An Experiential Aged Care Module for First-Year Undergraduate Medical Students
Abstract
1. Introduction
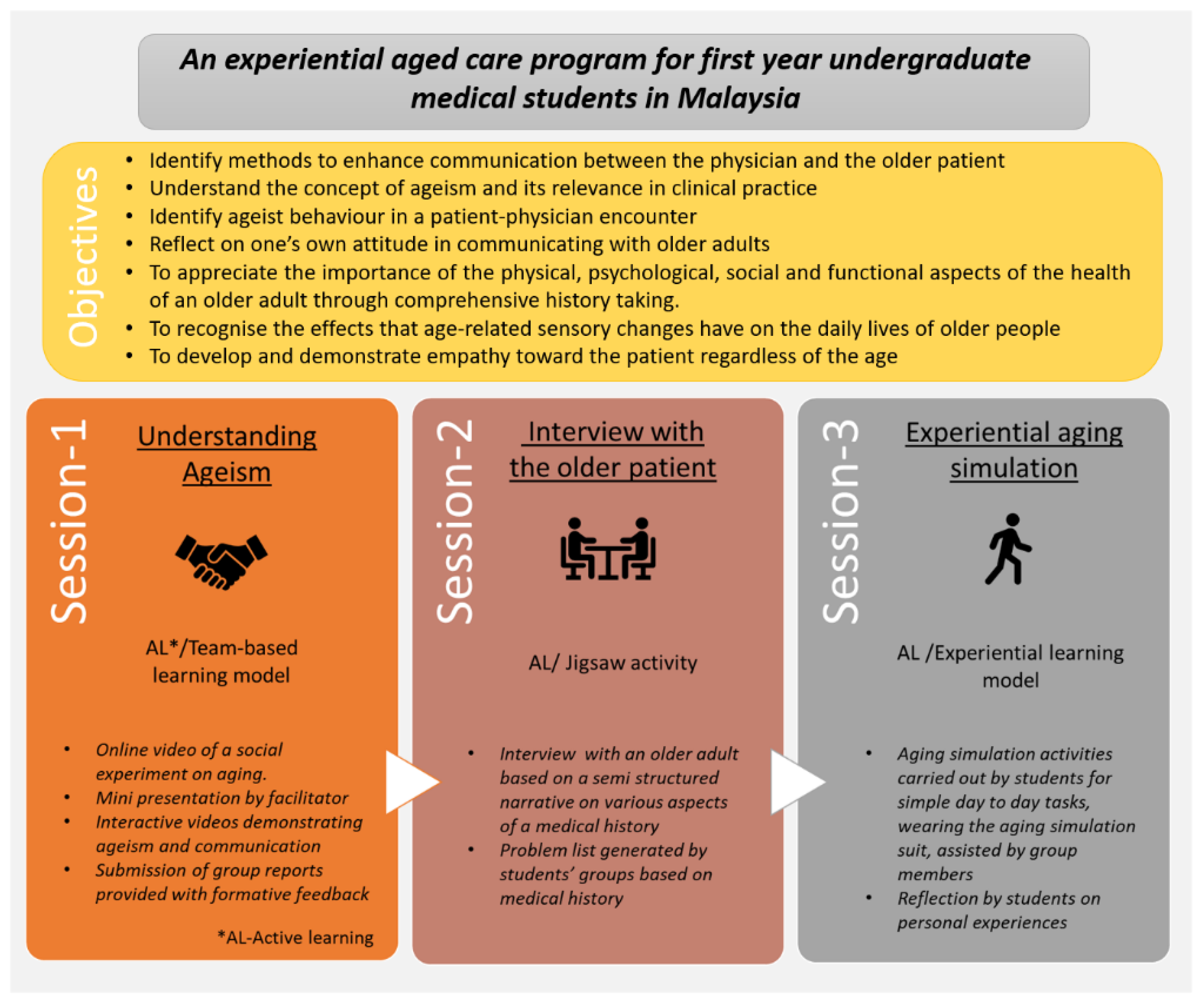
2. The Program
- Session 1: Understanding ageism
- Session 2: Interview with the older patient
- Session 3: Aging simulation
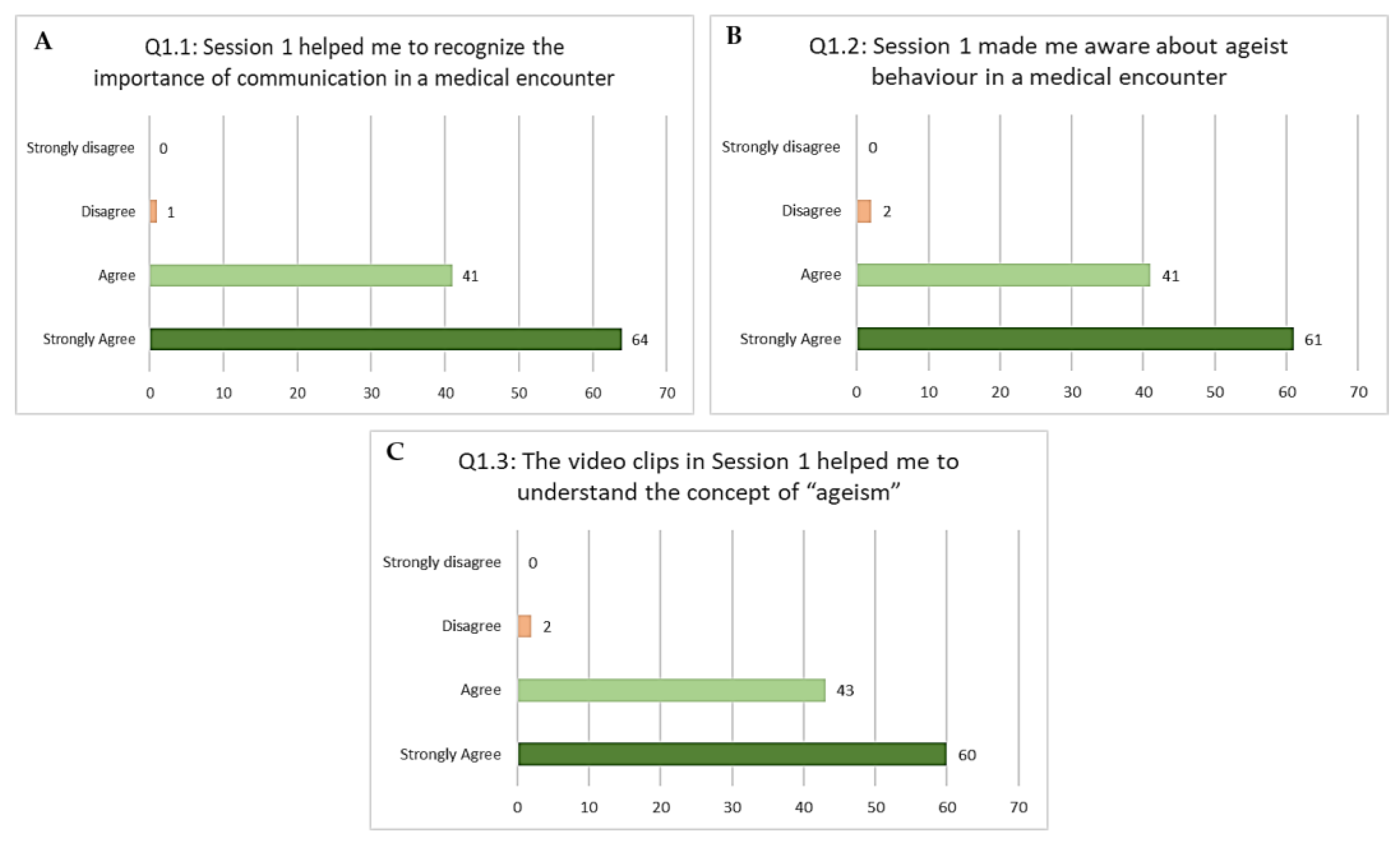
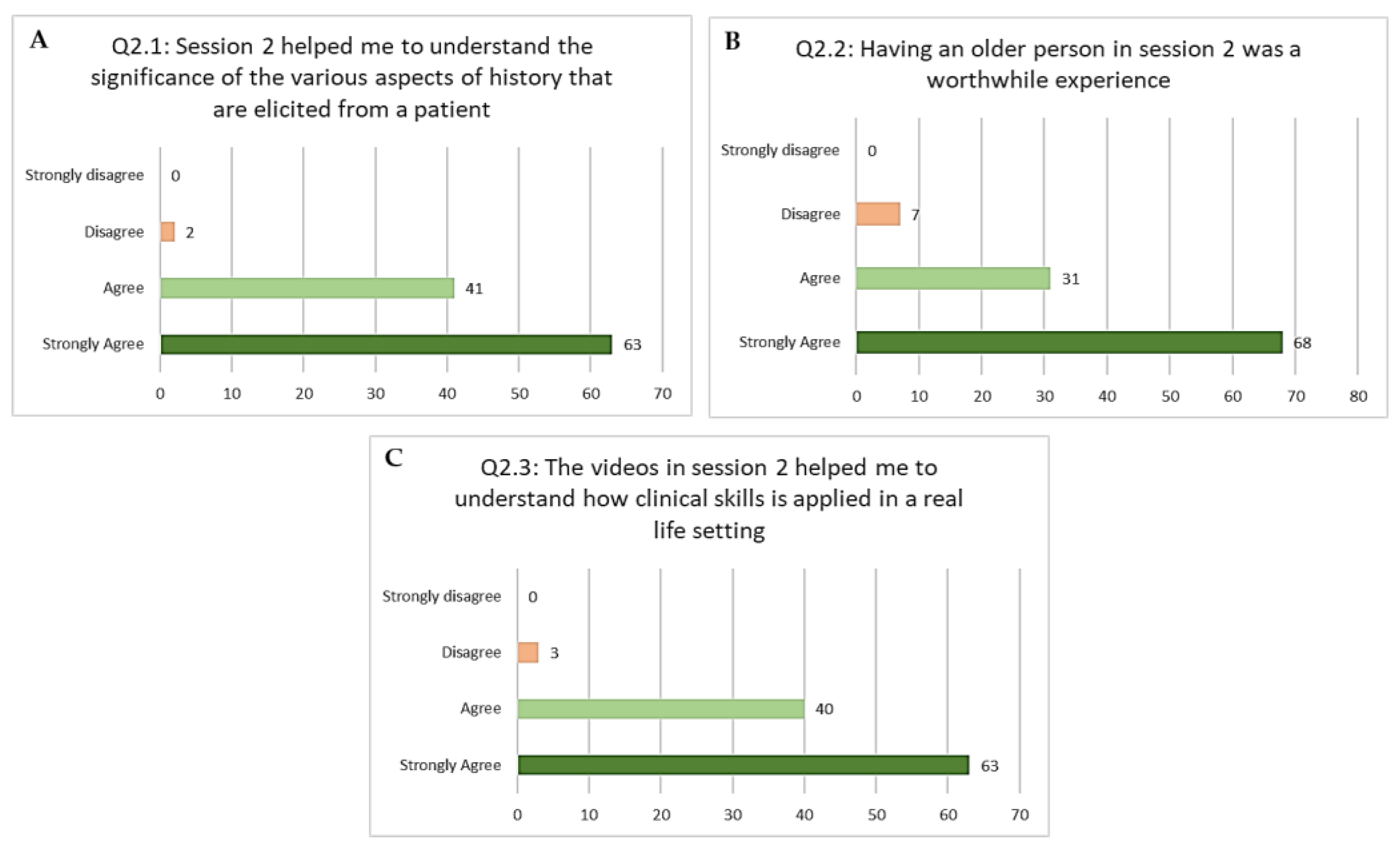
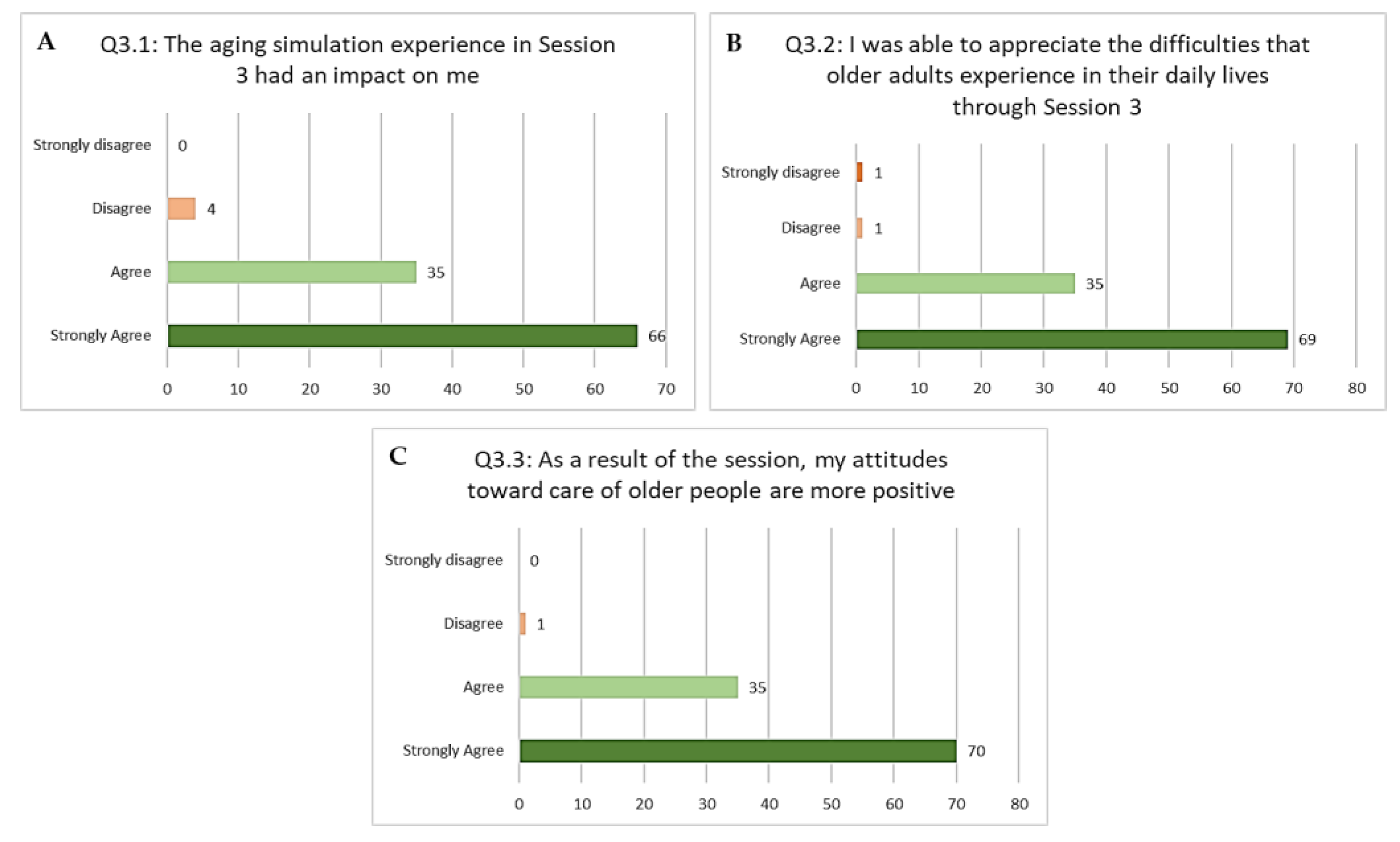
3. Feedback
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Population Division, Department of Economic and Social Affairs, United Nations. World Population Ageing 2017-Highlights (ST/ESA/SER.A/397); United Nations: New York, NY, USA, 2017. [Google Scholar]
- UNFPA Asia-Pacific Regional Office (APRO). Addressing Population Ageing in Asia and the Pacific Region: A Life-Cycle Approach; UNFPA: Bangkok, Thailand, 2021. [Google Scholar]
- Department of Statistics Malaysia. Current Population Estimates; Department of Statistics Malaysia: Putrajaya, Malaysia, 2020.
- Van den Heede, K.; Bouckaert, N.; Van de Voorde, C. The impact of an ageing population on the required hospital capacity: Results from forecast analysis on administrative data. Eur. Geriatr. Med. 2019, 10, 697–705. [Google Scholar] [CrossRef]
- Sallehuddin, H.; Tan, M.P.; Blundell, A.; Gordon, A.; Masud, T. A national survey on the teaching provision of undergraduate geriatric medicine in Malaysia. Gerontol. Geriatr. Educ. 2021, 1–12. [Google Scholar] [CrossRef] [PubMed]
- De Biasio, J.C.; Parkas, V.; Soriano, R.P. Longitudinal assessment of medical student attitudes toward older people. Med. Teach. 2016, 38, 823–828. [Google Scholar] [CrossRef] [PubMed]
- São José, J.M.S.; Amado, C.A.F.; Ilinca, S.; Buttigieg, S.C.; Taghizadeh Larsson, A. Ageism in health care: A systematic review of operational definitions and inductive conceptualizations. Gerontologist 2019, 59, e98–e108. [Google Scholar] [CrossRef] [PubMed]
- Mateos-Nozal, J.; Beard, J.R. Global approaches to geriatrics in medical education. Eur. Geriatr. Med. 2011, 2, 87–92. [Google Scholar] [CrossRef]
- Keller, I.; Makipaa, A.; Kalenscher, T.; Kalache, A. Global Survey on Geriatrics in the Medical Curriculum: A Collaborative Study of WHO and the International Federation of Medical Students’ Association; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Arai, H. Geriatrics in the most aged country, Japan. Arch. Gerontol. Geriatr. 2009, 49, S1–S2. [Google Scholar] [CrossRef][Green Version]
- Chen, L.-K. Geriatric medical education in rapidly aging Asia. Aging Med. Healthc. 2020, 11, 72–73. [Google Scholar] [CrossRef]
- Sallehuddin, H.; Tan, M.P.; Blundell, A.; Gordon, A.L.; Masud, T. Development of a Malaysian undergraduate geriatric medicine curriculum. Aging Med. Healthc. 2020, 11, 82–88. [Google Scholar] [CrossRef]
- Koh, G.C.; Merchant, R.A.; Lim, W.S.; Amin, Z. The knowledge-attitude dissociation in geriatric education: Can it be overcome? Ann. Acad. Med. Singap. 2012, 41, 383. [Google Scholar]
- Adelman, R.D.; Capello, C.F.; LoFaso, V.; Greene, M.G.; Konopasek, L.; Marzuk, P.M. Introduction to the older patient: A “first exposure” to geriatrics for medical students. J. Am. Geriatr. Soc. 2007, 55, 1445–1450. [Google Scholar] [CrossRef]
- Wolff, M.; Wagner, M.J.; Poznanski, S.; Schiller, J.; Santen, S. Not another boring lecture: Engaging learners with active learning techniques. J. Emerg. Med. 2015, 48, 85–93. [Google Scholar] [CrossRef]
- Chen, M.; Ni, C.; Hu, Y.; Wang, M.; Liu, L.; Ji, X.; Chu, H.; Wu, W.; Lu, C.; Wang, S. Meta-analysis on the effectiveness of team-based learning on medical education in China. BMC Med. Educ. 2018, 18, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Moffett, J. Twelve tips for “flipping” the classroom. Med. Teach. 2015, 37, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, B.; Mehta, B.; Mavai, M.; Singh, Y.R.; Singhal, A. Medical education/original article jigsaw method: An innovative way of cooperative learning in physiology. Indian J. Physiol. Pharm. 2017, 61, 315–321. [Google Scholar]
- Gugliucci, M.R.; Weiner, A. Learning by living: Life-altering medical education through nursing home-based experiential learning. Gerontol. Geriatr. Educ. 2013, 34, 60–77. [Google Scholar] [CrossRef] [PubMed]
- Lucchetti, A.L.; Duarte, B.S.; de Assis, T.V.; Laurindo, B.O.; Lucchetti, G. Is it possible to teach Geriatric Medicine in a stimulating way? Measuring the effect of active learning activities in Brazilian medical students. Australas. J. Ageing 2019, 38, e58–e66. [Google Scholar] [CrossRef] [PubMed]
- Punja, D.; Kalludi, S.N.; Pai, K.M.; Rao, R.K.; Dhar, M. Team-based learning as a teaching strategy for first-year medical students. Australas. Med. J. 2014, 7, 490. [Google Scholar] [CrossRef] [PubMed]
- Correia, R.H.; Klea, L.; Campbell, G.; Costa, A.P. Fostering intergenerational education: An experiential learning program for medical students and older adults. Can. Med. Educ. J. 2020, 11, e74. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, J.T.; Wray, L.A.; Halter, J.B.; Williams, B.C.; Supiano, M.A. Relating medical students’ knowledge, attitudes, and experience to an interest in geriatric medicine. Gerontologist 2003, 43, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Lucchetti, A.L.G.; Lucchetti, G.; de Oliveira, I.N.; Moreira-Almeida, A.; da Silva Ezequiel, O. Experiencing aging or demystifying myths?—Impact of different “geriatrics and gerontology” teaching strategies in first year medical students. BMC Med. Educ. 2017, 17, 1–9. [Google Scholar]
| Question | Excerpts from Students’ Feedback |
|---|---|
| Which part of the session was most useful to you and why? | “The very first session, because I never thought about the elderly and their health deeply. This session opened my eyes”. “Session 1 helped me to realize how important verbal and non-verbal cues are, when it comes to taking a medical history.” |
| “Interviewing an older person made me realize that they have different needs compared to the general population” “Session 2 was a meaningful experience. It showed me how older people communicate and how the different parts of history play an integral role in managing the patient as a whole” | |
| “When I wore the suit, I wanted to do everything by myself. I can see how you need to respect the independence of the older individual and not just do everything for them” “Going up and down the stairs was very difficult. It reminded me of my grandma who has arthritis.” |
| Question | Excerpts from Students’ Feedback |
|---|---|
| How did this curricular exposure influence you? | “I feel that I can better empathise and relate to the elderly better after the sessions. I found it difficult to understand why the elderly had constant aches and pains but now I feel that I will be able to address their concerns in a better way. I would like to thank the doctors for giving us this learning opportunity.” |
| “It made me more empathetic towards older people and realise how much they have to go through on a daily basis.” “I feel that people often assume that an old person is exaggerating their complaints. However, after these sessions, I am truly able to feel the frustration and helplessness elderly feel on a daily basis.” | |
| “It reminded me that we are going to be dealing with an ageing population and these 3 sessions helped me realise that we need to equip ourselves well for future encounters with the elderly.” “It gave me a very good experience and taught me to look at medicine, life and the elderly in a new angle. I appreciate the effort and this module as it gives us a more hands on experience to aid what we will face in the future. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alex, D.; Kumari, Y.; Kadirvelu, A. An Experiential Aged Care Module for First-Year Undergraduate Medical Students. Educ. Sci. 2021, 11, 565. https://doi.org/10.3390/educsci11100565
Alex D, Kumari Y, Kadirvelu A. An Experiential Aged Care Module for First-Year Undergraduate Medical Students. Education Sciences. 2021; 11(10):565. https://doi.org/10.3390/educsci11100565
Chicago/Turabian StyleAlex, Deepa, Yatinesh Kumari, and Amudha Kadirvelu. 2021. "An Experiential Aged Care Module for First-Year Undergraduate Medical Students" Education Sciences 11, no. 10: 565. https://doi.org/10.3390/educsci11100565
APA StyleAlex, D., Kumari, Y., & Kadirvelu, A. (2021). An Experiential Aged Care Module for First-Year Undergraduate Medical Students. Education Sciences, 11(10), 565. https://doi.org/10.3390/educsci11100565






