Supervised Learning by Evolutionary Computation Tuning: An Application to Blockchain-Based Pharmaceutical Supply Chain Cost Model
Abstract
1. Introduction
2. Literature Review
2.1. PSC and Its Components for a Hospital
2.2. BT Drives PSC
2.3. Evolutionary Computation and Supervised Learning
2.3.1. ACO and FA
2.3.2. KNN, DT, NB, and SVM
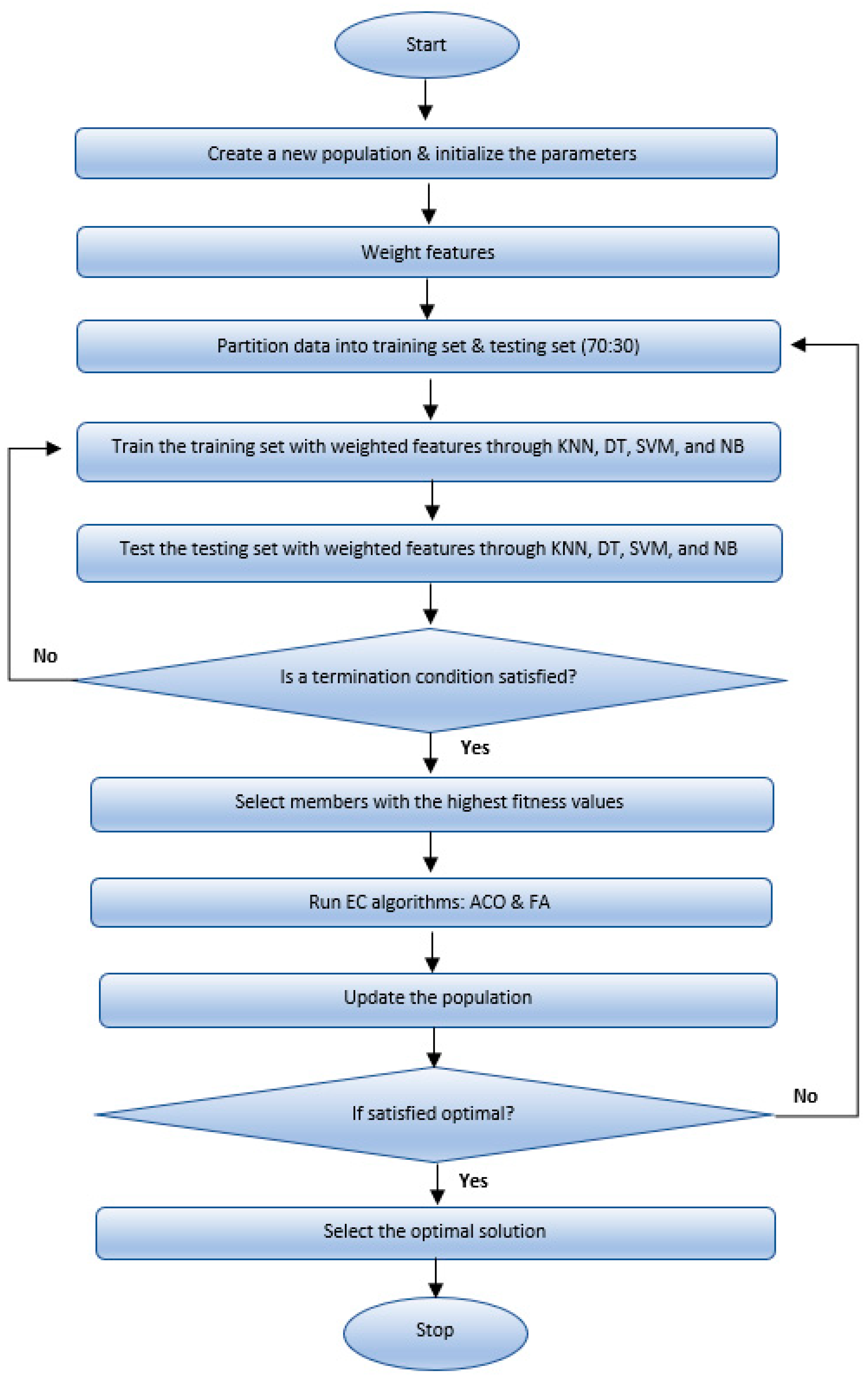
3. Methodology and Data Generation
4. Mathematical Cost Model for BT-Based PSC
- (1)
- Cp,Emergency_Purchases: The emergency purchases cost, at a higher price than the regular cost, can be made to satisfy the demand if there is not a sufficient amount of drugs in the inventory or if some medicines are expired (ep × eqp).
- (2)
- Cp,Shipping: The shipping cost of medications from the producer site to the hospital site is ((eqp + qp + sp) × tp). During shipping, it is necessary to keep some medications in certain conditions (such as temperature, light, or humidity). Therefore, the transportation cost varies with each medication type, although the distance between the producer and the hospital is constant.
- (3)
- Cp,Expired_Medication: The expired medication cost involves the safe disposal fees for different types of expired medication at government sites and the cost of shipping from the hospital to the safe government disposal sites (exptexp) × exqp). Expired medications incur governmental penalties and environmental forfeits due to their negative impact on the environment.
- (4)
- Cp,Holding: The holding cost is the inventory cost of the different types of medications at the hospital site (hp × ip).
- (5)
- Cp,Shortage: The Shortage cost is the cost that producers pay to the hospital due to the shortage in the supply of different types of medications (unsatisfied demand) and due to the outsourced medication cost satisfied by another pharmaceutical producer (πpop) × sp).
- (6)
- Cp,BT_transaction: The BT transaction cost consists of gasCost (gasUsed × gasPrice) and Storage cost (Gu × g × 365 + s × Cs) [24,30,31,32]. Gu × g is the BT transaction cost per day, and s × Cs is the storage cost per year. A secured cloud-based warehouse stores the actual data off-chain. An IBM Cloud website was used to calculate the storage cost [29].
- (7)
5. Results
5.1. FA Combined with Four SL
| FA_ KNN | Run | Feature Weighting | Performance Metrics | ||||||||||
| W_(Regular_Purchases) | W_(Emergency_Purchases) | W_(Shipping) | W_(Expired_Medication) | W_(Holding) | W_(Shortage) | W_(BT_Transaction) | W_(BT_Installation) | MSE | RMSE | MAE | R2 | ||
| 1 | 0.42761 | 0.70372 | 0.4019 | 0.77805 | 0.66441 | 0.54303 | 0.3898 | 0.75549 | 6,410,531.181 | 2531.9027 | 1911.4867 | 0.93669 | |
| 2 | 0.38097 | 0.40696 | 0.67108 | 0.07136 | 0.57776 | 0.96633 | 0.25649 | 0.71504 | 6,543,559.636 | 2558.0382 | 1844.5367 | 0.95009 | |
| 3 | 0.39918 | 0.22744 | 0.88195 | 1 | 0.45745 | 0.60981 | 0.28345 | 0.49667 | 7,109,497.639 | 2666.3641 | 1895.78 | 0.94165 | |
| 4 | 0.48472 | 0.70427 | 0.11742 | 0.56176 | 0.60325 | 0.55416 | 0.72756 | 0.70165 | 4,820,413.661 | 2195.544 | 1861.4267 | 0.94784 | |
| 5 | 0.44293 | 0.36279 | 1 | 1 | 0.27841 | 1 | 0.53327 | 0.66643 | 8,836,400.862 | 2972.6084 | 2380.51 | 0.95397 | |
| 6 | 0.57136 | 0.43084 | 0.086856 | 0.80261 | 0.38824 | 0.61953 | 0.7207 | 0.56945 | 3,341,730.069 | 1828.04 | 1563.43 | 0.96499 | |
| 7 | 0.29971 | 0.25515 | 0.25957 | 0.56899 | 0.69676 | 0.89902 | 0.37948 | 0.58159 | 7,298,087.42 | 2701.4973 | 2191.1033 | 0.93169 | |
| 8 | 0.51998 | 0.39227 | 0.11292 | 0.50207 | 0.30936 | 0.73901 | 0.25718 | 0.71075 | 4,636,038.367 | 2153.1462 | 1730.3067 | 0.95829 | |
| 9 | 0.38097 | 0.40696 | 0.67108 | 0.07136 | 0.57776 | 0.96633 | 0.25649 | 0.71504 | 6,543,559.636 | 2558.0382 | 1844.5367 | 0.95009 | |
| 10 | 0.39918 | 0.22744 | 0.88195 | 1 | 0.45745 | 0.60981 | 0.28345 | 0.49667 | 7,109,497.639 | 2666.3641 | 1895.78 | 0.94165 | |
| Average | 0.430661 | 0.411784 | 0.5084726 | 0.63562 | 0.501085 | 0.750703 | 0.408787 | 0.640878 | 6,264,931.611 | 2483.15432 | 1911.88968 | 0.947695 | |
| FA_ DT | Run | Feature Weighting | Performance Metrics | ||||||||||
| W_(Regular_Purchases) | W_(Emergency_Purchases) | W_(Shipping) | W_(Expired_Medication) | W_(Holding) | W_(Shortage) | W_(BT_Transaction) | W_(BT_Installation) | MSE | RMSE | MAE | R2 | ||
| 1 | 0.47321 | 1 | 0 | 0.55029 | 0.077932 | 0.98129 | 0 | 0.76499 | 20,931,129.39 | 4575.0551 | 3459.9621 | 0.78428 | |
| 2 | 0.68103 | 0 | 0.22354 | 0 | 0.86119 | 0.38003 | 0.88603 | 0.64452 | 35,006,777.18 | 5916.6525 | 4540.5366 | 0.71695 | |
| 3 | 0.15466 | 0.5686 | 0.54932 | 0.7612 | 0.58896 | 0.79381 | 0 | 0.2224 | 15,666,495.59 | 3958.0924 | 3054.3802 | 0.69542 | |
| 4 | 0.69663 | 0.44451 | 0.60297 | 0.45421 | 0.66456 | 0.24065 | 0.2454 | 0 | 19,723,753.67 | 4441.1433 | 3129.7053 | 0.82664 | |
| 5 | 0.019254 | 0.20955 | 0.56631 | 0.74343 | 0.6613 | 0 | 0.05882 | 0.92978 | 30,911,374.48 | 5559.7999 | 4279.7594 | 0.70113 | |
| 6 | 0.88511 | 0.14417 | 0.80373 | 0 | 0.8651 | 0.45487 | 0.46228 | 0.6855 | 16,236,754.9 | 4029.4857 | 3445.5285 | 0.8264 | |
| 7 | 0.47321 | 1 | 0 | 0.55029 | 0.077932 | 0.98129 | 0 | 0.76499 | 20,931,129.39 | 4575.0551 | 3459.9621 | 0.78428 | |
| 8 | 0.68103 | 0 | 0.22354 | 0 | 0.86119 | 0.38003 | 0.88603 | 0.64452 | 35,006,777.18 | 5916.6525 | 4540.5366 | 0.71695 | |
| 9 | 0.15466 | 0.5686 | 0.54932 | 0.7612 | 0.58896 | 0.79381 | 0 | 0.22248 | 15,666,495.59 | 3958.0924 | 3054.3802 | 0.69542 | |
| 10 | 0.69663 | 0.44451 | 0.60297 | 0.45421 | 0.66456 | 0.24065 | 0.2454 | 0 | 19,723,753.67 | 4441.1433 | 3129.7053 | 0.82664 | |
| Average | 0.4915424 | 0.437994 | 0.41217 | 0.427483 | 0.5911684 | 0.524643 | 0.278396 | 0.487918 | 22,980,444.11 | 4737.11722 | 3609.44563 | 0.757411 | |
| FA_ SVM | Run | Feature Weighting | Performance Metrics | ||||||||||
| W_(Regular_Purchases) | W_(Emergency_Purchases) | W_(Shipping) | W_(Expired_Medication) | W_(Holding) | W_(Shortage) | W_(BT_Transaction) | W_(BT_Installation) | MSE | RMSE | MAE | R2 | ||
| 1 | 0.23175 | 0.2259 | 0.53019 | 0.00011658 | 0.98963 | 0.99971 | 0.37348 | 0.32717 | 173,343.7829 | 416.3457 | 333.2585 | 0.99958 | |
| 2 | 0.49827 | 0.1213 | 0.044341 | 0.37469 | 0.078956 | 0.076338 | 0.84056 | 0.025916 | 123,519.554 | 351.4535 | 295.5338 | 0.99944 | |
| 3 | 0.23175 | 0.2259 | 0.53019 | 0.00011658 | 0.98963 | 0.99971 | 0.37348 | 0.32717 | 173,343.7829 | 416.3457 | 333.2585 | 0.99958 | |
| 4 | 0.49827 | 0.1213 | 0.044341 | 0.37469 | 0.078956 | 0.076338 | 0.84056 | 0.025916 | 123,519.554 | 351.4535 | 295.5338 | 0.99944 | |
| 5 | 0.11145 | 0.18245 | 0.80071 | 0.91571 | 0.3337 | 0.27808 | 0.999 | 0.1206 | 187,904.5992 | 433.4796 | 345.0264 | 0.99973 | |
| 6 | 0.062505 | 0.13831 | 0.17654 | 0.83871 | 0.55852 | 0.43634 | 0.21079 | 0.072986 | 133,984.4159 | 366.0388 | 304.2886 | 1 | |
| 7 | 0.12535 | 0.10758 | 0.88876 | 0.99971 | 0.28039 | 0.38197 | 0.99797 | 0.11452 | 217,426.4673 | 466.2901 | 349.1649 | 0.99967 | |
| 8 | 0.069619 | 0.11732 | 0.22129 | 0.89167 | 0.5806 | 0.5368 | 0.59439 | 0.075245 | 170,350.8234 | 412.7358 | 348.6053 | 0.9999 | |
| 9 | 0.070616 | 0.15011 | 0.19064 | 0.95425 | 0.4204 | 0.92513 | 0.22981 | 0.082785 | 119,067.7801 | 345.062 | 276.8873 | 0.99995 | |
| 10 | 0.038819 | 0.37321 | 0.098169 | 0.3057 | 0.17506 | 0.19189 | 0.30862 | 0.044591 | 167,675.474 | 409.482 | 356.8005 | 0.99984 | |
| Average | 0.1938399 | 0.176338 | 0.3525171 | 0.565536316 | 0.4485842 | 0.4902306 | 0.576866 | 0.1216899 | 159,013.6234 | 396.86867 | 323.83576 | 0.999713 | |
| FA_ NB | Run | Feature Weighting | Performance Metrics | ||||||||||
| W_(Regular_Purchases) | W_(Emergency_Purchases) | W_(Shipping) | W_(Expired_Medication) | W_(Holding) | W_(Shortage) | W_(BT_Transaction) | W_(BT_Installation) | MSE | RMSE | MAE | R2 | ||
| 1 | 0.032531 | 0.041745 | 0.08032 | 0.9808 | 0.10975 | 0.18195 | 1 | 0.031338 | 0.02788 | 0.16697 | 0.1257 | 1 | |
| 2 | 0.010457 | 0.015939 | 0.033751 | 0.99143 | 0.056218 | 0.05816 | 0.96678 | 0.011013 | 0.016316 | 0.12773 | 0.10697 | 1 | |
| 3 | 0.060931 | 0.084856 | 0.18278 | 0.91442 | 0.59413 | 0.3198 | 0.30078 | 0.063357 | 0.01369 | 0.117 | 0.096242 | 1 | |
| 4 | 0.060931 | 0.084856 | 0.18278 | 0.91442 | 0.59413 | 0.3198 | 0.30078 | 0.063357 | 0.01369 | 0.117 | 0.096242 | 1 | |
| 5 | 0.029986 | 0.052286 | 0.086725 | 0.99994 | 0.14185 | 0.24168 | 0.31756 | 0.033475 | 0.019494 | 0.13962 | 0.11491 | 1 | |
| 6 | 0.015173 | 0.017665 | 0.038483 | 0.99992 | 0.72279 | 0.077546 | 0.22372 | 0.014434 | 0.035156 | 0.1875 | 0.13605 | 1 | |
| 7 | 0.032531 | 0.041745 | 0.08032 | 0.9808 | 0.10975 | 0.18195 | 1 | 0.031338 | 0.02788 | 0.16697 | 0.1257 | 1 | |
| 8 | 0.010457 | 0.015939 | 0.033751 | 0.99143 | 0.056218 | 0.05816 | 0.96678 | 0.011013 | 0.016316 | 0.12773 | 0.10697 | 1 | |
| 9 | 0.060931 | 0.084856 | 0.18278 | 0.91442 | 0.59413 | 0.3198 | 0.30078 | 0.063357 | 0.01369 | 0.117 | 0.096242 | 1 | |
| 10 | 0.032531 | 0.041745 | 0.08032 | 0.9808 | 0.10975 | 0.18195 | 1 | 0.031338 | 0.02788 | 0.16697 | 0.1257 | 1 | |
| Average | 0.0346459 | 0.0481632 | 0.098201 | 0.966838 | 0.3088716 | 0.1940796 | 0.637718 | 0.035402 | 0.0211992 | 0.143449 | 0.1130726 | 1 | |
| Performance Metrics | ||||
|---|---|---|---|---|
| Methods | Ave_MSE | Ave_RMSE | Ave_MAE | Ave_R2 |
| FA_KNN | 6,264,931.611 | 2483.15432 | 1911.88968 | 0.930856 |
| FA_DT | 22,980,444.11 | 5916.6525 | 3609.44563 | 0.757411 |
| FA_SVM | 159,013.6234 | 396.86867 | 323.83576 | 0.999713 |
| FA_NB | 0.0211992 | 0.143449 | 0.1130726 | 1 |
| Feature Weighting | ||
|---|---|---|
| Methods | Max_Ave_Weighting | Min_ Ave_Weighting |
| FA_KNN | W_(BT_Installation) = 0.84988 | W_(Expired_Medication) = 0.34659 |
| FA_DT | W_(Holding) = 0.5911684 | W_(BT_Transaction) = 0.278396 |
| FA_SVM | W_(BT_Transaction) = 0.576866 | W_(BT_Installation) = 0.1216899 |
| FA_NB | W_(Expired_Medication) = 0.966838 | W_(Regular_Purchases) = 0.0346459 |
5.2. ACO Combined with Four SL Algorithms
| ACO_KNN | Run | Feature Weighting | Performance Metrics | ||||||||||
| W_(Regular_Purchases) | W_(Emergency_Purchases) | W_(Shipping) | W_(Expired_Medication) | W_(Holding) | W_(Shortage) | W_(BT_Transaction) | W_(BT_Installation) | MSE | RMSE | MAE | R2 | ||
| 1 | 0.35695 | 0.92549 | 0.89039 | 1 | 0.009856 | 0.18912 | 0.47227 | 0.99903 | 5,543,172.364 | 2354.3943 | 1949.4633 | 0.92596 | |
| 2 | 1 | 0.76434 | 0.43676 | 0 | 0.88697 | 1 | 0.34671 | 1 | 4,695,227.88 | 2166.8475 | 1864.3933 | 0.95763 | |
| 3 | 0.92009 | 0.62512 | 0.8734 | 1 | 0.76675 | 0 | 0.86776 | 0.84005 | 4,692,998.943 | 2166.3331 | 1818.2033 | 0.93246 | |
| 4 | 0.70324 | 0.64935 | 0.47864 | 0.021711 | 0.59772 | 0.26598 | 0.36632 | 0.45778 | 6,719,708.626 | 2592.2401 | 2065.3833 | 0.89936 | |
| 5 | 1 | 0.66795 | 0 | 0.15666 | 0.72265 | 1 | 0.55566 | 0.50375 | 6,928,149.833 | 2632.1379 | 2027.5067 | 0.94752 | |
| 6 | 0.48851 | 0.97333 | 0.65892 | 0 | 0.30371 | 1 | 0.41044 | 1 | 6,221,307.472 | 2494.2549 | 2142.3833 | 0.92888 | |
| 7 | 0.45446 | 0.51932 | 0.49337 | 0.38196 | 0.93485 | 1 | 0.34229 | 0.98086 | 4,565,317.918 | 2136.6605 | 1844.1267 | 0.94594 | |
| 8 | 0.36326 | 0.34374 | 1 | 0.47294 | 0.91225 | 0.4744 | 0.20598 | 0.99651 | 4,394,372.317 | 2096.2758 | 1794.3933 | 0.92742 | |
| 9 | 0.52039 | 0.70382 | 0.077738 | 0 | 0.69597 | 0 | 0.92397 | 1 | 10,706,939.15 | 3272.146 | 2655.27 | 0.90856 | |
| 10 | 0.40842 | 0.36388 | 0.21883 | 0.43267 | 0.95833 | 1 | 0.61236 | 0.72077 | 5,833,434.956 | 2415.2505 | 2088.6967 | 0.93483 | |
| Average | 0.621532 | 0.653634 | 0.5128048 | 0.3465941 | 0.6789056 | 0.59295 | 0.510376 | 0.849875 | 6,030,062.946 | 2432.65406 | 2024.98199 | 0.930856 | |
| ACO_DT | Run | Feature Weighting | Performance Metrics | ||||||||||
| W_(Regular_Purchases) | W_(Emergency_Purchases) | W_(Shipping) | W_(Expired_Medication) | W_(Holding) | W_(Shortage) | W_(BT_Transaction) | W_(BT_Installation) | MSE | RMSE | MAE | R2 | ||
| 1 | 0.36831 | 0.65313 | 0 | 0 | 0 | 1 | 0.48975 | 0 | 27,725,280.24 | 5265.4801 | 3918.345 | 0.8088 | |
| 2 | 0.78548 | 1 | 0 | 0.35183 | 0 | 0 | 0.96679 | 0.78077 | 17,268,337.62 | 4155.5189 | 3358.6605 | 0.73903 | |
| 3 | 0.39139 | 0.30496 | 0 | 1 | 0 | 0 | 0 | 0.078329 | 20,862,939.19 | 4567.5967 | 3543.8508 | 0.78735 | |
| 4 | 1 | 0.70817 | 0 | 1 | 0.61945 | 0.15374 | 0.36463 | 0.38276 | 14,114,845.23 | 3756.9729 | 3134.379 | 0.79848 | |
| 5 | 0.78077 | 0 | 0 | 0.39765 | 0 | 0 | 0 | 1 | 22,127,369.33 | 4703.9738 | 3421.1334 | 0.77706 | |
| 6 | 0.11978 | 0.46586 | 1 | 0.43738 | 0 | 1 | 0.86613 | 0 | 15,853,729.5 | 3981.6742 | 2765.302 | 0.83271 | |
| 7 | 0.41597 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 13,566,853.1 | 3683.3209 | 2900.3703 | 0.82056 | |
| 8 | 0.72963 | 0.5107 | 0 | 0 | 0.44327 | 0 | 0.58999 | 1 | 18,853,360.55 | 4342.0457 | 3218.8045 | 0.80982 | |
| 9 | 0.35453 | 0 | 0.50304 | 0.26006 | 0.29699 | 0 | 0 | 0.10223 | 19,129,278.4 | 4373.7031 | 3173.7969 | 0.83869 | |
| 10 | 0.35628 | 0.37771 | 0 | 0.89254 | 0 | 0.44445 | 0 | 0.27212 | 23,472,850.57 | 4844.8788 | 3620.1248 | 0.8251 | |
| Average | 0.530214 | 0.502053 | 0.150304 | 0.433946 | 0.135971 | 0.359819 | 0.327729 | 0.4616209 | 19297484.37 | 4367.51651 | 3305.47672 | 0.80376 | |
| Run | Feature Weighting | Performance Metrics | |||||||||||
| W_(Regular_Purchases) | W_(Emergency_Purchases) | W_(Shipping) | W_(Expired_Medication) | W_(Holding) | W_(Shortage) | W_(BT_Transaction) | W_(BT_Installation) | MSE | RMSE | MAE | R2 | ||
| ACO_SVM | 1 | 0.13205 | 0.17919 | 0.47213 | 0.99797 | 0.41098 | 0.53424 | 0.94092 | 0.16085 | 214,988.4336 | 463.6685 | 372.7033 | 0.99976 |
| 2 | 0.98237 | 0.26347 | 0.97017 | 0.0054287 | 0.65009 | 0.99563 | 0.69419 | 0.52966 | 118,716.9279 | 344.5532 | 291.8931 | 0.99858 | |
| 3 | 0.36341 | 0.07529 | 0.44152 | 0.94205 | 1 | 0.13531 | 0.35334 | 0.84212 | 85,394.6138 | 292.2236 | 239.0761 | 0.99908 | |
| 4 | 0.31839 | 0.21878 | 0.80193 | 0 | 0.88418 | 0.86379 | 0.34368 | 0.59425 | 178,499.0214 | 422.4914 | 337.9536 | 0.99957 | |
| 5 | 0.22478 | 0.99994 | 0.90923 | 0.99996 | 0.68076 | 0.62322 | 0.28197 | 0.23503 | 79,662.2247 | 282.245 | 220.6187 | 0.99944 | |
| 6 | 0.1891 | 0.181 | 0.81952 | 1 | 1 | 0.62985 | 0.99913 | 0.17333 | 282,360.1537 | 531.3757 | 415.7638 | 0.99926 | |
| 7 | 0.15083 | 0.32986 | 0.40481 | 0.99984 | 0.96917 | 0.93384 | 0.98662 | 0.21624 | 170,985.299 | 413.5037 | 343.692 | 0.9999 | |
| 8 | 0.97605 | 0.20016 | 0.47514 | 0.9965 | 0.98931 | 0.85258 | 0.99817 | 0.18793 | 168,623.3192 | 410.6377 | 350.2368 | 0.99905 | |
| 9 | 0.31839 | 0.21878 | 0.80193 | 0 | 0.88418 | 0.86379 | 0.34368 | 0.59425 | 178,499.0214 | 422.4914 | 337.9536 | 0.99957 | |
| 10 | 0.22478 | 0.99994 | 0.90923 | 0.99996 | 0.68076 | 0.62322 | 0.28197 | 0.23503 | 79,662.2247 | 282.245 | 220.6187 | 0.99944 | |
| Average | 0.388015 | 0.366641 | 0.700561 | 0.69417087 | 0.814943 | 0.705547 | 0.622367 | 0.376869 | 155,739.1239 | 386.54352 | 313.05097 | 0.999365 | |
| Run | Feature Weighting | Performance Metrics | |||||||||||
| ACO_NB | W_(Regular_Purchases) | W_(Emergency_Purchases) | W_(Shipping) | W_(Expired_Medication) | W_(Holding) | W_(Shortage) | W_(BT_Transaction) | W_(BT_Installation) | MSE | RMSE | MAE | R2 | |
| 1 | 0.066266 | 0.083497 | 0.16188 | 1 | 0.22171 | 0.36769 | 0.99974 | 0.064689 | 0.028975 | 0.17022 | 0.12833 | 1 | |
| 2 | 0.051676 | 0.076568 | 0.15739 | 1 | 0.39803 | 0.25806 | 1 | 0.055018 | 0.016852 | 0.12981 | 0.10561 | 1 | |
| 3 | 0.036712 | 0.055901 | 0.083755 | 0.99983 | 1 | 0.18925 | 0.19181 | 0.041779 | 0.01459 | 0.12079 | 0.092924 | 1 | |
| 4 | 0.052031 | 0.0655 | 0.11217 | 0.99977 | 0.32118 | 0.20282 | 0.99953 | 0.047636 | 0.020784 | 0.14417 | 0.12146 | 1 | |
| 5 | 0.066266 | 0.083497 | 0.16188 | 1 | 0.22171 | 0.36769 | 0.99974 | 0.064689 | 0.028975 | 0.17022 | 0.12833 | 1 | |
| 6 | 0.051676 | 0.076568 | 0.15739 | 1 | 0.39803 | 0.25806 | 1 | 0.055018 | 0.016852 | 0.12981 | 0.10561 | 1 | |
| 7 | 0.036712 | 0.055901 | 0.083755 | 0.99983 | 1 | 0.18925 | 0.19181 | 0.041779 | 0.01459 | 0.12079 | 0.092924 | 1 | |
| 8 | 0.052031 | 0.0655 | 0.11217 | 0.99977 | 0.32118 | 0.20282 | 0.99953 | 0.047636 | 0.020784 | 0.14417 | 0.12146 | 1 | |
| 9 | 0.05725 | 0.07226 | 0.1489 | 1 | 1 | 0.44111 | 0.52877 | 0.058602 | 0.032984 | 0.18161 | 0.1356 | 1 | |
| 10 | 0.045911 | 0.080262 | 0.13201 | 0.99984 | 0.23087 | 0.33649 | 1 | 0.053764 | 0.012642 | 0.11244 | 0.098423 | 1 | |
| Average | 0.0516531 | 0.0715454 | 0.13113 | 0.999904 | 0.511271 | 0.281324 | 0.791093 | 0.053061 | 0.0208028 | 0.142403 | 0.1130671 | 1 | |
| Feature Weighting | ||||
|---|---|---|---|---|
| Methods | Ave_MSE | Ave_RMSE | Ave_ MAE | Ave_R2 |
| ACO_KNN | 6,030,062.946 | 2432.65406 | 2024.98199 | 0.930856 |
| ACO_DT | 19,297,484.37 | 4367.51651 | 3305.47672 | 0.80376 |
| ACO_SVM | 155,739.1239 | 386.54352 | 313.05097 | 0.999365 |
| ACO_NB | 0.0208028 | 0.142403 | 0.1130671 | 1 |
| Feature Weighting | ||
|---|---|---|
| Methods | Max_Ave_Weighting | Min_Ave_Weighting |
| ACO_KNN | W_(BT_Installation) = 0.849875 | W_(Expired_Medication) = 0.3465941 |
| ACO_DT | W_(Regular_Purchases) = 0.530214 | W_(Holding) = 0.135971 |
| ACO_SVM | W_(Holding) = 0.814943 | W_(Emergency_Purchases) = 0.366641 |
| ACO_NB | W_(Expired_Medication) = 0.999904 | W_(Regular_Purchases) = 0.0516531 |
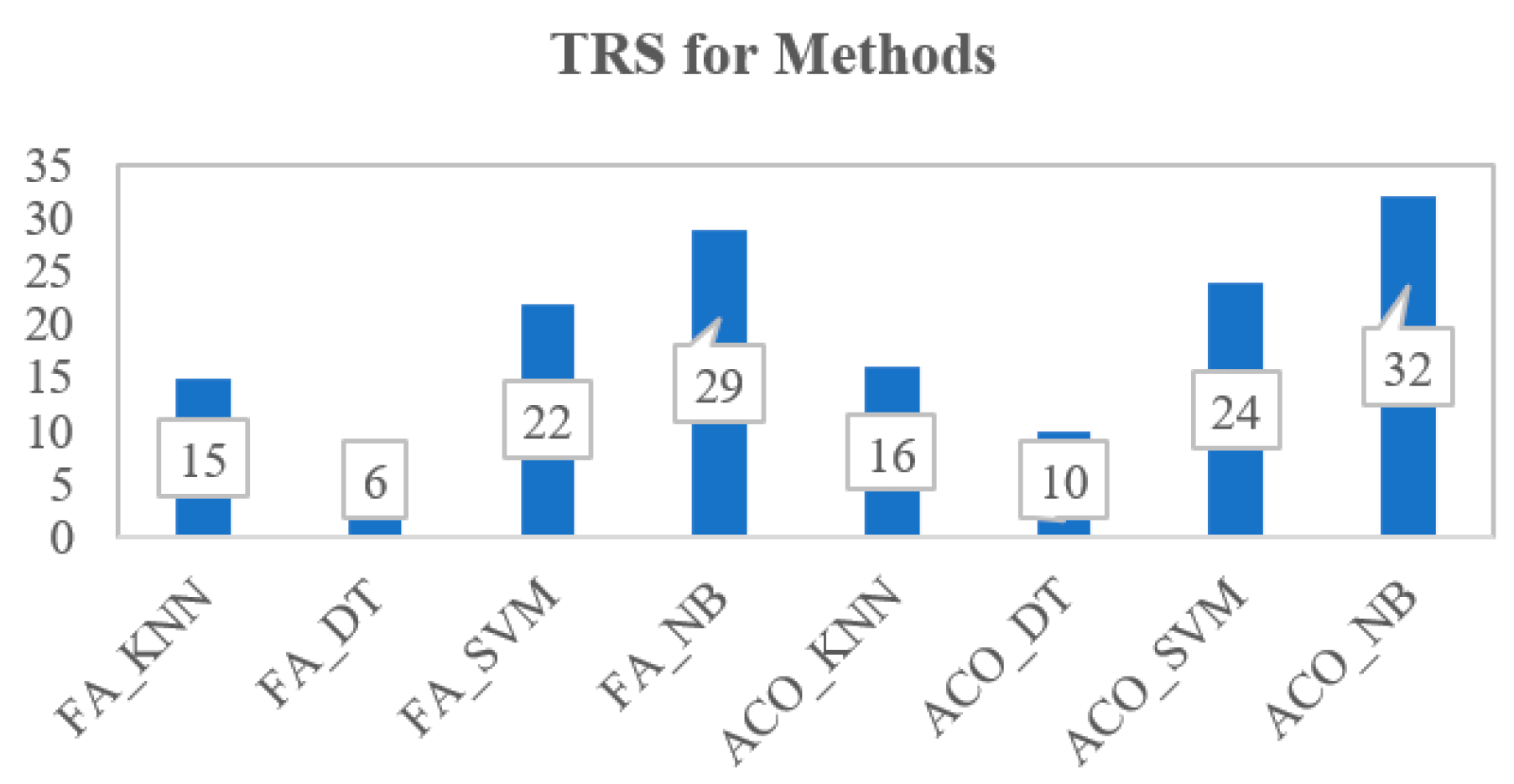
5.3. Determining Reliable Algorithms for BT-Based PSC Cost Model
| Performance Metrics | |||||||
|---|---|---|---|---|---|---|---|
| Methods | Ave_MSE | Ave_RMSE | Ave_MAE | Ave_R2 | TRS | Rank | |
| FA_KNN | 6,264,931.611 | 2483.15432 | 1911.88968 | 0.930856 | |||
| FA_DT | 22,980,444.11 | 5916.6525 | 3609.44563 | 0.757411 | |||
| FA_SVM | 159,013.6234 | 396.86867 | 323.83576 | 0.999713 | |||
| FA_NB | 0.0211992 | 0.143449 | 0.1130726 | 1 | |||
| ACO_KNN | 6,030,062.946 | 2432.65406 | 2024.98199 | 0.930856 | |||
| ACO_DT | 19,297,484.37 | 4367.51651 | 3305.47672 | 0.80376 | |||
| ACO_SVM | 155,739.1239 | 386.54352 | 313.05097 | 0.999365 | |||
| ACO_NB | 0.0208028 | 0.142403 | 0.1130671 | 1 | |||
| Ranking Score | FA_KNN | 3 | 3 | 4 | 5 | 15 | 6 |
| FA_DT | 1 | 1 | 1 | 3 | 6 | 8 | |
| FA_SVM | 5 | 5 | 5 | 7 | 22 | 4 | |
| FA_NB | 7 | 7 | 7 | 8 | 29 | 2 | |
| ACO_KNN | 4 | 4 | 3 | 5 | 16 | 5 | |
| ACO_DT | 2 | 2 | 2 | 4 | 10 | 7 | |
| ACO_SVM | 6 | 6 | 6 | 6 | 24 | 3 | |
| ACO_NB | 8 | 8 | 8 | 8 | 32 | 1 | |
| Methods | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ave_FW | FA_ KNN | FA_DT | FA_ SVM | FA_NB | ACO_ KNN | ACO_ DT | ACO_ SVM | ACO_ NB | TRS | Rank | |
| W_(Regular_Purchases) | 0.430661 | 0.4915424 | 0.1938399 | 0.0346459 | 0.621532 | 0.530214 | 0.388015 | 0.0516531 | |||
| W_(Emergency_Purchases) | 0.411784 | 0.437994 | 0.176338 | 0.0481632 | 0.653634 | 0.502053 | 0.366641 | 0.0715454 | |||
| W_(Shipping) | 0.5084726 | 0.41217 | 0.3525171 | 0.098201 | 0.5128048 | 0.150304 | 0.700561 | 0.13113 | |||
| W_(Expired_Medication) | 0.63562 | 0.427483 | 0.56553631 | 0.966838 | 0.3465941 | 0.433946 | 0.69417087 | 0.999904 | |||
| W_(Holding) | 0.501085 | 0.5911684 | 0.4485842 | 0.3088716 | 0.6789056 | 0.135971 | 0.814943 | 0.511271 | |||
| W_(Shortage) | 0.750703 | 0.524643 | 0.4902306 | 0.1940796 | 0.59295 | 0.359819 | 0.705547 | 0.281324 | |||
| W_(BT_Transaction) | 0.408787 | 0.278396 | 0.576866 | 0.637718 | 0.510376 | 0.327729 | 0.622367 | 0.791093 | |||
| W_(BT_Installation) | 0.640878 | 0.487918 | 0.1216899 | 0.035402 | 0.849875 | 0.4616209 | 0.376869 | 0.053061 | |||
| Ranking Score | W_(Regular_Purchases) | 3 | 6 | 3 | 1 | 5 | 8 | 3 | 1 | 30 | 5 |
| W_(Emergency_Purchases) | 2 | 4 | 2 | 3 | 6 | 7 | 1 | 3 | 28 | 6 | |
| W_(Shipping) | 5 | 2 | 4 | 4 | 3 | 2 | 6 | 4 | 30 | 5 | |
| W_(Expired_Medication) | 6 | 3 | 7 | 8 | 1 | 5 | 5 | 8 | 43 | 3 | |
| W_(Holding) | 4 | 8 | 5 | 6 | 7 | 1 | 8 | 6 | 45 | 2 | |
| W_(Shortage) | 8 | 7 | 6 | 5 | 4 | 4 | 7 | 5 | 46 | 1 | |
| W_(BT_Transaction) | 1 | 1 | 8 | 7 | 2 | 3 | 4 | 7 | 33 | 4 | |
| W_(BT_Installation) | 7 | 5 | 1 | 2 | 8 | 6 | 2 | 2 | 33 | 4 | |
6. Discussion
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Ahmadi, A.; Mousazadeh, M.; Torabi, S.A.; Pishvaee, M.S. OR Applications in Pharmaceutical Supply Chain Management. Oper. Res. Appl. Health Care Manag. 2017, 262, 461–491. [Google Scholar]
- Chircu, A.; Sultanow, E.; Saraswat, S.P. Healthcare RFID In Germany: An Integrated Pharmaceutical Supply Chain Perspective. J. Appl. Bus. Res. 2014, 30, 737–752. [Google Scholar] [CrossRef]
- Haq, I.; Esuka, O. Blockchain Technology in Pharmaceutical Industry to Prevent Counterfeit Drugs. Int. J. Comput. Appl. 2018, 180, 8–12. [Google Scholar] [CrossRef]
- Boulos, M.N.K.; Wilson, J.T.; Clauson, K.A. Geospatial blockchain: Promises, challenges, and scenarios in health and healthcare. Int. J. Health Geogr. 2018, 17, 25. [Google Scholar] [CrossRef] [PubMed]
- Salehi, V.; Salehi, R.; Mirzayi, M.; Akhavizadegan, F. Performance optimization of pharmaceutical supply chain by a unique resilience engineering and fuzzy mathematical framework. Hum. Factors Ergon. Manuf. Serv. Ind. 2020, 30, 336–348. [Google Scholar] [CrossRef]
- Uthayakumar, R.; Priyan, S. Pharmaceutical supply chain and inventory management strategies: Optimization for a pharmaceutical company and a hospital. Oper. Res. Health Care 2013, 2, 52–64. [Google Scholar] [CrossRef]
- Goodarzian, F.; Hosseini-Nasab, H.; Muñuzuri, J.; Fakhrzad, M.-B. A multi-objective pharmaceutical supply chain network based on a robust fuzzy model: A comparison of meta-heuristics. Appl. Soft Comput. 2020, 92, 106331. [Google Scholar] [CrossRef]
- Bamakan, S.M.H.; Moghaddam, S.G.; Manshadi, S.D. Blockchain-enabled pharmaceutical cold chain: Applications, key challenges, and future trends. J. Clean. Prod. 2021, 302, 127021. [Google Scholar] [CrossRef]
- Zahiri, B.; Jula, P.; Tavakkoli-Moghaddam, R. Design of a pharmaceutical supply chain network under uncertainty considering perishability and substitutability of products. Inf. Sci. 2018, 423, 257–283. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R.; Rab, S. Blockchain technology applications in healthcare: An overview. Int. J. Intell. Netw. 2021, 2, 130–139. [Google Scholar] [CrossRef]
- Badhotiya, G.K.; Sharma, V.P.; Prakash, S.; Kalluri, V.; Singh, R. Investigation and assessment of blockchain technology adoption in the pharmaceutical supply chain. Mater. Today Proc. 2021, 46, 10776–10780. [Google Scholar] [CrossRef]
- Zhang, W.; Gu, X.; Tang, L.; Yin, Y.; Liu, D.; Zhang, Y. Application of machine learning, deep learning and optimization algorithms in geoengineering and geoscience: Comprehensive review and future challenge. Gondwana Res. 2022, 109, 1–17. [Google Scholar] [CrossRef]
- Glover, F.; Sörensen, K. Metaheuristics. Scholarpedia 2015, 10, 6532. [Google Scholar] [CrossRef]
- Yusta, S.C. Different metaheuristic strategies to solve the feature selection problem. Pattern Recognit. Lett. 2009, 30, 525–534. [Google Scholar] [CrossRef]
- Garg, P. A Comparison between Memetic algorithm and Genetic algorithm forthe cryptanalysis of Simplified Data Encryption Standard algorithm. Int. J. Netw. Secur. Its Appl. 2009, 1, 34–42. [Google Scholar]
- Abd-Alsabour, N. Investigating the effect of fixing the subset length on the performance of ant colony optimization for feature selection for supervised learning. Comput. Electr. Eng. 2015, 45, 1–9. [Google Scholar] [CrossRef]
- Rojas-Morales, N.; Riff, M.-C.; Neveu, B. Learning and focusing strategies to improve ACO that solves CSP. Eng. Appl. Artif. Intell. 2021, 105, 104408. [Google Scholar] [CrossRef]
- Nourelfath, M.; Nahas, N.; Montreuil, B. Coupling ant colony optimization and the extended great deluge algorithm for the discrete facility layout problem. Eng. Optim. 2007, 39, 953–968. [Google Scholar] [CrossRef]
- Mashhour, E.M.; Houby, E.M.; TawfikWassif, K.; IbrahimSalah, A. A Novel Classifier based on Firefly Algorithm. J. King Saud Univ.—Comput. Inf. Sci. 2020, 32, 1173–1181. [Google Scholar] [CrossRef]
- Almomany, A.; Ayyad, W.R.; Jarrah, A. Optimized implementation of an improved KNN classification algorithm using Intel FPGA platform: Covid-19 case study. J. King Saud Univ.—Comput. Inf. Sci. 2022, 34, 3815–3827. [Google Scholar] [CrossRef]
- Kushwah, J.S.; Kumar, A.; Patel, S.; Soni, R.; Gawande, A.; Gupta, S. Comparative study of regressor and classifier with decision tree using modern tools. Mater. Today Proc. 2022, 56, 3571–3576. [Google Scholar] [CrossRef]
- Ren, Q.; Zhang, H.; Zhang, D.; Zhao, X.; Yan, L.; Rui, J.; Zeng, F.; Zhu, X. A framework of active learning and semi-supervised learning for lithology identification based on improved naive Bayes. Expert Syst. Appl. 2022, 202, 117278. [Google Scholar] [CrossRef]
- Zhang, H.; Shi, Y.; Yang, X.; Zhou, R. A firefly algorithm modified support vector machine for the credit risk assessment of supply chain finance. Res. Int. Bus. Financ. 2021, 58, 101482. [Google Scholar] [CrossRef]
- Havaeji, H.; Dao, T.-M.; Wong, T. The Generated Raw Data to Evaluate the Blockchain-Based Pharmaceutical Supply Chain Cost Model. 1 November 2022. Available online: https://data.mendeley.com/datasets/jxv5jrydnc (accessed on 1 November 2022).
- Al-Zoubi, A.M.; Hassonah, M.A.; Heidari, A.A.; Faris, H.; Mafarja, M.; Aljarah, I. Evolutionary competitive swarm exploring optimal support vector machines and feature weighting. Methodol. Appl. 2021, 25, 3335–3352. [Google Scholar] [CrossRef]
- Weraikat, D.; Zanjani, M.K.; Lehoux, N. Improving sustainability in a two-level pharmaceutical supply chain through Vendor-Managed Inventory system. Oper. Res. Health Care 2019, 21, 44–55. [Google Scholar] [CrossRef]
- Franco, C.; Alfonso-Lizarazo, E. Optimization under uncertainty of the pharmaceutical supply chain in hospitals. Comput. Chem. Eng. 2020, 135, 106689. [Google Scholar] [CrossRef]
- Havaeji, H.; Dao, T.-M.; Wong, T. Cost Optimization of Blockchain Technology-enabled Supply Chain System using Evolutionary Computation Approaches: A Healthcare Case Study. World Wide J. Multidiscip. Res. Dev. 2022, 8, 27–42. [Google Scholar]
- IBM. IBM Cloud. 2022. Available online: https://cloud.ibm.com/objectstorage/create#pricing (accessed on 1 February 2022).
- Longo, F.; Nicoletti, L.; Padovano, A.; d’Atri, G.; Forte, M. Blockchain-enabled supply chain: An experimental study. Comput. Ind. Eng. 2019, 136, 57–69. [Google Scholar] [CrossRef]
- Jabbar, A.; Dani, S. Investigating the link between transaction and computational costs in a blockchain environment. Int. J. Prod. Res. 2020, 58, 3423–3436. [Google Scholar] [CrossRef]
- Wood, G. Ethereum: A Secure Decentralised Generalised Transaction Ledger. Ethereum Proj. Yellow Pap. 2014, 151, 1–32. [Google Scholar]
- Gopalakrishnan, P.K.; Hall, J.; Behdad, S. Cost analysis and optimization of Blockchain-based solid waste management traceability system. Waste Manag. 2021, 120, 594–607. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ni, W.; Zha, X.; Yu, G.; Liu, R.P.; Georgalas, N.; Reeves, A. Capacity analysis of public blockchain. Comput. Commun. 2021, 177, 112–124. [Google Scholar] [CrossRef]
- ETH Gas Station. 2022. Available online: https://ethgasstation.info/ (accessed on 1 February 2022).
- Takyar, A. How to Determine the Cost of Blockchain Implementation? 2021. Available online: https://www.leewayhertz.com/cost-of-blockchain-implementation/ (accessed on 1 November 2022).

| Parameters | Explanation | Constraints |
|---|---|---|
| M | Number of medication types in the PSC variables (p = 1, 2, 3, …, M) | 45 |
| U | The number of Blockchain users | 4 |
| Cs | Cost of storage per year (USD/TB) for public outbound bandwidth service [29] | USD 20 × 12 = 2400 USD/yr |
| Gu | The amount of ether gasUsed per day | USD 1.31 ≤ Gu × g ≤ USD 3.94 |
| g | Number of gWei to be paid for gasUsed per day | |
| ip | Inventory level of medication type p | 25 ≤ ip ≤ 140 (integer) |
| qp | Order quantity for the pth medicine product per year | 10 ≤ qp ≤ 100 (integer) |
| s | The storage size to store the data | 2 TB/yr ≤ s ≤ 5 TB/yr |
| eqp | Number of lots of medicine types p purchased in case of emergency | 1 ≤ eqp ≤ 40 (integer) |
| exqp | Quantity of expired medication type p sent to the government disposal site | 1 ≤ exqp ≤ 25 (integer) |
| sp | Shortage quantity of medication type p that is needed to be outsourced | 1 ≤ sp ≤ 40 (integer) |
| rp | Regular cost of medicine type p (USD) | 15 ≤ rp ≤ 250 rp ≤ ep |
| ep | Emergency cost of medicine type p (USD) | 20 ≤ ep ≤ 300 |
| tp | Shipping cost of medication type p shipped to the hospital (USD) | 5 ≤ tp ≤ 35 |
| exp | Costs obligated by governments for each unit of medication type p disposed at their sites (USD) | 5 ≤ exp ≤ 10 |
| texp | Shipping cost of expired medication type p sent to the government disposal site (USD) | 1 ≤ texp ≤ 15 |
| hp | Holding cost of medication type p at the hospital site (USD) | 20 ≤ hp ≤ 30 |
| πp | Penalty that the producer pays to the hospital for each unit of shortage in the supply of medication type p (USD) | 10 ≤ πp ≤ 20 |
| op | Cost of outsourced medication type p that the producer could not satisfy (USD) | 12 ≤ op ≤ 18 |
| cfixed | The initial fixed cost per year | 580 ≤ cfixed ≤ 680 |
| conboarding | The onboarding cost | USD 20 ≤ conboarding ≤ USD 28 |
| cmc | The unit maintenance cost; cmc + cmo is 15%–25% of the project value | USD 15 ≤ cmc + cmo ≤ USD 25 |
| cmo | The unit monitoring cost; cmc + cmo is 15%–25% of the project value |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Havaeji, H.; Dao, T.-M.; Wong, T. Supervised Learning by Evolutionary Computation Tuning: An Application to Blockchain-Based Pharmaceutical Supply Chain Cost Model. Mathematics 2023, 11, 2021. https://doi.org/10.3390/math11092021
Havaeji H, Dao T-M, Wong T. Supervised Learning by Evolutionary Computation Tuning: An Application to Blockchain-Based Pharmaceutical Supply Chain Cost Model. Mathematics. 2023; 11(9):2021. https://doi.org/10.3390/math11092021
Chicago/Turabian StyleHavaeji, Hossein, Thien-My Dao, and Tony Wong. 2023. "Supervised Learning by Evolutionary Computation Tuning: An Application to Blockchain-Based Pharmaceutical Supply Chain Cost Model" Mathematics 11, no. 9: 2021. https://doi.org/10.3390/math11092021
APA StyleHavaeji, H., Dao, T.-M., & Wong, T. (2023). Supervised Learning by Evolutionary Computation Tuning: An Application to Blockchain-Based Pharmaceutical Supply Chain Cost Model. Mathematics, 11(9), 2021. https://doi.org/10.3390/math11092021






