In-Place Training: Optimizing Rural Health Workforce Outcomes through Rural-Based Education in Australia
Abstract
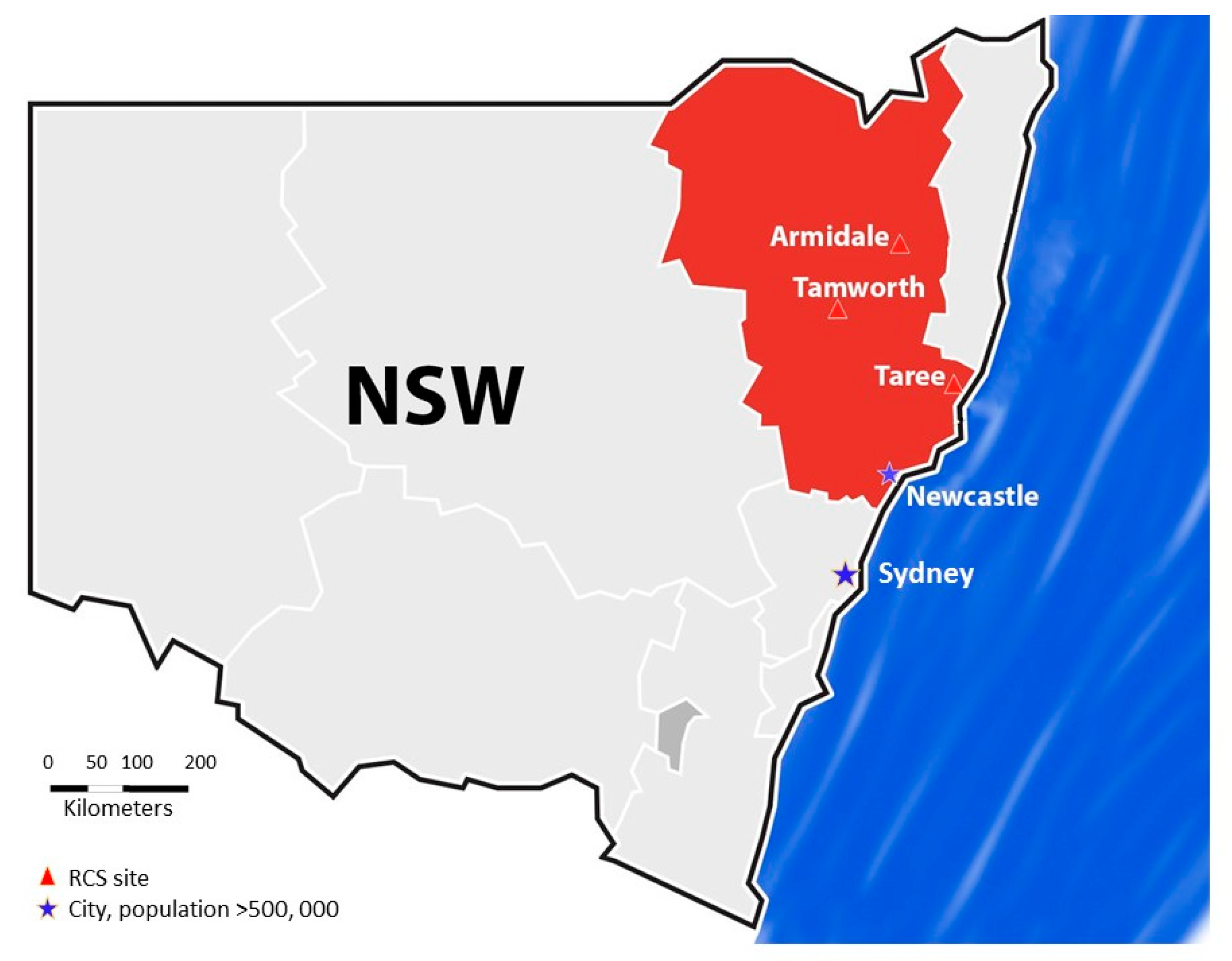
:1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Statistical Analyses
3. Results
Analysis
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- May, J. Clinical Service Integration-a stocktake of the Australian Experience. Futur. Hosp. J. 2015, 2, 142–146. [Google Scholar]
- Koh, C.; May, J. The challenge of health inequalities in rural and remote Australia. In Determining the Future—A Fair Go and Health for All; Connor Court: Canberra, Australia, 2011. [Google Scholar]
- Wilson, N.; Couper, I.; De Vries, E.; Reid, S.; Fish, T.; Marais, B. A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural Remote Health 2009, 9, 1060. Available online: https://www.rrh.org.au/journal/article/1060 (accessed on 23 January 2018). [PubMed]
- Humphreys, J.; Jones, J.; Jones, M.; Hugo, G.; Bamford, E.; Taylor, D. A critical review of rural medical workforce retention in Australia. Aust. Health Rev. 2001, 24, 91–102. [Google Scholar] [CrossRef] [PubMed]
- Mason, J. Review of Australian Government Workforce Programmes; Department of Health: Canberra, Australia, 2013.
- Buykx, P.; Humphreys, J.; Wakerman, J.; Pashen, D. Systematic review of effective retention incentives for health workers in rural and remote areas: Towards evidence-based policy. Aust. J. Rural Health 2010, 18, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Bosco, C.; Oandasan, I. Review of Family Medicine Within Rural and Remote Canada:Education, Practice, and Policy; College of Family Physicians of Canada: Mississauga, ON, Canada, 2016. [Google Scholar]
- McGrail, M.R.; Humphreys, J.S.; Joyce, C.M. Nature of association between rural background and practice location: A comparison of general practitioners and specialists. BMC Health Serv. Res. 2011, 11, 63. [Google Scholar] [CrossRef] [PubMed]
- Kondalsamy-Chennakesavan, S.; Eley, D.S.; Ranmuthugala, G.; Chater, A.B.; Toombs, M.R.; Darshan, D.; Nicholson, G.C. Determinants of rural practice: Positive interaction between rural background and rural undergraduate training. Med. J. Aust. 2015, 202, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Rabinowitz, H.; Diamond, J.; Veloski, J.; Gayle, J. The impact of multiple predictors on generalist physicians’ care of underserved populations. Am. J. Public Health 2000, 90, 1225–1228. [Google Scholar] [PubMed]
- Hays, R.B.; Lockhart, K.R.; Teo, E.; Smith, J.; Waynforth, D. Full medical program fees and medical student career intention. Med. J. Aust. 2015, 202, 46–49. [Google Scholar] [CrossRef] [PubMed]
- Australian Standard Geographical Classification—Remoteness Area (ASGC-RA). Available online: http://www.doctorconnect.gov.au/internet/otd/publishing.nsf/Content/locator (accessed on 5 December 2017).
- Modified Monash Model. Available online: http://www.doctorconnect.gov.au/internet/otd/publishing.nsf/Content/MMM_locator (accessed on 5 December 2017).
- May, J. Rural and Urban–An Exploration of Medical Workforce in Regional Centres in Australia; Monash: Melbourne, Australia, 2016. [Google Scholar]
- Playford, D.E.; Evans, S.F.; Atkinson, D.N.; Auret, K.A.; Riley, G.J. Impact of the Rural Clinical School of Western Australia on work location of medical graduates. Med. J. Aust. 2014, 200, 104–107. [Google Scholar] [CrossRef] [PubMed]
- Playford, D.E.; Nicholson, A.; Riley, G.J.; Puddey, I.B. Longitudinal rural clerkships: Increased likelihood of more remote rural medical practice following graduation. BMC Med. Educ. 2015, 15, 55. [Google Scholar] [CrossRef] [PubMed]
- Hall, L. Bond for going bush unfair. In The Land; Fairfax: Sydney, Australia, 2009. [Google Scholar]
- McGrail, M.R.; Russell, D.J.; O’Sullivan, B.G. Family effects on the rurality of GP’s work location: A longitudinal panel study. Hum. Resour. Health 2017, 15, 75. [Google Scholar] [CrossRef] [PubMed]
| Evidence-Informed Predictors of Long-Term Rural Residence | Current Commonwealth Policy | Local Regional University Response |
|---|---|---|
| Rural and regional origin is a key predictor for rural recruitment | Medical school rural quotas (currently 25% of Commonwealth Funded places) Preferred pathways for Aboriginal and Torres Strait Islander students | 34% rural origin using remote area (RA) classification Special entry “weeks” for Aboriginal students and systematic support through health courses |
| Obligation | ||
| Bonding of medical students requiring return of service provides some workforce | Bonded Medical Places Scheme (BMP) and Rural Medical Bonded Scholarship Scheme (MRBS) | Linkage and immersion with clear training pathways as these students should have access to maximised opportunities for skills acquisition given their need for subsequent service |
| Positive rural undergraduate exposure | Rural Health Multidisciplinary Training program (RHMT) | 25% of students have year-long placements in medicine Opportunities for year-long courses in 7 allied health disciplines Lengths of placements vary with disciplines (longer placements preferred) Interdisciplinary learning opportunities Community engagement and social activities coordinated with inexpensive on-site accommodation and local integration (Bachelor and Spinster Ball principle) |
| Training Pathways | ||
| Importance of mentoring | RHMT | All rural academics are practising clinicians. Mentoring encouraged |
| Importance of regional job opportunities—the end points of training | Regional training hub (RTH) | Local university partnerships with state and private hospitals to support workforce planning |
| Importance of rural connection and connection to place whilst training | RTH | Expanded role for university supporting postgraduate year 1 and 2 and vocational trainees through rural immersion Preferential rural recruitment and access to training options. Professional continuing education supported with vertical integration of multiple learners |
| Incentives | ||
| Differential remuneration or rebates | RHMT support | Subsidised accommodation Additional student support when required |
| Continuing professional development | RHMT | Academics support ongoing education across the clinical continuum with accredited programmes in individual disciplines |
| Importance of spousal employment opportunities | Nil or ad hoc | Recruitment task forces targeted to easy entry (university-supported) Flexibility by hospitals when considering dual doctor couples |
| “Sense of community” (community connection) | Nil or ad hoc | Social-engagement strategies provided by communities for students |
| Year Completed Year 5 | Total | |||
|---|---|---|---|---|
| 2012 | 2013 | 2014 | ||
| Graduates | 142 | 165 | 198 | 505 |
| International student | 21 | 19 | 30 | 70 |
| Unable to be traced | 0 | 3 | 4 | 7 |
| Working overseas | 0 | 1 | 1 | 2 |
| Included in study | 121 | 142 | 163 | 426 |
| Completed rural clinical school (RCS) year | 55 | 55 | 62 | 172 |
| Demographic | Background (RRAS Application) | p Value (χ2) | ||
|---|---|---|---|---|
| Rural, n (n = 132) | Non-Rural, n (n = 294) | Total, n (n = 426) | ||
| Principal place of practice (AHPRA) | ||||
| MMM 1–2 (Major or large regional city) | 107 | 278 | 385 | |
| MMM 3–4 (Medium-large or medium regional city) | 25 | 16 | 41 | <0.000 |
| 4th/5th year RCS placement | ||||
| At least 1 year | 69 | 102 | 171 | |
| Less than 1 year | 63 | 192 | 255 | 0.001 |
| Bonded (BMP/MRBS/RAMUS) | ||||
| Yes | 64 | 74 | 138 | |
| No | 68 | 220 | 288 | <0.000 |
| ATSI | ||||
| Yes | 2 | 6 | 8 | 0.712 |
| No | 130 | 288 | 418 | |
| Gender | ||||
| Female | 77 | 154 | 231 | 0.254 |
| Male | 55 | 140 | 195 | |
| Stage of postgraduate employment | ||||
| PGY 5 | 44 | 78 | 122 | |
| PGY 4 | 47 | 93 | 140 | 0.097 |
| PGY 3 | 41 | 123 | 164 | |
| Age at completion of medical degree | ||||
| 25 or more | 44 | 93 | 137 | 0.728 |
| 24 or less | 88 | 201 | 289 | |
| Characteristic | Odds Ratio (95% CI) | p |
|---|---|---|
| Univariate analysis | ||
| Origin: rural (v non-rural) | 4.060 (2.086–7.901) | <0.000 |
| RCS placement: at least 1 year (v less than 1 year) | 6.293 (2.919–13.566) | <0.000 |
| Bonding: BMP/MRBS/RAMUS (v unbonded) | 0.966 (0.484–1.928) | 0.921 |
| Gender: female (v male) | 2.189 (1.085–4.417) | 0.026 |
| Age at completion of medical degree: 25 or more (v 24 or less) | 2.182 (1.139–4.178) | 0.017 |
| Multivariate analysis | ||
| Origin: rural (v non-rural) | 3.613 (1.752–7.450) | 0.001 |
| RCS placement: at least 1 year (v less than 1 year) | 6.075 (2.716–13.591) | <0.000 |
| Bonding: BMP/MRBS/RAMUS (v unbonded) | 0.589 (0.272–1.275) | 0.179 |
| Gender: female (v male) | 1.794 (0.851–3.783) | 0.125 |
| Age at completion of medical degree: 25 or more (v 24 or less) | 2.550 (1.252–5.194) | 0.010 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
May, J.; Brown, L.; Burrows, J. In-Place Training: Optimizing Rural Health Workforce Outcomes through Rural-Based Education in Australia. Educ. Sci. 2018, 8, 20. https://doi.org/10.3390/educsci8010020
May J, Brown L, Burrows J. In-Place Training: Optimizing Rural Health Workforce Outcomes through Rural-Based Education in Australia. Education Sciences. 2018; 8(1):20. https://doi.org/10.3390/educsci8010020
Chicago/Turabian StyleMay, Jennifer, Leanne Brown, and Julie Burrows. 2018. "In-Place Training: Optimizing Rural Health Workforce Outcomes through Rural-Based Education in Australia" Education Sciences 8, no. 1: 20. https://doi.org/10.3390/educsci8010020
APA StyleMay, J., Brown, L., & Burrows, J. (2018). In-Place Training: Optimizing Rural Health Workforce Outcomes through Rural-Based Education in Australia. Education Sciences, 8(1), 20. https://doi.org/10.3390/educsci8010020





