Abstract
The medical workforce shortfall in rural areas is a major issue influencing the nature of undergraduate medical education in Australia. Exposing undergraduates to rural life through rural clinical school (RCS) placements is seen as a key strategy to address workforce imbalances. We investigated the influence of an extended RCS placement and rural origin on the rural principal place of practice (PPP) of the first 3 graduate cohorts (2012–2014) from a Joint Medical Program offered by two universities based in northern New South Wales. Data was available for 426 eligible graduates. Participation in an extended RCS placement (odds ratio (OR), 6.075, 95% confidence interval (CI) 2.716–13.591), rural background (OR 3.613, 95% CI 1.752–7.450) and being 25 years or older at completion of a medical degree (OR 2.550, 95% CI 1.252–5.194) were all independently associated with rural PPP. Being bonded into a program to practice rurally was not associated with rural PPP. Participation in an extended RCS placement is strongly associated with rural practice in the first 3 to 5 years of practice for graduates from both rural and metropolitan backgrounds. This finding indicates that strategies to improve the rural workforce should focus on the promotion of rural placements, in addition to rural background.
1. Introduction
Most developed countries are wrestling with the challenges of delivering cost-effective primary care. In the face of rapidly aging populations, with the challenging advent of chronic non-communicable diseases and technological innovations in diagnosis and management [1], Australia is facing rapidly increasing demands on both primary and secondary care sectors like many other countries. These demands intensify in underserved areas where health workforce disparities exist, while rural localities face additional service challenges.
With significant climatic extremes, the issues of rurality, isolation and resource allocation are challenging for rural communities, which are notable for higher risk factors and poorer health outcomes [2]. Health access for rural citizens in Australia has become more problematic, with an increasingly inequitable distribution of health professionals. Given that access to affordable health care is considered an important value within Australian society, successive governments have introduced policies aimed at improving recruitment and retention in a number of health professional workforces. These comprise polices targeting selection, training obligations and financial and non-financial incentives [3]. Whilst the health workforce maldistribution and its responses span many disciplines, including nursing and allied health, this paper concentrates on reviewing a regional university’s approach to medical-education enablers, and reflects the important confluence of policy in order to achieve long-term appropriate workforce retention.
Rural workforce policy has been led by the Commonwealth (national) government in Australia, with the states or provinces responsible for most of the post-vocational training positions for those in the medical workforce [4]. Obligatory rural recruitment strategies have had a chequered policy journey, with bonding programs for undergraduates, such as the Bonded Medical Places (BMP) Scheme, the Medical Rural Bonding Scheme (MRBS) and the Rural Australia Medical Undergraduate Scholarship (RAMUS), having been utilised in the last 10-plus years [5]. In 2016, the BMP Scheme return-of-service obligation was reduced from up to 6 years to 12 months for incoming participants. It is unclear whether the 11% of graduates who are bonded nationally will complete their return-of-service obligation [5]. A targeted approach to engaging students and graduates with such obligations to rural practice would be a useful strategy for improving retention. Moreover, there is evidence that a range of factors throughout the medical-training pathway influence the supply of doctors in rural areas [6]. With large increases in the number of medical students graduating in Australia, further focus has been on levers available to government to encourage rural practice. Workforce programs supporting rural-based training have been a key area of endeavour.
The University of Newcastle (UON) in New South Wales (NSW), Australia, has had a proud history of training students with interest in returning to regional and rural areas. It also has a strong history of educating Indigenous medical students (those identifying as Aboriginal or Torres Strait Islander), having trained an estimated 36.6% of the Indigenous doctors in Australia in 2014 [7]. The university has representation on the International Reference Group for Global Consensus for Social Accountability in Medical Schools. Following Commonwealth government funding in 2006, the university formalized rural clinical schools (RCS) in three communities in north-western NSW (Figure 1).
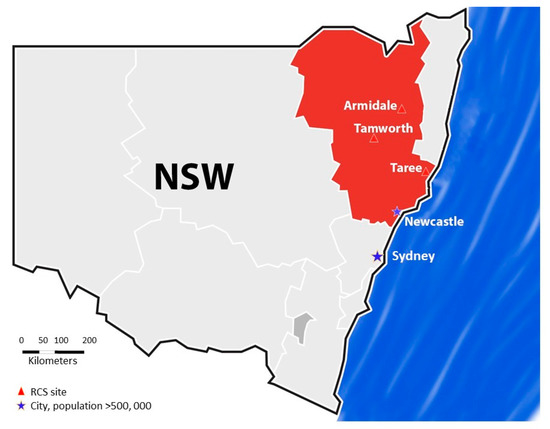
Figure 1.
Location of the Joint Medical Program (University of Newcastle and University of New England) within the Hunter and New England regions of NSW.
In 2008, the University of New England (UNE) joined with the UON to deliver a Joint Medical Program (JMP). The UON main campus is located in a major city with a population of 250,000 whereas UNE is located in Armidale, in northern NSW, a medium to large regional city (population 25,000). The JMP was established in partnership with the Hunter New England local health district and the Central Coast local health district. This unique combination of two universities and two local health districts (LHDs) has enabled the provision of medical training across rural, regional and metropolitan footprints in NSW. The region is also one of 17 regional areas in Australia now supported under the Commonwealth government-funded Rural Health Multidisciplinary Training (RHMT) workforce program.
During the final years of the JMP (4th and 5th year) all students have the opportunity to gain clinical experience in a rural setting by undertaking semester or year-long RCS-supported placements. In the 4th year, students undertake 6-week rotations in medicine/surgery and women, adolescent and children’s health and 2 electives. In the 5th year, rotations of 4 to 7 weeks’ duration are undertaken in medicine, psychiatry/palliative care, primary health care, emergency medicine and anaesthesia/intensive care, oncology/orthopaedic surgery and a student-initiated special study elective. Placements are configured so that students have an immersion experience in one community, with opportunities for community engagements.
Table 1 identifies the key evidence-informed approaches, the key parameters noted by government, and UON and UNE’s response in Australia. Similar themes and evidence-based approaches are seen in many countries [3,7].

Table 1.
Key evidence-informed predictors of long-term rural residence, Australian Commonwealth government policies and rationale.
Selecting students who are more likely to consider rural practice is well affirmed in the medical literature [8,9]. Existing evidence upholds the importance of supporting enrolment from underserved areas [10] and also notes that high levels of debt will reduce generalist careers and rural return [11]. The JMP has provided a pathway for rural and Indigenous students into medicine since 2008, with targeted outreach to attract students of low socio-economic status addressing the core UON value of ensuring equity of access to high-quality education. In Australia, multiple classifications are utilised for rural and remote programs; the Australian Standard Geographical Classification–Remoteness Area (ASGC–RA) system [12] is principally a geographic classification system, whereas the new Modified Monash classification system takes into account both geography and population size [13].
In 2016, 34.1% (58 students) of that year’s entry cohort of JMP students originated from rural and remote areas (ASGC–RA 2–5) and 10.6% (60 students) of the total medical student cohort identified as Indigenous. Students who enrol in the JMP apply to UON and, via a preference and allocation process, are offered places at either UON or UNE. High-school performance, the Undergraduate Medicine and Health Sciences Admission Test (UMAT), a multiple skills assessment (interview) and personal qualities assessment complete the rural admissions process. In NSW the postgraduate journey begins with a 2-year pre-vocational training experience undertaken in highly supervised (mainly hospital) settings, followed by entry into post-vocational training. Specialist training for general practice can be achieved in 3–5 years, with most of the other specialties taking 5–8 years to complete.
Demographic and workforce outcome data are being collected to identify the impacts of various policy approaches on JMP graduates’ locations, although the capacity for attribution of individual factors should be challenged as locational decision making is often a result of multiple synergistic influences or factors [6,14]. This study aimed to determine what influence extended RCS placements had on postgraduate-practice location. Our hypothesis was that extended RCS placements are positively associated with rural workforce location in the early postgraduate years. This paper reports the short-term workplace outcomes for the first three graduating cohorts of the JMP and explores the policy-relevant trends in the key evidenced attraction factors.
2. Materials and Methods
This is a retrospective cross-sectional study of the cohort of domestic students (all those not studying on international student visas) graduating from the JMP between 2012 and 2014. This study method was chosen as the data is routinely collected by the universities in order to satisfy Commonwealth funding requirements, and has been used by others in similar studies [15,16]. Ethics approval for the study was obtained from the University of Newcastle and University of New England Human Research Ethics Committees (H-2017-0191).
2.1. Data Collection
Demographic data relating to rural background, RCS placement, bonding, Aboriginal status, age and gender was collected for all JMP students from UON and UNE datasets. Application for entry into the JMP through the Rural and Remote Admissions Scheme (RRAS) was used as an indicator for rural background. The current principal place of practice (PPP) for each graduate was sourced from the Australian Health Practitioner Agency (AHPRA) website. Practice locations were classified into district of workforce shortage (DWS) using the Modified Monash Model (MMM) where category MMM 1–2 represents metropolitan and regional locations with populations >50,000 and MMM 3–4 represents large to medium regional/rural populations of 15,000 to 50,000. Graduates were presumed to be in their 5th, 4th and 3rd postgraduate years (PGY), respectively, at the time the AHPRA website data was sourced (October 2016–January 2017). Not all students complete the degree program within the minimum 5-year time frame, therefore data is reported on the basis of graduation year rather than year of program entry in order to compare graduate cohorts at similar stages of their careers.
2.2. Statistical Analyses
De-identified data was entered into Statistical Package for Social Sciences (SPSS, version 24, IBM Corp., New York, NY, USA). Univariate comparisons were performed on categorical variables using the Chi-square or Fishers exact tests with a p value less than 0.05 considered significant. Binomial logistic regression using the backwards stepwise elimination method (p = 0.2 cut off for non-significant variables) was used to determine factors predictive of rural practice. Interactions between all covariates (other than Aboriginality) were included in the analysis, but none were significant and were therefore not included in the final model. Further logistic regressions were undertaken to determine the effects of covariates independent of rural background and RCS participation. Odds ratios (OR) were calculated for statistically significant variables, together with 95% confidence intervals (CI).
3. Results
A total of 435 domestic students graduated from the JMP between 2012 and 2014. AHPRA records were found for 428 graduates (98%), 426 of whom were registered as practicing in Australia. A description of the graduate study cohort is presented in Table 2.

Table 2.
Description of UON/UNE Joint Medical Program medical graduates.
Of the 426 graduates included in the study, 132 (31%) applied for entry to the JMP under the RRAS (Table 3) and are considered to have a rural background for the purpose of this study. There were 138 graduates (32%) subject to some type of rural bonding agreement (BMP/MRBS/RAMUS), 54% of whom were from a non-rural background. Rural placements of at least one year in the 4th/5th year of the program had been undertaken by 171 (40%) graduates, 60% of whom were from a non-rural background. Overall, 9.8% of graduates were principally located in a regional/rural area (MMM 3–4); 8.5% in PGY 3, 8.6% in PGY 4 and 12.3% in PGY 5 (data not shown).

Table 3.
Demographic characteristics of UON/UNE Joint Medical Program graduates (2012–2014).
Analysis
There was a statistically significant difference in graduate background with respect to principal place of practice (p < 0.000), RCS placements (p = 0.001) and bonding (p < 0.000) (Table 3). Significant associations were also found with RCS placements and both gender (p = 0.042) and bonding (p = 0.008) (data not shown).
Univariate analysis of independent variables showed graduates who had undertaken RCS placements of at least one year (OR 6.293, 95% CI 2.919–13.566) were over 6 times more likely to be practicing in a rural location in postgraduate years 3–5, while those with a rural background were 4 times more likely (OR 4.060, 95% CI 2.086–7.901) (Table 4). Graduate age and gender had a smaller, but significant, effect on PPP location. Being female (OR 2.189, 95% CI 1.085–4.417) and at least 25 years old at completion of their medical degree (OR 2.182, 95% CI 1.139–4.178) was associated with rural PPP location. Aboriginality was not included in the analysis, as expected cell counts were too small (<5). The effect of bonding was not statistically significant.

Table 4.
Univariate and multivariate analysis of rural principal place of practice (MMM 3–4).
Multivariate logistic regression analysis for main effects showed that undertaking rural placements of at least one year (OR, 6.075, 95% CI 2.716–13.591), rural background (OR 3.613, 95% CI 1.752–7.450) and being 25 years or older at completion of a medical degree (OR 2.550, 95% CI 1.252–5.194) were predictive of practice in a rural location (Table 4). Gender (p = 0.125) and bonding (p = 0.179) were included in the model, but were not statistically significant predictors. The model explained 24% of the variance in PPP location and correctly classified 91.3% of cases. Sensitivity was 17.1%, specificity was 99.2%, positive predictive value was 70.0, and negative predictive value was 91.8%.
Interaction terms for RCS placement with bonding, origin and gender and for origin with bonding were included in an additional regression analysis, but none were found to predict rural practice significantly (results not shown).
4. Discussion
The lead-time before policy change impacts on the medical workforce is necessarily long. The RCS at UON commenced in 2006, meaning that the first cohort of graduates should now be reviewing their long-term practice location. Proxy markers of interest or long-term rural intent may be required. One of these might be the preferential recruitment into postgraduate hospital employment in regional locations where medical student training occurred. One of the challenges with this measure is that doctors often must return to city hospitals to get access to specialty training or special skills. The tracking data reported here for the first three cohorts of JMP graduates is preliminary, but does give cause for optimism in that both rural origin and rural exposure appear to correlate independently with rural practice postcode.
Rural background was again confirmed an important predictor of long-term rural residence. A RCS placement of at least one year does appear to be linked to PGY 3–5 workplace location, independent of rural background and bonding status. This affirms the independent effect of positive rural exposure seen by others [9,15]. It also supports the notion that multiple strategies are required to redress the rural medical workforce deficit, and that an emphasis on rural background only could miss a group of students who, when exposed to rural locations, can see a career for themselves. This is an important finding as it would support the policy of providing rural placements to students of both rural and metropolitan origin.
It is possible that rural intent could be set prior to the decision to participate in an extended RCS placement and, therefore, could be a potential confounder of practice location. Intent was not investigated in this study, since this data was not available to the researchers. A study of graduates from the University of Western Australia found a positive interaction between prior rural intent and RCS participation with respect to rural workforce outcomes in postgraduate years 2–5 [15].
Bonding was not related to rural-practice location. Given the early nature of this data along the training pathway, there is no indication whether rural bonded graduates were still training or if they had found alternative pathways out of the bond. This measure was unpopular with students and dissatisfaction has been reported in the medical press [17]. This may have led to the change in policy to shorten the bonding requirement in 2015. The success of bonding as a key obligatory strategy is not demonstrated and will require recasting and reviewing the long-term retention evidence.
The other factor of unclear significance was age. The inclusion of age as an independent variable is required in future analysis to investigate its relationship to long-term rural residence. Previous observations have suggested that an older age (more likely for those in postgraduate medical courses) may predict long-term rural recruitment [15].
Table 1 details major training pathway initiatives that have been used by the Commonwealth government. Evidence that longer later placements are positively associated with longer-term rural residence is continuing to accumulate [9]. The challenge has been to develop positive experiences for students in areas where clinicians have significant service delivery demands in addition to teaching. The opportunity for students to experience the benefits of work variety and clinical autonomy have to be balanced by the identification of positive workplace culture and perceived “work–life balance” [14]. Changing lifestyle factors such as the need for dual careers for most couples, and preference for coastal locations, will continue to influence the attractiveness of rural residence. Social factors such as spousal employment and educational requirements for children are both now known to influence retention [18].
Key questions remain about how to maximize rural-based medical education as a workforce strategy. They include better definition of rural origin, rural intent and the location of rural training and its impact. The other major challenge is predicting retention as opposed to recruitment. At a time where social change and technological impacts are changing the delivery of medical services, the understanding of what is reasonable retention must be explored.
Many of the important ingredients for a sustained long-term rural workforce do lie outside rural areas; however, a positive pipeline approach, such as described here, is already impacting the postgraduate workforce, providing an economic boom to the areas in which it is delivered, and shining a spotlight on the workforce and the health of rural and remote communities. With a long-term shared vision to include specialist training in the same locations, it will almost certainly assist in addressing medical workforce maldistribution.
5. Conclusions
Participation in extended JMP RCS placements is strongly associated with rural practice in the first 3 to 5 postgraduate years, irrespective of student background. This finding indicates that strategies aimed at expanding the rural workforce should include the promotion of rural placements as well as rural background. Further research on the longer-term workforce outcomes of this cohort, and evaluation of additional measures aimed at capitalising on the interest of graduates in rural locations in the early stages of their career, is required to meet the health care needs of rural populations.
Acknowledgments
The Australian Government funds the Rural Health Multidisciplinary Training Program.
Author Contributions
Jennifer May and Julie Burrows conceived and designed the tracking study with assistance from Leanne Brown. Julie Burrows extracted the data and performed the analysis. Jennifer May wrote the paper, Julie Burrows and Leanne Brown contributed to editing and writing.
Conflicts of Interest
The authors declare no conflict of interest. The funding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
References
- May, J. Clinical Service Integration-a stocktake of the Australian Experience. Futur. Hosp. J. 2015, 2, 142–146. [Google Scholar]
- Koh, C.; May, J. The challenge of health inequalities in rural and remote Australia. In Determining the Future—A Fair Go and Health for All; Connor Court: Canberra, Australia, 2011. [Google Scholar]
- Wilson, N.; Couper, I.; De Vries, E.; Reid, S.; Fish, T.; Marais, B. A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural Remote Health 2009, 9, 1060. Available online: https://www.rrh.org.au/journal/article/1060 (accessed on 23 January 2018). [PubMed]
- Humphreys, J.; Jones, J.; Jones, M.; Hugo, G.; Bamford, E.; Taylor, D. A critical review of rural medical workforce retention in Australia. Aust. Health Rev. 2001, 24, 91–102. [Google Scholar] [CrossRef] [PubMed]
- Mason, J. Review of Australian Government Workforce Programmes; Department of Health: Canberra, Australia, 2013.
- Buykx, P.; Humphreys, J.; Wakerman, J.; Pashen, D. Systematic review of effective retention incentives for health workers in rural and remote areas: Towards evidence-based policy. Aust. J. Rural Health 2010, 18, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Bosco, C.; Oandasan, I. Review of Family Medicine Within Rural and Remote Canada:Education, Practice, and Policy; College of Family Physicians of Canada: Mississauga, ON, Canada, 2016. [Google Scholar]
- McGrail, M.R.; Humphreys, J.S.; Joyce, C.M. Nature of association between rural background and practice location: A comparison of general practitioners and specialists. BMC Health Serv. Res. 2011, 11, 63. [Google Scholar] [CrossRef] [PubMed]
- Kondalsamy-Chennakesavan, S.; Eley, D.S.; Ranmuthugala, G.; Chater, A.B.; Toombs, M.R.; Darshan, D.; Nicholson, G.C. Determinants of rural practice: Positive interaction between rural background and rural undergraduate training. Med. J. Aust. 2015, 202, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Rabinowitz, H.; Diamond, J.; Veloski, J.; Gayle, J. The impact of multiple predictors on generalist physicians’ care of underserved populations. Am. J. Public Health 2000, 90, 1225–1228. [Google Scholar] [PubMed]
- Hays, R.B.; Lockhart, K.R.; Teo, E.; Smith, J.; Waynforth, D. Full medical program fees and medical student career intention. Med. J. Aust. 2015, 202, 46–49. [Google Scholar] [CrossRef] [PubMed]
- Australian Standard Geographical Classification—Remoteness Area (ASGC-RA). Available online: http://www.doctorconnect.gov.au/internet/otd/publishing.nsf/Content/locator (accessed on 5 December 2017).
- Modified Monash Model. Available online: http://www.doctorconnect.gov.au/internet/otd/publishing.nsf/Content/MMM_locator (accessed on 5 December 2017).
- May, J. Rural and Urban–An Exploration of Medical Workforce in Regional Centres in Australia; Monash: Melbourne, Australia, 2016. [Google Scholar]
- Playford, D.E.; Evans, S.F.; Atkinson, D.N.; Auret, K.A.; Riley, G.J. Impact of the Rural Clinical School of Western Australia on work location of medical graduates. Med. J. Aust. 2014, 200, 104–107. [Google Scholar] [CrossRef] [PubMed]
- Playford, D.E.; Nicholson, A.; Riley, G.J.; Puddey, I.B. Longitudinal rural clerkships: Increased likelihood of more remote rural medical practice following graduation. BMC Med. Educ. 2015, 15, 55. [Google Scholar] [CrossRef] [PubMed]
- Hall, L. Bond for going bush unfair. In The Land; Fairfax: Sydney, Australia, 2009. [Google Scholar]
- McGrail, M.R.; Russell, D.J.; O’Sullivan, B.G. Family effects on the rurality of GP’s work location: A longitudinal panel study. Hum. Resour. Health 2017, 15, 75. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).