Treatments, Perceived Stigma, and Employment Outcomes among Substance Abusers in China
Abstract
1. Introduction
1.1. Stigma of Substance Abuse
1.2. Substance Abuse and Stigma in China
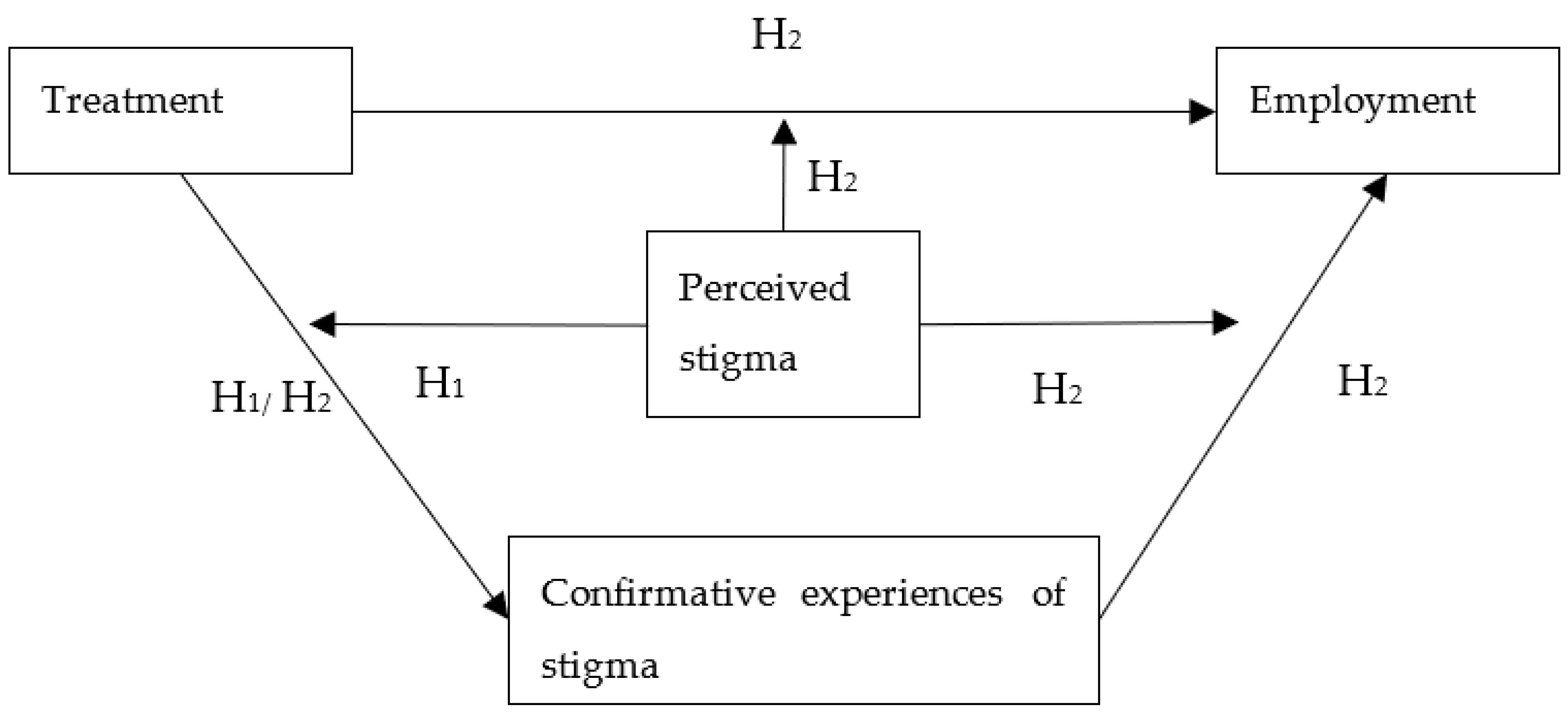
1.3. The Current Study
2. Materials and Methods
2.1. Data and Sample
2.2. Measurement
2.2.1. Dependent Variables
2.2.2. Independent Variables
2.2.3. Controlled Covariates
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Magura, S.; Staines, G.L.; Blankertz, L.; Madison, E.M. The Effectiveness of Vocational Services for Substance Users in Treatment. Subst. Use Misuse 2004, 39, 2165–2213. [Google Scholar] [CrossRef] [PubMed]
- Henkel, D. Unemployment and Substance Use: A Review of the Literature (1990-2010). Curr. Drug Abuse Rev. 2011, 4, 4–27. [Google Scholar] [CrossRef]
- Kessler, R.C.; House, J.S.; Turner, J.B. Unemployment and Health in a Community Sample. J. Health Soc. Behav. 1987, 51–59. [Google Scholar] [CrossRef]
- Magura, S.; Marshall, T. The Effectiveness of Interventions Intended to Improve Employment Outcomes for Persons with Substance Use Disorder: An Updated Systematic Review. Subst. Use Misuse 2020, 55, 2230–2236. [Google Scholar] [CrossRef] [PubMed]
- Walton, M.T.; Hall, M.T. The Effects of Employment Interventions on Addiction Treatment Outcomes: A Review of the Literature. J. Soc. Work Pract. Addict. 2016, 16, 358–384. [Google Scholar] [CrossRef]
- Fleury, M.-J.; Djouini, A.; Huỳnh, C.; Tremblay, J.; Ferland, F.; Ménard, J.-M.; Belleville, G. Remission from Substance Use Disorders: A Systematic Review and Meta-Analysis. Drug Alcohol Depend. 2016, 168, 293–306. [Google Scholar] [CrossRef]
- Smith, D.C.; Cleeland, L.; Dennis, M.L. Reasons for Quitting Among Emerging Adults and Adolescents in Substance-Use-Disorder Treatment*. J. Stud. Alcohol Drugs 2015. [Google Scholar] [CrossRef]
- Hammarlund, R.; Crapanzano, K.; Luce, L.; Mulligan, L.; Ward, K. Review of the Effects of Self-Stigma and Perceived Social Stigma on the Treatment-Seeking Decisions of Individuals with Drug- and Alcohol-Use Disorders. Subst. Abuse Rehabil. 2018, 9, 115–136. [Google Scholar] [CrossRef]
- Silverman, K.; Holtyn, A.F.; Morrison, R. The Therapeutic Utility of Employment in Treating Drug Addiction: Science to Application. Transl. Issues Psychol. Sci. 2016, 2, 203. [Google Scholar] [CrossRef]
- Mojtabai, R.; Chen, L.-Y.; Kaufmann, C.N.; Crum, R.M. Comparing Barriers to Mental Health Treatment and Substance Use Disorder Treatment among Individuals with Comorbid Major Depression and Substance Use Disorders. J. Subst. Abuse Treat. 2014, 46, 268–273. [Google Scholar] [CrossRef]
- Luoma, J.B.; Kohlenberg, B.S.; Hayes, S.C.; Bunting, K.; Rye, A.K. Reducing Self-Stigma in Substance Abuse through Acceptance and Commitment Therapy: Model, Manual Development, and Pilot Outcomes. Addict. Res. Theory 2008, 16, 149–165. [Google Scholar] [CrossRef] [PubMed]
- Goffman, E. Stigma: Notes on the Management of Spoiled Identity; Simon and Schuster: New York, NY, USA, 1963; ISBN 1-4391-8833-5. [Google Scholar]
- Jones, E.E. Social Stigma: The Psychology of Marked Relationships; WH Freeman: New York, NY, USA, 1984. [Google Scholar]
- Link, B.G.; Phelan, J.C. Conceptualizing Stigma. Annu. Rev. Sociol. 2001, 27, 363–385. [Google Scholar] [CrossRef]
- Palamar, J.J.; Halkitis, P.N.; Kiang, M.V. Perceived Public Stigma and Stigmatization in Explaining Lifetime Illicit Drug Use among Emerging Adults. Addict. Res. Theory 2013, 21, 516–525. [Google Scholar] [CrossRef]
- Schomerus, G.; Lucht, M.; Holzinger, A.; Matschinger, H.; Carta, M.G.; Angermeyer, M.C. The Stigma of Alcohol Dependence Compared with Other Mental Disorders: A Review of Population Studies. Alcohol Alcohol. Oxf. Oxfs. 2011, 46, 105–112. [Google Scholar] [CrossRef]
- Hing, N.; Russell, A.M.T. How Anticipated and Experienced Stigma Can Contribute to Self-Stigma: The Case of Problem Gambling. Front. Psychol. 2017, 8, 235. [Google Scholar] [CrossRef]
- Sibicky, M.; Dovidio, J.F. Stigma of Psychological Therapy: Stereotypes, Interpersonal Reactions, and the Self-Fulfilling Prophecy. J. Couns. Psychol. 1986, 33, 148–154. [Google Scholar] [CrossRef][Green Version]
- Kravitz, D.A. Affirmative Action. In Encyclopedia of Applied Psychology; Spielberger, C.D., Ed.; Elsevier: New York, NY, USA, 2004; pp. 65–77. ISBN 978-0-12-657410-4. [Google Scholar]
- Merton, R.K. The Self-Fulfilling Prophecy. Antioch Rev. 1948, 8, 193–210. [Google Scholar] [CrossRef]
- Luoma, J.B.; O’Hair, A.K.; Kohlenberg, B.S.; Hayes, S.C.; Fletcher, L. The Development and Psychometric Properties of a New Measure of Perceived Stigma Toward Substance Users. Subst. Use Misuse 2010, 45, 47–57. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Rao, D. On the Self-Stigma of Mental Illness: Stages, Disclosure, and Strategies for Change. Can. J. Psychiatry 2012, 57, 464–469. [Google Scholar] [CrossRef]
- Wahl, O.F. Mental Health Consumers’ Experience of Stigma. Schizophr. Bull. 1999, 25, 467–478. [Google Scholar] [CrossRef]
- Chi, P.; Li, X.; Zhao, J.; Zhao, G. Vicious Circle of Perceived Stigma, Enacted Stigma and Depressive Symptoms Among Children Affected by HIV/AIDS in China. AIDS Behav. 2014, 18, 1054–1062. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, P.W.; Larson, J.E.; Ruesch, N. Self-Stigma and the “Why Try” Effect: Impact on Life Goals and Evidence-Based Practices. World Psychiatry 2009, 8, 75. [Google Scholar] [CrossRef]
- da Silveira, P.S.; Casela, A.L.M.; Monteiro, É.P.; Ferreira, G.C.L.; de Freitas, J.V.T.; Machado, N.M.; Noto, A.R.; Ronzani, T.M. Psychosocial Understanding of Self-Stigma among People Who Seek Treatment for Drug Addiction. Stigma Health 2018, 3, 42–52. [Google Scholar] [CrossRef]
- Livingston, J.D.; Boyd, J.E. Correlates and Consequences of Internalized Stigma for People Living with Mental Illness: A Systematic Review and Meta-Analysis. Soc. Sci. Med. 2010, 71, 2150–2161. [Google Scholar] [CrossRef]
- Mak, W.W.S.; Ho, C.Y.Y.; Wong, V.U.T.; Law, R.W.; Chan, R.C.H. Cultural Model of Self-Stigma among Chinese with Substance Use Problems. Drug Alcohol Depend. 2015, 155, 83–89. [Google Scholar] [CrossRef]
- Tsang, H.W.; Fung, K.M.; Chung, R.C. Self-Stigma and Stages of Change as Predictors of Treatment Adherence of Individuals with Schizophrenia. Psychiatry Res. 2010, 180, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Vauth, R.; Kleim, B.; Wirtz, M.; Corrigan, P.W. Self-Efficacy and Empowerment as Outcomes of Self-Stigmatizing and Coping in Schizophrenia. Psychiatry Res. 2007, 150, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.; Shannon, L. Examining Barriers to and Motivations for Substance Abuse Treatment among Pregnant Women: Does Urban-Rural Residence Matter? Women Health 2012, 52, 570–586. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Watson, A.C. The Paradox of Self-Stigma and Mental Illness. Clin. Psychol. Sci. Pract. 2002, 9, 35–53. [Google Scholar] [CrossRef]
- Calabrese, S.K.; Burke, S.E.; Dovidio, J.F.; Levina, O.S.; Uusküla, A.; Niccolai, L.M.; Heimer, R. Internalized HIV and Drug Stigmas: Interacting Forces Threatening Health Status and Health Service Utilization among People with HIV Who Inject Drugs in St. Petersburg, Russia. AIDS Behav. 2016, 20, 85–97. [Google Scholar] [CrossRef]
- Zhang, R.; Mak, W.W.S.; Chan, R.C.H. Perceived Primal Threat of Mental Illness and Recovery: The Mediating Role of Self-Stigma and Self-Empowerment. Am. J. Orthopsychiatry 2017, 87, 44–51. [Google Scholar] [CrossRef]
- Keyes, K.M.; Hatzenbuehler, M.L.; McLaughlin, K.A.; Link, B.; Olfson, M.; Grant, B.F.; Hasin, D. Stigma and Treatment for Alcohol Disorders in the United States. Am. J. Epidemiol. 2010, 172, 1364–1372. [Google Scholar] [CrossRef] [PubMed]
- Gates, P.; Copeland, J.; Swift, W.; Martin, G. Barriers and Facilitators to Cannabis Treatment. Drug Alcohol Rev. 2012, 31, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Gourlay, J.; Ricciardelli, L.; Ridge, D. Users’ Experiences of Heroin and Methadone Treatment. Subst. Use Misuse 2005, 40, 1875–1882. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liu, L.; Chui, W.H. Rehabilitation Policy for Drug Addicted Offenders in China: Current Trends, Patterns, and Practice Implications. Asia Pac. J. Soc. Work Dev. 2018, 28, 192–204. [Google Scholar] [CrossRef]
- Lin, S.; Zhang, Y. Risk Control and Rational Recreation: A Qualitative Analysis of Synthetic Drug Use among Young Urbanites in China. Int. J. Drug Policy 2014, 25, 769–775. [Google Scholar] [CrossRef] [PubMed]
- Deng, Q.; Hu, M.; Yu, F.; Liu, Q.; Hao, W.; Wu, Q.; Luo, T. A Community-Based Investigation of Stigma Toward Individuals Receiving Methadone Maintenance Treatment in China: A Randomized Case Vignette Study. Front. Psychiatry 2020, 11, 1277. [Google Scholar] [CrossRef]
- Duan, S.; Jin, Z.; Liu, X.; Yang, Y.; Ye, R.; Tang, R.; Gao, M.; Ding, Y.; He, N. Tobacco and Alcohol Use among Drug Users Receiving Methadone Maintenance Treatment: A Cross-Sectional Study in a Rural Prefecture of Yunnan Province, Southwest China. BMJ Open 2017, 7, e014643. [Google Scholar] [CrossRef]
- Zhang, L.; Zou, X.; Xu, Y.; Medland, N.; Deng, L.; Liu, Y.; Su, S.; Ling, L. The Decade-Long Chinese Methadone Maintenance Therapy Yields Large Population and Economic Benefits for Drug Users in Reducing Harm, HIV and HCV Disease Burden. Front. Public Health 2019, 7, 327. [Google Scholar] [CrossRef]
- Li, Y.; Zeng, X.; Zhou, H. Relationship between Anxiety and Drug Abstention Motivation in Men with Substance Use Disorders: A Cross-Sectional Study of Compulsory Isolation Rehabilitation in China. J. Ethn. Subst. Abuse. 2021. [Google Scholar] [CrossRef]
- Yang, J.; Giummarra, M.J. Compulsory and Voluntary Drug Treatment Models in China: A Need for Improved Evidence-Based Policy and Practice to Reduce the Loaded Burden of Substance Use Disorders. Int. J. Drug Policy 2021, 92, 103063. [Google Scholar] [CrossRef]
- Li, L.; Liang, L.-J.; Lin, C.; Feng, N.; Wu, Z. Comparison Between Urinalysis Results and Self-Reported Heroin Use Among Patients Undergoing Methadone Maintenance Treatment in China. Subst. Use Misuse 2017, 52, 1307–1314. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Luo, T.; Wang, J.; Li, Y.; Wang, X.; Tan, L.; Deng, Q.; Thakoor, J.P.D.; Hao, W. Stigmatization of People with Drug Dependence in China: A Community-Based Study in Hunan Province. Drug Alcohol Depend. 2014, 134, 285–289. [Google Scholar] [CrossRef]
- Zhang, C.; Li, X.; Liu, Y.; Zhou, Y.; Shen, Z.; Chen, Y. Impacts of HIV Stigma on Psychosocial Well-Being and Substance Use Behaviors Among People Living With HIV/AIDS In China: Across the Life Span. AIDS Educ. Prev. 2018, 30, 108–119. [Google Scholar] [CrossRef] [PubMed]
- Brockner, J.; Chen, Y.-R. The Moderating Roles of Self-Esteem and Self-Construal in Reaction to a Threat to the Self: Evidence from the People’s Republic of China and the United States. J. Pers. Soc. Psychol. 1996, 71, 603. [Google Scholar] [CrossRef]
- Blume, A.W. Advances in Substance Abuse Prevention and Treatment Interventions among Racial, Ethnic, and Sexual Minority Populations. Alcohol Res. Curr. Rev. 2016, 38, 47. [Google Scholar]
- Bobrova, N.; Rhodes, T.; Power, R.; Alcorn, R.; Neifeld, E.; Krasiukov, N.; Latyshevskaia, N.; Maksimova, S. Barriers to Accessing Drug Treatment in Russia: A Qualitative Study among Injecting Drug Users in Two Cities. Drug Alcohol Depend. 2006, 82, S57–S63. [Google Scholar] [CrossRef]
- Conner, K.O.; Rosen, D. “You’re Nothing but a Junkie”: Multiple Experiences of Stigma in an Aging Methadone Maintenance Population. J. Soc. Work Pract. Addict. 2008, 8, 244–264. [Google Scholar] [CrossRef]
- Gunn, A.; Guarino, H. “Not Human, Dead Already”: Perceptions and Experiences of Drug-Related Stigma among Opioid-Using Young Adults from the Former Soviet Union Living in the US. Int. J. Drug Policy 2016, 38, 63–72. [Google Scholar] [CrossRef]
- Notley, C.; Maskrey, V.; Holland, R. The Needs of Problematic Drug Misusers Not in Structured Treatment–a Qualitative Study of Perceived Treatment Barriers and Recommendations for Services. Drugs Educ. Prev. Policy 2012, 19, 40–48. [Google Scholar] [CrossRef]
- Bojko, M.J.; Mazhnaya, A.; Makarenko, I.; Marcus, R.; Dvoriak, S.; Islam, Z.; Altice, F.L. “Bureaucracy & Beliefs”: Assessing the Barriers to Accessing Opioid Substitution Therapy by People Who Inject Drugs in Ukraine. Drugs Educ. Prev. Policy 2015, 22, 255–262. [Google Scholar]
- Khadjesari, Z.; Stevenson, F.; Godfrey, C.; Murray, E. Negotiating the ‘Grey Area between Normal Social Drinking and Being a Smelly Tramp’: A Qualitative Study of People Searching for Help Online to Reduce Their Drinking. Health Expect. 2015, 18, 2011–2020. [Google Scholar] [CrossRef] [PubMed]
- Gilchrist, G.; Moskalewicz, J.; Nutt, R.; Love, J.; Germeni, E.; Valkova, I.; Kantchelov, A.; Stoykova, T.; Bujalski, M.; Poplas-Susic, T. Understanding Access to Drug and Alcohol Treatment Services in Europe: A Multi-Country Service Users’ Perspective. Drugs Educ. Prev. Policy 2014, 21, 120–130. [Google Scholar] [CrossRef]
- Bifftu, B.B.; Dachew, B.A. Perceived Stigma and Associated Factors among People with Schizophrenia at Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia: A Cross-Sectional Institution Based Study. Psychiatry J. 2014, 2014, e694565. [Google Scholar] [CrossRef] [PubMed]
- Hadera, E.; Salelew, E.; Girma, E.; Dehning, S.; Adorjan, K.; Tesfaye, M. Magnitude and Associated Factors of Perceived Stigma among Adults with Mental Illness in Ethiopia. Psychiatry J. 2019, 2019, 8427561. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.Y.; Strain, E.C.; Crum, R.M.; Mojtabai, R. Gender Differences in Substance Abuse Treatment and Barriers to Care among Persons with Substance Use Disorders with and without Comorbid Major Depression. J. Addict. Med. 2013, 7, 325. [Google Scholar] [CrossRef]
- Derogatis, L.R. BSI Brief Symptom Inventory. Adm. Scoring Proced. Man. 1993. [Google Scholar]
- Mattoo, S.K.; Sarkar, S.; Gupta, S.; Nebhinani, N.; Parakh, P.; Basu, D. Stigma Towards Substance Use: Comparing Treatment Seeking Alcohol and Opioid Dependent Men. Int. J. Ment. Health Addict. 2015, 13, 73–81. [Google Scholar] [CrossRef]
- Haile, S.R. Interpreting Interactions 2017. Available online: https://www.ebpi.uzh.ch/dam/jcr:5764104b-a3b3-451d-828d-34bed6c804fb/InteractionsStataR20170622.pdf (accessed on 29 November 2021).
- Breen, R.; Karlson, K.B.; Holm, A. Total, Direct, and Indirect Effects in Logit and Probit Models. Sociol. Methods Res. 2013, 42, 164–191. [Google Scholar] [CrossRef]
- Kohler, U.; Karlson, K.B.; Holm, A. Comparing Coefficients of Nested Nonlinear Probability Models. Stata J. 2011, 11, 420–438. [Google Scholar] [CrossRef]
- Brown, S.A.; Kramer, K.; Lewno, B.; Dumas, L.; Sacchetti, G.; Powell, E. Correlates of Self-Stigma among Individuals with Substance Use Problems. Int. J. Ment. Health Addict. 2015, 13, 687–698. [Google Scholar] [CrossRef]
- Luoma, J.B.; Nobles, R.H.; Drake, C.E.; Hayes, S.C.; O’Hair, A.; Fletcher, L.; Kohlenberg, B.S. Self-Stigma in Substance Abuse: Development of a New Measure. J. Psychopathol. Behav. Assess. 2013, 35, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Crockett, K.B.; Kalichman, S.C.; Kalichman, M.O.; Cruess, D.G.; Katner, H.P. Experiences of HIV-Related Discrimination and Consequences for Internalised Stigma, Depression and Alcohol Use. Psychol. Health 2019, 34, 796–810. [Google Scholar] [CrossRef] [PubMed]
- Arria, A.M.; Garnier-Dykstra, L.M.; Cook, E.T.; Caldeira, K.M.; Vincent, K.B.; Baron, R.A.; O’Grady, K.E. Drug Use Patterns in Young Adulthood and Post-College Employment. Drug Alcohol Depend. 2013, 127, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Holtyn, A.F.; Toegel, F.; Novak, M.D.; Silverman, K. Factors Associated with Obtaining Employment among Opioid Use Disorder Patients Enrolled in a Therapeutic Workplace Intervention. Drug Alcohol Depend. 2021, 226, 108907. [Google Scholar] [CrossRef]
- Mittal, D.; Sullivan, G.; Chekuri, L.; Allee, E.; Corrigan, P.W. Empirical Studies of Self-Stigma Reduction Strategies: A Critical Review of the Literature. Psychiatr. Serv. 2012, 63, 974–981. [Google Scholar] [CrossRef]
- Aho-Mustonen, K.; Tiihonen, J.; Repo-Tiihonen, E.; Ryynänen, O.-P.; Miettinen, R.; Räty, H. Group Psychoeducation for Long-term Offender Patients with Schizophrenia: An Exploratory Randomised Controlled Trial. Crim. Behav. Ment. Health 2011, 21, 163–176. [Google Scholar] [CrossRef] [PubMed]
| Female | Male | Total | |
|---|---|---|---|
| N | 339 (8.01%) | 3893 (91.99%) | 4232 (100.00%) |
| N of employed | 239 (70.50%) | 2974 (76.39%) | 3217 (76.02%) |
| N having confirmative experiences of stigma | 163 (48.08%) | 2216 (56.92%) | 2387 (56.40%) |
| N participating in treatment | |||
| Community treatment | 315 (92.92%) | 3609 (92.70%) | 3933 (92.94%) |
| Institutional treatment | 314 (92.63%) | 3601 (92.50%) | 3924 (92.72%) |
| Reentry treatment | 304 (89.68%) | 3571 (91.73%) | 3884 (91.78%) |
| Employment treatment | 308 (90.86%) | 3505 (90.03%) | 3821 (90.29%) |
| N not having perceived stigma | 154 (45.43%) | 1794 (46.08%) | 1951 (46.10%) |
| Ms of psychological symptoms | |||
| Anxiety | 1.31 (0.03) | 1.28 (0.01) | 1.27 (0.01) |
| Depression | 1.31 (0.03) | 1.29 (0.01) | 1.30 (0.01) |
| Somatization | 1.26 (0.03) | 1.26 (0.01) | 1.26 (0.01) |
| M of abstinence duration (month) | 3.28 (0.06) | 3.33 (0.02) | 3.32 (0.02) |
| M of personal monthly income (1000 CNY) | 3.94 (0.09) | 4.37 (0.02) | 4.34 (1.47) |
| M of years of education | 8.81 (0.17) | 8.53 (0.05) | 8.55 (0.05) |
| M of years of age | 33.85 (0.47) | 38.36 (0.15) | 38.00 (0.15) |
| N of married | 159 (46.90%) | 2224 (57.13%) | 2387 (56.40%) |
| N having at least one child | 190 (56.05%) | 2558 (65.71%) | 2752 (65.02%) |
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| Predictors | OR | 95% C.I. | OR | 95% C.I. | OR | 95% C.I. |
| Psychological symptoms | ||||||
| Anxiety | 0.82 | 0.59~1.12 | 0.86 | 0.61~1.21 | 0.87 | 0.62~1.22 |
| Depression | 0.46 *** | 0.34~0.62 | 0.57 *** | 0.42~0.79 | 0.56 *** | 0.41~0.77 |
| Somatization | 1.09 | 0.84~1.43 | 1.18 | 0.88~1.57 | 1.18 | 0.88~1.57 |
| Duration of abstinence (month) | 1.04 | 0.97~1.11 | 1.00 | 0.93~1.07 | 1.00 | 0.94~1.08 |
| Type of substance (Base = no usage) | ||||||
| Heroin | 1.10 | 0.92~1.31 | 1.16 | 0.95~1.41 | 1.15 | 0.94~1.39 |
| Methamphetamines | 0.84 * | 0.72~0.99 | 0.94 | 0.79~1.13 | 0.95 | 0.79~1.13 |
| Other | 1.02 | 0.84~1.24 | 1.05 | 0.85~1.29 | 1.04 | 0.84~1.28 |
| Demographics | ||||||
| Male (Base = female) | 0.63 *** | 0.49~0.80 | 0.57 *** | 0.44~0.75 | 0.58 *** | 0.45~0.76 |
| Have at least one child (Base = none) | 0.88 | 0.73~1.06 | 0.92 | 0.75~1.14 | 0.92 | 0.75~1.14 |
| Married (Base = others) | 1.13 | 0.95~1.36 | 1.21 | 0.99~1.47 | 1.22 * | 1.00~1.49 |
| Personal monthly income (CNY) | 1.00 *** | 1.00~1.00 | 1.00 *** | 1.00~1.00 | 1.00 *** | 1.00~1.00 |
| Years of education | 1.01 | 0.98~1.03 | 1.01 | 0.98~1.03 | 1.01 | 0.98~1.04 |
| Years of age | 1.00 | 0.99~1.01 | 0.99 | 0.98~1.00 | 0.99 | 0.98~1.00 |
| Treatments (Base = not participating in one of the treatments below) | ||||||
| Community treatment | 1.04 | 0.75~1.45 | 1.10 | 0.71~1.72 | ||
| Institutional treatment | 0.88 | 0.64~1.23 | 0.85 | 0.56~1.29 | ||
| Reentry treatment | 1.05 | 0.74~1.47 | 0.88 | 0.58~1.35 | ||
| Employment treatment | 1.00 | 0.74~1.36 | 0.70 * | 1.00~2.03 | ||
| No perceived stigma (Base = having perceived stigma) | 6.20 *** | 5.36~7.16 | 2.27 ** | 0.49~1.00 | ||
| Moderation terms | ||||||
| Community treatment × No perceived stigma | 0.82 | 0.42~1.60 | ||||
| Institutional treatment × No perceived stigma | 1.17 | 0.62~2.20 | ||||
| Reentry treatment × No perceived stigma | 1.42 | 0.76~2.68 | ||||
| Employment treatment × No perceived stigma | 2.22 *** | 1.29~3.81 | ||||
| Goodness-of-fit | ||||||
| Wald test (df) | 181.29 *** (13) | 766.95 *** (18) | 782.24 *** (22) | |||
| Likelihood ratio (df) | 676.83 *** (5) | 17.19 *** (4) | ||||
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| Predictors | OR | 95% C.I. | OR | 95% C.I. | OR | 95% C.I. |
| Psychological symptoms | ||||||
| Anxiety | 0.90 | 0.64~1.28 | 0.94 | 0.66~1.33 | 0.94 | 0.66~1.34 |
| Depression | 0.91 | 0.69~1.19 | 0.88 | 0.66~1.16 | 0.88 | 0.67~1.16 |
| Somatization | 0.89 | 0.65~1.21 | 0.93 | 0.68~1.27 | 0.92 | 0.68~1.26 |
| Duration of abstinence (month) | 0.96 | 0.88~1.04 | 0.95 | 0.88~1.04 | 0.95 | 0.88~1.03 |
| Type of substance (Base = no usage) | ||||||
| Heroin | 1.40 *** | 1.11~1.78 | 1.44 *** | 1.13~1.84 | 1.44 *** | 1.13~1.84 |
| Methamphetamines | 1.20 | 0.96~1.49 | 1.18 | 0.95~1.48 | 1.18 | 0.95~1.48 |
| Other | 0.96 | 0.75~1.24 | 0.98 | 0.75~1.27 | 0.98 | 0.76~1.27 |
| Demographics | ||||||
| Male (Base = female) | 1.09 | 0.81~1.48 | 1.07 | 0.79~1.46 | 1.07 | 0.79~1.46 |
| Have at least one child (Base = none) | 1.01 | 0.79~1.30 | 1.04 | 0.81~1.34 | 1.04 | 0.81~1.33 |
| Married (Base = others) | 1.24 | 0.98~1.57 | 1.23 | 0.97~1.57 | 1.24 | 0.98~1.57 |
| Personal monthly income (CNY) | 1.00 *** | 1.00~1.00 | 1.00 *** | 1.00~1.00 | 1.00 *** | 1.00~1.00 |
| Years of education | 0.97 | 0.94~1.01 | 0.97 | 0.94~1.01 | 0.97 | 0.94~1.01 |
| Years of age | 0.98 *** | 0.97~0.99 | 0.98 *** | 0.97~0.99 | 0.98 *** | 0.97~0.99 |
| Treatment (Base = not participating in one of the treatments below) | ||||||
| Community treatment | 1.65 *** | 1.17~2.33 | 1.28 | 0.81~2.02 | ||
| Institutional treatment | 1.03 | 0.72~1.46 | 1.30 | 0.82~2.07 | ||
| Reentry treatment | 0.83 | 0.57~1.21 | 0.79 | 0.49~1.30 | ||
| Employment treatment | 2.07 *** | 1.48~2.90 | 2.01 ** | 1.33~3.03 | ||
| No confirmative experience of stigma (Base = having confirmative experiences of stigma) | 0.81 * | 0.67~0.99 | 0.95 | 0.71~1.27 | ||
| No perceived stigma(Base = having perceived stigma) | 0.99 *** | 0.82~1.21 | 0.97 | 0.41~2.26 | ||
| Moderation terms | ||||||
| Community treatment × No perceived stigma | 1.93 * | 0.96~3.88 | ||||
| Institutional treatment × No perceived stigma | 0.57 | 0.27~1.17 | ||||
| Reentry treatment × No perceived stigma | 1.02 | 0.47~2.22 | ||||
| Employment treatment × No perceived stigma | 1.08 | 0.54~2.19 | ||||
| No confirmative experience of stigma × No perceived stigma | 0.74 | 0.49~1.10 | ||||
| Goodness-of-fit | ||||||
| Wald test (df) | 1036.14 *** (13) | 1080.91 *** (19) | 1087.97 *** (24) | |||
| Likelihood ratio (df) | 44.77 *** (6) | 7.06 (5) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, L.; Jia, C.X. Treatments, Perceived Stigma, and Employment Outcomes among Substance Abusers in China. Healthcare 2022, 10, 130. https://doi.org/10.3390/healthcare10010130
Han L, Jia CX. Treatments, Perceived Stigma, and Employment Outcomes among Substance Abusers in China. Healthcare. 2022; 10(1):130. https://doi.org/10.3390/healthcare10010130
Chicago/Turabian StyleHan, Li, and Cindy Xinshan Jia. 2022. "Treatments, Perceived Stigma, and Employment Outcomes among Substance Abusers in China" Healthcare 10, no. 1: 130. https://doi.org/10.3390/healthcare10010130
APA StyleHan, L., & Jia, C. X. (2022). Treatments, Perceived Stigma, and Employment Outcomes among Substance Abusers in China. Healthcare, 10(1), 130. https://doi.org/10.3390/healthcare10010130






