1. Introduction
Amidst the ever-evolving field of healthcare, particularly in terms of systems and technology, a pressing conundrum persists–data silos, interoperability hurdles, and the complexities of efficient communication. The point is that we should look at the healthcare ecosystem and see that these challenges are not impediments but opportunities for transformation.
Healthcare systems grapple with fragmented data and communication bottlenecks. Without robust integration, clinicians face delayed access to critical patient information, administrative staff are burdened by repetitive data entry tasks, and decision making is impaired due to incomplete datasets. This paper posits that a synergy of cutting-edge technologies can be the antidote. GraphQL, renowned for its prowess in efficient data retrieval, promises streamlined communication. openEHR, a stalwart in healthcare data management, champions interoperability through a unified data model. Redis steps in as the stalwart of scalable data storage, unlocking possibilities for real-time data processing. Pervasive Business Intelligence, the herald of data analytics, empowers informed decision-making in the healthcare domain.
The convergence of these technologies presents an opportunity to address the challenges healthcare systems face. By integrating them, healthcare organizations can overcome data silos, enhance interoperability, improve data access and retrieval, and leverage advanced analytics for informed decision-making. This integration also mitigates the negative impacts of disjointed systems, such as inefficiencies in clinical workflows, resource overutilization, and elevated costs associated with redundant or manual processes. This paper delves deeper into each technology, exploring its individual benefits, integration possibilities, and potential synergies in the context of healthcare systems. Through in-depth analysis and a real-world case study, we aim to highlight the transformative potential of this integration and provide insights for future implementations in the healthcare domain.
The manuscript follows a clearly defined structure, consisting of six essential sections.
Section 1 provides the necessary contextualization for the background clarification. Following that,
Section 2 establishes the necessary technical and theoretical foundations. Expanding on this basis,
Section 3, named State of the Art, examines existing literature from a critical perspective, identifying comparable research and their results. This comparative study aims to strengthen the research motivation and outline the main contributions of this work.
Section 4 provides a thorough examination of the particular case study, carefully describing its implementation and results. Following a thorough analysis,
Section 5 delves into a rigorous discourse on the obtained outcomes, analyzing their importance and their consequences. Ultimately, the text concludes with a thorough and all-encompassing part. This final section,
Section 6, emphasizes the conclusions on the actualized implementation and outcomes. Furthermore, it lays the foundation for future research by pinpointing prospective directions for further investigation that are inspired by the established research trajectory.
2. Background
While embarking on an exploration of healthcare’s technological landscape, it is extremely important to provide a foundational understanding of key concepts shaping the industry. Therefore, a technical explanation of the technologies—GraphQL, openEHR, Redis, and Pervasive Business Intelligence—is provided. Each plays a distinctive role, from GraphQL’s prowess in data retrieval to openEHR’s standards-based healthcare data management, Redis’ scalable data storage capabilities, and Pervasive Business Intelligence’s role in comprehensive analytics. By navigating these essential concepts, we set the stage for an in-depth exploration of their integration, aiming to redefine healthcare practices and pave the way for an era marked by advanced data processing, informed decision-making, and elevated patient care standards.
2.1. GraphQL
Efficient data management and seamless information exchange are pivotal in the evolving healthcare landscape. GraphQL, a robust query language, is a promising technology to address these needs. This section delves into the capabilities and potential applications of GraphQL within healthcare systems, highlighting its benefits and integration possibilities [
1].
GraphQL is a query language designed to facilitate efficient data communication between clients and servers by allowing clients to request specific data structures and properties. Unlike traditional REST APIs, which often return fixed data structures, GraphQL enables clients to define the data they require. This ability to retrieve tailored data reduces over-fetching and under-fetching, improving data transmission efficiency [
2,
3].
In healthcare systems, where data accuracy and timely access are paramount, GraphQL offers notable advantages. The flexibility of GraphQL queries accommodates the diverse information needs of different stakeholders, from medical professionals seeking patient records to administrators monitoring resource allocation. This adaptability streamlines data retrieval processes, contributing to faster decision-making and improved patient care [
4,
5].
Furthermore, GraphQL’s hierarchical nature allows for retrieving complex and interconnected healthcare data in a single query, reducing the need for multiple requests. This design pattern is particularly advantageous when retrieving patient data spanning various medical domains, such as medical history, lab results, and prescriptions. The reduced latency in data retrieval improves the overall user experience and facilitates real-time monitoring and intervention [
6].
Moreover, GraphQL’s support for introspection enables automated documentation generation. In healthcare, where data accuracy and compliance are imperative, automatically generated documentation ensures that developers and stakeholders are aligned to understand data structures and available queries. It promotes transparency and reduces the potential for misinterpretation [
7]. While GraphQL presents numerous benefits, it is essential to consider its challenges.
Table 1 presents the summary of advantages and disadvantages of GraphQL usage:
When evaluating technologies for efficient data retrieval in healthcare systems, several alternatives, including REST APIs, were considered. REST APIs are widely adopted and well-suited for straightforward data exchange due to their simplicity and well-established standards. Their extensive adoption ensures compatibility with numerous systems, making them a practical choice for less complex applications. However, REST APIs often fall short in addressing the intricate requirements of modern healthcare environments. Fixed data structures returned by REST endpoints can result in over-fetching or under-fetching of information, introducing inefficiencies and delays that are detrimental to time-critical healthcare operations [
9].
GraphQL was selected over REST APIs primarily due to its ability to tailor data requests to specific client needs, reducing unnecessary data transmission and improving the efficiency of information exchange. This flexibility is crucial in healthcare systems, where stakeholders such as clinicians, administrators, and researchers often require precise, diverse, and rapidly accessible data. Furthermore, GraphQL’s support for hierarchical queries allows for retrieving interconnected data in a single request, enhancing performance and usability, particularly in cases involving complex datasets like electronic health records spanning multiple domains [
9,
10].
2.2. openEHR
The effective management of healthcare data is central to delivering high-quality healthcare services. However, disparate data formats and systems often hinder interoperability and data exchange. This section explores the role of openEHR in addressing these challenges by providing a standardized framework for healthcare data management. It explores the architecture, benefits, and integration possibilities of openEHR within healthcare systems.
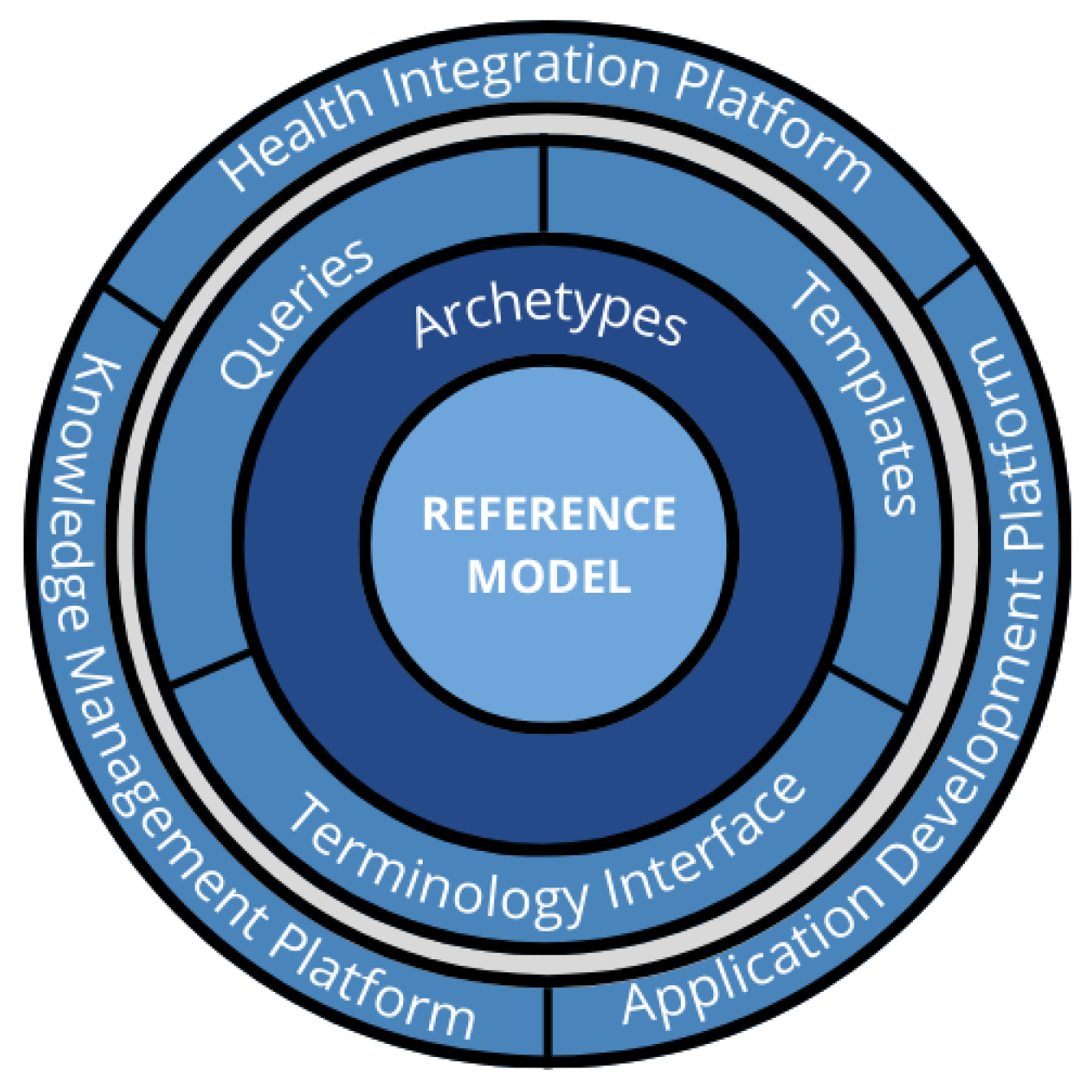
openEHR is an open-source standard designed to support the sharing, exchanging, and storing of Electronic Health Records (EHRs). It offers a dual-level modeling approach: the Reference Model—providing the foundational data structures, and Archetypes—offering domain-specific definitions for clinical concepts. This two-tiered approach ensures both flexibility and consistency in healthcare data representation [
11].
The openEHR architecture consists of three core components: the Reference Model, Archetypes, and Templates. The Reference Model establishes a standard structure for representing health information, ensuring semantic interoperability across different systems. Archetypes capture domain-specific clinical concepts, while Templates provide practical instances of Archetypes for specific use cases. This modular architecture promotes data reusability and adaptability [
12,
13].
Figure 1 provides an overview of the openEHR architecture.
The integration of openEHR with GraphQL enhances data accessibility. GraphQL queries can be constructed to retrieve structured healthcare data directly from openEHR repositories, allowing for precise data retrieval tailored to user needs. Combining openEHR with Redis accelerates data access and caching, reducing frequently accessed clinical information response times. Integrating openEHR’s standardized data with Pervasive Business Intelligence platforms enables advanced analytics and informed decision-making [
5].
The adoption of this standard must be carefully considered since, while it has many benefits, it may also provide certain obstacles.
Table 2 presents a resume of the advantages and disadvantages of openEHR’s use.
When evaluating standards for healthcare data management and interoperability, HL7 FHIR was a key alternative to openEHR. HL7 FHIR is widely recognized for its focus on interoperability and data transmission. Its modular structure and use of commonly adopted IT standards make it highly effective to facilitate data exchange between diverse healthcare systems. Additionally, FHIR provides its own data model, enabling developers to implement interoperability solutions with relative ease. However, its primary emphasis on data transmission and exchange can limit its effectiveness for long-term data persistence and advanced modeling requirements [
15,
16].
In contrast, openEHR focuses on comprehensive data modeling and persistence, making it well-suited for scenarios requiring robust, domain-specific clinical models. Its dual-level architecture separates foundational data structures (Reference Model) from domain-specific content (Archetypes), ensuring semantic interoperability and adaptability over time. While openEHR has expanded to include data transfer specifications using REST APIs, its primary strength lies in creating standardized, reusable clinical information models that ensure consistency and scalability across healthcare applications. This focus on persistent, structured healthcare data gives openEHR a unique advantage for long-term, scalable implementations compared to HL7 FHIR’s interoperability-centric approach [
15,
17].
2.3. Redis
Efficient data storage and rapid data retrieval are indispensable in modern healthcare systems. The exponential growth of healthcare data calls for innovative solutions to manage and access information in real time. This section delves into the capabilities of Redis, a versatile in-memory data store, and explores its application as a scalable data storage and caching system within healthcare contexts.
Redis, short for Remote Dictionary Server, is an open-source, in-memory data structure store that supports various data types such as strings, lists, sets, and hashes. It is known for its exceptional speed and ability to handle high-throughput scenarios. Redis employs an in-memory caching approach, ensuring rapid data access and reducing the need to query databases for frequently accessed information repeatedly [
18].
Redis’ publish–subscribe feature facilitates real-time data updates and event notifications. It proves valuable in scenarios like remote patient monitoring, where continuous data streams from wearable devices must be relayed to medical professionals promptly for timely intervention [
18,
19].
Redis’ integration with other technologies like GraphQL and openEHR enhances its utility. Combining Redis with GraphQL optimizes data fetching by storing frequently accessed data in memory, reducing the load on back-end systems, and improving response times [
20,
21]. When integrated with openEHR, Redis accelerates data retrieval by caching standardized health records, minimizing the need to repeatedly fetch data from distributed repositories [
22].
The advantages and disadvantages of the use of Redis are outlined in
Table 3.
When considering data storage and retrieval solutions, traditional SQL databases were evaluated alongside Redis. SQL databases are well-suited for managing structured data, offering robust querying capabilities, ACID compliance, and transactional integrity. These features make SQL a reliable choice for applications requiring complex analytics or relational data structures. However, SQL databases often struggle with high-throughput, real-time data scenarios due to the overhead of disk-based storage and query optimization processes. In healthcare, where low-latency access to time-sensitive data is vital, this limitation can lead to suboptimal performance [
24,
25].
Redis was selected over SQL databases for its ability to handle high-throughput workloads and deliver real-time data access using its in-memory data store architecture. Its support for diverse data structures, such as hashes and sorted sets, enables flexibility in managing complex healthcare data, including patient monitoring streams and frequently accessed records. Additionally, Redis’ publish–subscribe capabilities facilitate instant notifications and updates, a feature particularly valuable in applications like remote patient monitoring and real-time alerts. While SQL databases remain indispensable for complex analytics, Redis complements healthcare systems with speed and efficiency, where real-time data retrieval is paramount [
24].
2.4. Pervasive Business
The use of data-driven technology is essential in healthcare to improve patient outcomes and optimize resource usage. Pervasive Business Intelligence (BI) plays a vital role in this transformation by offering advanced analytics and visualization capabilities to users at all levels of an organization [
26]. This section explores the significance of Pervasive BI in healthcare, its applications, and its integration with GraphQL, openEHR, and Redis for comprehensive insights and improved healthcare delivery.
Pervasive BI enables users to explore data and gain insights independently, going beyond traditional executive dashboards to make data accessible to everyone in an organization [
27,
28]. This means that clinicians, administrators, and analysts can use data to improve patient care, streamline operations, and plan strategically. In healthcare, Pervasive BI has many applications, including real-time monitoring of patient vitals, effective resource allocation, and identification of potential breakthroughs [
28]. Integration with GraphQL, openEHR, and Redis enhances data consistency and accuracy, expediting query processing for real-time analytics. Though Pervasive BI has many benefits in healthcare, implementing robust data governance frameworks is crucial to overcome challenges such as data security, privacy concerns, and data accuracy and validity. As healthcare generates more data, Pervasive BI’s role will continue to grow. Integrating AI and machine learning with Pervasive BI can provide predictive analytics, aiding in early disease detection and treatment planning. Wearable and Internet of Things (IoT) devices can also be integrated with Pervasive BI for holistic patient insights. Pervasive BI empowers stakeholders with actionable insights and fosters data-driven decisions that can transform patient care, operational efficiency, and strategic planning.
When exploring analytics tools for healthcare, traditional BI platforms like Power BI were considered. Power BI excels in creating detailed reports and dashboards, offering user-friendly interfaces and strong integration with Microsoft ecosystems. It is an excellent choice for centralized data analysis and executive-level reporting. However, traditional BI tools often rely on pre-defined reports and data pipelines, which can limit their adaptability and real-time analytics capabilities. These constraints make them less effective for empowering users at all organizational levels, particularly in dynamic healthcare environments where data needs evolve rapidly.
Pervasive BI was chosen over traditional BI tools for its ability to democratize data access, enabling stakeholders across various roles—clinicians, administrators, and researchers—to independently analyze data and generate actionable insights. Unlike traditional tools, Pervasive BI focuses on real-time analytics and self-service exploration, ensuring that users can respond promptly to emerging trends and anomalies. Its seamless integration with other technologies like GraphQL, openEHR, and Redis enhances data consistency and query performance, making it a more suitable choice for healthcare applications requiring agility and comprehensive data accessibility.
3. State of the Art
When searching the topic under discussion in this paper, there are various topics and respective applications that need to be addressed. Therefore, this section covers topics ranging from the use of the technologies listed above in healthcare institutions to the trends and innovations expected in the future.
Starting with GraphQL, in recent years, the healthcare industry has recognized the potential of GraphQL to address data integration challenges [
4]. Currently, GraphQL is employed to efficiently retrieve patient records, lab results, and other health-related data, improving the responsiveness and speed of EHR systems [
5,
29]. In accordance, this query language also facilitates seamless data exchange between different healthcare systems and organizations, promoting interoperability and collaboration [
4,
5]. More recently, GraphQL is being used to fetch relevant clinical data, aiding in real-time decision-making for healthcare professionals [
30]. These studies underscore the versatility of GraphQL in improving healthcare data management but primarily focus on its stand-alone benefits or limited integrations.
The use of GraphQL in healthcare has been explored in various studies, with promising results. Ref. [
4] demonstrated the performance, cost-effectiveness, scalability, and flexibility of a GraphQL and HL7 FHIR-based approach for Healthcare Information Exchange (HIE). Ref. [
31] proposed a methodology, SQL2Neo, for converting healthcare data from relational to graph databases, which are better suited for handling highly related data. Ref. [
32] presented a framework for efficient data management and data services in large-scale healthcare systems using graph databases, which can reduce complexity and enhance data accessibility. Ref. [
33] reported success in prototyping a problem-oriented medical record for connected health using TypeGraphQL, which can connect to HL7 FHIR medical records and biomedical repositories. These studies collectively highlight the potential of GraphQL in improving data exchange, data management, and data services in healthcare.
Now, focusing on interoperability, using worldwide accepted standards is the right path. openEHR plays a pivotal role in promoting interoperability among heterogeneous healthcare systems. Healthcare organizations can facilitate seamless data exchange across different platforms by adhering to a standardized data model. In addition, openEHR’s focus on semantic interoperability ensures that data retain their intended meaning regardless of its originating system, which is crucial in maintaining the accuracy and context of clinical information [
11,
34]. openEHR is actively collaborating with the Health Level Seven International (HL7) in specific Fast Healthcare Interoperability Resources (FHIR) standards, promoting a synergistic approach to healthcare interoperability [
35].
openEHR has been evaluated for storing computable representations of EHR phenotyping algorithms, demonstrating its potential to accelerate precision medicine [
36]. It has also been identified as a key component in achieving semantic interoperability among International Patient Summary sources in the European Union (EU) [
37]. The use of openEHR archetypes has been shown to be feasible and scalable, with significant reuse across diverse health datasets [
38]. These studies collectively highlight the versatility and potential of openEHR in various healthcare applications.
The implementation of openEHR in Portuguese healthcare facilities has been explored in several studies. Refs. [
34,
39] both discuss the initial steps and the adoption of openEHR in these settings, highlighting the potential for improved knowledge acquisition and clinical decision support.
In the rapidly evolving landscape of healthcare technology, Redis stands out as a crucial asset, revolutionizing the industry with its unparalleled capabilities. As evidenced by [
23], Redis has proven to be invaluable in optimizing the search for medical supplies through the innovative integration of geospatial data. This not only enhances efficiency but also demonstrates a substantial improvement in system working speed when compared to traditional databases. Moreover, the exploration of real-world data in healthcare, with a keen examination of the potential role of Redis, offers valuable insights into the challenges and limitations inherent in this transformative approach, as highlighted by [
40].
The use of GraphQL, openEHR, and Redis in a synergistic manner has been explored in various studies. Ref. [
41] demonstrated the performance benefits of using graph databases, such as Neo4j, for implementing openEHR clinical repositories. This approach could be further enhanced by the use of GraphQL, as suggested by [
42], who compared SPARQL with GraphQL for querying building datasets. Finally, Ref. [
43] presented a system called IBM Db2 Graph, which supports synergistic graph and SQL analytics, potentially enhancing the performance of openEHR systems. These studies collectively suggest that the use of GraphQL, openEHR, and Redis in a synergistic manner could lead to improved performance and efficiency in healthcare data management.
Conclusively, while the studies presented underscore the significant relevance of these technologies in healthcare, it is noteworthy that none of them have explored the tripartite synergy of Redis, openEHR, and GraphQL. This trifecta presents a unique and promising avenue for efficiently managing vast datasets in accordance with globally recognized data standards. The integration of Redis for rapid data retrieval, openEHR for standardized health information exchange, and GraphQL for streamlined data querying and manipulation holds the potential to redefine the landscape of healthcare information systems. Future research endeavors should consider delving into this unexplored territory to unveil the collective power of these technologies, ultimately contributing to the advancement of data management practices in healthcare on a global scale. This unified framework bridges the gap in prior research by demonstrating the synergistic integration of GraphQL, openEHR, and Redis in the scope of healthcare institutions. The proposed solution not only overcomes the limitations of isolated or partial implementations but also sets a foundation for future advancements in healthcare data management. By addressing interoperability, performance, and scalability simultaneously, this approach has the potential to transform healthcare information systems globally, offering new avenues for improved patient care and operational efficiency.
Despite its potential benefits, this integration within a unified framework presents significant challenges that must be addressed to ensure its effective implementation. Interoperability remains a pivotal issue, as aligning data formats, query structures, and semantic standards across heterogeneous systems can be complex. While openEHR provides standardized data models to support semantic interoperability, its integration with GraphQL’s flexible querying capabilities and Redis’ in-memory data architecture necessitates careful coordination to avoid mismatches in schema representations and data exchange processes. Moreover, the real-time analytics demands of Pervasive BI add an additional layer of complexity, requiring seamless data flow and consistent performance across all components of the framework.
Performance optimization and scalability further complicate the integration. Redis’ memory-intensive operations and GraphQL’s hierarchical querying capabilities, while powerful, can strain server resources and increase computational overhead if not carefully managed. Ensuring data security and compliance with regulations such as GDPR introduces additional challenges, particularly when multiple technologies interact, each with its own access points and potential vulnerabilities. Furthermore, the integration demands effective governance and stakeholder collaboration, requiring multidisciplinary coordination among medical professionals, IT specialists, and data analysts. Training stakeholders to leverage the capabilities of the system while managing resistance to change and aligning the framework with clinical workflows are critical for achieving widespread adoption. Addressing these challenges is essential to fully realize the transformative potential of this unified framework in healthcare data management.
4. Case Study
The focal point of this case study is the Centro Hospitalar Universitário do Porto, a community hospital located in Portugal, which endeavors to enhance its medical services through the integration of technology. The hospital’s core mission is to improve the sharing of data across different departments, implement real-time monitoring of patients, and promote data-driven decision-making. In pursuit of these objectives, the hospital has embraced GraphQL to streamline data retrieval, incorporated openEHR to standardize health records, employed Redis for accelerated data access, and implemented Pervasive Business Intelligence for informed insights, combined in a web interface that can replace its EHR.
4.1. Requirement Collection
The requirement collection process was a pivotal step in ensuring the successful design and implementation of the proposed study. This process involved a combination of focus-group interviews and observational studies, which enabled a thorough understanding of the system’s needs from multiple perspectives. Stakeholders, including medical professionals, IT experts, and data analysts, actively participated in this phase to ensure that their diverse expertise and expectations were adequately addressed. The construction of focus groups was a deliberate and structured process, designed to ensure that the diverse perspectives and expertise of stakeholders were adequately represented and effectively harnessed. This approach was key for the comprehensive collection of system requirements, as it facilitated targeted discussions and fostered collaboration among participants. A key initial step in building focus groups was the identification and segmentation of stakeholders into distinct categories based on their roles and expertise. This resulted in 3 major groups, as follows:
To improve the effectiveness of the focus groups created, independent agendas were developed to align discussions with the domain knowledge and priorities of the participants. Moderators facilitated the focus group sessions, involving participants so that they could freely share their insights and engage in constructive dialogue. Indeed, moderators ensured that all inside the meeting were heard and that discussions remained focused on the objectives of the study. The Clinical Staff group was composed of physicians, nurses, and administrative staff who interact directly with healthcare workflows and patient care. Their insights were invaluable in understanding clinical processes, patient data requirements, and regulatory compliance issues. The discussions centered around clinical workflows, the accessibility and usability of patient data, and ensuring compliance with healthcare regulations. Key topics included real-time data needs and the integration of diverse data sources. Comprising system architects, database administrators, and developers, this group focused on the technical infrastructure, system integration, and security challenges associated with the proposed solution. This group addressed the technical challenges of system integration, focusing on topics such as the feasibility of integrating technologies like GraphQL, openEHR, and Redis. Security protocols and strategies for ensuring scalability and reliability were also emphasized. Not least important is the Data Analysts and Management group, which comprises professionals who are responsible for interpreting healthcare data to support operational and strategic decision-making, and the actual decision-makers. Their expertise provided essential input on data formats, reporting capabilities, and opportunities for leveraging advanced analytics.
4.2. Implementation Requirements
The abovementioned focus groups in their sessions explored the requirements for data visualization, reporting, and analysis. The discussions included the need for advanced analytics, predictive modeling, and support for heterogeneous data formats. These focus groups resulted not only in a list of functional, non-functional, technical, and security requirements but also in the identification of possible bottleneck points for the proposed tasks. The following list presents the most important requirements with their categorization:
User-friendly interfaces tailored to healthcare workflows (functional);
Support for diverse data formats (functional);
Real-time data retrieval (functional);
System reliability (non-functional);
System scalability (non-functional);
High-performance data processing (non-functional);
Compatibility with existing systems or Legacy Data Integration (technical);
Adherence to interoperability standards (technical);
Compliance with GDPR (security);
The focus groups also pinpointed some opportunities for leveraging emerging technologies like AI for predictive analytics and enhanced decision-making, and this completely aligns with the preconized implementation. Moreover, stakeholders helped prioritize requirements based on urgency, feasibility, and impact. In the end, the main focus was to align perspectives across groups and ensure that all requirements served the overarching goal of improving healthcare system efficiency and patient outcomes.
To ensure an effective implementation of the framework, the prioritization of requirements was guided by stakeholder input, technical feasibility, and resource constraints. Stakeholder input played a pivotal role, as the success of the system depends on addressing the specific needs of end users, including medical professionals, IT specialists, and data analysts and management. This input was gathered through a series of interviews and workshops, in which stakeholders were asked to rank the importance of various functionalities, such as real-time data access, interoperability with existing systems, and data visualization capabilities.
In parallel, technical feasibility was assessed by evaluating the complexity of integrating identified requirements with the capabilities of GraphQL, openEHR, Redis, and Pervasive BI. High-priority requirements were those that aligned closely with the technologies’ strengths and could be implemented with minimal modifications. Finally, resource constraints, including time, budget, and available expertise, influenced the prioritization process. Requirements that required extensive customization or significant investment in infrastructure were unprioritized for the initial phase, ensuring that the project remained practical and achievable within the scope of the case study. This systematic approach allowed for a balanced prioritization that met significant user needs while staying within practical limitations.
4.3. Interface Design
The interface design process employed an iterative prototyping methodology, widely recognized for its effectiveness in the development of user-centered systems. This approach facilitated the development of an interface that evolved through successive iterations, each informed by stakeholder feedback and usability testing. Initial low-fidelity prototypes were designed to outline the system’s fundamental layout and functionalities. These prototypes provided a basis for early evaluation and refinement. As the process advanced, higher-fidelity prototypes were developed, incorporating increasingly complex features and addressing usability challenges identified during earlier phases. This iterative approach ensured that the final interface aligned with the functional requirements and practical needs of end-users, fostering an intuitive and efficient user experience.
The involvement of key stakeholders was a key point to the success of the interface design process. Stakeholders included medical professionals, IT specialists, and data analysts, whose diverse expertise and operational insights informed the system’s development. Engagement activities comprised semi-structured interviews, collaborative workshops, and iterative feedback sessions. These activities aimed to capture stakeholder’s perspectives on essential functionalities, usability concerns, and workflow integration. Regular meetings with task-based work groups provided opportunities to test each iteration of the prototype, ensuring that the evolving interface met the practical demands of clinical environments. This collaborative process not only validated design decisions but also fostered stakeholder ownership of the system.
The final interface integrates seamlessly with the underlying system architecture, which comprises GraphQL middleware, openEHR repositories, Redis cache, and the Pervasive BI platform. Its design focuses on addressing user needs for efficiency, accuracy, and accessibility, as identified during stakeholder engagement. The main features include the following:
Personalized Dashboards: customized views tailored to medical professionals’ specific roles, displaying real-time patient data and operational metrics to support timely decision-making.
Dynamic Data Visualization: interactive charts and graphs that provide actionable insights into patient health trends and institutional performance, enhancing data comprehension.
Customizable Query System: integration with GraphQL’s introspection capabilities enables users to tailor data queries to their specific requirements, facilitating efficient and targeted data retrieval.
Responsive Design: a layout optimized for multiple devices, ensuring accessibility in diverse clinical settings such as hospitals, outpatient clinics, and administrative offices.
Fast Data Access: leveraging Redis’ in-memory caching architecture for rapid retrieval of frequently accessed information, improving response times during crucial workflows.
These features were designed to optimize clinical and operational outcomes, ensuring the interface is both functional and adaptable to the dynamic needs of healthcare environments.
The overall system architecture is depicted in
Figure 2. This architecture illustrates the integration of GraphQL middleware for streamlined data requests, openEHR repositories for standardized data storage, Redis cache for rapid data access, and the Pervasive BI platform for analytics and visualization. The interface acts as a front-end application, enabling medical professionals to interact with the system efficiently.
An early prototype of the interface, shown in
Figure 3, demonstrates the initial design and functionality of the user interface. This prototype was instrumental in refining the system through stakeholder feedback and iterative improvements.
The integration of GraphQL, openEHR, Redis, and Pervasive BI through the developed interface produced several notable outcomes. Using GraphQL’s tailored queries and Redis’ caching mechanisms, data retrieval times were significantly reduced, enabling near-instantaneous access to patient information. The standardization of healthcare records via openEHR ensured data consistency and facilitated accurate analysis across heterogeneous systems. The Pervasive BI platform, integrated within the interface, enabled the creation of dynamic, real-time dashboards for patient monitoring and operational oversight. These features collectively improved resource allocation, supported timely clinical interventions, and enhanced decision-making processes at multiple levels within the healthcare organization.
The platform’s contextualized analytics and customized user interfaces enable healthcare professionals and administrators to perform a variety of analytical queries tailored to clinical and operational needs. Clinically, the interface supports tracking patient vitals, monitoring treatment progress, and analyzing trends in chronic disease management. These features allow for a granular understanding of individual and aggregate patient outcomes. Operationally, the system facilitates queries for resource allocation, such as bed occupancy, equipment usage, and staff workload, providing actionable insights to improve hospital efficiency. Advanced capabilities include predictive analytics to identify patients at risk of complications or readmissions and allow proactive interventions. The integration of GraphQL ensures that these queries are highly customizable, while Redis provides rapid data retrieval to support real-time analytics. openEHR guarantees that all data accessed adhere to standardized formats, enhancing interoperability and consistency across the system. By delivering these insights through dynamic and user-friendly dashboards, the system empowers stakeholders to make data-driven decisions quickly and efficiently.
4.4. Cross-Functional Team Collaboration Methodology
The success of this project is heavily dependent on the ability to bring together medical professionals, IT experts, and data analysts to work collaboratively. Each group brought unique perspectives, so a structured approach was necessary to align their efforts and ensure the project stayed on track. To achieve this, the SCRUM framework was adopted, focusing on iterative development and open communication. Regular meetings, such as daily stand-ups, sprint planning, and retrospectives, created opportunities for the team to share updates, address challenges, and refine strategies. These frequent interactions ensured transparency and helped everyone stay aligned with the project’s goals.
Collaboration was also supported by digital tools. Project management software made it easier to track tasks and allocate resources, while communication platforms like Slack or Teams allowed for instant messaging and quick problem-solving. Shared repositories were set up so that all team members could access and update key documents, code, and data. In addition, interdisciplinary workshops were organized to promote mutual learning. Medical professionals explained clinical workflows, while IT experts and data analysts clarified technical and analytical processes. These sessions ensured that everyone understood how their work contributed to the larger picture.
However, such collaboration was not without its challenges. One of the main issues was the different terminologies and ways of thinking each group brought to the table, which sometimes led to confusion. To address this, the team created a shared glossary of terms and encouraged everyone to simplify their language during discussions. Regular cross-training sessions also helped build a common understanding among team members. Another challenge was balancing priorities. Medical professionals naturally focused on patient care, IT experts prioritized system stability, and data analysts were most concerned with data accuracy. These differences were resolved by the SCRUM product owner, who worked to mediate and align priorities with the broader goals of the project. Scheduling meetings was also difficult, especially for medical professionals with demanding schedules. To accommodate this, the team opted for flexible meeting times and relied on asynchronous updates when necessary.
In the end, this cross-functional collaboration approach proved to be highly effective. By addressing communication barriers and finding ways to align diverse priorities, the team was able to develop a tool that was not only technically sound but also met the practical needs of its users. This experience highlighted the value of a structured yet flexible approach to teamwork in interdisciplinary projects, setting a strong foundation for future initiatives.
4.5. Data Governance and Compliance
Implementing robust data governance and security frameworks is essential in healthcare development to protect sensitive patient information, ensure data integrity, and comply with regulatory standards [
44]. Therefore, during this study, a robust data governance framework was implemented, outlining clear policies, standards, and roles. IT teams managed technical safeguards, management ensured GDPR adherence, and clinical staff and data analysts maintained data accuracy. Regular updates and audits strengthened the framework’s effectiveness. Security measures included industry-standard encryption for data in transit and at rest, along with role-based access controls to restrict unauthorized access. These measures, aligned with openEHR’s architecture, ensured robust protection. A key advantage of openEHR is its separation of demographic and clinical data, which supported GDPR compliance [
45]. By isolating personally identifiable information, the system reduced the risk of unauthorized access and facilitated data anonymization, enhancing privacy and enabling secure data sharing for research and operational purposes. This approach balanced data protection with usability, ensuring regulatory compliance and operational efficiency.
5. Discussion
This manuscript and study emphasizes the effort behind creating an EHR designed to comply with healthcare workflows at the Centro Hospitalar Universitário do Porto. The system integrates not only technologies such as GraphQL, Redis, and Pervasive Business Intelligence but also healthcare standards like openEHR, to tackle the specific demands of clinical staff and the management board. Through a systematic requirement collection process involving diverse stakeholder groups—clinical staff, IT experts, and data analysts—key system needs were identified and addressed, ensuring that the solution aligned with practical demands and technical feasibility. One of the most important outcomes was the observed improvement in clinical efficiency and workflow speed achieved. By consolidating dispersed data into a unified, user-friendly interface, healthcare professionals could access patient information in near real-time. The integration of GraphQL middleware and Redis caching mechanisms reduced data retrieval times during our preliminary evaluations. These settings and architecture enabled faster decision-making during pressing moments. Moreover, efficiency gains translate directly into reduced administrative burden and increased time for patient care, showcasing the implementation’s potential to optimize resource allocation in the clinical domain. The application also demonstrates transformative potential in healthcare delivery. With features like personalized dashboards, dynamic data visualization, and real-time monitoring capabilities, healthcare professionals are equipped to make data-driven decisions with greater accuracy and confidence. These functionalities have improved operational oversight and patient care by reducing diagnostic errors and promoting timely interventions. Although the app is in its early deployment stages, stakeholders have reported enhanced collaboration and communication across departments, further strengthening its impact on care quality. As of now, the application is actively used by over 50 healthcare professionals, including physicians and nurses, across multiple departments, but with a greater focus on the Internal Medicine Department. Feedback is collected systematically through user surveys, focus groups, and usability testing sessions, ensuring a comprehensive understanding of user experiences and areas for improvement. Key aspects of feedback include interface usability, system reliability, and the effectiveness of data visualization tools. In initial user feedback, the app’s intuitive design and its ability to streamline data access led to over 80% of users expressing satisfaction with its performance. The expected impact of the application extends beyond clinical efficiency to include cost reduction, resource optimization, and improved patient outcomes. Preliminary analysis suggests that the app could reduce administrative workload and cut operational costs related to data management. These projections are based on task analysis and usage patterns observed during initial deployment. Future assessments will focus on quantifying broader impacts, including reduced hospital stay durations and improved patient satisfaction scores. Additionally, longitudinal studies are planned to evaluate the app’s effect on clinical decision-making accuracy and error reduction over a 12-month period. Despite its early successes, the project faced several challenges, including aligning the diverse priorities of clinical, technical, and analytical teams. These were mitigated through structured collaboration methodologies, such as SCRUM, and tools like shared repositories and communication platforms. Another significant challenge was ensuring compliance with data governance regulations, particularly GDPR. By leveraging openEHR’s robust data separation architecture, the app ensured secure and standardized data handling while maintaining operational efficiency. To build upon these initial successes, the project will focus on expanding user adoption, refining interface functionalities, and integrating predictive analytics powered by AI. These enhancements aim to further improve healthcare delivery by enabling advanced decision-making and resource planning capabilities. This case study demonstrates the potential of leveraging interdisciplinary collaboration and innovative technologies to address complex challenges in healthcare. The developed application not only improves clinical efficiency and speed but also sets a strong foundation for transforming healthcare delivery. With ongoing refinements and a commitment to a user-centered design, this solution promises to make a lasting impact on the quality and efficiency of medical care.
6. Conclusions
This conclusion section encapsulates the essence of this research by synthesizing its key findings and charting a course for future advancements. To provide clarity and focus, it is structured into two subsections: the main contributions and the future work guidelines. The first subsection highlights the transformative potential of integrating GraphQL, openEHR, Redis, and Pervasive Business Intelligence in addressing crucial challenges in healthcare systems. The second subsection outlines a forward-looking agenda, emphasizing the need to tackle implementation hurdles, validate findings across diverse settings, and explore emerging analytics technologies. Together, these discussions aim to underscore the significance of this work while setting the stage for continued innovation.
6.1. Main Contributions
This article delves into the potential advantages of combining GraphQL, openEHR, Redis, and Pervasive Business Intelligence in healthcare systems. Each technology offers distinct benefits. GraphQL streamlines data retrieval, openEHR standardizes healthcare data, Redis accelerates data access, and Pervasive Business Intelligence enables data-driven decision-making. This exploration has yielded significant findings and contributions.
Primarily, integrating these technologies provides a comprehensive solution to long-standing healthcare system issues. It promotes interoperability, enhances data accessibility, accelerates data processing, and empowers stakeholders with valuable insights. As a result, patient care is improved, operations are streamlined, and informed decision-making is possible across all levels of healthcare organizations.
Furthermore, the real-world case study presented in this article showcases the practical advantages of integration. It demonstrates how these technologies can be seamlessly integrated to create a more efficient and effective healthcare system. The results of the case study highlight the tangible benefits of this integration, ranging from reduced data retrieval times to enhanced patient monitoring and resource optimization.
6.2. Future Work
While this study presents promising outcomes, it also opens avenues for further research and development. Future work will focus on addressing implementation challenges, such as ensuring data security, scalability, and compliance with evolving healthcare regulations. Additional case studies across diverse healthcare settings will be conducted to validate the generalizability and robustness of the proposed integration. Furthermore, incorporating advanced analytics, such as predictive modeling through AI and machine learning, will be explored to unlock new opportunities for early disease detection and personalized medicine. This ongoing research aims to refine and expand the application of these technologies to fully realize their transformative potential in healthcare systems.