A Review of Assistive Devices in Synovial Joints: Records, Trends, and Classifications
Abstract
1. Introduction
2. Materials and Methods
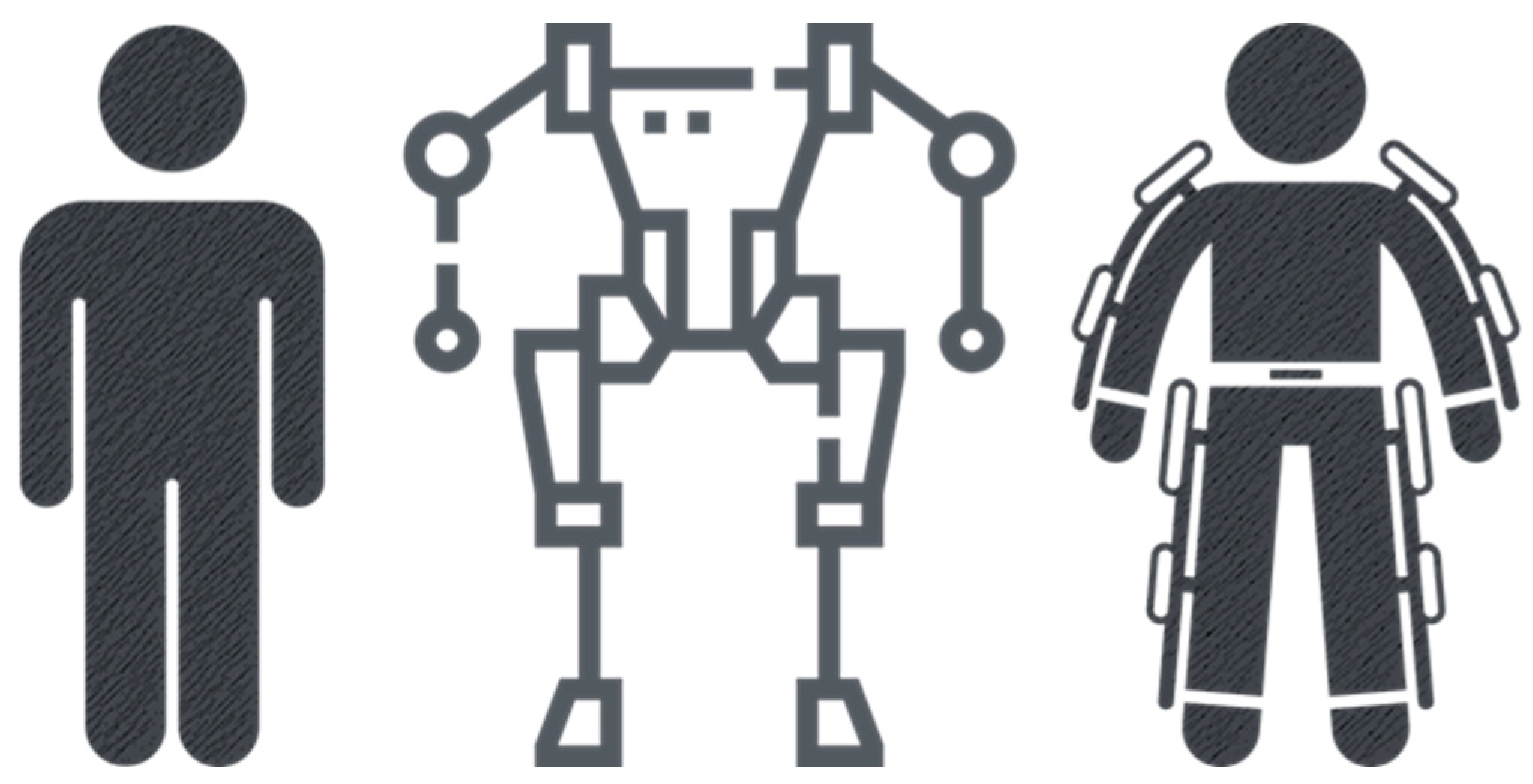
2.1. Splints, Prostheses, Orthoses, and Artificial Exoskeletons
- Splint: It is based on the immobilization of the joint(s).
- Prosthesis: It has two characteristics: to replace the function of amputated areas or to reinforce damaged areas.
- Orthosis: It is based on limiting the range of motion of a single joint.
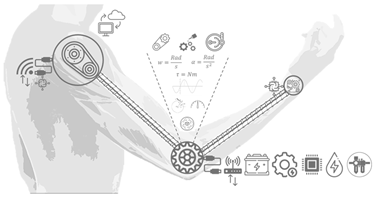
- Artificial exoskeleton: It is based on increasing physical resistance and the smoothness of movements in the joint(s).
2.2. Musculoskeletal System
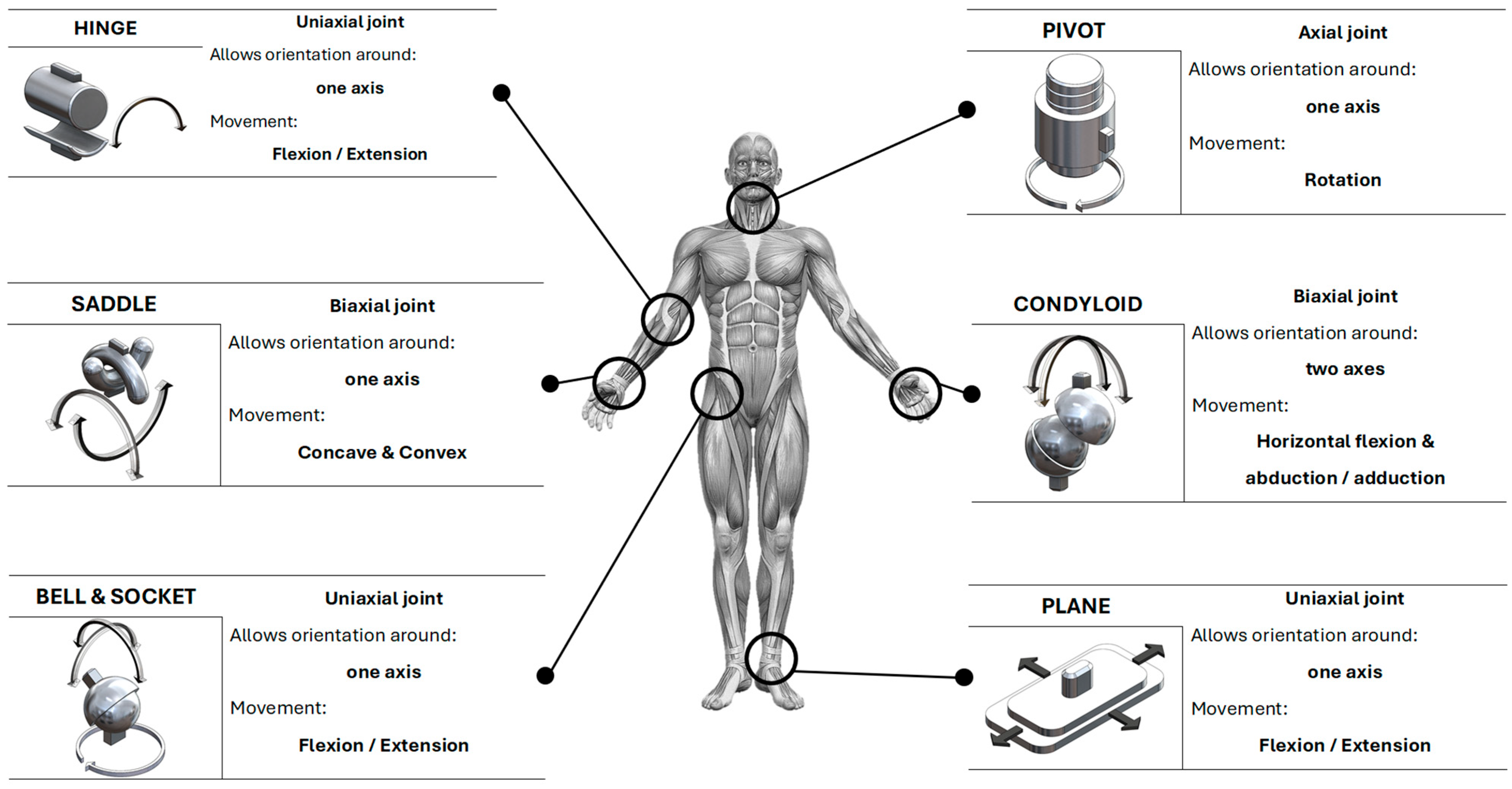
2.3. Joints
3. Results
3.1. Artificial Exoskeletons
3.2. From Biological to Artificial
3.3. Classification of Artificial Exoskeletons
- It must be an external structure to the body.
- It must be parallel to the musculoskeletal system.
- It must assist or enhance the forces and movements of the joints.
3.4. Types of Structure for an Artificial Exoskeleton
3.5. Types of Mobility of an Artificial Exoskeleton
3.6. Type of Power Supply for an Artificial Exoskeleton
3.7. Type of Artificial Exoskeleton System
3.8. Type of Communication of an Artificial Exoskeleton
3.9. Types of Robotic Exoskeleton Construction
- XoMotion (Simon Fraser University): Researchers at Simon Fraser University (SFU) created XoMotion, a cutting-edge robotic exoskeleton. This device enables people with mobility disabilities to stand and walk without additional support. It offers a wide range of activities, including walking, climbing stairs, and squatting. XoMotion uses sensors to mimic the human body’s logic and generate balanced movement [49].
- Stanford Ankle Exoskeleton: Researchers at Stanford University developed an ankle exoskeleton that enables people to walk more efficiently. Training and customization are key to its success. This device connects to the shoe and around the leg, mimicking a motorized exoskeleton. It helps users push forward while walking and maintain balance [50].
- Stanford Wireless Exoskeleton: Another achievement by Stanford University, this is a wireless exoskeleton that increases walking speed by applying torque to the ankle. It facilitates movement during walking and is especially useful for individuals with mobility disabilities [51].
- ATOUN Inc.
- (Nara City, Nara Prefecture, Japan) Exoskeletons for physical task assistance.
- Bioness Inc.
- (Santa Clarita City, CA, USA) Neuromuscular stimulation devices and exoskeletons.
- Bionik Laboratories Corp.
- (Toronto City, ON, Canada) Exoskeletons for medical rehabilitation.
- Comau
- (Grugliasco City, Turin, Italy) Exoskeletons for industrial work assistance.
- Cyberdyne Inc.
- (Tsukuba City, Ibaraki Prefecture, Japan) Robotic exoskeletons for rehabilitation and mobility.
- Ekso Bionics
- (San Rafael City, CA, USA) Exoskeletons for medical and industrial rehabilitation.
- Exy—Empowering People
- (Curitiba City, Paraná, Brazil) Exoskeletons for workplace injury reduction.
- Fourier Intelligence
- (Xiu Pu Lu City, Shanghai, China) Robotic exoskeletons for rehabilitation.
- German Bionic
- (Augsburg City, Bavaria, Germany) Smart exoskeletons for industrial assistance.
- Honda Motor Co., Ltd.
- (Minato City, Tokyo, Japan) Mobility and rehabilitation assistive devices.
- Hyundai Motor Company
- (Seocho-gu City, Seoul, Republic of Korea) Exoskeletons for mobility and industrial tasks.
- INDI
- (Monterrey City, Nuevo León, Mexico) Pediatric exoskeletons for walking assistance.
- Lockheed Martin Corporation
- (Bethesda City, MD, USA) Exoskeletons for military and industrial applications.
- Marsi Bionics
- (Rivas Vaciamadrid City, Madrid, Spain) Exoskeletons for children with neuromuscular disorders.
- Myomo Inc.
- (Burlington City, MA, USA) Exoskeletons for neuromuscular injury support.
- Ottobock
- (Duderstadt City, Niedersachsen, Germany) Exoskeletons and prosthetics for mobility enhancement.
- Panasonic Corporation
- (Kadoma City, Osaka Prefecture, Japan) Exoskeletons for mobility and industrial tasks.
- Parker Hannifin
- (Mayfield Heights City, OH, USA) Exoskeletons for rehabilitation and medical assistance.
- Raytheon Company
- (Arlington City, VA, USA) Exoskeletons for military use.
- ReWalk Robotics
- (Yokne‘am Illit City, Northern District, Israel) Exoskeletons for people with spinal cord injuries.
- Rex Bionics
- (Auckland City, Auckland Region (North Island), New Zealand) Autonomous exoskeletons for people with reduced mobility.
- Sarcos Robotics
- (Salt Lake City, UT, USA) Industrial and military exoskeletons.
- SuitX
- (Emeryville City, CA, USA) Modular exoskeletons for rehabilitation and industry.
- Technaid
- (Arganda del Rey City, Madrid, Spain) Exoskeletons for research and rehabilitation.
- Wandercraft SAS
- (Paris City, France) Autonomous exoskeletons for personal mobility.
4. Discussion
- Structures: Rigid structures are mostly, if not entirely, made from metal materials due to their high resistance to bending and compression. However, these properties are functional for devices that require excessive physical strength, structural resistance, or conditions that could be dangerous for the user. On the other hand, in the medical field, devices for the rehabilitation of limbs or their segments require lower structural resistance, as the movements are slow and do not usually require prolonged or excessive fatigue. Military devices, while requiring strength, may also require physical resistance for walking or lumbar support, where metallic structures are too heavy for transportation over long distances. Materials with low density and high resistance to bending and compression are ideal to replace the rough and heavy metal structures, which not only are heavy but also have high manufacturing and material costs. Polymers, however, would be ideal for devices that do not require high physical demand. Their use could reduce production costs, given their low manufacturing costs and potential for molding or 3D printing, enabling the creation of complex joints where geometry would help create structures that are both stronger and cheaper with quicker construction timelines.
- Energy Consumption: The type of structure impacts energy consumption. Larger structures tend to have greater weight, which translates into higher torque. Large torques require high energy consumption, adding more weight due to the larger actuators. Lighter structures would result in lower torques, allowing the use of smaller actuators, which reduces weight and, in turn, energy consumption. This would be advantageous for mobile devices, as their autonomy would increase significantly with the same battery bank.
- Energy Efficiency: Developing energy-efficient actuators and control systems would be essential for enhancing the autonomy of mobile devices. By minimizing energy consumption through smart power management and lightweight designs, manufacturers can extend the operational time of devices between charges, making them more practical for users.
- Production Times: Structures would be manufactured with ideal characteristics, since designing in CAD environments allows for complex calculations and geometries that metal structures could not achieve, all at lower cost and time. With polymers, geometries would not be an issue as they can be created using molds or additive manufacturing at low production costs and considerably faster manufacturing times than conventional or CNC metal pieces.
- Design Improvements: Future designs could prioritize lightweight materials with high strength-to-weight ratios, such as advanced polymers or composites, which would significantly reduce the overall weight of devices while maintaining structural integrity. This would allow for greater mobility and usability, particularly in applications where prolonged use is required.
- Cost Reduction Strategies: Implementing additive manufacturing techniques, such as 3D printing, could lower production costs and time. This method enables the creation of complex geometries that are difficult or costly to achieve with traditional metal fabrication. By optimizing designs for manufacturability, manufacturers can streamline production processes, reducing material waste and labor costs.
- Integration of AI and Machine Learning: The incorporation of artificial intelligence and machine learning algorithms could enhance the adaptability and functionality of assistive devices. Smart systems could learn from user interactions, adjusting in real-time to optimize support and improve user experience. This would enable devices to provide personalized assistance based on the user’s specific needs and movements, increasing effectiveness during rehabilitation and daily activities.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Musculoskeletal Health. World Health Organization. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions (accessed on 19 February 2025).
- Tomańska, A.; Stawinoga, M.; Gębarowski, T.; Janeczek, M.; Klećkowska-Nawrot, J.; Goździewska-Harłajczuk, K.; Dobrzyński, M. The musculoskeletal anatomy of the hind limbs of the Komodo dragon (Varanus komodoensis, Varanidae). Animals 2025, 15, 35. [Google Scholar] [CrossRef]
- Li, J.; Sun, Z.; Wei, X.; Tan, Q.; He, X. Effect of structure on osteogenesis of bone scaffold: Simulation analysis based on mechanobiology and animal experiment verification. Bioengineering 2024, 11, 1120. [Google Scholar] [CrossRef]
- Mattucci, S.; Speidel, J.; Liu, J.; Kwon, B.K.; Tetzlaff, W.; Oxland, T.R. Basic biomechanics of spinal cord injury: How injuries happen in people and how animal models have informed our understanding. Clin. Biomech. 2019, 64, 58–68. [Google Scholar] [CrossRef]
- André, A.D.; Martins, P. Exoskeletal support devices: Summary of technical aspects. Bioengineering 2023, 10, 1328. [Google Scholar] [CrossRef]
- Garzón, I.; Muñoz-Hurtado, J.; Pereira-Martínez, J.; Ionescu, A.M.; Cardona, J.D.L.C.; Tejada-Casado, M.; Pérez, M.D.M.; Campos, F.; Chato-Astrain, J.; Alaminos, M. Development of new squid gladius biomaterials for corneal tissue engineering. Mar. Drugs 2024, 22, 535. [Google Scholar] [CrossRef]
- Sutton, G.P. Animal biomechanics: A new silent partner in the control of motion. Curr. Biol. 2013, 23, R651–R652. [Google Scholar] [CrossRef]
- Nerlich, A.G.; Zink, A.; Szeimies, U.; Hagedorn, H.G. Ancient Egyptian prosthesis of the big toe. Lancet 2000, 356, 2176–2179. [Google Scholar] [CrossRef]
- Fess, E.E. A history of splinting: To understand the present, view the past. J. Hand Ther. 2002, 15, 97–132. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Fragility Fractures; World Health Organization: Geneva, Switzerland, 2024; Available online: https://www.who.int/news-room/fact-sheets/detail/fragility-fractures#:~:text=In%202019%2C%20there%20were%20178,by%20population%20growth%20and%20ageing (accessed on 19 February 2025).
- A.D.A.M. Medical Encyclopedia. How to Make a Splint. National Library of Medicine, 2023. [About 3 p.]. Available online: https://medlineplus.gov/ency/article/000040.htm (accessed on 19 February 2025).
- A.D.A.M. Medical Encyclopedia. Prosthesis. National Library of Medicine. 2023. Available online: https://medlineplus.gov/ency/article/002286.htm (accessed on 19 February 2025).
- University of Michigan Health. Orthoses (Braces). Rehabilitation Medicine. 2024. Available online: https://www.uofmhealth.org/conditions-treatments/rehabilitation/orthoses#:~:text=An%20orthosis%20is%20a%20device,Muscular%20Dystrophy (accessed on 19 February 2025).
- Velarde, M.A.G.; Rosado, W.M.A.; Ortega, A.B.; Abúndez, A.; Cortés, C.; Colin, J. Lower limb assistance systems: A state of the art. Lat. Am. Appl. Res. 2022, 52, 89–99. [Google Scholar] [CrossRef]
- Urrea, C.; Agramonte, R. Improving exoskeleton functionality: Design and comparative evaluation of control techniques for pneumatic artificial muscle actuators in lower limb rehabilitation and work tasks. Processes 2023, 11, 3278. [Google Scholar] [CrossRef]
- Lim, P.N.; Wang, Z.; Wang, D.; Konishi, T.; Thian, E.S. Development in additive printing for tissue-engineered bone and tendon regeneration. Curr. Opin. Biomed. Eng. 2017, 2, 99–104. [Google Scholar] [CrossRef]
- Elrod, C.S. Chapter 5—Musculoskeletal system. In Acute Care Handbook for Physical Therapists, 4th ed.; Paz, J.C., West, M.P., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2014; pp. 85–122. [Google Scholar] [CrossRef]
- Betts, J.G.; Young, K.A.; Wise, J.A.; Johnson, E.; Poe, B.; Kruse, D.H.; Korol, O.; Johnson, J.E.; Womble, M.; DeSaix, P. Chapter 9.4 Synovial joints. In Anatomy and Physiology; Ingram: La Vergne, TN, USA, 2013; Available online: https://openstax.org/books/anatomy-and-physiology/pages/9-4-synovial-joints (accessed on 19 February 2025).
- Betts, J.G.; Young, K.A.; Wise, J.A.; Johnson, E.; Poe, B.; Kruse, D.H.; Korol, O.; Johnson, J.E.; Womble, M.; DeSaix, P. 9.1 Classification of joints. In Anatomy and Physiology; Ingram: La Vergne, TN, USA, 2013; Available online: https://openstax.org/books/anatomy-and-physiology/pages/9-1-classification-of-joints (accessed on 19 February 2025).
- Kapandji, A.I. Joint Physiology: Commented Diagrams of Human Mechanics, Upper Limb, 6th ed.; Editorial Medica Panamericana: Madrid, Spain, 2006; Available online: https://www.medicapanamericana.com/es-MX/libros/fisiologia-articular-tomo-1-miembro-superior-tomo-1-miembro-superior-6a-edicion (accessed on 19 February 2025).
- Kapandji, A.I. Joint Physiology: Commented Diagrams of Human Mechanics, Lower Limb, 6th ed.; Editorial Medica Panamericana: Madrid, Spain, 2012; Available online: https://www.medicapanamericana.com/es-MX/libros/fisiologia-articular-tomo-2-miembro-inferior-tomo-2-miembro-inferior (accessed on 19 February 2025).
- Kapandji, A.I. Joint Physiology: Commented Diagrams of Human Mechanics, Trunk and Spine, 6th ed.; Editorial Medica Panamericana: Madrid, Spain, 2012; Available online: https://www.medicapanamericana.com/es-MX/libros/fisiologia-articular-tomo-3-tronco-y-raquis-tomo-3-tronco-y-raquis-6a-edicion (accessed on 19 February 2025).
- Kong, W.; Sessa, S.; Zecca, M.; Takanishi, A. Anatomical calibration through post-processing of standard motion tests data. Sensors 2016, 16, 2011. [Google Scholar] [CrossRef]
- s.v. “splint, n”. In Oxford English Dictionary; Oxford University Press eBooks: Oxford, UK, 2023. [CrossRef]
- s.v. “prosthesis, n”. In Oxford English Dictionary; Oxford University Press eBooks: Oxford, UK, 2023. [CrossRef]
- s.v. “orthosis, n”. In Oxford English Dictionary; Oxford University Press eBooks: Oxford, UK, 2024. [CrossRef]
- s.v. “exoskeleton, n”. In Oxford English Dictionary; Oxford University Press eBooks: Oxford, UK, 2024. [CrossRef]
- Ellis, H. The early days of splints and splinting. J. Perioper. Pract. 2011, 21, 251–252. [Google Scholar] [CrossRef]
- Gray, B.; Santy-Tomlinson, J. The Thomas’ splint: Application and patient care. Int. J. Orthop. Trauma Nurs. 2018, 30, 20–22. [Google Scholar] [CrossRef]
- Forssmann, A. Sophistication in Ancient Egypt: A 3000-year-old prosthesis. In National Geographic History; National Geographic Partners: Washington, DC, USA, 2017; Available online: https://historia.nationalgeographic.com.es/a/sofisticacion-antiguo-egipto-protesis-hace-3000-anos_11639 (accessed on 19 February 2025).
- Genêt, F.; Schnitzler, A.; Mathieu, S.; Autret, K.; Théfenne, L.; Dizien, O.; Maldjian, A. Orthotic devices and gait in polio patients. Ann. Phys. Rehabil. Med. 2010, 53, 51–59. [Google Scholar] [CrossRef]
- Yagn, N. Apparatus for Facilitating Walking, Running, and Jumping. United States Patent Office. United States Patent 420,179, 28 January 1890. Available online: https://patents.google.com/patent/US420179A/en (accessed on 19 February 2025).
- Guan, X.; Ji, L.; Wang, R. Development of exoskeletons and applications in rehabilitation. MATEC Web Conf. 2016, 40, 02004. [Google Scholar] [CrossRef]
- Splint. In Cambridge Dictionary; Cambridge University Press: Cambridge, UK, 2024; Available online: https://dictionary.cambridge.org/us/dictionary/english/splint (accessed on 19 February 2025).
- Prosthesis. In Cambridge Dictionary; Cambridge University Press: Cambridge, UK, 2024; Available online: https://dictionary.cambridge.org/us/dictionary/english/prosthesis?q=Prosthesis (accessed on 19 February 2025).
- Orthosis. In Cambridge Dictionary; Cambridge University Press: Cambridge, UK, 2024; Available online: https://dictionary.cambridge.org/us/dictionary/english/orthosis?q=Orthosis (accessed on 19 February 2025).
- Exoskeleton. In Cambridge Dictionary; Cambridge University Press: Cambridge, UK, 2024; Available online: https://dictionary.cambridge.org/us/dictionary/english/exoskeleton (accessed on 19 February 2025).
- Ferula. Diccionario Médico. (s. f.). Available online: https://www.cun.es/diccionario-medico/terminos/ferula (accessed on 19 February 2025).
- splint. In En Merriam-Webster Dictionary; Merriam-Webster: Springfield, MA, USA, 2025; Available online: https://www.merriam-webster.com/dictionary/splint (accessed on 19 February 2025).
- Vargas Negrín, F. Indications of orthoses in primary care. FMC—Contin. Med. Educ. Prim. Care 2017, 24, 465–478. [Google Scholar] [CrossRef]
- Manuel, C.B.J. Biomechanics in AFOs: Podopediatric AFOs. Span. J. Podiatry 2012, 23, 184–194. [Google Scholar]
- National Institute for Occupational Safety and Health (INSST). NTP 1162: Exoskeletons I: Definition and Classification. INSST Portal. 2021. Available online: https://www.insst.es/documentacion/colecciones-tecnicas/ntp-notas-tecnicas-de-prevencion/34-serie-ntp-numeros-1152-a-1168-ano-2021/ntp-1162-exoesqueletos-i-definicion-y-clasificacion (accessed on 19 February 2025).
- Arroyave-Tobon, S.; Drapin, J.; Moretto, P.; Linares, J.-M. Design features of the kinematic chain of the ant exoskeleton. Procedia CIRP 2023, 119, 855–860. [Google Scholar] [CrossRef]
- Crea, S.; Beckerle, P.; De Looze, M.; De Pauw, K.; Grazi, L.; Kermavnar, T.; Masood, J.; O’Sullivan, L.W.; Pacifico, I.; Rodríguez-Guerrero, C.; et al. Occupational exoskeletons: A roadmap toward large-scale adoption. Methodology and challenges of bringing exoskeletons to workplaces. Wearable Technol. 2021, 2, e11. [Google Scholar] [CrossRef] [PubMed]
- Miao, Q.; Zhang, M.; Cao, J.; Xie, S.Q. Reviewing high-level control techniques on robot-assisted upper-limb rehabilitation. Adv. Robot. 2018, 32, 1253–1268. [Google Scholar] [CrossRef]
- Preethichandra, D.M.G.; Piyathilaka, L.; Sul, J.-H.; Izhar, U.; Samarasinghe, R.; Arachchige, S.D.; de Silva, L.C. Passive and active exoskeleton solutions: Sensors, actuators, applications, and recent trends. Sensors 2024, 24, 7095. [Google Scholar] [CrossRef] [PubMed]
- Denby, C.; Stone, T. Chapter 18—Neurological measurement. In Clinical Engineering, 2nd ed.; Taktak, A., Ganney, P.S., Long, D., Axell, R.G., Eds.; Academic Press: Cambridge, MA, USA, 2020; pp. 309–319. [Google Scholar] [CrossRef]
- Zhao, Y.; He, F.; Guo, Y. EEG signal processing techniques and applications. Sensors 2023, 23, 9056. [Google Scholar] [CrossRef] [PubMed]
- Human In Motion Robotics—Intelligent Innovation in Human Motion. 2014. Available online: https://humaninmotion.com/ (accessed on 19 February 2025).
- Ankle Exoskeleton Enables Faster Walking. Stanford Report, Stanford University. 2021. Available online: https://news.stanford.edu/stories/2021/04/ankle-exoskeleton-enables-faster-walking (accessed on 19 February 2025).
- Exoskeleton Makes Walking Faster, Less Tiring. Stanford Report, Stanford University. 2022. Available online: https://news.stanford.edu/stories/2022/10/exoskeleton-makes-walking-faster-less-tiring (accessed on 19 February 2025).



| Section | Articulation | Segments | Location | |
|---|---|---|---|---|
| Upper limb |  | 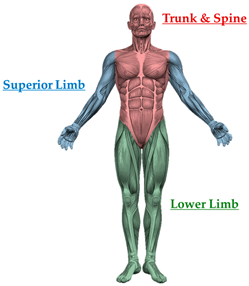 |  | |
| Trunk and spine | 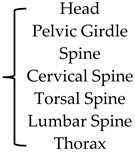 | |||
| Lower limb | 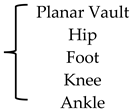 | |||
| (a) | (b) |
| Articulation | Mobility (Axis) | Description |
|---|---|---|
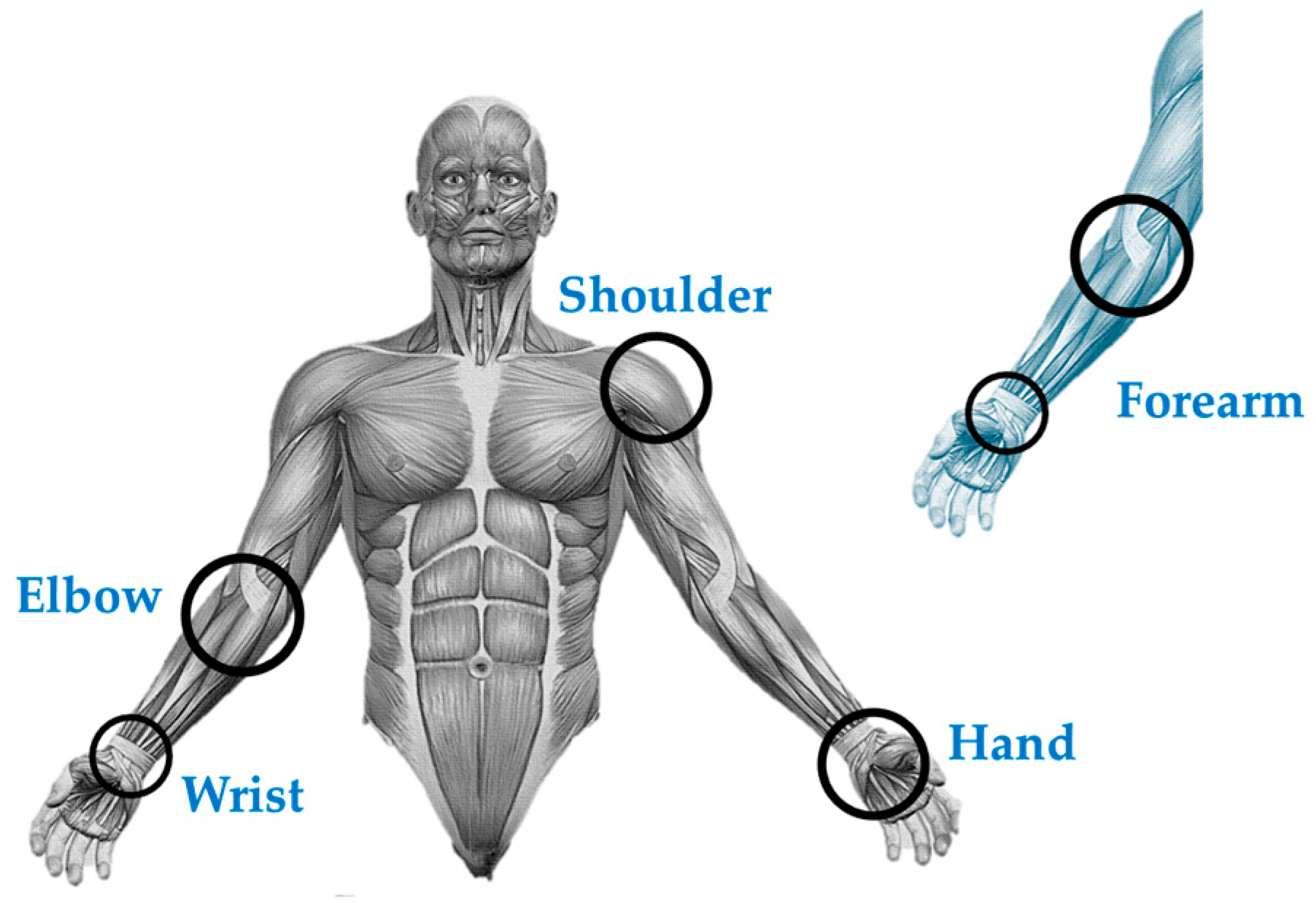
| Shoulder | 3 | This joint is formed between the humerus, scapula, and clavicle [20] (pp. 2–13). Superficial muscles, such as the deltoid and trapezius, along with deep muscles (supraspinatus, infraspinatus, teres minor, and subscapularis), reinforce this joint. The shoulder is crucial for movements such as abduction, adduction, flexion, and rotation of the arm [20] (pp. 13–74). |
| Arm | - | The humerus is the main bone in this region. The arm muscles include the biceps brachii, brachialis, and coracobrachialis [20] (pp. 102–145). These muscles are innervated by the brachial plexus and enable movements such as elbow flexion and extension [20] (pp. 102–145). |
| Elbow | 1 | The elbow joint involves three bones: the humerus, radius, and ulna [20] (pp. 76–90). It allows for flexion, extension, pronation, and supination movements. The muscles of the anterior compartment (coracobrachialis, brachialis, biceps brachii) and posterior compartment (triceps brachii) are responsible for these movements [20] (pp. 92–102). |
| Forearm (Elbow–Wrist) | 1 | In this region, the radius and ulna are the main bones [20] (pp. 104–132). The radial, ulnar, and median nerves innervate the muscles of the forearm. These muscles are divided into anterior compartments (superficial, intermediate, and deep) and posterior compartments (superficial and deep) [20] (pp. 134–144). |
| Wrist | 2 | The wrist joint, also known as the radiocarpal joint, is an anatomical structure that connects the bones of the forearm (ulna and radius) with the carpal bones, allowing the connection between the forearm and the hand [20] (pp. 146–150). The joint between the distal radius and the pyramidal bone is indirect and facilitated by the biconcave articular disk, enabling flexion, extension, adduction, and abduction movements [20] (pp. 150–194). |
| Hand | 25 | The hand consists of several carpal bones (scaphoid, lunate, pyramidal, pisiform, trapezium, trapezoid, capitate, and hamate), five metacarpals, and phalanges [20] (pp. 198–234). The radial, ulnar, and median nerves also innervate the muscles of the hand, such as the thenar, hypothenar, and metacarpal groups [20] (pp. 238–340). |
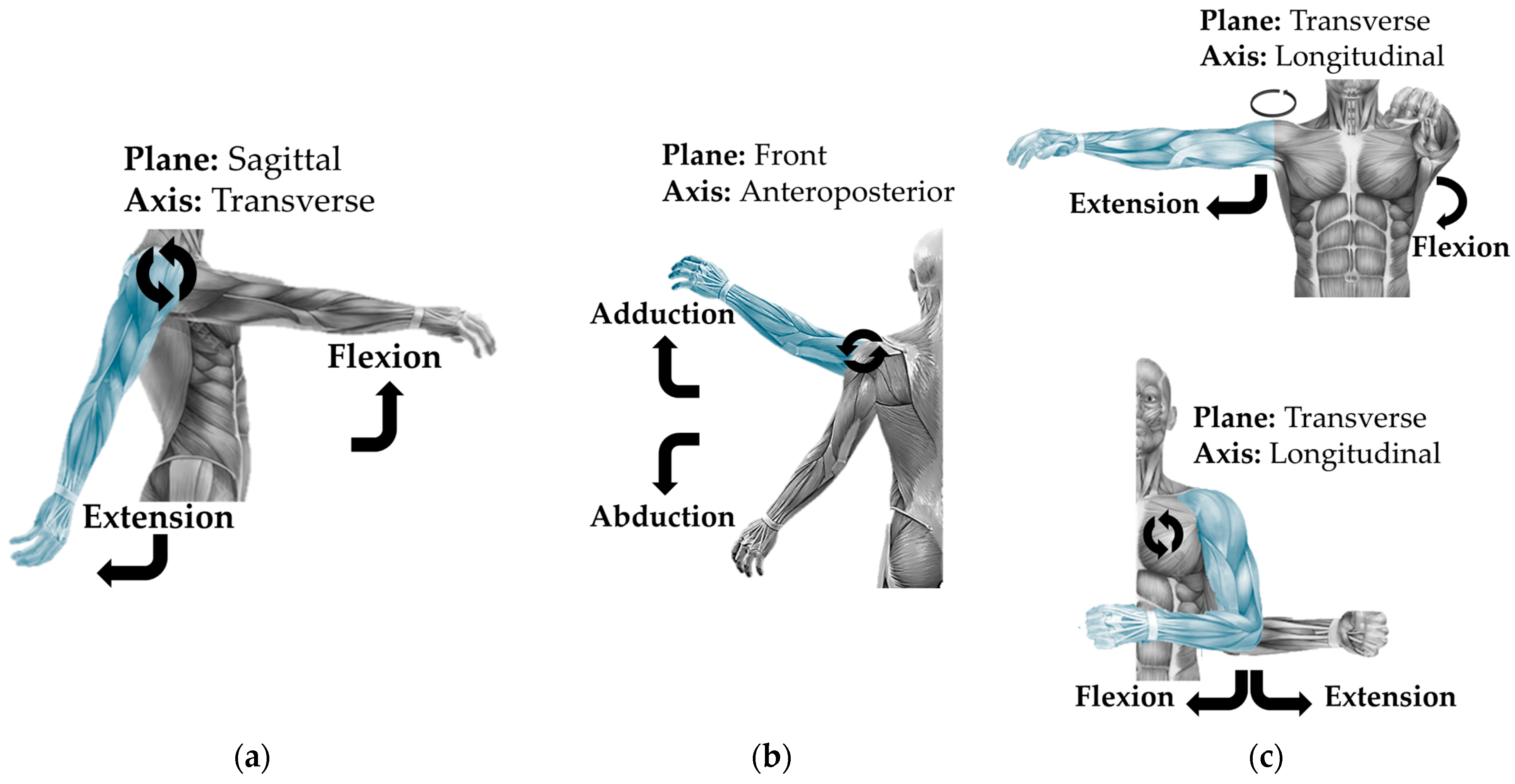
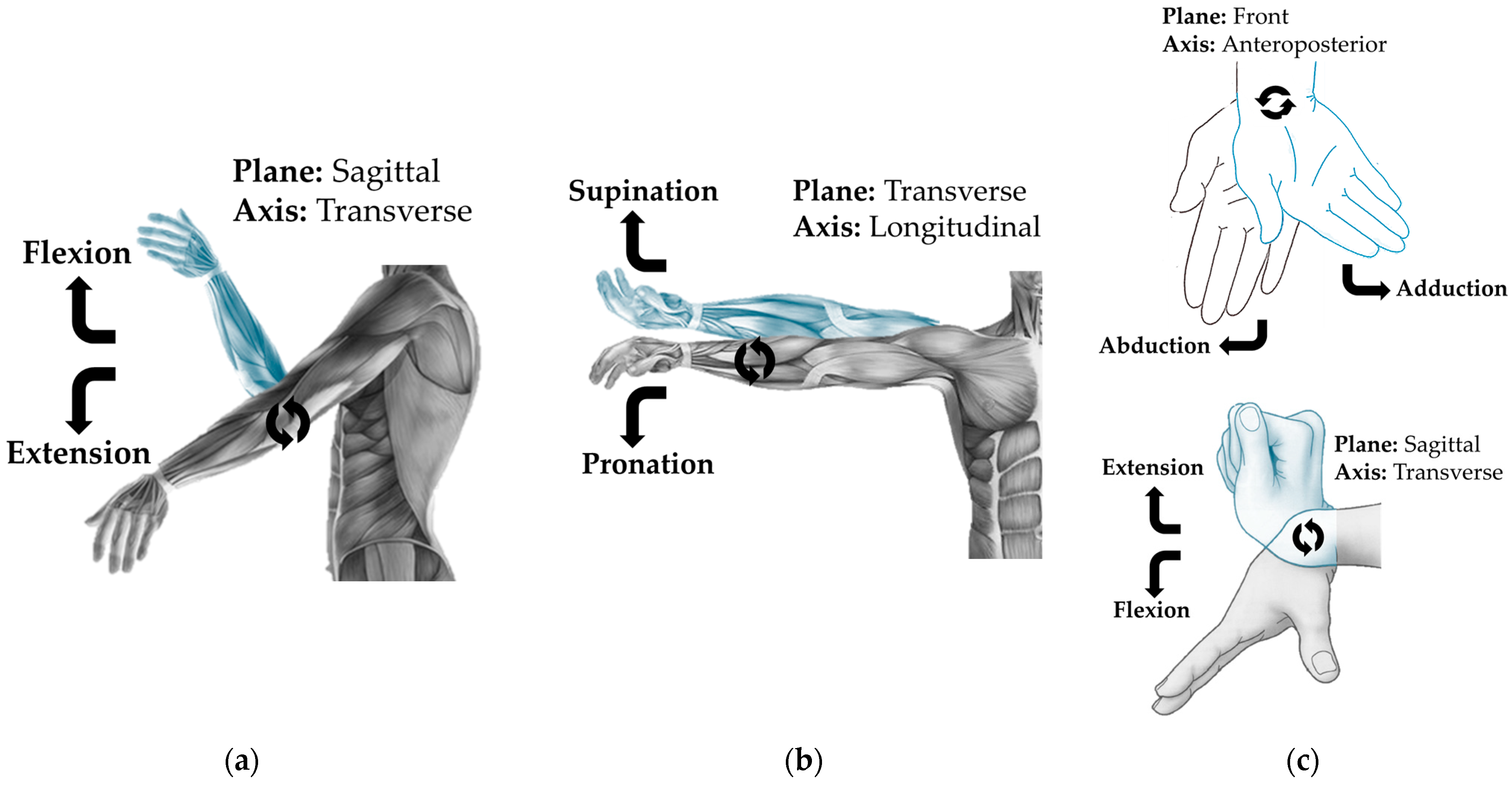
| Articulation | DOF | Axis | Plane | Characteristic Movement | Figure | |
|---|---|---|---|---|---|---|
| Shoulder | 3 | Transverse | Sagittal | F/E | Figure 4a | |
| Anteroposterior | Frontal | Ab/Ad | Figure 4b | |||
| Longitudinal | Transverse | F/E Horizontal | Figure 4c | |||
| Elbow | 1 | Transverse | Sagittal | F/E | Figure 5a | |
| Forearm | 1 | Longitudinal | Transverse | P/S | Figure 5b | |
| Wrist | 2 | Transverse | Sagittal | F/E | Figure 5c | |
| Anteroposterior | Frontal | Ab/Ad | ||||
| Hand | 25 | Finger | DOF | Axis | Characteristic movement | Finger movements produce excessive volume of content. The book A. I. Kapandji is recommended: Physiology, upper limb [20] (pp. 198–340). |
| Thumb | 5 | Interphalangeal | F/E | |||
| Metacarpophalangeal | F/E—Ab/Ad | |||||
| Carpometacarpal | F/E—Ab/Ad | |||||
| Index Middle Ring Pinky | 5 | Distal Interphalangeal | F/E | |||
| Proximal | F/E | |||||
| Metacarpophalangeal | F/E—Ab/Ad | |||||
| Carpometacarpal | F/E | |||||
| Articulation | Mobility (Axis) | Description |
|---|---|---|
| Hip | 3 | It is a type of ball-and-socket joint that connects the hip bone (formed by the ilium, ischium, and pubis) with the femur [21] (pp. 14–32). The joint capsule is strong and fibrous, surrounding the joint. Movements include flexion, extension, abduction, adduction, and rotation [21] (pp. 34–72). |
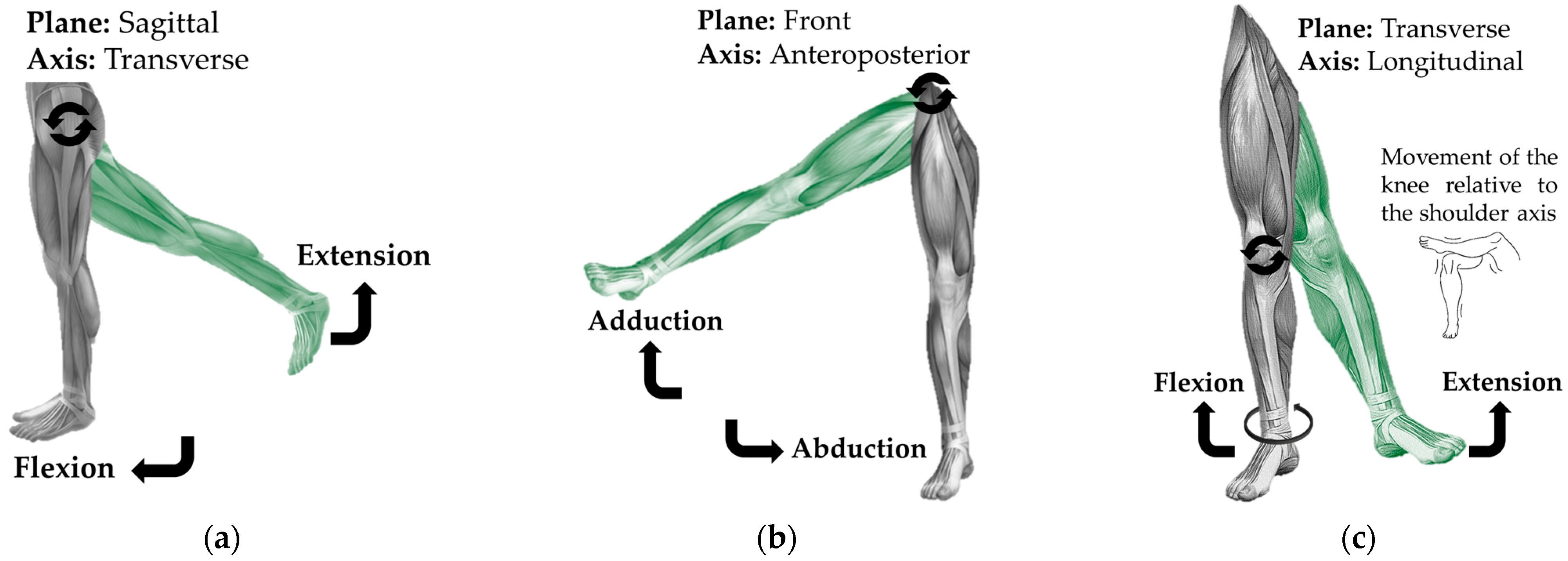
| Knee | 1 | It is a synovial joint that connects the femur with the tibia and the patella. The articular surfaces are the femoral condyles and the tibial surfaces [21] (pp. 76–86). The main movements are flexion and extension. In terms of planes and axes, flexion and extension occur in the sagittal plane around the transverse axis [21] (pp. 88–156). |
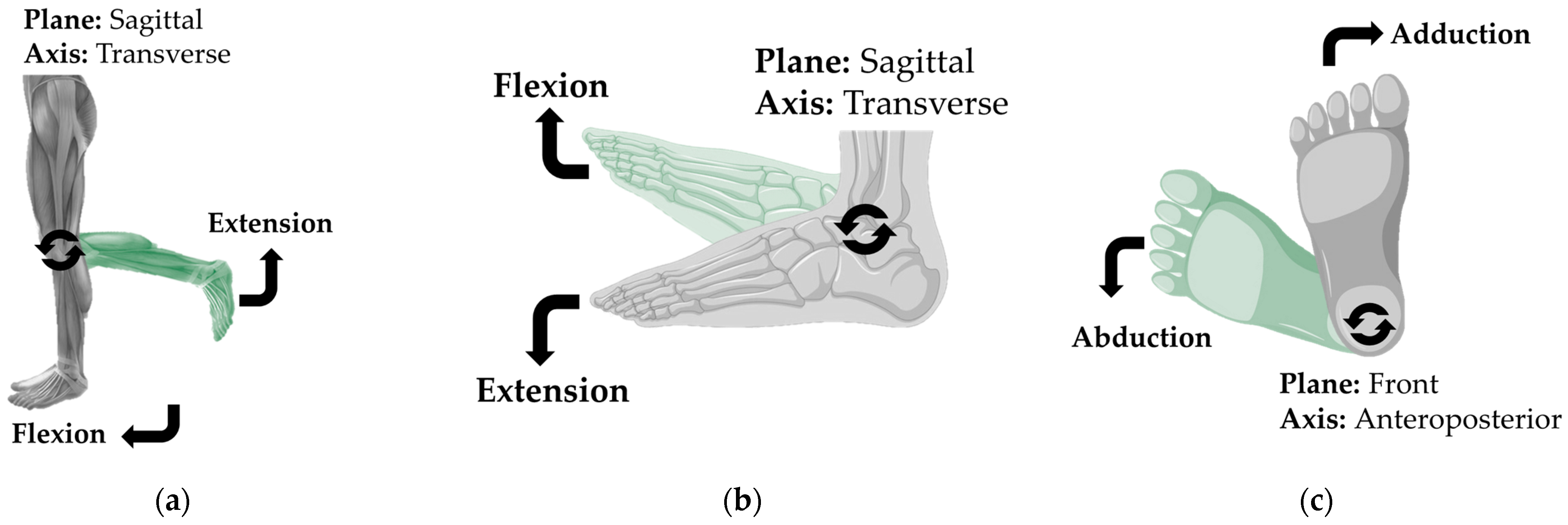
| Ankle | 2 | It is a joint that connects the tibia and fibula with the talus. The articular surfaces are the tibiofibular mortise and the talus [21] (pp. 160–162). Movements include plantar flexion (pointing the toes downward) and dorsiflexion (lifting the toes). These movements occur in the sagittal plane around the transverse axis [21] (pp. 164–174). |
| Foot | 33 | These include the tarsometatarsal, metatarsophalangeal, and interphalangeal joints [21] (pp. 178–182). These allow movements such as flexion, extension, abduction, and adduction of the toes [21] (pp. 184–224). |
| Articulation | DOF | Axis | Plane | Characteristic Movement | Figure | ||
|---|---|---|---|---|---|---|---|
| Hip | 3 | Transverse | Sagittal | F/E * | Figure 6a | ||
| Anteroposterior | Frontal | Ab/Ad * | Figure 6b | ||||
| Longitudinal | Transverse | F/E Horizontal | Figure 6c | ||||
| Knee | 1 | Transverse | Sagittal | F/E—P/S * | Figure 7a | ||
| Ankle | 2 | Transverse | Sagittal | Fd/Fp * | Figure 7b,c | ||
| Longitudinal | Transverse | I/E * | |||||
| Foot | 33 | Articulation | DOF | Axis | Characteristic movement | Finger movements produce excessive volume of content. The book by A. I. Kapandji is recommended: Physiology, upper limb [21] (pp. 178–224). | |
| Talocrural | 2 | Transverse | Fd/Fp | ||||
| Talocalcaneonavicular | 2 | Anteroposterior | I/E | ||||
| Calcaneocuboid | 1 | Anteroposterior | MD * | ||||
| Toes | 30 | ||||||
| Big | 1 | Interphalangeal | F/E—Ab/Ad | ||||
| Second, Third, Fourth, Fifth | 2 | Proximal | F/E—Ab/Ad | ||||
| Distal | F/E—Ab/Ad | ||||||
| Device | Function | Application | Figure |
|---|---|---|---|
| Splint | The angle of the joint at which the device is placed will remain in that position until the device is removed. | Medical and Civil | 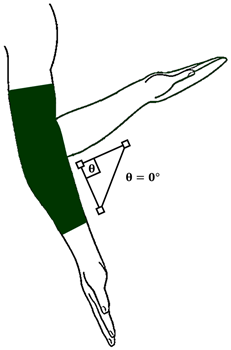 |
| Prosthesis | It replaces or adapts artificial devices in segments with fractures or amputations, substituting the function of the bone, muscle, or joint, or all of them. | Medical and Civil | 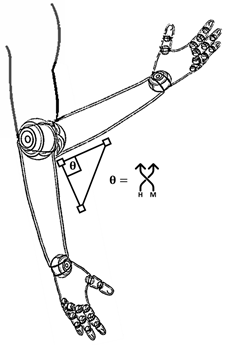 |
| Orthosis | It allows the joint to move within a set range. It can completely stop the movement of the joint. | Medical and Civil | 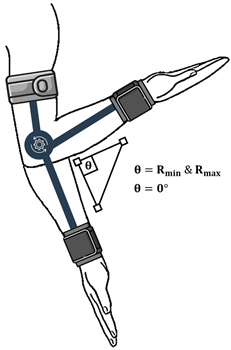 |
| Artificial exoskeleton | It replaces the function of muscles and joints with mechanical or powered movement. It moves within the biomechanical range of the limb or a smaller range. It allows ergonomic mobility or immobility of the joint. | Medical, Military, Industrial and Civil |  |
| Section | Device | Description |
|---|---|---|
| Origin of the Word | Splint | The term “splint” likely originates from multiple sources: Middle Low German, referring to a thin piece of iron; Middle Dutch cognate “splinter”; or Swedish, meaning a wooden nail or wedge. All interpretations align with the concept of a plate or strip applied to the skin, typically made from splinters of metal or wood [24]. |
| Prosthesis | “Prosthesis” has a history spanning thousands of years, with roots in ancient Egypt and Greece, and continues to evolve today with artificial devices for body repair. The term derives from Late Latin, from the Greek “prosthesis,” meaning “to add,” from “prostithenai” (to add to) and “tithenai” (to place) [25]. | |
| Orthosis | Compared to earlier devices like splints, “orthosis” is relatively modern, having been in use for only a few decades. It comes from the Greek “orthōsis,” meaning “to straighten,” derived from “orthoun” (to straighten) [26]. | |
| Exoskeleton | The term “exoskeleton” refers to any hardened external structure, such as the shells of crustaceans or the plates of fish and reptiles, particularly when bone-like. It is derived from the Greek “exo-” (outside) and “skeleton,” and is grounded in zoological terminology [27]. |
| Section | Device | Year |
|---|---|---|
| First Record | Splint | 1325 [24] |
| Prosthesis | 1550 [25] | |
| Orthosis | 1958 [26] | |
| Artificial exoskeleton | 1839 [27] |
| Section | Device | Description |
|---|---|---|
| First Appearance | Splint | In the 20th century, during excavations in Egypt, fractures from 5000 years ago were found, bound with bark tablets, wrapped in linen, and secured with bandages. Surgeon Percival Pott standardized the immobilization splint, known as Pott’s splint [28]. Later, the Thomas splint emerged to immobilize the lower limb in cases of fractures and chronic bone diseases. During World War I, the splint evolved, and plaster of Paris was used, becoming known as the Tobruk splint, which remains the most used today [29]. |
| Prosthesis | The University of Basel found a wooden prosthesis belonging to the foot of the daughter of an Egyptian priest in a female burial at Tomb Tebana 95, dating back 3000 years [30]. | |
| Orthosis | The appearance of the first orthotic device dates to the earliest civilizations, when rudimentary forms of splints and supports were used. Over time, orthotics has evolved to become a highly specialized field of medicine, with increasingly complex devices tailored to the individual needs of patients. F. Genêt, F. et al. (2010) describes the importance that a device called an orthosis had in the mid-twentieth century, a disease “Heine–Medin syndrome” (Poliomyelitis) and the poliovirus frequently attacked the respiratory systems and caused paralysis of the upper and lower limbs of those infected. As a result, devices called leather and steel orthoses became quite popular [31]. | |
| Artificial exoskeleton | The oldest exoskeleton-like device known was developed in 1890 by Russian engineer Nicholas Yagn with a patent under the name “Apparatus for facilitating walking, running, and jumping [32].” It was not until 1960 that the first mobile machine with anthropomorphic movements appeared: the Hardiman, a device developed by General Electric and the U.S. government [33]. |
| Section | Device | Description |
|---|---|---|
| Definition | Splint | The word “splint” comes from the noun “to splint.” The Cambridge Dictionary defines “to splint” as an object made of rigid or flexible material used to immobilize an area with injury or fracture [34]. |
| Prosthesis | The Cambridge Dictionary defines “prosthesis” as the science or part of medicine that deals with artificial body parts [35]. | |
| Orthosis | The Cambridge Dictionary defines “orthosis” as a device made to support an injured or malformed part of the body [36]. | |
| Artificial exoskeleton | In biological terms. The Cambridge Dictionary defines “exoskeleton” as a hard outer layer that covers, supports, and protects an invertebrate animal [37]. In medical or military terms. The Cambridge Dictionary defines “exoskeleton” as a suit that supports the body or part of it. It is used by people with injuries to help them walk or by soldiers to help them carry heavy equipment [37]. |
| Section | Device | Description |
|---|---|---|
| Utility | Splint | According to the University of Navarra Clinic [38] and the medical dictionary [39], a splint is used to immobilize a fractured, dislocated, or paralyzed body part, which should be kept at rest, in a proper position, or unloaded, as is the case with inflammatory joint diseases, paralysis, dislocation, or fractures. |
| Prosthesis | According to Standard UNE 11-909-90/1, adopted from ISO 8549/1, a prosthesis is an external device used to replace, either partially or entirely, a deficient or absent limb segment [40]. | |
| Orthosis | According to Standard UNE 11-909-90/1, adopted from ISO 8549/1, an orthosis is any device applied externally to the human body, used to modify the structural or functional characteristics of the neuromusculoskeletal system, with the purpose of maintaining, improving, or recovering function [41]. | |
| Artificial exoskeleton | According to Standards NTP 1162 and NTP 1163 [42]. Exoskeletons I and II, an exoskeleton is a portable external device placed on the user’s body, used to increase ergonomic intervention capabilities and improve working conditions, particularly concerning physical load. |
| Device | Type | Description |
|---|---|---|
| Exoskeletons Artificial | Structure | Rigid Flexible |
| Mobility | Mobile Fixed Supported | |
| Power | Electric Hydraulic Pneumatic No power | |
| Communication | Control panel Electromyography (EMG) Electroencephalogram (EEG) No communication | |
| System | Passive Semi-Passive Semi-Active Active | |
| Construction | Private Public |
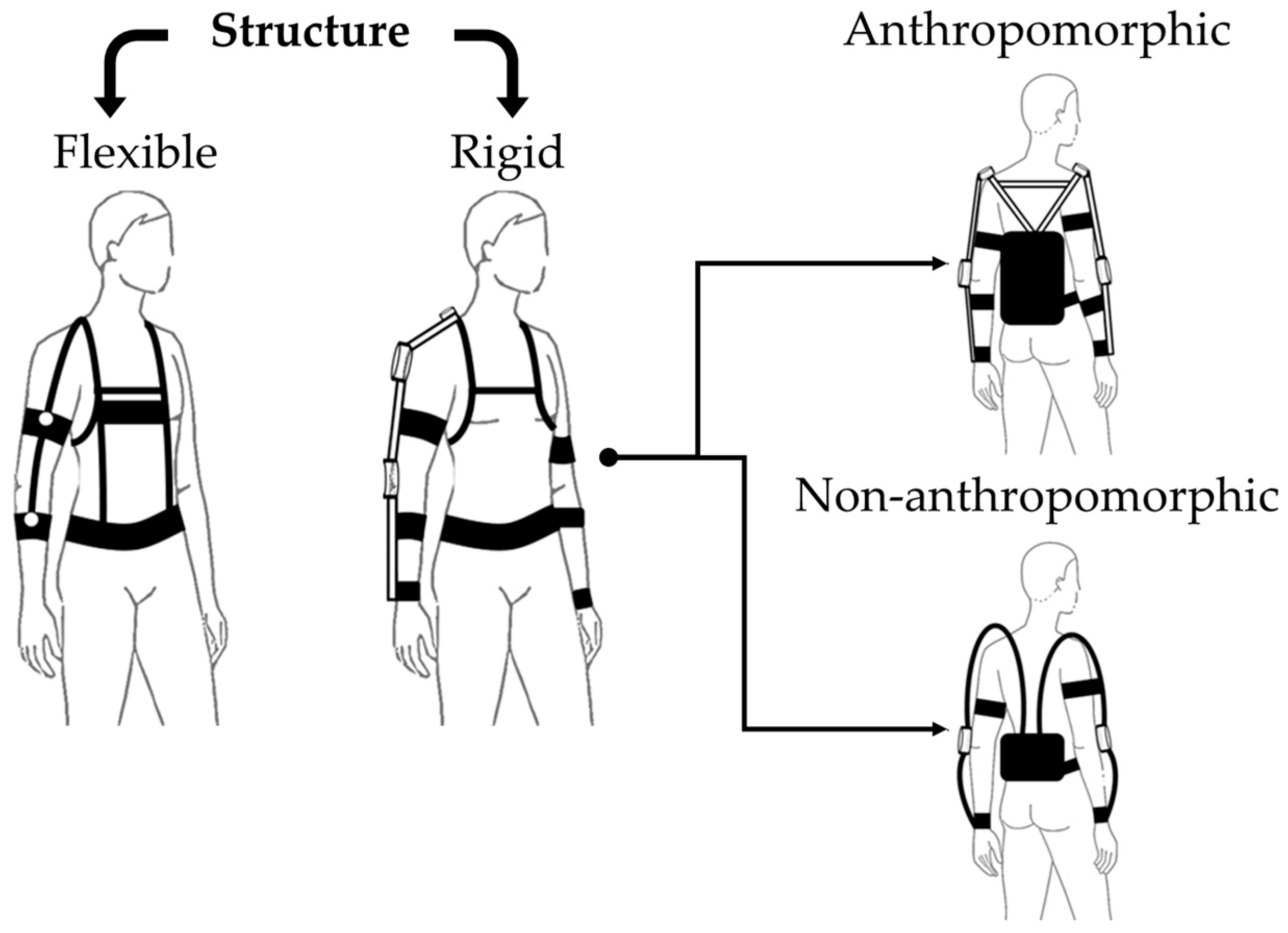
| Structure | Description | Type | Description |
|---|---|---|---|
| Rigid [44] | It is built with low-flexibility links: metals, polymers, among others. It provides support and stability. These are designed to resist mechanical loads and maintain the integrity of the device. | Anthropomorphic | Replicates human joints and proportions. |
| No anthropomorphic | Prioritizes efficiency and adaptation to perform tasks. | ||
| Flexible | It is composed of cables or elastic bands. It provides movement adaptability since it is not a heavy structure. They are designed to collect information or assist with posture during prolonged periods in terms of physical endurance. | This does not apply | This does not apply |
| Mobility | Description |
|---|---|
| Free | This type of mobility has no displacement limits. Since the structure is placed on the user, it allows the user to move with it. As it is user-dependent, a battery bank must be implemented if required, or a power supply line, which would limit the user to an area with a range determined by the length of the power system. |
| Fixed | This type of mobility represents a structure fixed to the ground or a wall. The links are supported by the base, causing the user to have no direct interaction with the structure, only with the movements. The displacement is restricted to the area where it is installed, providing greater stability and power, as it may be connected to a power supply source. |
| Anchored | This type of mobility suspends the structure with harnesses or cables on a fixed or mobile rail. This allows externally assisted displacement. This type of mobility combines the semi-freedom of a mobile device with the energy efficiency and structural integrity of a fixed device. These types of devices are ideal for companies and rehabilitation of lower limbs. |
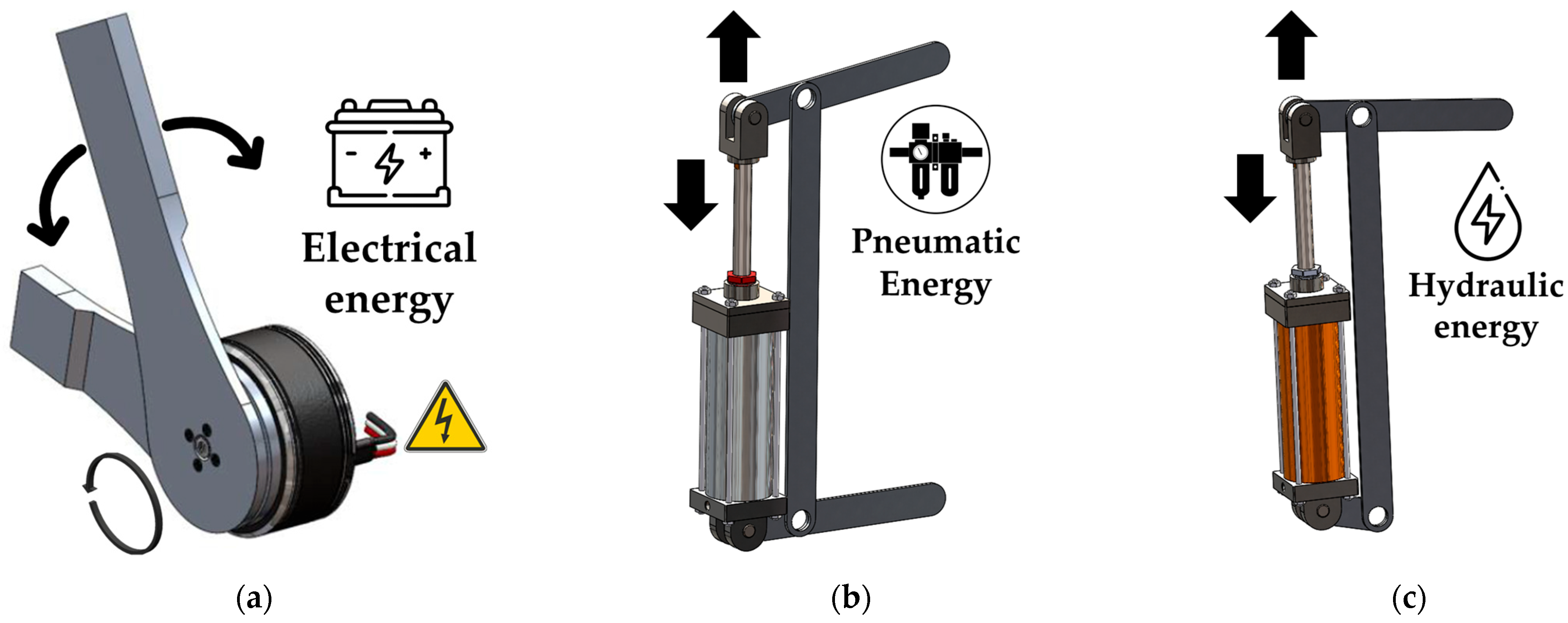
| Energy | Description | Icon |
|---|---|---|
| Electrical (E) | Powers the device hardware Generates the actuation motion |  |
| Hydraulics (H) | Generates the actuation motion |  |
| Pneumatic (N) | Generates the actuation motion |  |
| Without power (M) | Movement generated by mechanical components |  |
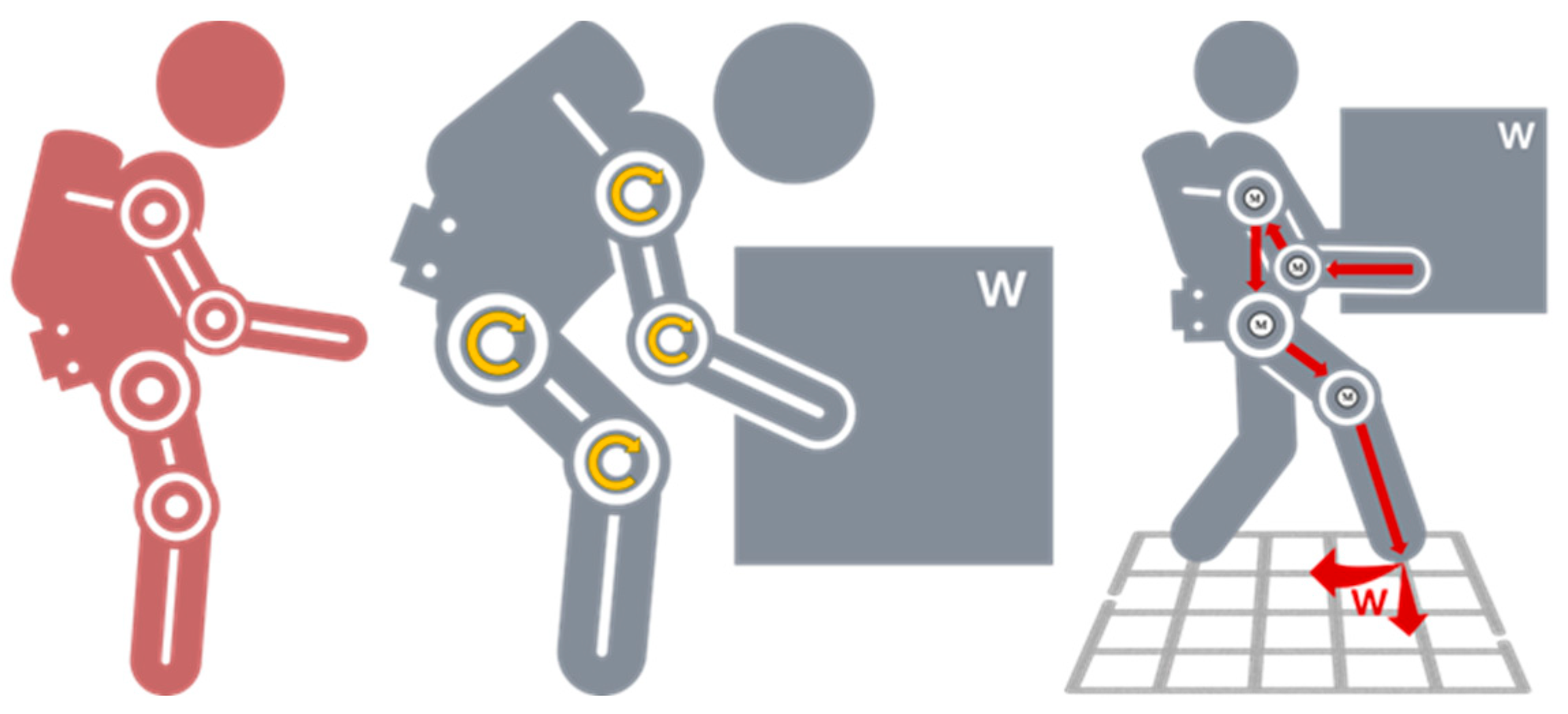
| Exoskeleton | System |
|---|---|
| Mechanical | Passive |
 | A passive mechanical exoskeleton operates without external energy, processing systems, or actuation. Instead, it relies on mechanical structures such as springs, dampers, and elastic components to assist movement and provide support. Its primary function is to enhance ergonomic intervention capabilities by reducing physical strain, improving posture, and minimizing fatigue during repetitive or physically demanding tasks. |
| Robotic | Semi-passive |
 | A semi-passive robotic exoskeleton utilizes external energy sources and processing systems but does not incorporate actuation mechanisms. It is designed primarily for data collection, using sensors and computational systems to monitor and analyze limb movement. This type of exoskeleton is commonly used in research and rehabilitation settings to assess biomechanics, track motion patterns, and provide valuable insights for improving assistive technologies. |
| Semi-active | |
 | An active–passive robotic exoskeleton uses external energy sources, processing systems, and actuation mechanisms for joint rehabilitation, assisting individuals recovering from injuries. It provides controlled assistance to facilitate movement while allowing the user’s muscles to engage, or it can actively block joint movement when needed. This combination of external actuation and natural muscle engagement supports gradual recovery and adaptive rehabilitation strategies. |
| Active | |
| This active–passive robotic exoskeleton harnesses external energy from hydraulic, pneumatic, electrical, and mechanical sources, incorporating advanced processing systems for data control, reception, and transmission. Its actuation function replaces the user’s muscle and joint effort, enhancing ergonomic intervention and absorbing external forces to improve load bearing and mobility. This design enables users to perform physical tasks with greater ease and safety. |
| Dispositive | System | Description | Application |
|---|---|---|---|
| Mechanical Exoskeleton | Passive |
| It is used to enhance ergonomic intervention capabilities. |
| Robotic Exoskeleton | Semi Passive |
| It is used to collect information on limb movement. |
| Semi Active |
| It is used for the rehabilitation of a joint with injury. It is used to block the movement of the joint with actuation. It uses a percentage of movement provided by the system, with the other percentage coming from the muscle. | |
| Active |
| It replaces the total muscle and joint effort. It is used to increase assisted ergonomic intervention. It is used to absorb all external forces that interact with the user, enhancing their load bearing and mobility capacity. |
| Communication | Description | Icon |
|---|---|---|
| Sensors | They allow the device to interpret external and internal elements to collaborate with programmed actions to create behaviors and solutions. |  |
| Control Panel | It is a board that changes the system configuration. The user or a third party controls almost everything about the device’s behavior and operation. |  |
| Electromyography (EMG) | These are analog signals coming from the muscles [47] and the nervous system, which are interpreted as operational amplifiers. |  |
| Electroencephalogram (EEG) | These signals come from the electrical activity in the brain [48]. They are amplified signals, as they fall within the micro to millivolt range, interpreted as operational amplifiers. |  |
| No control | The operation does not require instrumentation. |  |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cruz-Flores, F.; Sánchez-Brito, A.L.; Campos Amezcua, R.; Barrera Sánchez, A.; Azcaray Rivera, H.R.; Martínez Mata, A.J.; Blanco Ortega, A. A Review of Assistive Devices in Synovial Joints: Records, Trends, and Classifications. Technologies 2025, 13, 292. https://doi.org/10.3390/technologies13070292
Cruz-Flores F, Sánchez-Brito AL, Campos Amezcua R, Barrera Sánchez A, Azcaray Rivera HR, Martínez Mata AJ, Blanco Ortega A. A Review of Assistive Devices in Synovial Joints: Records, Trends, and Classifications. Technologies. 2025; 13(7):292. https://doi.org/10.3390/technologies13070292
Chicago/Turabian StyleCruz-Flores, Filiberto, Ana L. Sánchez-Brito, Rafael Campos Amezcua, Agustín Barrera Sánchez, Héctor R. Azcaray Rivera, Arturo J. Martínez Mata, and Andrés Blanco Ortega. 2025. "A Review of Assistive Devices in Synovial Joints: Records, Trends, and Classifications" Technologies 13, no. 7: 292. https://doi.org/10.3390/technologies13070292
APA StyleCruz-Flores, F., Sánchez-Brito, A. L., Campos Amezcua, R., Barrera Sánchez, A., Azcaray Rivera, H. R., Martínez Mata, A. J., & Blanco Ortega, A. (2025). A Review of Assistive Devices in Synovial Joints: Records, Trends, and Classifications. Technologies, 13(7), 292. https://doi.org/10.3390/technologies13070292











