rosati, F.; Pistella, J.; Baiocco, R. Italian Sexual Minority Older Adults in Healthcare Services: Identities, Discriminations, and Competencies. Sex. Res. Soc. Policy 2021, 18, 64–74. [Google Scholar] [CrossRef]
- Stuckey, H.L. Three Types of Interviews: Qualitative Research Methods in Social Health. J. Soc. Health Diabetes 2013, 1, 056–059. [Google Scholar] [CrossRef]
- Lester, J.N.; Cho, Y.; Lochmiller, C.R. Learning to Do Qualitative Data Analysis: A Starting Point. Hum. Resour. Dev. Rev. 2020, 19, 94–106. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Attride-Stirling, J. Thematic Networks: An Analytic Tool for Qualitative Research. Qual. Res. 2001, 1, 385–405. [Google Scholar] [CrossRef]
- de Oliveira, J.M.; Costa, C.G.; Nogueira, C. The Workings of Homonormativity: Lesbian, Gay, Bisexual, and Queer Discourses on Discrimination and Public Displays of Affections in Portugal. J. Homosex. 2013, 60, 1475–1493. [Google Scholar] [CrossRef]
- Meyer, I.H. Prejudice, Social Stress, and Mental Health in Lesbian, Gay, and Bisexual Populations: Conceptual Issues and Research Evidence. Psychol. Bull. 2003, 129, 2003. [Google Scholar] [CrossRef]
- Padfield, D.; Zakrzewska, J.M. (Eds.) Encountering Pain; UCL Press: London, UK, 2021. [Google Scholar]
- Salamon, G. The Phenomenology of Rheumatology: Disability, Merleau-Ponty, and the Fallacy of Maximal Grip. Hypatia 2012, 27, 243–260. [Google Scholar] [CrossRef]
- Eliason, M.J.; Schope, R. Does ‘Don’t Ask Don’t Tell’ Apply to Health Care? Lesbian, Gay, and Bisexual People’s Disclosure to Health Care Providers. J. Gay Lesbian Med. Assoc. 2001, 5, 125–134. [Google Scholar] [CrossRef]
- Cruikshank, M. The Gay and Lesbian Liberation Movement; Routledge: New York, NY, USA, 1992. [Google Scholar]
- Moleiro, C.; Pinto, N.; de Oliveira, J.M.; Santos, M.H. Violência Doméstica: Boas Práticas No Apoio a Vítimas LGBT: Guia de Boas Práticas Para Profissionais de Estruturas de Apoio a Vítimas; Comissão para a Cidadania e Igualdade de Género: Porto, Portugal, 2016. [Google Scholar]
- Santos, A.C. Social Movements and Sexual Citizenship in Southern Europe; Palgrave Macmillan: Basingstoke, UK, 2013. [Google Scholar]
- Henriquez, N.R.; Ahmad, N. ‘The Message Is You Don’t Exist’: Exploring Lived Experiences of Rural Lesbian, Gay, Bisexual, Transgender, Queer/Questioning (LGBTQ) People Utilizing Health Care Services. SAGE Open Nurs. 2021, 7. [Google Scholar] [CrossRef]
- Burgwal, A.; Gvianishvili, N.; Hård, V.; Kata, J.; Nieto, I.; Orre, C.; Smiley, A.; Vidić, J.; Motmans, J. The Impact of Training in Transgender Care on Healthcare Providers Competence and Confidence: A Cross-Sectional Survey. Healthcare 2021, 9, 967. [Google Scholar] [CrossRef] [PubMed]
| Age | Participants (n) |
|---|---|
| <20 | 2 |
| 20–29 | 9 |
| 30–39 | 16 |
| 40–49 | 1 |
| 50–59 | 4 |
| Total | 32 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pieri, M.; Brilhante, J. “The Light at the End of the Tunnel”: Experiences of LGBTQ+ Adults in Portuguese Healthcare. Healthcare 2022, 10, 146. https://doi.org/10.3390/healthcare10010146
Pieri M, Brilhante J. “The Light at the End of the Tunnel”: Experiences of LGBTQ+ Adults in Portuguese Healthcare. Healthcare. 2022; 10(1):146. https://doi.org/10.3390/healthcare10010146
Chicago/Turabian StylePieri, Mara, and Joana Brilhante. 2022. "“The Light at the End of the Tunnel”: Experiences of LGBTQ+ Adults in Portuguese Healthcare" Healthcare 10, no. 1: 146. https://doi.org/10.3390/healthcare10010146
APA StylePieri, M., & Brilhante, J. (2022). “The Light at the End of the Tunnel”: Experiences of LGBTQ+ Adults in Portuguese Healthcare. Healthcare, 10(1), 146. https://doi.org/10.3390/healthcare10010146






