1. Introduction
This is a conference paper for a special edition journal, related to the Association for the Advancement of Technology in Europe (AAATE) conference (2017), under the theme “Harnessing Technology to Improve Lives” [
1].
It is estimated that 400,000 residents are now living in care homes in the UK [
1]. Many have based their decision to move on the nature of their needs, for example enduring a disability that can no longer be supported in their own home [
1,
2]. Due to the increasingly aging population, it is likely that the need for care homes will increase across England [
3]. This will necessitate the development and assessment of innovative methods for delivering efficient health care in care homes [
4]. Videoconferencing has been trialled in care homes in a range of countries with the aim of improving resident access to health care for a wide range of purposes, such as; assessment [
2,
3,
4,
5,
6,
7,
8,
9], management [
10,
11,
12,
13,
14] and diagnosis [
15]. Associated evaluation and research has looked at a range of clinical outcomes such as; hospital admissions [
3,
16,
17,
18,
19,
20], A&E attendances [
21] and medication use [
13], with the main body of evidence originating from America [
2,
3,
8,
9,
12,
13,
14,
15,
19,
22,
23,
24].
A scoping review previously undertaken identified relevant research to inform survey content. The most popular research design reported in the search yield was case studies, exploring the feasibility of videoconferencing in different care home contexts [
25]. All (26) papers identified in the review reported on outcomes post- implementation of videoconferencing and consequently no information was identified regarding the knowledge/attitude of staff and residents pre- implementation. Nine papers reported evidence suggesting that staff satisfaction is high in care homes using videoconferencing [
2,
7,
8,
12,
14,
17,
21,
22,
26]. However, Vidyo (2018) has since commissioned a study to look at the primary reasons for non-adoption of virtual health services in America. Three of the main reasons identified were due to cost, others include: infrastructure, staffing, privacy and concern over successful integration of health care records [
27].
Three papers identified in the scoping review explored the use of videoconferencing in the UK [
11,
18,
20], with two looking at videoconferencing in care homes for older adults [
18,
20] and one looking at the use of it in psychiatric patients [
11]. Both Pope et al. (2013) and Hex (2015) found videoconferencing reduced health care costs and emergency department attendances. Hex (2015) observed these effects in care homes that used the 24/7 Airedale hub.
Airedale NHS Trust established a Telehealth Hub in 2011 and since then have implemented videoconferencing in 534 care homes across the Yorkshire and Humber region [
28]. Services include; the Gold Line (a line that provides support for palliative care) and the intermediate care hub where staff can be called 24 h a day, seven days a week for advice about residents’ health. If deemed necessary calls can be escalated to emergency care staff, a doctor at the hospital or an out-of-hours GP [
29].
However, despite this innovation in service delivery in one region of England, there is a deficit of literature on other providers of such services and on care home managers’ perceptions of videoconferencing across England [
5].
The survey described in this paper aimed to explore the use of videoconferencing to access health care in English care homes, identifying levels of knowledge of, and attitudes towards videoconferencing. The survey was conducted in early 2015, with the findings being used to inform Clinical Commissioning Groups (CCGs) who commission the majority of hospital and community NHS services in England [
30] and health care professionals regarding the current state of provision as part of larger evaluation. The findings from the study were reported as guidelines for commissioners and health professionals [
31].
2. Materials and Methods
Qualitative interviews were used to develop a cross-sectional survey to enable the interpretation of views from a range of care home managers [
32]. Four care home managers took part in the qualitative interviews and 124 participants were included in the analysis for the survey. In total 124 participants took part.
The content for the survey (See
Supplementary) was developed following five key stages defined by Steven (2012) [
33]. The first was identifying participants to inform the development of the survey. Due to time constraints, the researcher invited care home managers at a Special Interest Group (SIG) to participate. This event was one in a series of special interest groups held by Sheffield University, UK and was organised to raise awareness of technology’s potential for the care sector and to foster discussion. Attendees included care home managers, healthcare workers, technology providers, researchers, staff from the local authority, NHS Trusts and service commissioners. Two of the care home managers were from nursing homes (one home that used videoconferencing and one that did not) and two managers from residential homes (one home that used videoconferencing and one that did not). The second step was to decide on the method and design of interviews for survey development. In order to explore participant’s experiences and allow for cross-case comparability semi-structured interviews were used [
34]. The interview guide that was developed, considered the information needed in order to map current provision, attitudes and knowledge of videoconferencing in the region. The findings were analysed thematically. Where concerns had been raised regarding the benefits of technology or videoconferencing, these were used to inform response categories (for example, reasons for why homes may not want to implement videoconferencing), as well as to identify other possible factors that may influence uptake and effectiveness. The findings from the scoping review [
25], notes from the SIG and the interviews (See
Supplementary) were used to inform/refine the response categories for the survey. This ensured that the most pertinent factors were represented in the survey, with the categories being exhaustive [
35]. The interviewed participants then piloted the questionnaire either in the postal or online format. The observations of those who completed the pilot survey informed the development of the instrument to make it more concise and questions were re-worded where participants stated these were unclear [
35].
The survey was composed of a range of ranking, likert scale, multiple choice and open ended questions to enable the collection of a broad range of data. Open ended questions were included to allow the respondent to provide additional feedback [
32]. The instructions highlighted that the survey would take between 10–15 min to complete. The researcher posted the survey and covering letter to 859 care homes registered with the UK Care Quality Commission (CQC) as caring for people solely over the age of 65, with the intention that the manager would complete it. The cover letter included a link to the online version of the survey and information on the prize draw they would be entered into upon completing and returning the survey. The researcher believed this would help improve the response rate. The researcher received ethical approval from the School of Health and Related Research (ScHARR) ethics committee for this study.
4. Discussion
Prior published work reported a deficit in knowledge on attitudes, knowledge and views of staff towards videoconferencing in care homes prior to implementation and only nine papers had examined staff satisfaction post implementation.
The aim of this mixed methods study was to explore the use of videoconferencing as a means of improving access to health care in care homes; identifying knowledge, attitudes and views towards videoconferencing in Yorkshire and the Humber, England.
The response rate to the survey was limited with only 124/859 (14%) returned. There was difficulty in engaging this sector in research which could be due to time and resource constraints on care staff [
8].
The majority of survey respondents were from private residential care homes. This could explain why, on average, contracted hours for care staff are higher than onsite nursing staff. The higher rate of residential to nursing home responses, may reflect differences in provision of or interest in videoconferencing.
Of the respondents that reported using videoconferencing, 78% came from care home managers in urban geographical locations and 22% were in rural. This is an interesting given that theory suggests videoconferencing would be of most benefit to those geographically isolated [
43] and suggests that the uptake of videoconferencing may be influenced by more than geographical factors [
25].
The average care home accommodated 35 residents, meaning most homes were relatively small in size. The dominant ethnicity of residents in all care homes was British, demonstrating a lack of diversity in terms of language and culture in care homes. Therefore, language and cultural barriers were not as pertinent as those in other studies [
14].
The most frequently accessed health care services were face to face services, with respondents’ reporting using out of hours and ICT services less frequently. This may indicate that there is a lack of confidence in using ICT or technology enabled services or concerns over quality of care when using ICT services over face-to face services. An alternative explanation may include residents not being comfortable consulting with a health care professional this way; this may be particularly pertinent in residents that have dementia.
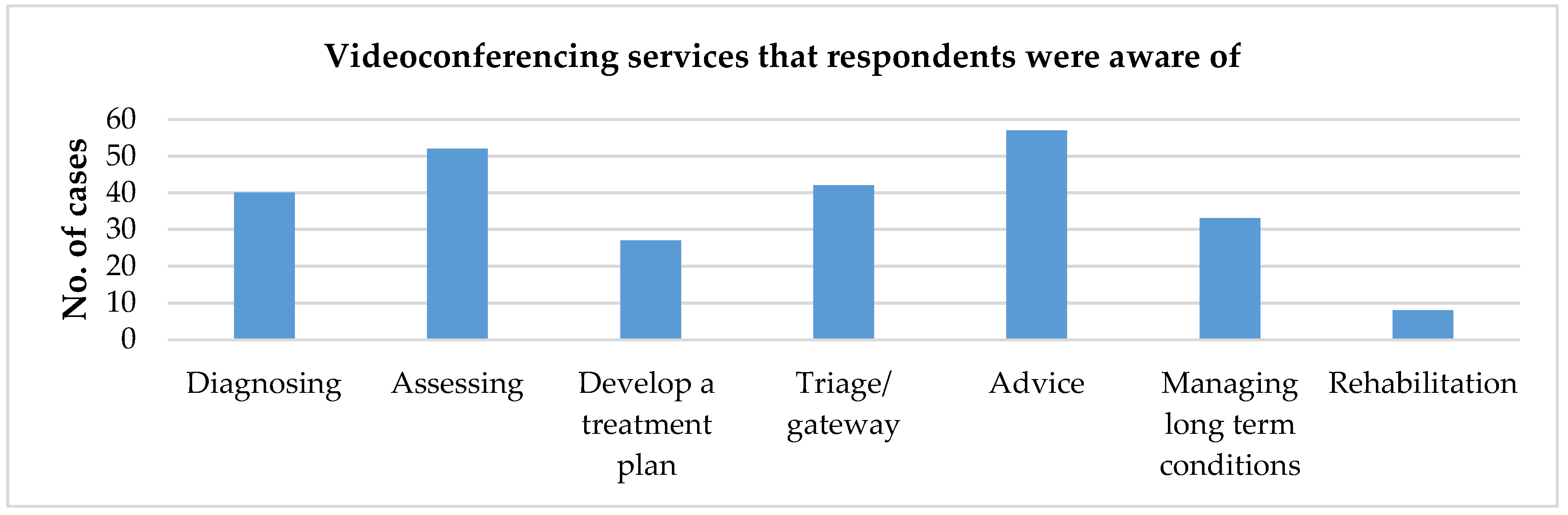
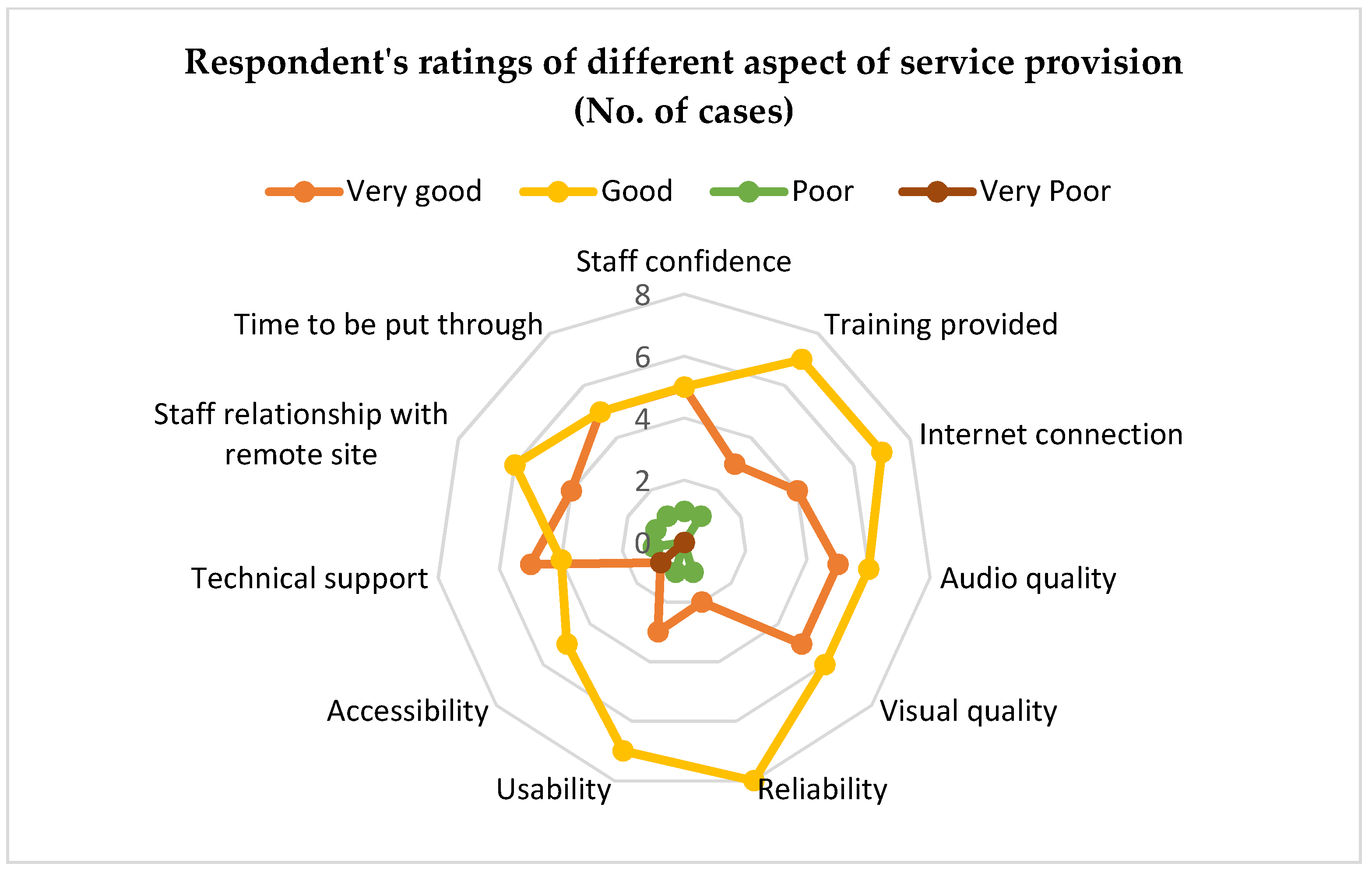
There seemed to be a general awareness among respondents of how important it is to try and reduce hospital admissions, with over half reporting implementing some kind of initiative to try and reduce hospital admissions. Again, the majority of the services relied on face to face contact, with most reporting initiatives that include GP, community services or upskilling care home staff. However, 85% of homes reported having access to Wi-Fi and over half of respondents reported having heard of videoconferencing as a method of health care provision. This suggests a general distrust of technology or more confidence in traditional practices. Further findings reinforce this, with the majority of respondents stating that they would need to know more before implementing it or that they were not sure videoconferencing would be worthwhile as they already had adequate service provision. Service providers should therefore ensure they effectively disseminate information about their services and allow care homes the opportunity to trial videoconferencing before committing to implementing it. More readily available information with regard to the cost of implementation may also be helpful in encouraging uptake. Where homes had implemented videoconferencing services respondents rated them as being either very good or good, suggesting respondents were more confident in using the technology after implementation.
Respondents reported ‘faster access to services’ as the most likely reason for implementing videoconferencing. Additionally, those who had no experience in using videoconferencing also rated ‘improved quality of care of the residents’ as being a pertinent reason for considering implementing the service. The most likely reason for not implementing the system was reported as ‘residents not comfortable being seen in this way.’ This suggests that if care home managers do not perceive there to be an advantage over other services, perhaps due to the lack of face to face communication, this may hinder uptake and suggests that dissatisfaction with alternative services may drive uptake. Participants ranked ’confidence in using ICT’ as the least important issue, suggesting that confidence in being able to use videoconferencing may not be the biggest barrier to uptake. These findings are congruent with the findings of the qualitative interviews. However, it is important to note that a number of responses were reduced due to respondent error, on reflection, this might have been due to the ranking questions not being sufficiently clear, which may have influenced findings.
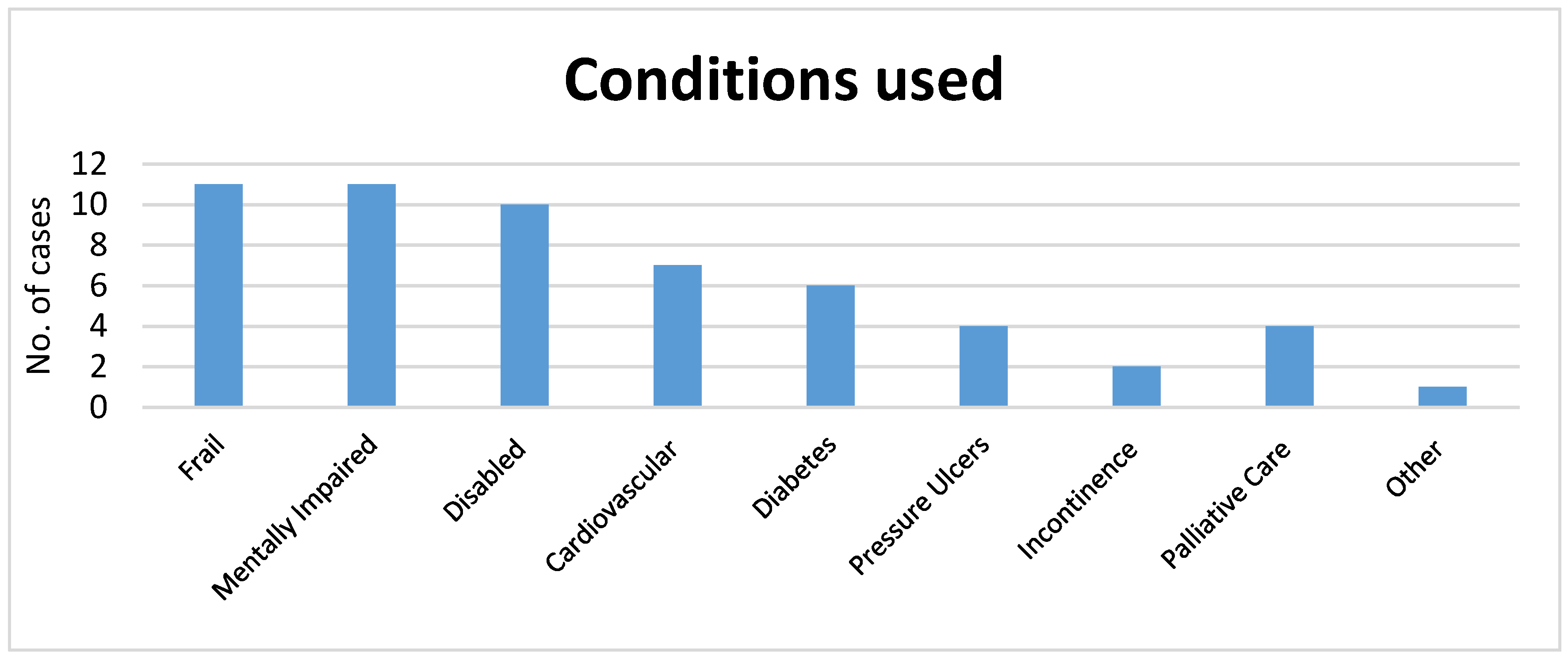
Four respondents reported videoconferencing being very poor for rehabilitation and reported using the service most frequently for residents who were elderly mentally impaired, elderly frail or disabled. As respondents reported as using videoconferencing most frequently out of hours; this suggests that dissatisfaction with currently available out of hours’ services may be a driver to uptake and sustainability of videoconferencing.
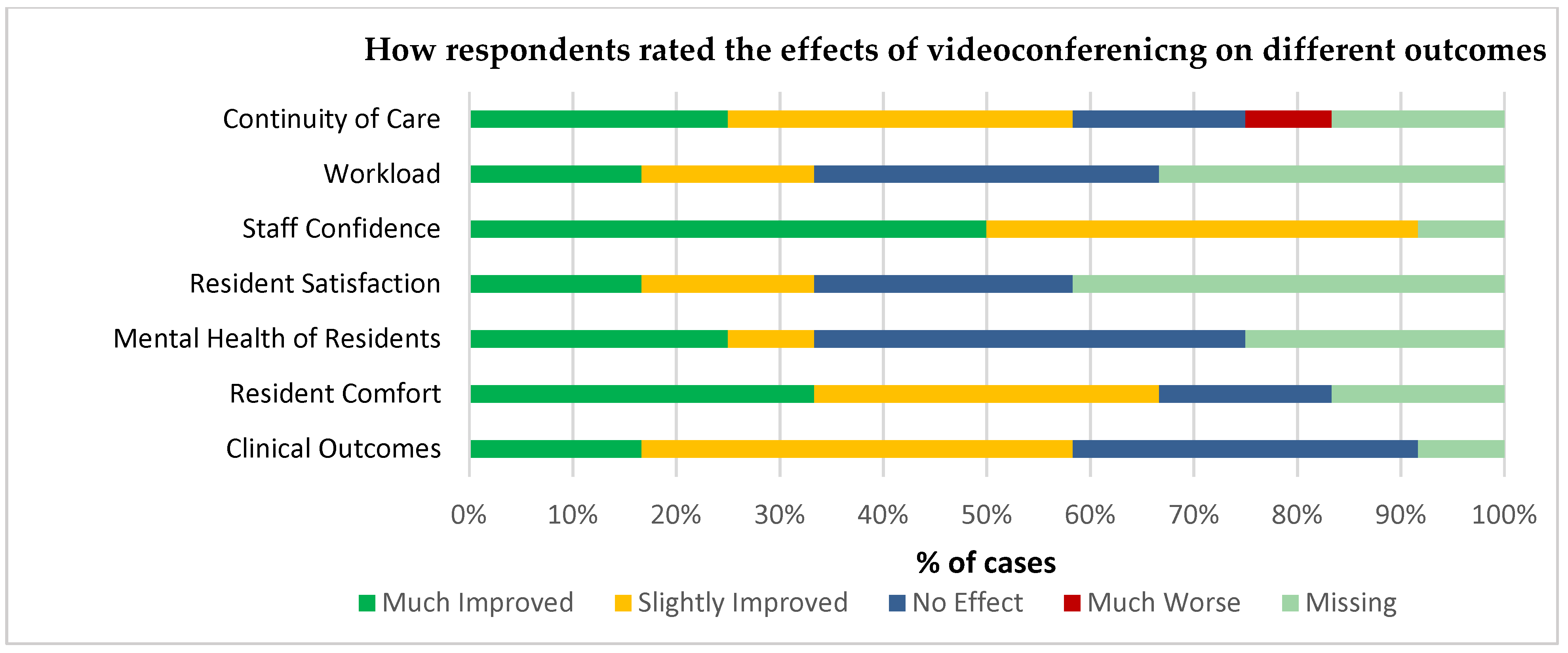
Overall, videoconferencing was rated by those who had experience using it as being ‘very good’ or ‘good,’ meaning that post implementation users are generally happy with the service. With technical support, time to be put through to a member of staff at the remote site and staff confidence being the highest rated factors affecting service provision. This is in line with the above findings that staff confidence and speedier access to services are important in using the system and suggests technical barriers (any difficulty in using videoconferencing that negatively affects the outcome of the call) again may not be a pertinent problem. When reviewing outcomes, managers reported observing the greatest impact in staff confidence, suggesting staff became more confident in managing resident care as a result of having access to the system.
The findings from this survey suggest that greater dissemination of information about the potential uses of and cost of the service may assist in increasing the uptake of videoconferencing. The possibility of being able to trial the system may also be beneficial so that managers and staff have the opportunity to identify how they may be able to implement such a system in ways that will benefit residents and staff. This may be particularly pertinent in homes where staff may be unsure of benefit given their current access to health services.
Further, more in-depth research is required to get a better understanding of the mechanisms impeding and aiding the uptake and sustainability within the care home context, which include aspects of the organizational context such as leadership [
44].