An Efficient System for Eye Movement Desensitization and Reprocessing (EMDR) Therapy: A Pilot Study
Abstract
:1. Introduction
2. Related Work
3. Materials and Methods
3.1. Materials
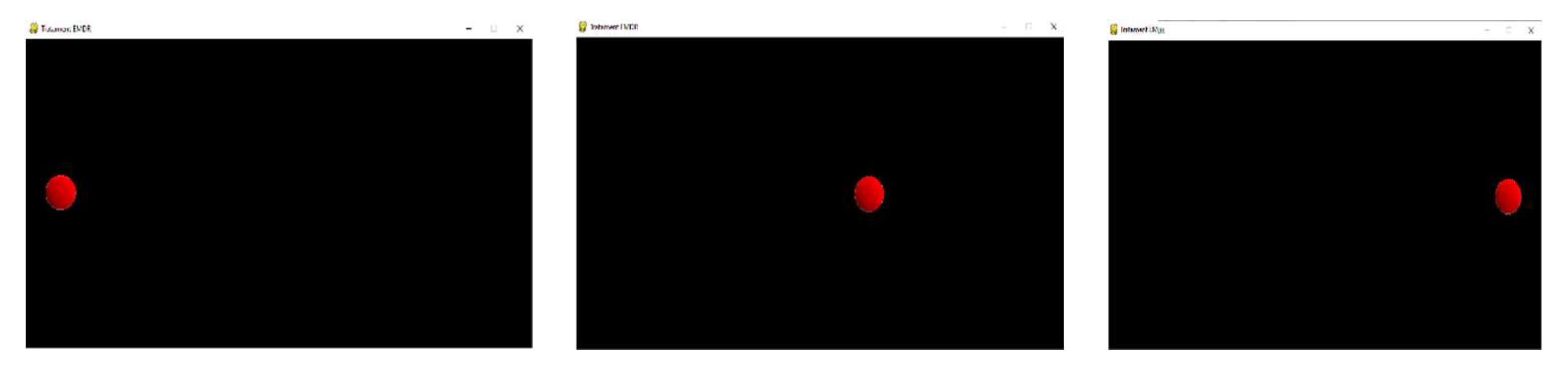
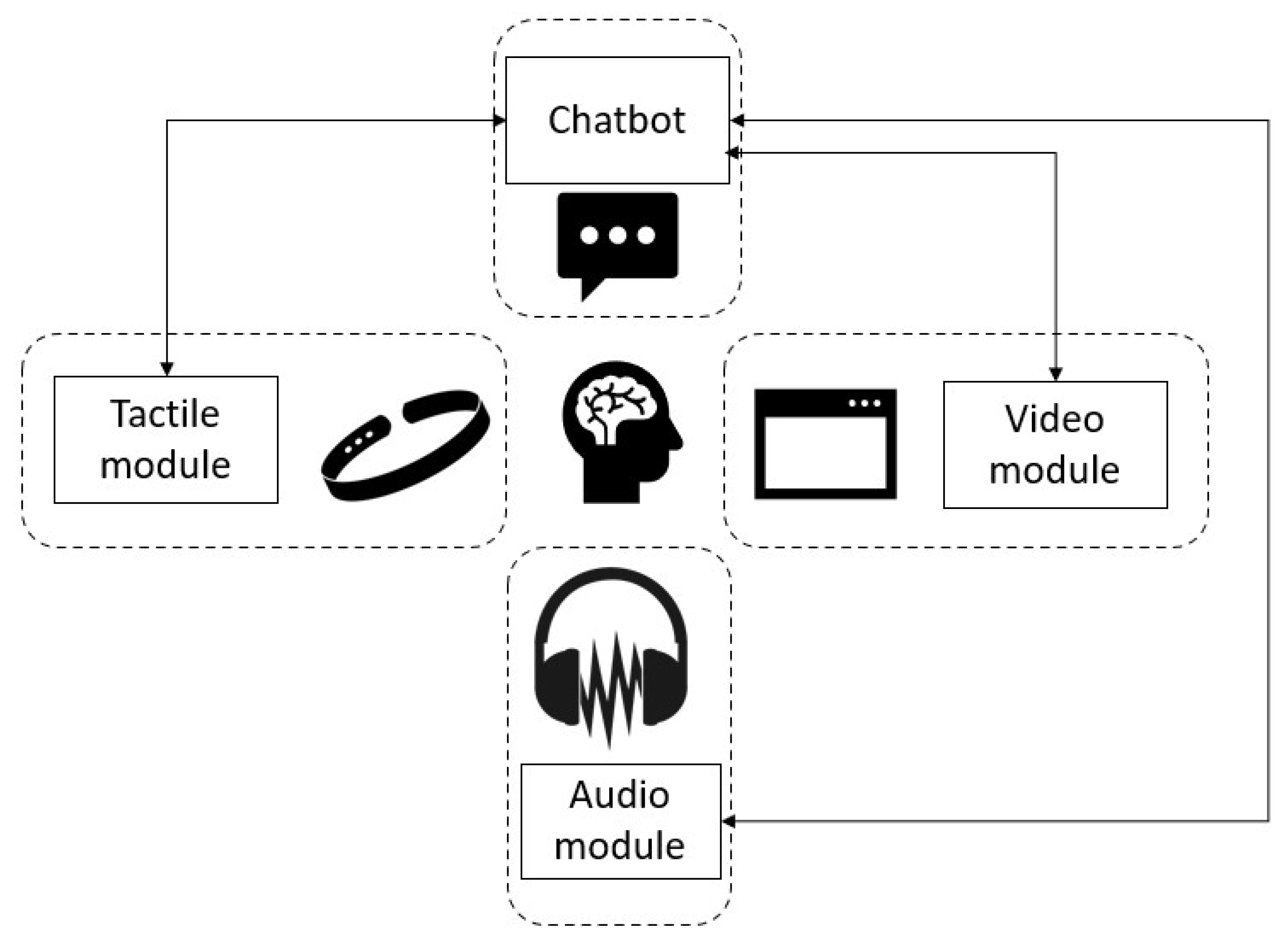
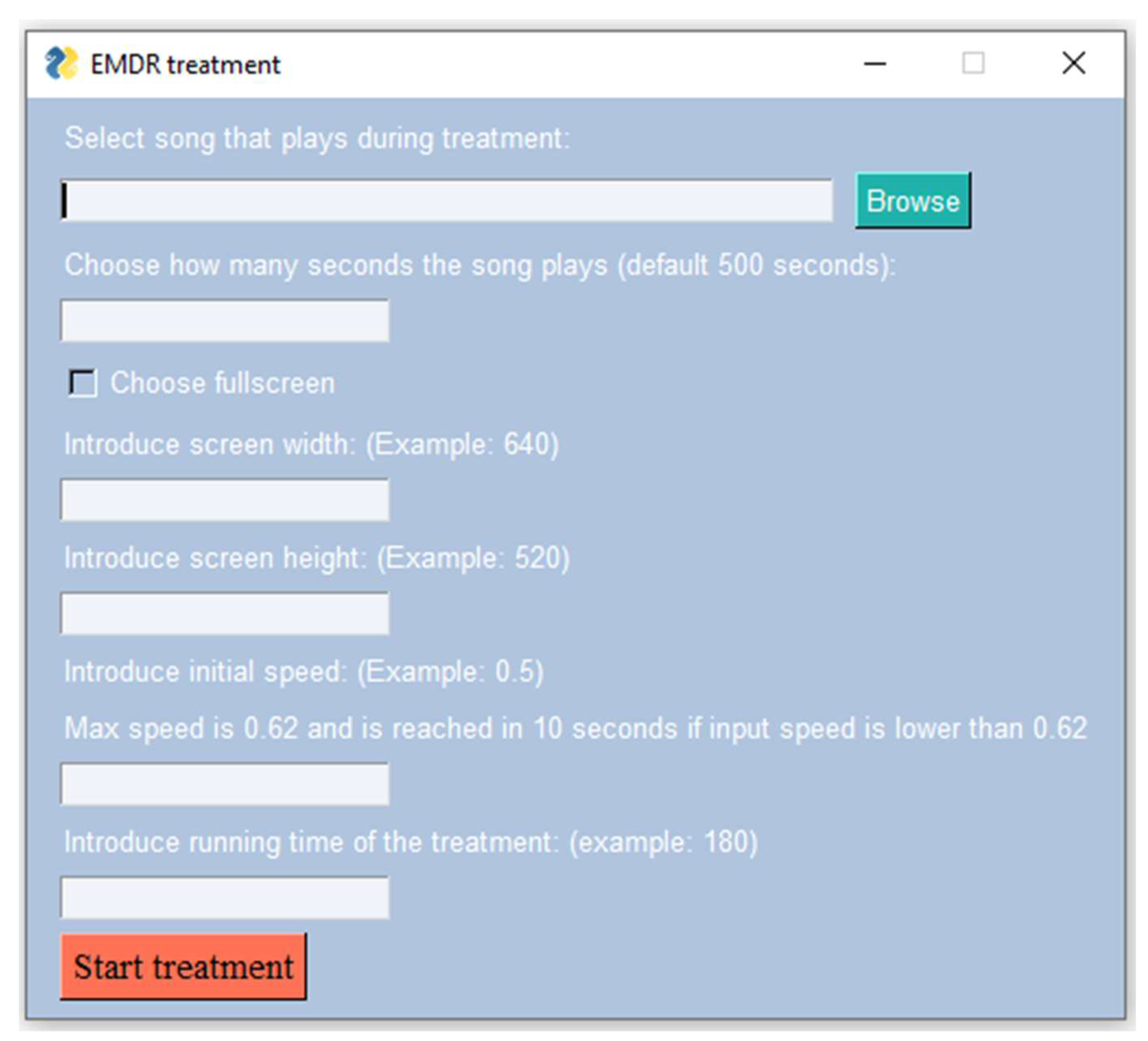
- Video stimulus using a rendered ball on a graphical display;
- Audio stimulus simulating a moving sound source;
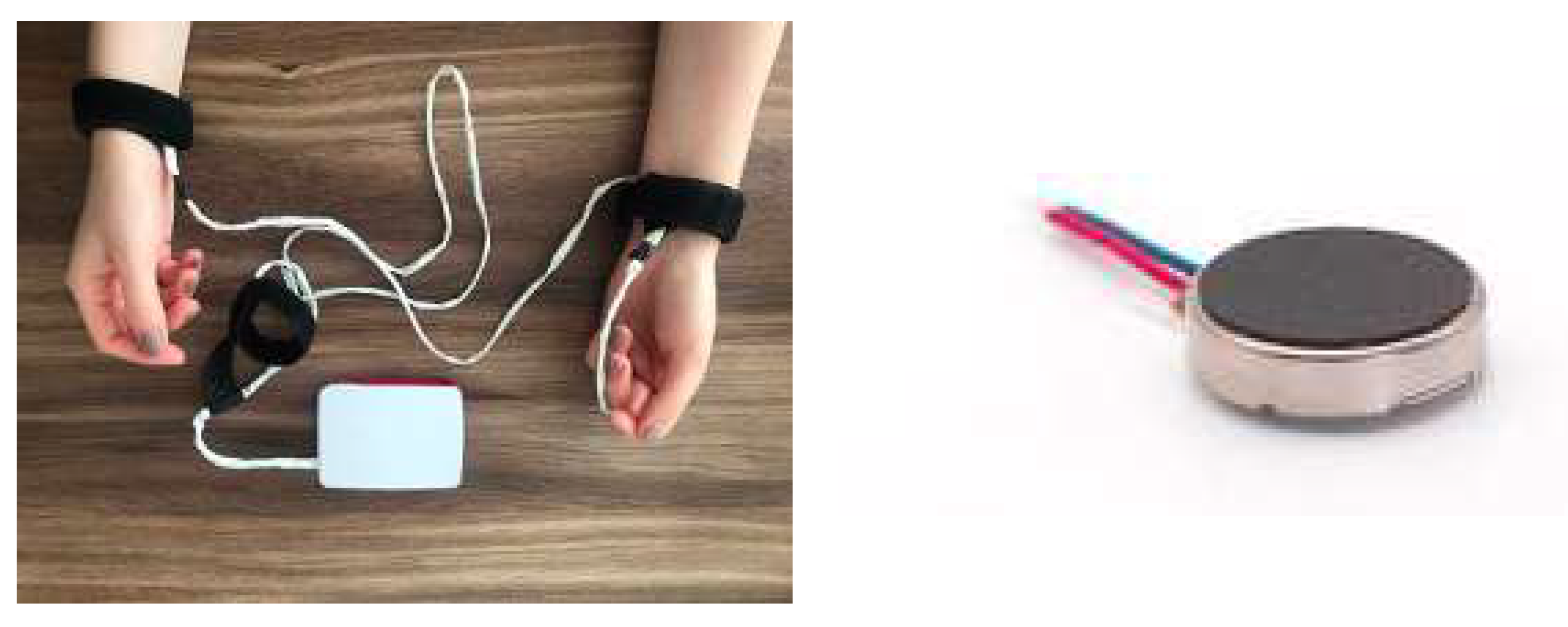
- Tactile stimulation using vibration motors placed on the user using bracelets—stimuli are synchronized to maximize the effectiveness;
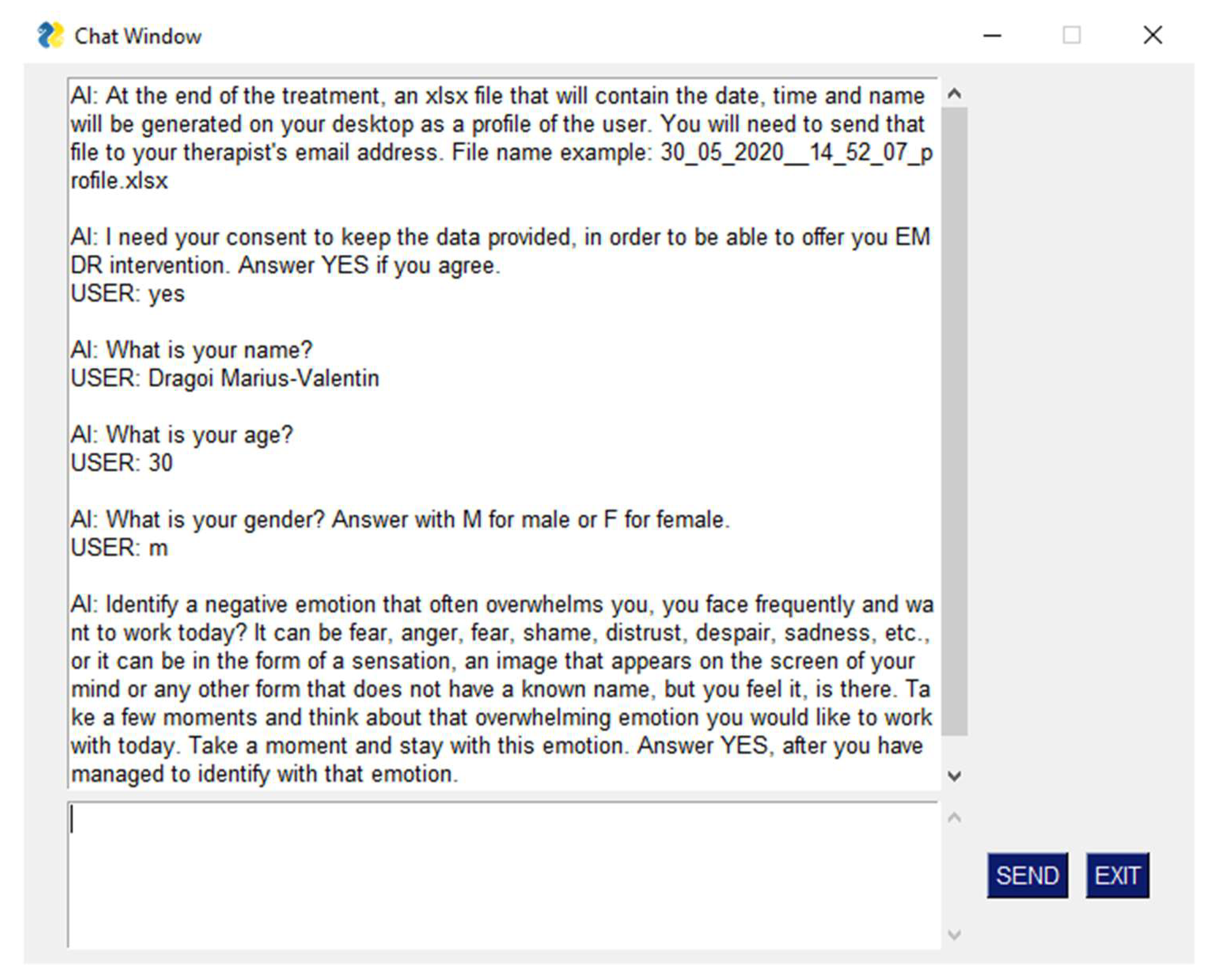
- A chatbot for communicating with the user according to the EMDR protocol, allowing the system to function autonomously, i.e., in the absence of a therapist.
3.2. Recruitment
3.3. Procedure
3.4. Instruments
3.4.1. Primary Outcome Measures
3.4.2. Secondary Outcome Measures
4. Results
4.1. Primary Outcome Measures
4.2. Secondary Outcome Measures
5. Discussion
6. Conclusions
- The presence of an AI-driven chatbot, following the eight essential phases of EMDR [10], which can be further enhanced with new dialogue options and evaluation strategies;
- The ability to customize the interaction based on the patient’s characteristics. For example, using different stimulation methods (visual, audio, tactile) makes the EMDR procedure accessible for people with disabilities (severe visual impairment or even blindness, hearing loss);
- The possibility of applying EMDR treatments in a fully unsupervised manner, using the aforementioned chatbot, i.e., the assistance of a trained clinician is not required;
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Shapiro, F. Eye Movement Desensitization and Reprocessing: Basic Principles, Protocols and Procedures, 2nd ed.; Guilford: New York, NY, USA, 2001; ISBN 978-1572306721. [Google Scholar]
- Sikes, C.; Sikes, V. EMDR: Why the controversy? Traumatology 2003, 9, 169–182. [Google Scholar] [CrossRef]
- Waterman, L.Z.; Cooper, M. Self-administered EMDR therapy: Potential solution for expanding the availability of psychotherapy for PTSD or unregulated recipe for disaster? BJPsych Open 2020, 6, e115. [Google Scholar] [CrossRef] [PubMed]
- Berg, D.P.V.D.; van der Gaag, M. Treating trauma in psychosis with EMDR: A pilot study. J. Behav. Ther. Exp. Psychiatry 2012, 43, 664–671. [Google Scholar] [CrossRef]
- Ironson, G.; Freund, B.; Strauss, J.; Williams, J. Comparison of two treatments for traumatic stress: A community-based study of EMDR and prolonged exposure. J. Clin. Psychol. 2001, 58, 113–128. [Google Scholar] [CrossRef]
- Cuijpers, P.; Van Veen, S.C.; Sijbrandij, M.; Yoder, W.; Cristea, I.A. Eye movement desensitization and reprocessing for mental health problems: A systematic review and meta-analysis. Cogn. Behav. Ther. 2020, 49, 165–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horst, F.; Den Oudsten, B.; Zijlstra, W.; de Jongh, A.; Lobbestael, J.; De Vries, J. Cognitive Behavioral Therapy vs. Eye Movement Desensitization and Reprocessing for Treating Panic Disorder: A Randomized Controlled Trial. Front. Psychol. 2017, 8, 1409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gauhar, Y.W.M. The Efficacy of EMDR in the Treatment of Depression. J. EMDR Pr. Res. 2016, 10, 59–69. [Google Scholar] [CrossRef]
- Logie, R. EMDR-more than just a therapy for PTSD? Psychologist 2014, 27, 512–517. [Google Scholar]
- Shapiro, F. Eye Movement Desensitization and Reprocessing (EMDR) Therapy, Third Edition: Basic Principles, Protocols, and Procedures; The Guilford Press: New York, NY, USA, 2018; ISBN 9781462532766. [Google Scholar]
- De Bont, P.A.J.M.; Berg, D.V.D.; Van Der Vleugel, B.M.; De Roos, C.; De Jongh, A.; van der Gaag, M.; Van Minnen, A.M. Prolonged exposure and EMDR for PTSDv. a PTSD waiting-list condition: Effects on symptoms of psychosis, depression and social functioning in patients with chronic psychotic disorders. Psychol. Med. 2016, 46, 2411–2421. [Google Scholar] [CrossRef]
- Mosquera, D.; Leeds, A.M.; Gonzalez, A. Application of EMDR Therapy for Borderline Personality Disorder. J. EMDR Pr. Res. 2014, 8, 74–89. [Google Scholar] [CrossRef]
- Mosquera, D.; Knipe, J. Understanding and Treating Narcissism with EMDR Therapy. J. EMDR Pr. Res. 2015, 9, 46–63. [Google Scholar] [CrossRef]
- Novo, P.; Landin-Romero, R.; Radua, J.; Vicens, V.; Fernandez, I.; Garcia, F.; Pomarol-Clotet, E.; McKenna, P.J.; Shapiro, F.; Amann, B.L. Eye movement desensitization and reprocessing therapy in subsyndromal bipolar patients with a history of traumatic events: A randomized, controlled pilot-study. Psychiatry Res. 2014, 219, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Flores, D.O.A.; Pineda-Lopez, F.; Aucatoma, E.L.G.; Cordova, F.E.I. Automated system on android platform for use in the implementation psychotherapeutic technical EMDR. In Proceedings of the 2014 XIX Symposium on Image, Signal Processing and Artificial Vision, Armenia, Colombia, 17–19 September 2014; pp. 1–5. [Google Scholar] [CrossRef]
- Ben-Tsvi, Y. IOIO Documentation on GitHub. Available online: https://github.com/ytai/ioio/wiki. (accessed on 15 November 2021).
- Eastman, J.D. Systems and Methods for Self Directed Stress Assistance. U.S. Patent 201201513119A1, 14 June 2012. [Google Scholar]
- Gazit, N.; Gazit, L.; Bar, T. Desensitization and Reprocessing Therapy. U.S. Patent 20200086077A1, 19 March 2020. [Google Scholar]
- Burgio, P.A.; Spurrill, A.T.; Burgio, D.J. Method and Apparatus for Providing Automatic Eye Focused Therapy. U.S. Patent 20090156886A1, 18 June 2009. [Google Scholar]
- Amano, T.; Toichi, M. The Role of Alternating Bilateral Stimulation in Establishing Positive Cognition in EMDR Therapy: A Multi-Channel Near-Infrared Spectroscopy Study. PLoS ONE 2016, 11, e0162735. [Google Scholar] [CrossRef]
- Rousseau, P.-F.; Boukezzi, S.; Garcia, R.; Chaminade, T.; Khalfa, S. Cracking the EMDR code: Recruitment of sensory, memory and emotional networks during bilateral alternating auditory stimulation. Aust. N. Z. J. Psychiatry 2020, 54, 818–831. [Google Scholar] [CrossRef]
- Vibration Motor 1027. Available online: www.vibrationmotors.com/product-catalogue/coin-vibration-motors/coin-vibration-motor-bvm1027-x10-1b02u-b (accessed on 5 October 2021).
- Leon, A.C.; Davis, L.L.; Kraemer, H.C. The role and interpretation of pilot studies in clinical research. J. Psychiatr. Res. 2011, 45, 626–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weiss, D.S.; Marmar, C.R. The Impact of Event Scale-Revised. In Assessing Psychological Trauma and PTSD: A Practitioner’s Handbook; Wilson, J.P., Keane, T.M., Eds.; Guilford Press: New York, NY, USA, 1997; pp. 399–411. [Google Scholar]
- Weiss, D.S. The Impact of Event Scale: Revised. In Cross-Cultural Assessment of Psychological Trauma and PTSD; Wilson, J.P., Tang, C.S., Eds.; Springer International and Cultural Psychology Series; Springer Science & Business Media: Boston, MA, USA, 2007; pp. 219–238. [Google Scholar]
- Beck, J.G.; Grant, D.; Read, J.P.; Clapp, J.; Coffey, S.F.; Miller, L.M.; Palyo, S.A. The Impact of Event Scale-Revised: Psychometric properties in a sample of motor vehicle accident survivors. J. Anxiety Disord. 2008, 22, 187–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Creamer, M.; Bell, R.; Failla, S. Psychometric properties of the Impact of Event Scale—Revised. Behav. Res. Ther. 2003, 41, 1489–1496. [Google Scholar] [CrossRef]
- Doroga, C.; Băban, A. Traumatic exposure and posttraumatic symptoms for train drivers involved in railway incidents. Clujul Med. 2013, 86, 144–149. [Google Scholar]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.; Vagg, P.R.; Jacobs, G.A. Manual for the State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Pitariu, H.; Peleasa, C. Manual for the Romanian Version of State-Trait Anxiety Inventory form Y; Sinapsis: Cluj-Napoca, Romania, 2007. [Google Scholar]
- Balbo, M.; Cavallo, F.; Fernandez, I. Integrating EMDR in psychotherapy. J. Psychother. Integr. 2019, 29, 23–31. [Google Scholar] [CrossRef]
- Shapiro, F. Efficacy of the eye movement desensitization procedure in the treatment of traumatic memories. J. Trauma. Stress 1989, 2, 199–223. [Google Scholar] [CrossRef]
- Puffer, M.K.; Greenwald, R.; Elrod, D.E. A single session EMDR study with twenty traumatized children and adolescents. Traumatology 1998, 3, 6. [Google Scholar] [CrossRef]
- Rogers, S.; Silver, S.M.; Goss, J.; Obenchain, J.; Willis, A.; Whitney, R.L. A Single Session, Group Study of Exposure and Eye Movement Desensitization and Reprocessing in Treating Posttraumatic Stress Disorder Among Vietnam War Veterans: Preliminary Data. J. Anxiety Disord. 1999, 13, 119–130. [Google Scholar] [CrossRef]
- Maxfield, L.; Melnyk, W.T. Single Session Treatment of Test Anxiety with Eye Movement Desensitization and Reprocessing (EMDR). Int. J. Stress Manag. 2000, 7, 87–101. [Google Scholar] [CrossRef]
- Servan-Schreiber, D. Eye movement desensitization and reprocessing: Is psychiatry missing the point? Psychiatr. Times 2000, 17, 36–40. [Google Scholar]
- Kutz, I.; Resnik, V.; Dekel, R. The Effect of Single-Session Modified EMDR on Acute Stress Syndromes. J. EMDR Pr. Res. 2008, 2, 190–200. [Google Scholar] [CrossRef]
- Tarquinio, C.; Brennstuhl, M.-J.; Rydberg, J.A.; Bassan, F.; Peter, L.; Tarquinio, C.L.; Auxéméry, Y.; Rotonda, C.; Tarquinio, P. EMDR in Telemental Health Counseling for Healthcare Workers Caring for COVID-19 Patients: A Pilot Study. Issues Ment. Health Nurs. 2021, 42, 3–14. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- McGrowder, D.A.; Miller, F.G.; Vaz, K.; Cross, M.A.; Anderson-Jackson, L.; Bryan, S.; Latore, L.; Thompson, R.; Lowe, D.; McFarlane, S.R.; et al. The Utilization and Benefits of Telehealth Services by Health Care Professionals Managing Breast Cancer Patients during the COVID-19 Pandemic. Health 2021, 9, 1401. [Google Scholar] [CrossRef]
- Maxfield, L. Low-Intensity Interventions and EMDR Therapy. J. EMDR Pr. Res. 2021, 15, 86–98. [Google Scholar] [CrossRef]
- Marotta-Walters, S.A.; Jain, K.; Dinardo, J.; Kaur, P.; Kaligounder, S. A Review of Mobile Applications for Facilitating EMDR Treatment of Complex Trauma and Its Comorbidities. J. EMDR Pr. Res. 2018, 12, 2–15. [Google Scholar] [CrossRef]


| Paper | Advantages | Disadvantages | Differences between Our System and Related Work |
|---|---|---|---|
| Aleluma Flores et al. [15] | Uses visual, tactile, and auditory therapy. Can be customized. | Implements only the desensitization phase in the EMDR protocol. Used only by psychotherapists/clinicians. The presence of a trained clinician is mandatory, cannot be used independently. | Presence of intelligent chatbot which implements the preparation, evaluation, and ending phases in the EMDR protocol. The system has the potential to be autonomous, the presence of a trained clinician not being mandatory. |
| Jeffrey D. Eastman [17] | Visual stimulation can be dynamically adjusted based on feedback from the user. | Only visual and auditory stimuli. Audio is mostly used for playing relaxation sounds, very little information is given about bilateral audio stimulation. Only patent, not validated. | Presence of intelligent chatbot which implements the preparation, evaluation, and ending phases in the EMDR protocol. Audio, video, and tactile-based actuators that make the EMDR system more efficient. |
| Gazit et al. [18] | Selection of the intensity of stimuli. | No intelligent chatbot. The system is designed to intermediate the relation between client and clinician and can be used remotely but requires the intervention of a therapist for setting the parameters. | The proposed system has the potential to be autonomous. |
| Burgio et al. [19] | Opaque glasses that block light from reaching the eyes and thus prevent simultaneous exposure to other visual stimuli. Uses chemical stimulation. | The system is dependent on the presence of the therapist Different from the standardized EMDR procedure Only patent, not validated. | The proposed system includes an intelligent chatbot offering autonomy. Designed in relation to standardized EMDR procedures. |
| Characteristics | Category | n | % |
|---|---|---|---|
| Age (years) | Mean ± standard deviation | 26.2 ± 4.21 | |
| Gender | Male | 14 | 45.2 |
| Female | 17 | 54.8 | |
| Education | High school diploma | 4 | 12.9 |
| College degree | 10 | 32.3 | |
| Master’s degree | 15 | 28.4 | |
| Doctorate (Ph.D) | 2 | 6.5 | |
| Health condition | No treatment in the last 6 months | 23 | 74.2 |
| Under treatment in the last 6 months | 8 | 25.8 | |
| Months since the traumatic event | Less than 6 months | 1 | 3.2 |
| Between 6 and 12 months | 13 | 41.9 | |
| Between 12 and 24 months | 6 | 19.4 | |
| Between 24 and 36 months | 7 | 22.6 | |
| More than 36 months | 4 | 12.9 | |
| Criteria for inclusion | (18–40 years of age; at least medium scores on IES-R and STAI) | 31 | 88.5 |
| Criteria for exclusion | (Scored very high on both measures; suicidal; taking psychotropic medication; diagnosed psychological condition) | 4 | 11.6 |
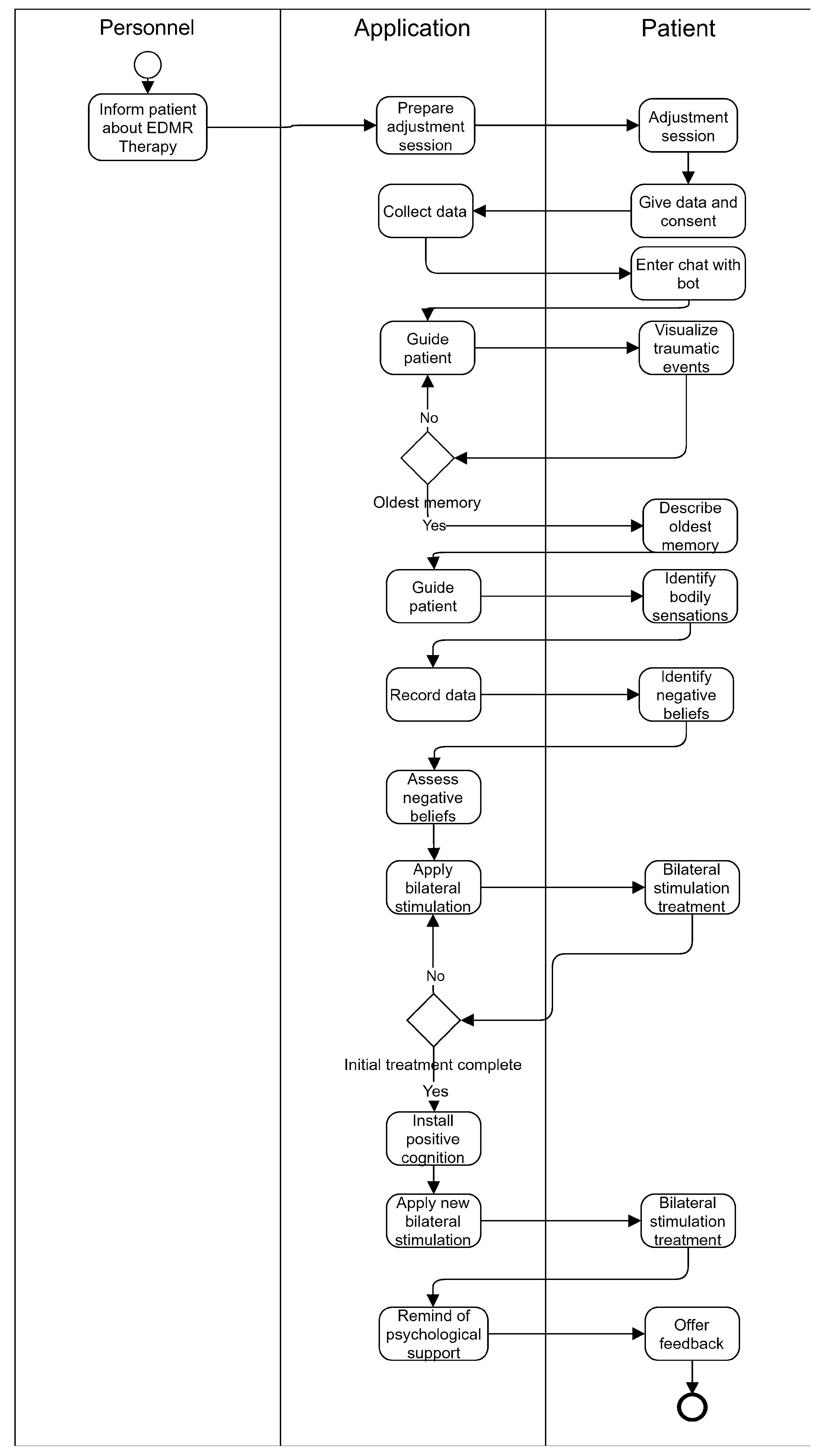
| The Phase of the Intervention | Description |
|---|---|
| 1. Introduction | Participants were informed about EMDR therapy and how bilateral sensory stimulation helps process traumatic memories. It was mentioned that they could withdraw at any time if they were not comfortable with the procedure. At the same time, the participants went through an adjustment session with bilateral stimulations. |
| 2. Demographic info | The application requested demographic information (gender and age) and the agreement for participation. |
| 3. Preparation for accessing the traumatic event | Through intelligent chatbot guiding, the participant was led to access overwhelming emotions that sometimes interfere with their usual activity and primary events recorded in memory associated with overwhelming emotions. The participant was also guided to visualize that event mentally as a movie scene. Once the oldest memory associated with those emotions was identified, the participant was asked to describe it briefly. |
| 4. Body scanning | The participant was intelligently guided to identify the bodily sensations associated with that event (tension, tremor, cold, heat, pressure, or sounds). The information obtained was noted and recorded by the application. |
| 5. Identification of negative beliefs | Identification of negative beliefs (about oneself, others, the world, or life in general) caused by the traumatic event. |
| 6. Emotions and cognitions intensity assessment | Assessment of the intensity of negative cognitions/beliefs and emotions associated with that event (VOC and SUD scale) |
| 7. Treatment phase | Application of bilateral stimulation (audio, video, and sensory) in several sessions of four minutes each and assessment of the intensity of cognitions and emotions after each session of bilateral stimulation done through the guidance of the chatbot. |
| 8. Positive cognition identification and installing | Identifying and installing positive cognition through a new session of bilateral stimulation. |
| 9. Closure | The intelligent chatbot reminds the participant that they can benefit from psychological support. |
| 10. Feedback | The participant can share their impressions related to the experience of using the application. |
| 95% CI For Cohen’s D | ||||||
|---|---|---|---|---|---|---|
| t | df | p | Cohen’s d | Lower | Upper | |
| IES-R Pre-, IES-R Post- | 10.521 | 30 | <0.001 | 1.890 | 1.292 | 2.476 |
| STAI Pre-, STAI Post- | 11.759 | 30 | <0.001 | 2.112 | 1.469 | 2.744 |
| N | Mean | SD | SE | |
|---|---|---|---|---|
| IES-R Pre- | 31 | 39.806 | 14.077 | 2.528 |
| IES-R Post- | 31 | 13.742 | 5.785 | 1.039 |
| STAI Pre- | 31 | 56.774 | 8.330 | 1.496 |
| STAI Post- | 31 | 33.839 | 4.620 | 0.830 |
| t | df | p | |
|---|---|---|---|
| VOC Pre-, VOC Post - | 14.471 | 30 | <0.001 |
| SUD Pre-, SUD Post - | 75.904 | 30 | <0.001 |
| N | Mean | SD | SE | |
|---|---|---|---|---|
| VOC Pre- | 31 | 2.968 | 0.657 | 0.118 |
| VOC Post- | 31 | 6.097 | 0.887 | 0.156 |
| SUD Pre- | 31 | 9.161 | 0.735 | 0.132 |
| SUD Post- | 31 | 0.774 | 0.717 | 0.129 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goga, N.; Boiangiu, C.-A.; Vasilateanu, A.; Popovici, A.-F.; Drăgoi, M.-V.; Popovici, R.; Gancea, I.O.; Pîrlog, M.C.; Popa, R.C.; Hadăr, A. An Efficient System for Eye Movement Desensitization and Reprocessing (EMDR) Therapy: A Pilot Study. Healthcare 2022, 10, 133. https://doi.org/10.3390/healthcare10010133
Goga N, Boiangiu C-A, Vasilateanu A, Popovici A-F, Drăgoi M-V, Popovici R, Gancea IO, Pîrlog MC, Popa RC, Hadăr A. An Efficient System for Eye Movement Desensitization and Reprocessing (EMDR) Therapy: A Pilot Study. Healthcare. 2022; 10(1):133. https://doi.org/10.3390/healthcare10010133
Chicago/Turabian StyleGoga, Nicolae, Costin-Anton Boiangiu, Andrei Vasilateanu, Alexandru-Filip Popovici, Marius-Valentin Drăgoi, Ramona Popovici, Ionatan Octavian Gancea, Mihail Cristian Pîrlog, Ramona Cristina Popa, and Anton Hadăr. 2022. "An Efficient System for Eye Movement Desensitization and Reprocessing (EMDR) Therapy: A Pilot Study" Healthcare 10, no. 1: 133. https://doi.org/10.3390/healthcare10010133
APA StyleGoga, N., Boiangiu, C.-A., Vasilateanu, A., Popovici, A.-F., Drăgoi, M.-V., Popovici, R., Gancea, I. O., Pîrlog, M. C., Popa, R. C., & Hadăr, A. (2022). An Efficient System for Eye Movement Desensitization and Reprocessing (EMDR) Therapy: A Pilot Study. Healthcare, 10(1), 133. https://doi.org/10.3390/healthcare10010133








