Awareness and Related Factors of Dyslipidemia in Menopausal Women in Korea
Abstract
:1. Introduction
2. Methods
2.1. Research Design
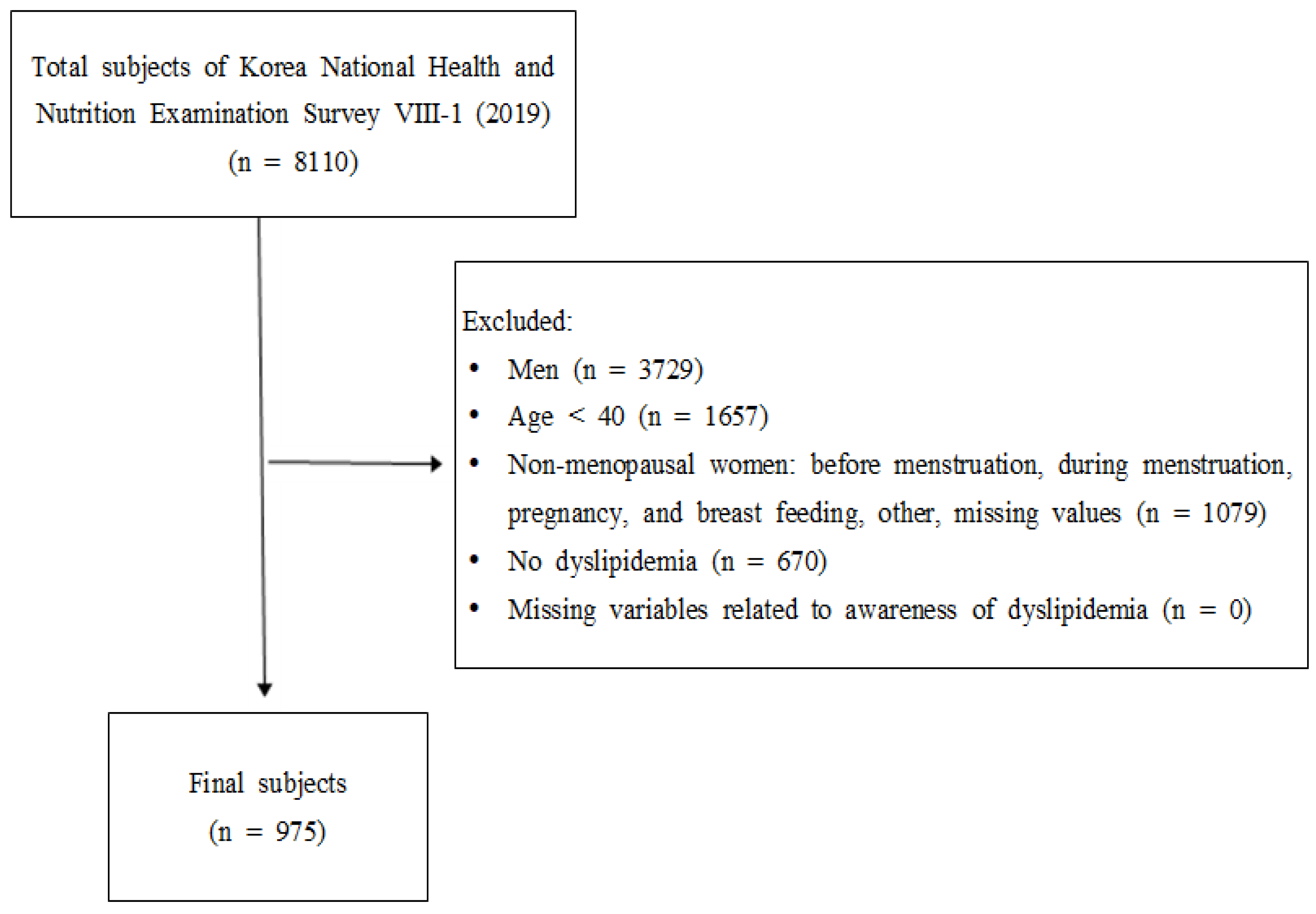
2.2. Research Data and Subjects
2.3. Variable Selection
2.3.1. General Characteristics
2.3.2. Health-Related Characteristics
2.3.3. Dyslipidemia Awareness Level
2.4. Data Analysis Method
2.5. Ethical Considerations
3. Results
3.1. Subjects’ General and Health-Related Characteristics and Awareness Level on Dyslipidemia
3.2. Factors Related to the Subjects’ Dyslipidemia Awareness Level
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jee, S.H.; Jang, Y.; Oh, D.J.; Oh, B.-H.; Lee, S.H.; Park, S.-W.; Seung, K.-B.; Mok, Y.; Jung, K.J.; Kimm, H.; et al. A coronary heart disease prediction model: The Korean Heart Study. BMJ Open 2014, 4, e005025. [Google Scholar] [CrossRef] [PubMed]
- Reiner, Z.; Catapano, A.L.; De Backer, G.; Graham, I.; Taskinen, M.R.; Wiklund, O.; Agewall, S.; Alegria, E.; Chapman, M.J.; Durrington, P.N.; et al. ESC/EAS Guidelines for the management of dyslipidaemias: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur. Hear. J. 2011, 32, 1769–1818. [Google Scholar] [CrossRef] [Green Version]
- Di Francesco, S.; Caruso, M.; Robuffo, I.; Militello, A.; Toniato, E. The Impact of Metabolic Syndrome and Its Components on Female Sexual Dysfunction: A Narrative Mini-Review. Curr. Urol. 2019, 12, 57–63. [Google Scholar] [CrossRef]
- Carr, M.C. The Emergence of the Metabolic Syndrome with Menopause. J. Clin. Endocrinol. Metab. 2003, 88, 2404–2411. [Google Scholar] [CrossRef] [PubMed]
- Sook, K.K. Related Factors of Dyslipidemia among Pre- and Post-Menopausal Women in South Korea-Based on the Data of the Sixth Korea National Health and Nutrition Examination Survey (2013~2015). Asia-Pac. J. Multimed. Serv. Converg. Art Humanit. Soc. 2018, 8, 139–152. [Google Scholar] [CrossRef]
- Rhee, E.-J. Prevalence and Current Management of Cardiovascular Risk Factors in Korean Adults Based on Fact Sheets. Endocrinol. Metab. 2020, 35, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Miner, M.; Esposito, K.; Guay, A.; Montorsi, P.; Goldstein, I. Cardiometabolic Risk and Female Sexual Health: The Princeton III Summary (CME). J. Sex. Med. 2012, 9, 641–651. [Google Scholar] [CrossRef]
- Servadei, F.; Anemona, L.; Cardellini, M.; Scimeca, M.; Montanaro, M.; Rovella, V.; Di Daniele, F.; Giacobbi, E.; Legramante, I.M.; Noce, A.; et al. The risk of carotid plaque instability in patients with metabolic syndrome is higher in women with hypertriglyceridemia. Cardiovasc. Diabetol. 2021, 20, 98. [Google Scholar] [CrossRef]
- Ke, C.; Zhu, X.; Zhang, Y.; Shen, Y. Metabolomic characterization of hypertension and dyslipidemia. Metabolomics 2018, 14, 117. [Google Scholar] [CrossRef]
- Eltoft, A.; Arntzen, K.A.; Wilsgaard, T.; Mathiesen, E.B.; Johnsen, S.H. Interleukin-6 is an independent predictor of progressive atherosclerosis in the carotid artery: The Tromsø Study. Atherosclerosis 2018, 271, 1–8. [Google Scholar] [CrossRef] [PubMed]
- März, W.; Scharnagl, H.; Winkler, K.; Tiran, A.; Nauck, M.; Boehm, B.O.; Winkelmann, B.R. Low-Density Lipoprotein Triglycerides Associated With Low-Grade Systemic Inflammation, Adhesion Molecules, and Angiographic Coronary Artery Disease. Circulation 2004, 110, 3068–3074. [Google Scholar] [CrossRef] [Green Version]
- Nordestgaard, B.G. Triglyceride-Rich Lipoproteins and Atherosclerotic Cardiovascular Disease. Circ. Res. 2016, 118, 547–563. [Google Scholar] [CrossRef]
- Doi, H.; Kugiyama, K.; Oka, H.; Sugiyama, S.; Ogata, N.; Koide, S.-I.; Nakamura, S.-I.; Yasue, H. Remnant Lipoproteins Induce Proatherothrombogenic Molecules in Endothelial Cells Through a Redox-Sensitive Mechanism. Circulation 2000, 102, 670–676. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Libby, P.; Ridker, P.M.; Maseri, A. Inflammation and Atherosclerosis. Circulation 2002, 105, 1135–1143. [Google Scholar] [CrossRef] [PubMed]
- Toth, P.; Phan, B.A. Dyslipidemia in women: Etiology and management. Int. J. Women’s Health 2014, 6, 185–194. [Google Scholar] [CrossRef] [Green Version]
- Gomina, M.; Ele, R.; Imorou, R.; Alassani, A.; Djidonou, G.; Sina, H.; Baba-Moussa, L.; Simon, A. Prevalence and Factors Associated with Dyslipidemia among Menopausal Women in the City of Parakou (Benin). Int. Res. J. Biochem. Bioinform. 2017, 7, 12–18. [Google Scholar] [CrossRef]
- O’Meara, J.G.; Kardia, S.L.R.; Armon, J.J.; Brown, C.A.; Boerwinkle, E.; Turner, S.T. Ethnic and Sex Differences in the Prevalence, Treatment, and Control of Dyslipidemia Among Hypertensive Adults in the GENOA Study. Arch. Intern. Med. 2004, 164, 1313–1318. [Google Scholar] [CrossRef] [Green Version]
- Busari, O.A.; Olanrewaju, T.O.; Desalu, O.O.; Opadijo, O.G.; Jimoh, A.K.; Agboola, S.M.; Busari, O.E.; Olalekan, O. Impact of Patients’ Knowledge, Attitude and Practices on Hypertension on Compliance with Antihypertensive Drugs in a Resource-Poor Setting. TAF Prev. Med. Bull. 2010, 9, 87–92. [Google Scholar]
- Boo, S.; Yoon, Y.J.; Oh, H. Evaluating the prevalence, awareness, and control of hypertension, diabetes, and dyslipidemia in Korea using the NHIS-NSC database. Medicine 2018, 97, e13713. [Google Scholar] [CrossRef] [PubMed]
- Alkerwi, A.; Pagny, S.; Lair, M.-L.; Delagardelle, C.; Beissel, J. Level of Unawareness and Management of Diabetes, Hypertension, and Dyslipidemia among Adults in Luxembourg: Findings from ORISCAV-LUX Study. PLoS ONE 2013, 8, e57920. [Google Scholar] [CrossRef]
- Leuzzi, C.; Marzullo, R.; Modena, M.G. La menopausa è un fattore di rischio per la cardiopatia ischemica? G Italy Cardiol. 2012, 13, 401–406. [Google Scholar] [CrossRef]
- The Eighth Korea National Health and Nutrition Examination Survey (KNHANES VIII-1). Available online: https://knhanes.kdca.go.kr/knhanes/sub03/sub03_02_05.do (accessed on 10 August 2021).
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cho-lesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation 2002, 106, 3143–3421. [CrossRef]
- Kim, J.; Ahn, S. Impact of Menopausal Status, Metabolic Syndrome and its Risk Factors on Impaired Quality of Life above Middle-aged Women. Korean J. Women Health Nurs. 2016, 22, 275–286. [Google Scholar] [CrossRef] [Green Version]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- The Asian-Pacific Perspective: Redefining Obesity and Its Treatment. Available online: https://apps.who.int/iris/handle/10665/206936 (accessed on 21 August 2021).
- Clinical Guideline for Obesity Treat-Ment. Available online: http://General.Kosso.or.Kr/Html/?Pmode=BBBS0001300003 (accessed on 19 August 2021).
- Kim, S.J.; Kwon, O.D.; Lee, E.-J.; Ock, S.M.; Kim, K.-S. Impact of a family history of cardiovascular disease on prevalence, awareness, treatment, control of dyslipidemia, and healthy behaviors: Findings from the Korea National Health and Nutrition Examination Survey. PLoS ONE 2021, 16, e0254907. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Yang, Z.; Wu, Y.; Yin, R.-X.; Liao, Y.; Wang, J.; Gao, B.; Zhang, L. The prevalence, awareness, treatment and control of dyslipidemia among adults in China. Atherosclerosis 2016, 248, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.K.; Choi, H.M.; Kim, M.H. Menopausal Knowledge and Management in Peri-menopausal Women. J. Korean Soc. Menopause 2012, 18, 124–131. [Google Scholar] [CrossRef] [Green Version]
- Schoenaker, D.A.; A Jackson, C.; Rowlands, J.V.; Mishra, G.D. Socioeconomic position, lifestyle factors and age at natural menopause: A systematic review and meta-analyses of studies across six continents. Int. J. Epidemiol. 2014, 43, 1542–1562. [Google Scholar] [CrossRef] [Green Version]
- Zhu, D.; Chung, H.-F.; Dobson, A.J.; Pandeya, N.; Giles, G.G.; Bruinsma, F.; Brunner, E.; Kuh, D.; Hardy, R.; E Avis, N.; et al. Age at natural menopause and risk of incident cardiovascular disease: A pooled analysis of individual patient data. Lancet Public Health 2019, 4, e553–e564. [Google Scholar] [CrossRef] [Green Version]
- Mosca, L.; Benjamin, E.J.; Berra, K.; Bezanson, J.L.; Dolor, R.J.; Lloyd-Jones, D.M.; Newby, L.K.; Piña, I.L.; Roger, V.L.; Shaw, L.J.; et al. Effectiveness-Based Guidelines for the Prevention of Cardiovascular Disease in Women—2011 Update: A Guideline from the American Heart Association. J. Am. Coll. Cardiol. 2011, 57, 1404–1423. [Google Scholar] [CrossRef] [Green Version]
- Rosenstock, I.M. Why People Use Health Services. Milbank Mem. Fund Q. 1966, 44, 94. [Google Scholar] [CrossRef] [Green Version]
- Zhu, D.; Chung, H.-F.; Pandeya, N.; Dobson, A.J.; Kuh, D.; Crawford, S.L.; Gold, E.B.; Avis, N.E.; Giles, G.G.; Bruinsma, F.; et al. Body mass index and age at natural menopause: An international pooled analysis of 11 prospective studies. Eur. J. Epidemiol. 2018, 33, 699–710. [Google Scholar] [CrossRef]
- Kapoor, E.; Collazo-Clavell, M.L.; Faubion, S.S. Weight Gain in Women at Midlife: A Concise Review of the Pathophysiology and Strategies for Management. Mayo Clin. Proc. 2017, 92, 1552–1558. [Google Scholar] [CrossRef]
- Hee, K.Y. Health Promoting Lifestyle, Self-Efficacy, and Life Satisfaction of Middle-Aged Women. J. Korean Data Anal. Soc. 2013, 15, 937–948. [Google Scholar]
- Kuwabara, M.; Kuwabara, R.; Niwa, K.; Hisatome, I.; Smits, G.; Roncal-Jimenez, C.A.; MacLean, P.S.; Yracheta, J.M.; Ohno, M.; Lanaspa, M.A.; et al. Different Risk for Hypertension, Diabetes, Dyslipidemia, and Hyperuricemia According to Level of Body Mass Index in Japanese and American Subjects. Nutrients 2018, 10, 1011. [Google Scholar] [CrossRef] [Green Version]
- Rawshani, A.; Rawshani, A.; Rawshani, A.; Franzén, S.; Sattar, N.; Eliasson, B.; Svensson, A.-M.; Zethelius, B.; Miftaraj, M.; McGuire, D.K.; et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. New Engl. J. Med. 2018, 379, 633–644. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Kwon, O.D.; Kim, K.-S. Prevalence, awareness, treatment, and control of dyslipidemia among diabetes mellitus patients and predictors of optimal dyslipidemia control: Results from the Korea National Health and Nutrition Examination Survey. Lipids Health Dis. 2021, 20, 29. [Google Scholar] [CrossRef]
- Di Francesco, S.; Tenaglia, R.L. Obesity, Diabetes Mellitus and Vascular Disease: A Complex Relationship with Prostate Cancer. J. Cancer Ther. 2014, 5, 442–447. [Google Scholar] [CrossRef] [Green Version]
- Francesco, S.; Tenaglia, R. The Association of Obesity and Sistemic Arterial Hypertension with High-Grade Prostate Cancer: Our Experience. J. Cancer Res. Updates 2014, 3, 191–195. [Google Scholar] [CrossRef]
| Characteristics | n (%) | Dyslipidemia Awareness | p | |||
|---|---|---|---|---|---|---|
| Rate | Yes, n (%) | No, n (%) | ||||
| Total | 27.3 | 270 (100) | 705 (100) | |||
| Age (yrs) | 40–49 | 25 (3.0) | 2.1 | 1 (0.2) | 24 (4.1) | <0.001 |
| 50–59 | 339 (39.9) | 21.0 | 72 (30.7) | 267 (43.3) | ||
| 60–69 | 335 (32.2) | 33.6 | 111 (39.7) | 224 (29.4) | ||
| ≥70 | 276 (24.6) | 32.2 | 86 (29.4) | 190 (23.2) | ||
| M ± SE | 62.85 ± 0.38 | |||||
| Residence | County | 233 (21.0) | 25.8 | 65 (19.9) | 168 (21.4) | 0.611 |
| City | 742 (79.0) | 27.6 | 205 (80.1) | 537 (78.6) | ||
| Educational level * (n = 965) | Elementary school or less | 367 (34.8) | 34.4 | 125 (43.8) | 251 (31.4) | 0.004 |
| Middle school | 148 (14.7) | 27.7 | 45 (14.9) | 103 (14.6) | ||
| High school | 289 (33.1) | 24.2 | 69 (29.3) | 220 (34.5) | ||
| College or higher | 161 (17.4) | 18.7 | 31 (12.0) | 130 (19.5) | ||
| Currently working | No | 541 (54.9) | 30.0 | 165 (60.4) | 376 (58.2) | 0.059 |
| Yes | 434 (45.1) | 23.9 | 105 (39.6) | 329 (47.2) | ||
| Household Income (in quartile) * (n = 970) | High | 224 (24.3) | 20.1 | 48 (18.1) | 176 (26.6) | 0.062 |
| Upper-middle | 215 (23.8) | 27.1 | 59 (23.9) | 156 (23.8) | ||
| Lower-middle | 238 (23.5) | 27.9 | 70 (24.2) | 168 (23.2) | ||
| Low | 293 (28.4) | 32.2 | 91 (33.7) | 202 (26.4) | ||
| Spouse | Yes | 659 (69.8) | 24.9 | 172 (63.7) | 487 (72.1) | 0.031 |
| No | 316 (30.2) | 32.8 | 98 (36.3) | 218 (27.9) | ||
| Menopause period (yrs) * (n = 965) | <10 | 393 (45.5) | 19.2 | 79 (32.1) | 314 (50.6) | <0.001 |
| ≥10 | 572 (54.5) | 34.0 | 189 (67.9) | 383 (49.4) | ||
| M ± SE | 12.91 ± 0.43 | |||||
| Characteristics | n (%) | Dyslipidemia Awareness | p | |||
|---|---|---|---|---|---|---|
| Rate | Yes, n (%) | No, n (%) | ||||
| Total | 27.3 | 270 (100) | 705 (100) | |||
| Perceived health status | Good | 226 (22.9) | 20.3 | 44 (17.0) | 182 (25.1) | <0.001 |
| Not bad | 518 (54.9) | 24.8 | 131 (50.0) | 387 (56.8) | ||
| Bad | 231 (22.2) | 40.5 | 95 (33.0) | 136 (18.2) | ||
| Health screening * (n = 974) | No | 248 (26.1) | 32.0 | 72 (30.6) | 176 (24.4) | 0.104 |
| Yes | 726 (73.9) | 25.6 | 198 (69.4) | 528 (75.6) | ||
| Smoking * (n = 973) | Non-smoker | 890 (90.9) | 26.4 | 240 (87.9) | 650 (92.0) | 0.203 |
| Ex-smoker | 41 (4.0) | 33.4 | 14 (4.9) | 27 (3.6) | ||
| Current smoker | 42 (5.1) | 38.6 | 16 (7.2) | 26 (4.3) | ||
| Drinking amount * (n = 973) | None | 701 (70.5) | 30.3 | 210 (78.1) | 491 (67.7) | 0.045 |
| ≤2 glass | 148 (15.3) | 19.4 | 32 (10.9) | 116 (16.9) | ||
| 3–6 glass | 97 (11.3) | 20.9 | 22 (8.7) | 75 (12.3) | ||
| ≥7 glass | 27 (2.9) | 22.6 | 6 (2.4) | 21 (3.1) | ||
| Exercise * (n = 974) | No | 886 (90.9) | 27.2 | 248 (90.7) | 638 (91.0) | 0.890 |
| Yes | 88 (9.1) | 28.0 | 22 (9.3) | 66 (9.0) | ||
| Diet * (n = 883) | No | 618 (69.7) | 25.6 | 159 (65.8) | 459 (71.1) | 0.182 |
| Yes | 265 (30.3) | 30.6 | 86 (34.2) | 179 (28.9) | ||
| Body mass index (kg/m2) * (n = 971) | <22.9 (normal) | 374 (38.5) | 20.5 | 81 (28.9) | 293 (42.0) | 0.003 |
| 23.0–24.9 (overweight) | 250 (26.3) | 27.8 | 66 (26.8) | 184 (26.1) | ||
| ≥25 (obese) | 347 (35.2) | 34.3 | 122 (44.3) | 225 (31.8) | ||
| Underlying disease | None | 621 (64.5) | 17.4 | 112 (41.2) | 509 (73.3) | <0.001 |
| Hypertension only | 241 (24.3) | 36.2 | 89 (32.3) | 152 (21.3) | ||
| Diabetes mellitus only | 35 (3.2) | 60.7 | 18 (7.2) | 17 (1.8) | ||
| Both | 78 (7.9) | 66.2 | 51 (19.3) | 27 (3.7) | ||
| Family history * (n = 892) | No | 505 (55.0) | 26.1 | 131 (54.4) | 374 (55.2) | 0.859 |
| Yes | 387 (45.0) | 26.7 | 111 (45.6) | 276 (44.8) | ||
| Characteristics | Simple Logistic Regression | Multiple Logistic Regression | |||
|---|---|---|---|---|---|
| Adjusted OR (95% CI) | p | Adjusted OR (95% CI) | p | ||
| Age (yrs) | 40–49 | 1 | 1 | ||
| 50–59 | 12.32 (1.56–97.32) | 0.018 | 12.77 (1.59–102.58) | 0.017 | |
| 60–69 | 23.44 (3.10–177.06) | 0.002 | 14.71 (1.82–118.74) | 0.012 | |
| ≥70 | 21.98 (2.78–173.50) | 0.004 | 7.50 (0.82–68.29) | 0.073 | |
| Residence | County | 1 | |||
| City | 1.10 (0.77–1.56) | 0.611 | |||
| Educational level | Elementary school or less | 1 | 1 | ||
| Middle school | 0.73 (0.44–1.21) | 0.218 | 1.20 (0.67–2.15) | 0.534 | |
| High school | 0.61 (0.44–0.85) | 0.004 | 1.13 (0.66–1.93) | 0.663 | |
| College or higher | 0.44 (0.28–0.69) | <0.001 | 1.12 (0.58–2.15) | 0.742 | |
| Currently working | No | 1 | |||
| Yes | 0.73 (0.53–1.01) | 0.059 | |||
| Household income (in quartile) | High | 1 | 1 | ||
| Upper-middle | 1.48 (0.90–2.45) | 0.124 | 1.23 (0.74–2.04) | 0.424 | |
| Lower-middle | 1.54 (0.93–2.54) | 0.091 | 0.99 (0.57–1.72) | 0.976 | |
| Low | 1.89 (1.21–2.93) | 0.005 | 1.07 (0.58–1.96) | 0.825 | |
| Spouse | Yes | 1 | 1 | ||
| No | 1.47 (1.04–2.10) | 0.032 | 1.27 (0.83–1.97) | 0.273 | |
| Menopause period (yrs) | <10 | 1 | 1 | ||
| ≥10 | 2.17 (1.56–3.01) | <0.001 | 1.57 (0.98–2.51) | 0.058 | |
| Perceived health status | Good | 1 | 1 | ||
| Not bad | 1.30 (0.83–2.03) | 0.255 | 1.31 (0.80–2.13) | 0.284 | |
| Bad | 2.68 (1.70–4.22) | <0.001 | 2.10 (1.27–3.48) | 0.004 | |
| Health Screening | No | 1 | |||
| Yes | 0.73 (0.50–1.07) | 0.105 | |||
| Smoking | Non-smoker | 1 | |||
| Ex-smoker | 1.40 (0.67–2.91) | 0.371 | |||
| Current smoker | 1.75 (0.84–3.62) | 0.133 | |||
| Drinking amount | None | 1 | 1 | ||
| ≤2 glass | 0.56 (0.33–0.94) | 0.027 | 0.67 (0.39–1.15) | 0.147 | |
| 3–6 glass | 0.61 (0.35–1.08) | 0.088 | 0.79 (0.42–1.49) | 0.466 | |
| ≥7 glass | 0.67 (0.27–1.70) | 0.398 | 0.63 (0.20–1.97) | 0.420 | |
| Exercise | No | 1 | |||
| Yes | 0.89 (0.58–1.86) | 0.890 | |||
| Diet | No | 1 | |||
| Yes | 1.28 (0.89–1.84) | 0.182 | |||
| Body mass index (kg/m2) | <22.9 (normal) | 1 | 1 | ||
| 23.0–24.9 (overweight) | 1.49 (0.96–2.32) | 0.076 | 1.22 (0.75–1.96) | 0.424 | |
| ≥25 (obesity) | 2.02 (1.41–2.91) | <0.001 | 1.51 (1.04–2.20) | 0.033 | |
| Underlying disease | None | 1 | 1 | ||
| Hypertension only | 2.70 (1.92–3.79) | <0.001 | 2.57 (1.67–3.98) | <0.001 | |
| Diabetes mellitus only | 7.35 (3.17–17.01) | <0.001 | 6.12 (2.58–14.51) | <0.001 | |
| Both | 9.31 (5.21–16.63) | <0.001 | 7.60 (3.99–14.47) | <0.001 | |
| Family history | No | 1 | |||
| Yes | 1.03 (0.73–1.47) | 0.859 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, J.; Kim, M. Awareness and Related Factors of Dyslipidemia in Menopausal Women in Korea. Healthcare 2022, 10, 112. https://doi.org/10.3390/healthcare10010112
Jeong J, Kim M. Awareness and Related Factors of Dyslipidemia in Menopausal Women in Korea. Healthcare. 2022; 10(1):112. https://doi.org/10.3390/healthcare10010112
Chicago/Turabian StyleJeong, Jeonghee, and Mijin Kim. 2022. "Awareness and Related Factors of Dyslipidemia in Menopausal Women in Korea" Healthcare 10, no. 1: 112. https://doi.org/10.3390/healthcare10010112
APA StyleJeong, J., & Kim, M. (2022). Awareness and Related Factors of Dyslipidemia in Menopausal Women in Korea. Healthcare, 10(1), 112. https://doi.org/10.3390/healthcare10010112






